Abstract
Objective
Asian Americans have low prevalence of overweight/obesity based on standard BMI cut points yet have higher rates of diabetes. We examined the prevalence of overweight/obesity, using lower BMI cut points recommended by the World Health Organization (WHO) for Asians, and diabetes in Asian American subgroups in California.
Method
Secondary analysis of the 2009 adult California Health Interview Survey (n = 45,946) of non-Hispanic Whites (NHW), African Americans, Hispanics and Asians (Vietnamese, Chinese, Korean, Filipino, South Asian and Japanese). WHO Asian BMI cut points (overweight = 23–27.5 kg/m2; obese ≥ 27.5 kg/m2) were used for Asian subgroups. Standard BMI cut points (overweight = 25–29.9 kg/m2; obese ≥ 30 kg/m2) were applied for other groups.
Results
Among Asian subgroups, overweight/obesity was highest among Filipinos (78.6%), which was higher than NHWs (p < 0.001) but similar to African Americans and Hispanics. Compared to NHW, diabetes prevalence was higher for Vietnamese, Koreans, Filipinos and South Asians with BMI = 23–24.9 kg/m2 and Koreans, Filipinos and Japanese with BMI = 27.5–29.9 kg/m2, the ranges WHO recommends as overweight or obese for Asians but not for other groups.
Conclusions
Filipinos should be a priority population for overweight/obesity screening. Filipinos, Vietnamese, Korean, South Asians and Japanese have higher diabetes prevalence at lower BMI cut points. WHO Asian BMI cut points may have clinical utility to identify at-risk Asian Americans.
Keywords: Obesity, Overweight, Type 2 diabetes mellitus, Asian Americans, Minority health
Introduction
Overweight/obesity is a global and growing public health problem associated with type 2 diabetes and cardiovascular disease (Manson and Bassuk, 2003; Must et al., 1999). Recent recognition of obesity as a disease by the American Medical Association underscores the importance of appropriate identification and treatment of obesity in clinical settings (American Medical Association, 2013). Body mass index (BMI) is a convenient surrogate measure of body fatness in clinical settings and has strong associations with health risks and mortality across populations. The standard BMI cut points that World Health Organization (WHO) has recommended since 1993 are 25–29.9 kg/m2 for overweight and ≥30 kg/m2 for obese, which have been adopted by most countries as the standard overweight/obesity cut points (World Health Organization, 1995).
For the same amount of body fat, age and sex, Asians tend to have a consistently lower BMI by about 2–3 kg/m2 in comparison to Whites, partly due to differences in body build and muscularity (Deurenberg et al., 2002). Moreover, conventional cut points for overweight/obesity do not correspond to similar absolute or relative metabolic risk in all ethnic groups (Pan et al., 2004; Simmons et al., 1991; World Health Organization, 2004; World Health Organization et al., 2000). Based on these shortcomings of the BMI measure in Asian populations, a WHO Expert Consultation panel, using all available data from Asian countries, in 2002 proposed lowering BMI cut points to trigger public health action for Asians, categorizing 23–27.5 kg/m2 as overweight and BMI ≥27.5 kg/m2 as obese (World Health Organization, 2004). However, there has been debate on the adoption of Asian specific BMI cut points, particularly in Westernized countries (Low et al., 2009; Pan and Yeh, 2008; Razak et al., 2007; Stevens, 2003).
In the United States (US), Asian Americans have low rates of overweight/obesity defined by the standard BMI cut points compared to non-Hispanic Whites (NHW), African Americans and Hispanics (Bates et al., 2008; Lauderdale and Rathouz, 2000; Ogden et al., 2013; Wang and Beydoun, 2007). Despite a relatively favorable body weight profile, Asian Americans suffer from a disproportionate burden of type 2 diabetes and associated metabolic abnormalities (Karter et al., 2013; King et al., 2012; Lee et al., 2011; Palaniappan et al., 2011). Consistently, type 2 diabetes has been found to develop at a lower BMI in Asians (Chan et al., 2009; Chiu et al., 2011; Karter et al., 2013; Lee et al., 2011; McNeely and Boyko, 2004; Steinbrecher et al., 2012; Wander et al., 2013). The application of the WHO Asian BMI cut points may provide better estimates of health conditions attributable to overweight/obesity using more population-appropriate cut points (Karter et al., 2013; King et al., 2012; Palaniappan et al., 2011) but are currently not recommended as screening guidelines for clinical use (American Diabetes Association, 2013; Moyer, 2012; National Institutes of Health, 1998). Using standard BMI cut points to examine overweight/obesity among Asians American subgroups may underestimate its impact in these populations.
Few studies have examined overweight/obesity in Asian Americans, defined by the WHO Asian BMI cut points, compared to rates seen in other major racial/ethnic groups. We compared the prevalence of overweight/obesity among Asian Americans subgroups using the WHO Asian BMI cut points to its prevalence among NHW, African American and Hispanic respondents, using the standard cut points. We also examined the prevalence of self-reported diabetes among respondents with BMI of 23–24.9 kg/m2 or 27.5–29.9 kg/m2, the two BMI ranges differentially classified by the WHO for Asians and compared to other groups.
Methods
Study design and sample
We used publicly available cross-sectional data from the 2009 California Health Interview Survey (CHIS), a population-based random-dial telephone survey of non-institutionalized Californians administered since 2001 by the University of California Los Angeles Center for Health Policy and Research. CHIS was conducted in English, Spanish, Mandarin, Cantonese, Korean and Vietnamese languages. The 2009 survey oversampled Korean and Vietnamese populations. The CHIS uses complex weighting to provide representative population estimates that account for the differential sampling rates and participant non-response (California Health Interview Survey, 2011) and imputes missing responses on specific items. The response rate for the adult extended survey was 49% in 2009 (California Health Interview Survey, 2011).
We restricted our analysis to non-pregnant adults aged 18 and older who self-reported solely as NHW, non-Hispanic African American, Hispanic or non-Hispanic Asian. We further restricted attention to 6 major non-Hispanic Asian subgroups (Chinese, Filipino, Japanese, Korean, South Asian and Vietnamese) among respondents that reported only one Asian ethnic group. The overall non-Hispanic Asian sample includes other Asian subgroups and respondents who report more than one Asian ethnicity.
Measures
All measures were based on self-report by respondents. BMI was calculated by self-report of height and weight and provided by CHIS. We examined overweight/obesity by using standard BMI cut points in NHW, African American and Hispanic populations, and the WHO Asian BMI cut points in Asian groups. Using the standard cut points, the 3 BMI categories are as follows: 18.5–24.9 kg/m2 (normal weight), 25–29.9 kg/m2 (overweight) and ≥30 kg/m2 (obese) (World Health Organization, 1995). Using the WHO Asian BMI risk cut points, the 3 categories are 18.5–22.9 kg/m2 (normal weight), 23–27.5 kg/m2 (overweight) and ≥27.5 kg/m2 (obese) (World Health Organization, 2004). We also examined BMI using 5 categories (18.5–22.9, 23–24.9, 25–27.49, 27.5–29.9 and ≥30 kg/m2) incorporating cut points from the standard and WHO Asian BMI scale. Respondents with BMI < 18.5 kg/m2 were restricted from analysis.
We also examined select socio-demographic characteristics including age, sex, nativity, years lived in the US for those foreign born and language spoken at home. The self-reported prevalence of tobacco use (current smoker, never smoker and prior smoker), type 2 diabetes, hypertension and heart disease were assessed.
Statistical analysis
We used complex survey methods available in Stata Version 12.1 [Stata Corp, College Station, TX]. Following CHIS guidelines, we incorporated the survey weights in all analyses and used jackknife methods to obtain standard errors, confidence intervals and p-values. Statistical significance was set at p < 0.05 level.
We used a multinomial logit model in combination with regression standardization to estimate age, sex and nativity adjusted prevalence of overweight and obesity by race/ethnicity. For each Asian subgroup, an overall test of equality of the prevalence of overweight and obesity was performed relative to NHW, African American and Hispanic groups.
We also used a logistic model with regression standardization to estimate age, sex and nativity adjusted prevalence of type 2 diabetes, hypertension and heart disease by race/ethnicity in each of the 5 BMI categories described earlier. In particular, we focused on prevalence of diabetes in the category 23–24.9 kg/m2, in which Asians are considered overweight by the WHO guidelines while non-Asians are not, and in the category 27.5–29.9 kg/m2, in which Asians are considered obese but the other the groups are classified as overweight.
In addition, we examined the sensitivity, specificity, percent correctly classified and the area under receiver operating characteristic curve (AUROC) of standard and WHO Asian BMI cut points for overweight/obesity for detecting prevalent type 2 diabetes, hypertension and heart disease. AUROC estimates were compared using bootstrap resampling.
In both models, we accommodated violations of the linearity assumption for age using a restricted cubic spline transformation. In sensitivity analyses, given the association between smoking and obesity (Mackay et al., 2013) and the great variability in smoking prevalence by sex and racial subgroups across Asian populations (Maxwell et al., 2012), we checked for differences in the effect of race/ethnicity by smoking status on the measures of overweight and obesity.
Given that we used publicly available de-identified data for all analyses, it was determined that our study did not meet the definition of human subject research based on guidelines provided by our institution’s Committee on Human Research.
Results
The 2009 CHIS sample included 45,946 respondents eligible for analysis. Table 1 illustrates weighted unadjusted sociodemographic and health characteristics for each racial/ethnic group.
Table 1.
Sociodemographic and health characteristics by racial/ethnic group from the 2009 California Health Interview Survey. Means and percentages are weighted to be representative of the target populations in California. All cell values are percentages unless otherwise indicated.
| NHW (n = 31,085) | African American (n = 1,848) | Hispanic (n = 8,222) | Total Asian (n = 4,791)* | Vietnamese (n = 1,403) | Chinese (n = 1,006) | Korean (n = 930) | Filipino (n = 425) | South Asian (n = 398) | Japanese (n = 364) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age, mean, years | 49.2 | 46.3 | 40.1 | 43.4 | 42.1 | 45.2 | 38.3 | 45.1 | 38.5 | 57.1 |
| Female | 50.6 | 54.3 | 48.5 | 52.7 | 49.0 | 51.3 | 71.1 | 51.6 | 40.0 | 60.3 |
| Nativity | ||||||||||
| US | 91.0 | 89.5 | 42.2 | 27.9 | 20.0 | 21.3 | 34.6 | 31.6 | 14.8 | 76.8 |
| Asia | 2.8 | 1.1 | 0.1 | 70.8 | 79.9 | 76.8 | 65.4 | 67.8 | 82.1 | 22.0 |
| Other | 6.2 | 9.4 | 57.7 | 1.3 | 0.1 | 1.9 | – | 0.6 | 3.1 | 1.2 |
| Years lived in the US for foreign born | ||||||||||
| ≤1–4 | 7.1 | 31.7 | 5.7 | 8.9 | 7.2 | 8.1 | 18.0 | 6.9 | 11.5 | 7.0 |
| 5–9 | 6.7 | 5.9 | 10.0 | 11.9 | 8.9 | 7.8 | 18.2 | 10.8 | 24.4 | 4.2 |
| 10–14 | 9.6 | 7.3 | 16.1 | 14.7 | 7.3 | 18.2 | 10.4 | 10.8 | 20.2 | 11.0 |
| 15+ | 76.5 | 55.2 | 68.2 | 64.5 | 76.5 | 65.8 | 53.3 | 71.5 | 44.0 | 77.7 |
| Language spoken at home | ||||||||||
| English | 89.8 | 91.0 | 19.7 | 24.3 | 9.1 | 14.6 | 12.1 | 35.0 | 20.7 | 75.6 |
| Asian | – | – | – | 19.7 | 33.2 | 36.4 | 34.7 | 3.2 | 5.9 | 1.3 |
| English and Asian | 0.2 | 0.2 | 0.1 | 48.0 | 54.1 | 37.7 | 47.5 | 54.3 | 72.0 | 1.3 |
| Body mass index, mean, kg/m2 | 26.5 | 27.9 | 28.1 | 23.9 | 23.2 | 23.2 | 22.7 | 25.5 | 23.6 | 24.6 |
| Tobacco use | ||||||||||
| Current | 14.3 | 16.6 | 12.9 | 10.3 | 14.8 | 5.0 | 20.8 | 11.6 | 9.4 | 9.0 |
| Prior | 30.2 | 20.1 | 17.4 | 12.4 | 17.0 | 9.6 | 15.5 | 15.2 | 5.1 | 25.1 |
| Never | 55.5 | 63.2 | 69.7 | 77.3 | 68.3 | 85.4 | 63.7 | 73.1 | 85.5 | 65.9 |
| Type 2 diabetes | 5.4 | 10.8 | 8.5 | 6.7 | 2.4 | 4.3 | 5.5 | 12.7 | 4.9 | 10.1 |
| Hypertension | 27.6 | 36.4 | 24.4 | 22.5 | 21.3 | 20.1 | 13.1 | 34.9 | 10.4 | 35.3 |
| Heart disease | 7.4 | 5.8 | 4.5 | 3.4 | 1.6 | 4.2 | 1.3 | 3.7 | 2.5 | 9.2 |
US = United States; “–” represents 0; NHW = non-Hispanic White;
total Asian population also includes other Asian subgroups and respondents with more than one Asian ethnicity.
Among the 6 Asian subgroups, mean BMI was highest among Filipinos (25.5 kg/m2), but this was lower than the means for the NHW, African Americans and Hispanic groups. Filipinos also reported the highest prevalence of type 2 diabetes (12.7%) across all groups, while Vietnamese and Chinese had the lowest prevalence of diabetes overall.
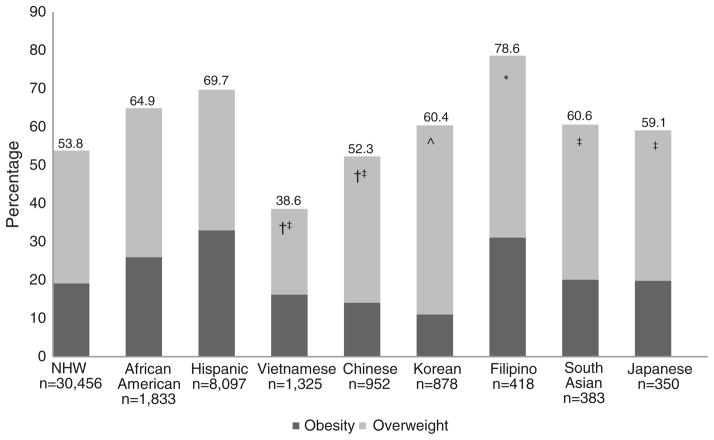
Fig. 1 shows the age, sex and nativity adjusted prevalence of overweight/obesity for each racial/ethnic group, using the WHO cut points for Asians and the standard cut points for the other three groups. Across all groups, the combined adjusted prevalence of overweight/obesity was highest among Filipinos (78.6%) followed by Hispanics (69.7%) and African Americans (64.9%). The prevalence of overweight/obesity was not statistically different between Filipinos and Hispanics (p = 0.15) and African Americans (p = 0.06). However, Filipinos had significantly higher prevalence of overweight/obesity than NHW (p < 0.001).
Fig. 1.
Weighted prevalence of overweight/obesity by racial/ethnic group adjusting for age, sex and nativity in a multinomial logistic model from the 2009 California Health Interview Survey. For non-Hispanic Whites (NHW), African American and Hispanic groups, bar represents overweight (BMI = 25–29.9 kg/m2) and obesity (body mass index [BMI] ≥ 30 kg/m2) using standard BMI cut points. For each Asian subgroup, bar represents overweight (BMI = 23–27.49 kg/m2) and obesity (BMI ≥ 27.5 kg/m2) using the World Health Organization Asian-specific BMI cut points. Prevalence of overweight/obesity among Asian subgroups was compared to other racial/ethnic groups. Statistically significant differences (p < 0.05) are indicated as follows: *versus NHW, †versus African American, ‡versus Hispanic and ^versus NHW, African American and Hispanic.
Among the other Asian ethnicities, in addition to Filipinos, the prevalence of reported overweight/obesity was over half among South Asians (60.6%), Koreans (60.4%), Japanese (59.1%) and Chinese (52.3%). The prevalence of overweight/obesity among South Asians was similar to NHWs (p = 0.33) and African Americans (p = 0.53). While the prevalence of overweight/obesity among Koreans was lower than African Americans and Hispanics (p < 0.01 for each comparison), Koreans had a higher prevalence of overweight/obesity than NHW (p = 0.01). The adjusted prevalence of overweight/obesity in the Japanese group was comparable to the prevalence among NHWs (p = 0.32) and African Americans (p = 0.26). The prevalence of overweight/obesity among Chinese was similar to NHWs (p = 0.41). Vietnamese (38.6%) ethnicity had the lowest prevalence of overweight/obesity, which was consistent with their lower prevalence of type 2 diabetes compared to the other racial/ethnic groups.
Table 2 presents age, sex and nativity adjusted prevalence ratios (APR) for overweight or obesity versus normal weight for each race/ethnicity compared to NHW. Filipinos were more likely to be overweight or obese as NHWs (overweight APR 2.94, 95% CI 1.60–5.39; obese APR 3.49, 95% CI 1.92–6.34) and African Americans (overweight APR 2.00, 95% CI 1.08–3.70; obese APR 1.95, 95% CI 1.06–3.58). However, the relative prevalence of overweight or obesity was similar among Filipinos and Hispanics (overweight APR 1.82, 95% CI 0.99–3.35; obese APR 1.32, 95% CI 0.69–2.53). The prevalence of overweight was similar among Chinese, Korean, South Asian and Japanese relative to NHWs; in addition, obesity among Vietnamese, Chinese, Korean, South Asians and Japanese was comparable to NHWs.
Table 2.
Age, sex and nativity adjusted prevalence ratio (APR) for overweight or obese versus normal weight for each race/ethnicity compared to non-Hispanic Whites (NHW) from the 2009 California Health Interview Survey. For NHW, African Americans and Hispanic groups, normal weight (body mass index [BMI] = 18.5–24.9 kg/m2), overweight (BMI = 25–29.9 kg/m2) and obese (BMI ≥ 30 kg/m2) were defined by the standard BMI cut points. For each Asian subgroup, normal weight (BMI = 18.5–22.9 kg/m2), overweight (BMI = 23–27.49 kg/m2) and obese (BMI ≥ 27.5 kg/m2) were defined using cut points suggested by the World Health Organization.
| Race/ethnicity | Overweight APR (95% CI) | Obese APR (95% CI) |
|---|---|---|
| NHW | 1 (ref) | 1 (ref) |
| African American | 1.47 (1.15–1.88) | 1.79 (1.41–2.27) |
| Hispanic | 1.62 (1.39–1.88) | 2.64 (2.25–3.09) |
| Vietnamese | 0.49 (0.27–0.87) | 0.64 (0.31–1.32) |
| Chinese | 1.07 (0.71–1.61) | 0.71 (0.38–1.33) |
| Korean | 1.66 (0.97–2.85) | 0.67 (0.33–1.35) |
| Filipino | 2.94 (1.60–5.39) | 3.49 (1.92–6.34) |
| South Asian | 1.37 (0.89–2.10) | 1.23 (0.71–2.15) |
| Japanese | 1.28 (0.93–1.77) | 1.17 (0.72–1.91) |
Findings from the sensitivity analysis showed that tobacco status did not modify the racial/ethnic differences in the prevalence of overweight/obesity (p = 0.24).
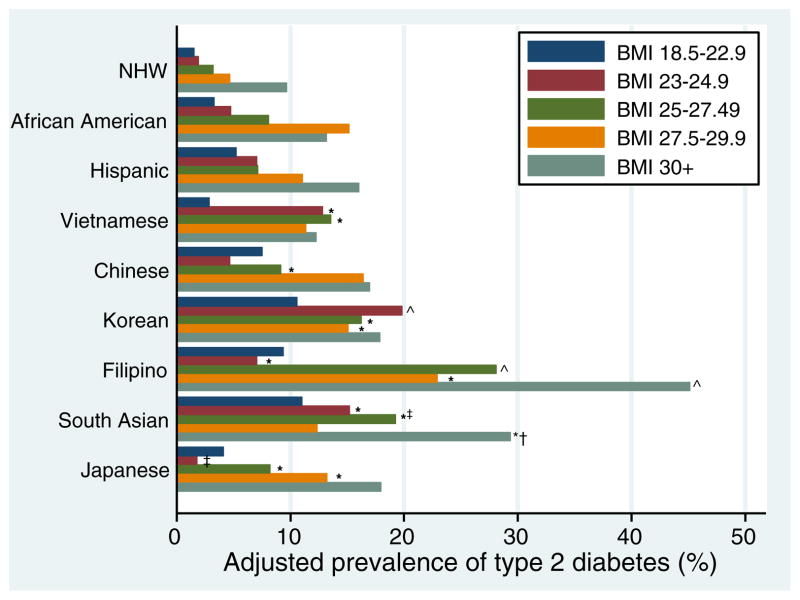
Fig. 2 shows the prevalence of self-reported type 2 diabetes within 5 BMI categories for NHW, African American, Hispanic and Asian subgroups. The adjusted prevalence of diabetes in the BMI 23–24.9 kg/m2 category was higher in Vietnamese (p < 0.001), Korean (p < 0.001), Filipino (p = 0.03) and South Asian (p = 0.003) groups compared to NHWs. Filipinos also had a higher adjusted prevalence of diabetes compared to NHWs in the stratum with BMI 25–27.49 kg/m2 (p < 0.001), 27.5–29.9 kg/m2 (p = 0.001) and ≥30 kg/m2 (p = 0.005). Diabetes prevalence was also elevated in the 27.5–29.9 kg/m2 stratum among Koreans (p = 0.03) and Japanese compared to NHWs (p = 0.003). The adjusted prevalence of hypertension and heart disease within 5 BMI categories for each population are included in the appendices (Figs. A1 and A2). The adjusted prevalence of hypertension in the BMI 23–24.9 kg/m2 category was higher in Filipinos (p = 0.005) compared to NHWs (Fig. A1).
Fig. 2.
Weighted age, sex and nativity adjusted prevalence of type 2 diabetes by body mass index (BMI, kg/m2) strata for each racial/ethnic group from the 2009 California Health Interview Survey. BMI strata incorporate cut points from the standard and World Health Organization (WHO) Asian BMI scale. The prevalence of diabetes in each BMI strata in Asian subgroups was compared to non-Hispanic Whites (NHW) in the same BMI strata. Statistically significant differences (p < 0.05) are indicated as follows: *versus NHW, †versus African American, ‡versus Hispanic and ^versus NHW, African American and Hispanic.
The WHO Asian BMI cut points for overweight/obesity compared to standard cut points had increased sensitivity but reduced specificity for type 2 diabetes, hypertension and heart disease except for BMI ≥ 27.5 kg/m2 for heart disease (Table A1). The AUROC for WHO Asian BMI cut points compared to standard BMI cut points was significantly higher in predicting prevalent hypertension but not for diabetes or heart disease (Table A1).
Discussion
Using a population-based representative sample of Asian Americans, we found that the adjusted prevalence of overweight/obesity in Filipinos using the WHO Asian BMI cut points is as high as or higher than traditionally high risk racial/ethnic populations. Over half of surveyed South Asians, Koreans, Japanese and Chinese met WHO Asian BMI criteria for overweight/obesity. Moreover, the prevalence of diabetes was higher among Vietnamese, Koreans, Filipinos and South Asians than NHWs in the BMI stratum 23–24.9 kg/m2, categorized by WHO as overweight for Asians but not for NHW, African Americans or Hispanics. The prevalence of diabetes was also higher among Koreans, Filipinos and Japanese in the BMI stratum 27.5–29.9 kg/m2, differentially categorized as obese by WHO and overweight by the standard BMI definition. This study suggests that Filipino, Vietnamese, Japanese, Korean and South Asian ethnicities are priority Asian populations for screening for overweight/obesity using the modified WHO Asian BMI criteria.
Consistent with prior work, Filipinos had the highest prevalence of overweight/obesity among all Asian American subgroups (Maxwell et al., 2012; Oza-Frank et al., 2009). Filipinos also have a high burden of type 2 diabetes and obesity-related cardiovascular disease (Karter et al., 2013; Lee et al., 2011; Palaniappan et al., 2011). Our study noted high rates of diabetes among Filipinos, which is consistent with past research identifying Filipinos as at higher risk of diabetes (Karter et al., 2013; Lee et al., 2011). The higher prevalence of self-reported diabetes was seen at BMI ≥ 23 kg/m2 among Filipinos, which suggests that WHO Asian BMI cut points may be important for screening for diabetes in this population. The use of the WHO Asian BMI cut points by health providers to screen Filipinos for overweight/obesity may be a valuable approach to identify at-risk patients and serve as an opportunity to counsel and intervene prior to the development of obesity-related diseases.
Overweight/obesity is also highly prevalent among South Asians, Koreans, Japanese and Chinese. With disparate rates of type 2 diabetes in these Asian American groups, particularly among South Asians (Gupta et al., 2011; Kanaya et al., 2010; Karter et al., 2013; Oza-Frank et al., 2009; Steinbrecher et al., 2012; Wander et al., 2013), these groups may benefit from targeted provider screening and counseling on weight management and lifestyle changes. In view of our finding of elevated diabetes prevalence in among Vietnamese, Korean and South Asians with BMI of 23–24.9 kg/m2, earlier screening for diabetes among those with BMI >23.0 kg/m2 in these subgroups may be useful clinically.
BMI is an imperfect proxy of adiposity and other anthropometric measures such as waist circumference, waist-to-hip ratio and waist-to-height ratio may provide additional precision to the estimation of obesity and risk for associated conditions (Dalton et al., 2003; Gelber et al., 2008; Lear et al., 2007). Radiographic assessments of ectopic fat depots (i.e., visceral fat, hepatic fat and intermuscular fat) are more closely associated to insulin resistance, systemic inflammation and incident metabolic disease than any anthropometric measures (Kanaya et al., 2006; Koster et al., 2010; Wander et al., 2013). Since these precise adiposity measures are impractical for large-scale epidemiologic or surveillance studies, BMI remains an acceptable and widely used screening tool for assessing overweight/obesity in clinical practice and in prioritizing populations at greatest risk (Moyer, 2012; World Health Organization, 2004). Federal prevention guidelines recommend that clinicians use BMI or waist circumference to identify patients’ obesity status (Moyer, 2012).
Moreover, the metabolically obese normal weight phenotype (Florez and Castillo-Florez, 2012; Lee, 2009) may be largely explained by smaller statured Asian populations with high metabolic risk. Studies examining the “obesity paradox,” in which being overweight or obese may confer mortality benefit relative to being normal weight in diabetes and cardiovascular disease (Carnethon et al., 2012; Gruberg et al., 2002), have not fully stratified by race/ethnicity with disaggregation of Asian American populations. High rates of diabetes seen in specific Asian American subgroups at lower BMI may suggest the need for an ethnic-specific definition of overweight/obesity.
While we examined overweight/obesity using recommended WHO Asian BMI cut points across all Asian groups, prior research has suggested that Asian ethnicity-specific BMI cut points for overweight/obesity may be warranted to best account for potential variations in lifestyle and dietary factors and the relationship of BMI with body fat for each Asian population (Low et al., 2009; Pan and Yeh, 2008; Razak et al., 2007; World Health Organization, 2004). Pooled analysis of prospective data from Asia suggests East versus South Asian differences in the association of BMI and mortality from any cause and cardiovascular disease (Chen et al., 2013; Zheng et al., 2011). Further research is needed to identify optimal BMI cutoffs for overweight/obesity in each Asian subgroup.
Study limitations and strengths
Our study has several limitations. Due to the cross-sectional design, the identified associations cannot be used to infer causation. In addition, our study relied on the analysis of self-reported height and weight used to calculate BMI. In general, survey respondents tend to under-report their weight and over-report their height, resulting in the underestimation of BMI (Connor Gorber et al., 2007; Elgar and Stewart, 2008; Merrill and Richardson, 2009). Self-reported height and weight bias has been associated with age and sex (Elgar and Stewart, 2008; Merrill and Richardson, 2009; Rowland, 1990), which were included in our multivariate modeling. There has been some evidence of differential bias in self-reported BMI by race/ethnicity among NHW, African American and Hispanic groups (Gillum and Sempos, 2005; Wen and Kowaleski-Jones, 2012), but the degree of BMI reporting bias among Asian ethnicities is not clear. In addition, self-reported diabetes is an imperfect measure and may be more prone to misclassification bias among lower socioeconomic groups, who may have poorer access or utilization of healthcare (Tang et al., 2003). However, the CHIS sample contained a large number of Asian Americans, allowing for analysis by subgroup.
Conclusions
The prevalence of overweight/obesity among Filipinos is the highest among all Asian American groups when using the WHO Asian BMI cut points, exceeds rates seen in NHWs and is comparable to African American and Hispanic populations. Filipinos should be considered as a high priority population for screening, counseling and treatment of overweight/obesity and related conditions. South Asian, Korean, Japanese and Chinese groups also had substantial rates of overweight/obesity and merit consideration as additional target populations for clinician screening and intervention. The WHO-recommended BMI cut point of 23 kg/m2 for Asians was associated with higher diabetes prevalence in some Asian groups including Vietnamese, Koreans, Filipinos and South Asians. The WHO Asian BMI cut points of 23 kg/m2 for overweight and 27.5 kg/m2 for obesity may better correspond to the public health impact of overweight/obesity among Asian Americans. Attention in clinical practice to lower BMI cut points among Asian Americans may be an important factor to identify and address metabolic and cardiovascular risks prior to progression to obesity-related conditions.
Supplementary Material
Acknowledgments
Jane Jih is supported by a Ruth L. Kirschstein National Research Service Award (T32HP19025).
Appendix A. Supplementary data
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.ypmed.2014.04.010.
Footnotes
Conflict of interest statement
The authors declare that there are no conflicts of interest.
References
- American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36 (Suppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Medical Association. AMA Adopts New Policies on Second Day of Voting at Annual Meeting. American Medical Association; 2013. [Accessed October 2, 2013]. Available from: < http://www.ama-assn.org/ama/pub/news/news/2013/2013-06-18-new-ama-policies-annual-meeting.page>. [Google Scholar]
- Bates LM, Acevedo-Garcia D, Alegria M, Krieger N. Immigration and generational trends in body mass index and obesity in the United States: results of the National Latino and Asian American Survey, 2002–2003. Am J Public Health. 2008;98:70–77. doi: 10.2105/AJPH.2006.102814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Health Interview Survey. CHIS 2009 Methodology Series: Report 4—Response Rates. UCLA Center for Health Policy Research; Los Angeles, CA: 2011. [Google Scholar]
- Carnethon MR, De Chavez PJD, Biggs ML, et al. Association of weight status with mortality in adults with incident diabetes. JAMA. 2012;308:581–590. doi: 10.1001/jama.2012.9282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan JN, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301:2129–2140. doi: 10.1001/jama.2009.726. [DOI] [PubMed] [Google Scholar]
- Chen Y, Copeland WK, Vedanthan R, et al. Association between body mass index and cardiovascular disease mortality in east Asians and south Asians: pooled analysis of prospective data from the Asia Cohort Consortium. BMJ. 2013:347. doi: 10.1136/bmj.f5446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu M, Austin PC, Manuel DG, Shah BR, Tu JV. Deriving ethnic-specific BMI cutoff points for assessing diabetes risk. Diabetes Care. 2011;34:1741–1748. doi: 10.2337/dc10-2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8:307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- Dalton M, Cameron AJ, Zimmet PZ, et al. Waist circumference, waist–hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. J Intern Med. 2003;254:555–563. doi: 10.1111/j.1365-2796.2003.01229.x. [DOI] [PubMed] [Google Scholar]
- Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3:141–146. doi: 10.1046/j.1467-789x.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- Elgar FJ, Stewart JM. Validity of self-report screening for overweight and obesity. Evidence from the Canadian Community. Health Survey Can J Public Health. 2008;99:423–427. doi: 10.1007/BF03405254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florez H, Castillo-Florez S. Beyond the obesity paradox in diabetes: fitness, fatness, and mortality. JAMA. 2012;308:619–620. doi: 10.1001/jama.2012.9776. [DOI] [PubMed] [Google Scholar]
- Gelber RP, Gaziano JM, Orav EJ, Manson JE, Buring JE, Kurth T. Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol. 2008;52:605–615. doi: 10.1016/j.jacc.2008.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillum RF, Sempos CT. Ethnic variation in validity of classification of overweight and obesity using self-reported weight and height in American women and men: the Third National Health and Nutrition Examination Survey. Nutr J. 2005;4:27. doi: 10.1186/1475-2891-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruberg L, Weissman NJ, Waksman R, et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 2002;39:578–584. doi: 10.1016/s0735-1097(01)01802-2. [DOI] [PubMed] [Google Scholar]
- Gupta LS, Wu CC, Young S, Perlman SE. Prevalence of diabetes in New York City, 2002–2008: comparing foreign-born South Asians and other Asians with U.S.-born whites, blacks, and Hispanics. Diabetes Care. 2011;34:1791–1793. doi: 10.2337/dc11-0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanaya AM, Wassel Fyr C, Vittinghoff E, et al. Adipocytokines and incident diabetes mellitus in older adults: the independent effect of plasminogen activator inhibitor 1. Arch Intern Med. 2006;3:350–360. doi: 10.1001/archinte.166.3.350. [DOI] [PubMed] [Google Scholar]
- Kanaya AM, Wassel CL, Mathur D, et al. Prevalence and correlates of diabetes in South Asian Indians in the United States: findings from the metabolic syndrome and atherosclerosis in South Asians living in America study and the multi-ethnic study of atherosclerosis. Metab Syndr Relat Disord. 2010;8:157–164. doi: 10.1089/met.2009.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karter AJ, Schillinger D, Adams AS, et al. Elevated rates of diabetes in Pacific Islanders and Asian subgroups: the Diabetes Study of Northern California (DISTANCE) Diabetes Care. 2013;36:574–579. doi: 10.2337/dc12-0722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King GL, McNeely MJ, Thorpe LE, et al. Understanding and addressing unique needs of diabetes in Asian Americans, Native Hawaiians, and Pacific Islanders. Diabetes Care. 2012;35:1181–1188. doi: 10.2337/dc12-0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koster A, Stenholm S, Alley DE, et al. Body fat distribution and inflammation among obese older adults with and without metabolic syndrome. Obesity (Silver Spring) 2010;18:2354–2361. doi: 10.1038/oby.2010.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Rathouz PJ. Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. Int J Obes Relat Metab Disord. 2000;24:1188–1194. doi: 10.1038/sj.ijo.0801365. [DOI] [PubMed] [Google Scholar]
- Lear SA, Humphries KH, Kohli S, Birmingham CL. The use of BMI and waist circumference as surrogates of body fat differs by ethnicity. Obesity (Silver Spring) 2007;15:2817–2824. doi: 10.1038/oby.2007.334. [DOI] [PubMed] [Google Scholar]
- Lee K. Metabolically obese but normal weight (MONW) and metabolically healthy but obese (MHO) phenotypes in Koreans: characteristics and health behaviors. Asia Pac J Clin Nutr. 2009;18:280–284. [PubMed] [Google Scholar]
- Lee JW, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997–2008. Diabetes Care. 2011;34:353–357. doi: 10.2337/dc10-0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low S, Chin MC, Ma S, Heng D, Deurenberg-Yap M. Rationale for redefining obesity in Asians. Ann Acad Med Singapore. 2009;38:66–69. [PubMed] [Google Scholar]
- Mackay DF, Gray L, Pell JP. Impact of smoking and smoking cessation on overweight and obesity: Scotland-wide, cross-sectional study on 40,036 participants. BMC Public Health. 2013;13:348. doi: 10.1186/1471-2458-13-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manson JE, Bassuk SS. Obesity in the United States: a fresh look at its high toll. JAMA. 2003;289:229–230. doi: 10.1001/jama.289.2.229. [DOI] [PubMed] [Google Scholar]
- Maxwell AE, Crespi CM, Alano RE, Sudan M, Bastani R. Health risk behaviors among five Asian American subgroups in California: identifying intervention priorities. J Immigr Minor Health. 2012;14:890–894. doi: 10.1007/s10903-011-9552-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely MJ, Boyko EJ. Type 2 diabetes prevalence in Asian Americans: results of a national health survey. Diabetes Care. 2004;27:66–69. doi: 10.2337/diacare.27.1.66. [DOI] [PubMed] [Google Scholar]
- Merrill RM, Richardson JS. Validity of self-reported height, weight, and body mass index: findings from the National Health and Nutrition Examination Survey, 2001–2006. Prev Chronic Dis. 2009;6:A121. [PMC free article] [PubMed] [Google Scholar]
- Moyer VA. Screening for and management of obesity in adults: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2012;157:373–378. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res. 1998;6 (Suppl 2):51S–209S. [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among adults: United States, 2011–2012. National Center for Health Statistics; Hyattsville, MD: 2013. [Google Scholar]
- Oza-Frank R, Ali MK, Vaccarino V, Narayan KM. Asian Americans: diabetes prevalence across U.S. and World Health Organization weight classifications. Diabetes Care. 2009;32:1644–1646. doi: 10.2337/dc09-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palaniappan LP, Wong EC, Shin JJ, Fortmann SP, Lauderdale DS. Asian Americans have greater prevalence of metabolic syndrome despite lower body mass index. Int J Obes (Lond) 2011;35:393–400. doi: 10.1038/ijo.2010.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan WH, Yeh WT. How to define obesity? Evidence-based multiple action points for public awareness, screening, and treatment: an extension of Asian-Pacific recommendations. Asia Pac J Clin Nutr. 2008;17:370–374. [PubMed] [Google Scholar]
- Pan WH, Flegal KM, Chang HY, Yeh WT, Yeh CJ, Lee WC. Body mass index and obesity-related metabolic disorders in Taiwanese and US whites and blacks: implications for definitions of overweight and obesity for Asians. Am J Clin Nutr. 2004;79:31–39. doi: 10.1093/ajcn/79.1.31. [DOI] [PubMed] [Google Scholar]
- Razak F, Anand SS, Shannon H, et al. Defining obesity cut points in a multiethnic population. Circulation. 2007;115:2111–2118. doi: 10.1161/CIRCULATIONAHA.106.635011. [DOI] [PubMed] [Google Scholar]
- Rowland ML. Self-reported weight and height. Am J Clin Nutr. 1990;52:1125–1133. doi: 10.1093/ajcn/52.6.1125. [DOI] [PubMed] [Google Scholar]
- Simmons D, Williams DR, Powell MJ. The Coventry Diabetes Study: prevalence of diabetes and impaired glucose tolerance in Europids and Asians. Q J Med. 1991;81:1021–1030. doi: 10.1093/qjmed/81.3.1021. [DOI] [PubMed] [Google Scholar]
- Steinbrecher A, Erber E, Grandinetti A, Nigg C, Kolonel LN, Maskarinec G. Physical activity and risk of type 2 diabetes among Native Hawaiians, Japanese Americans, and Caucasians: the Multiethnic Cohort. J Phys Act Health. 2012;9:634–641. doi: 10.1123/jpah.9.5.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens J. Ethnic-specific revisions of body mass index cutoffs to define overweight and obesity in Asians are not warranted. Int J Obes Relat Metab Disord. 2003;27:1297–1299. doi: 10.1038/sj.ijo.0802417. [DOI] [PubMed] [Google Scholar]
- Tang M, Chen Y, Krewski D. Gender-related differences in the association between socioeconomic status and self-reported diabetes. Int J Epidemiol. 2003;32:381–385. doi: 10.1093/ije/dyg075. [DOI] [PubMed] [Google Scholar]
- Wander PL, Boyko EJ, Leonetti DL, McNeely MJ, Kahn SE, Fujimoto WY. Change in visceral adiposity independently predicts a greater risk of developing type 2 diabetes over 10 years in Japanese Americans. Diabetes Care. 2013;36:289–293. doi: 10.2337/dc12-0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Wen M, Kowaleski-Jones L. Sex and ethnic differences in validity of self-reported adult height, weight and body mass index. Ethn Dis. 2012;22:72–78. [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Report of a WHO Expert Consultation: World Health Organization Technical Report, Series number 854. World Health Organization; Geneva: 1995. Physical status: the use and interpretation of anthropometry. [PubMed] [Google Scholar]
- World Health Organization. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- World Health Organization, International Association for the Study of Obesity, International Obesity Task Force. Health Communications Australia. 2000. The Asia-Pacific perspective: Redefining obesity and its treatment. [Google Scholar]
- Zheng W, McLerran DF, Rolland B, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364:719–729. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.