Abstract
Purpose
The conventional treatment for postlaparotomy wound dehiscence usually involves surgical revision. Recently, vacuum-assisted closure has been successfully used in postlaparotomy wound dehiscence. The aim of the present study was to compare the clinical outcome of 207 patients undergoing vacuum-assisted closure therapy or conventional treatment for postlaparotomy wound dehiscence.
Methods
Two hundred and seven consecutive patients underwent treatment for postlaparotomy wound dehiscence: vacuum-assisted closure therapy (January 2007 through August 2012, n = 25) or conventional treatment (January 2001 through August 2012, n = 182).
Results
The failure rate to first-line treatment with vacuum-assisted closure and conventional treatment were 0% and 14.3%, respectively (P = 0.002). There was no statistically significant difference in the enterocutaneous fistulas and hospital stay after vacuum-assisted closure therapy or conventional treatment respectively.
Conclusion
Our findings support that vacuum-assisted closure therapy is a safe and reliable option in postlaparotomy wound dehiscence with very low failure rate in surgical revision compared with conventional treatment.
Keywords: Vacuum-assisted closure, Dehiscence, Wound
INTRODUCTION
Postlaparotomy wound dehiscence occurs in 0.25% to 3% of patients [1,2], and multiple factors can contribute to its occurrence. The most common local factors associated with wound breakdown are wound infection, hematoma, and seroma [3]. Regional factors include bowel edema and abdominal distention, which may be caused by intra-abdominal infections, hemorrhage, and trauma [2,4,5], while systemic factors commonly associated with abdominal wound dehiscence are ad vanced age, malnutrition [2,5], pulmonary disease, renal failure, obesity, diabetes mellitus, steroid use, administration of radiotherapy, and/or administration of chemotherapy [6,7]. Imperfect surgical technique and emergency laparotomies are associated with and increased risk of wound dehiscence as well [1,8].
Several wound-healing strategies have been established for the treatment of postlaparotomy wound dehiscence. Conventional forms of treatment usually include surgical revision with open dressings or closed irrigation, temporary cover including the "Bogota bag", saline-soaked gauze dressing or towel pack, zipper dressing, absorbable or permanent (polytetrafluoroethylene) mesh, and other synthetic materials such as silicone sheets sutured to the fascial edges [9,10]. Several studies have reported promising results with the use of vacuum-assisted closure (VAC) therapy in wound dehiscence. In these patients, the VAC therapy has been successful, either as a single-line therapy or as a procedure for providing optimal conditions for delayed wound closure. However, there are few studies about VAC therapy for postlaparotomy wound dehiscence compared with the conventional therapy.
The aim of the present study was to compare the clinical outcome of conventional therapy and VAC therapy for postlaparotomy wound dehiscence.
METHODS
From January 2001 and December 2012, 207 patients were treated for postlaparotomy wound dehiscence at Korea University Anam Hospital. To compare the clinical outcome of conventional therapy and VAC therapy, the medical records of the 207 patients were reviewed.
Conventional treatment consisted of nonadhesive saline-soaked gauze dressing providing adequate coverage of the wound, then sealed with occlusive dressings. Dressings were changed every day or every other day, and visible debris was removed with cotton-based tissue.
In cases of VAC therapy, first, foam-based sponges (pore size ranging from 400 to 600 Am) provided in sterile packaging were cut and placed inside the wound. Suction tubing was then placed on top of the sponge, and the area was sealed with adhesive, providing complete coverage of the site extending 3-5 cm beyond the wound over clean, dry, hairless skin. If a tight seal could not be achieved, stoma adhesive paste (Duoderm, Convatec, Princeton, NJ, USA) was applied as a sealant. The tubing was connected to a computerized vacuum pump, and subatmospheric pressure was applied. Initially the pressure was set to 50 mmHg and increased to a maximum 125 mmHg over the course of about 10 minutes, depending on patient toleration. The foam and dressing were changed under clean conditions every 3 days. The suction was turned off for 30 to 60 minutes prior to changing the VAC dressing.
Inclusion criteria for this study was postlaparotomy wound dehiscence including skin-only exposed or exposed bowel/omentum. However, cases of enterocutaneous fistula were excluded.
Statistical analysis was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). The Mann-Whitney U-test was used to examine statistical associations, and significance was set at P < 0.05.
RESULTS
There were 207 patients treated for postlaparotomy wound dehiscence at Korea University Anam Hospital. All these patients were adults. One hundred eighty-two patients (87.9%) were treated by conventional treatment between January 2001 and December 2012. In January 2007, some surgeons changed their standard therapy in cases of postlaparotomy wound dehiscence from conventional treatment to VAC therapy. Since then, VAC has been used as single-line treatment in 25 patients (12.1%) with postlaparotomy wound dehiscence.
Baseline demographic characteristics were similar in the two groups (Table 1). There was no difference in hospital stay between conventional therapy group and VAC therapy group (Table 2). But, failure rate to fascia close was 14.3% in the convention therapy and 0% in the VAC therapy (P = 0.002). Enterocutaneous fistula formation rate was 2.7% in the convention therapy and 0% in the VAC therapy. But, there was no statistical significant difference (P = 0.06).
Table 1.
Patient characteristics
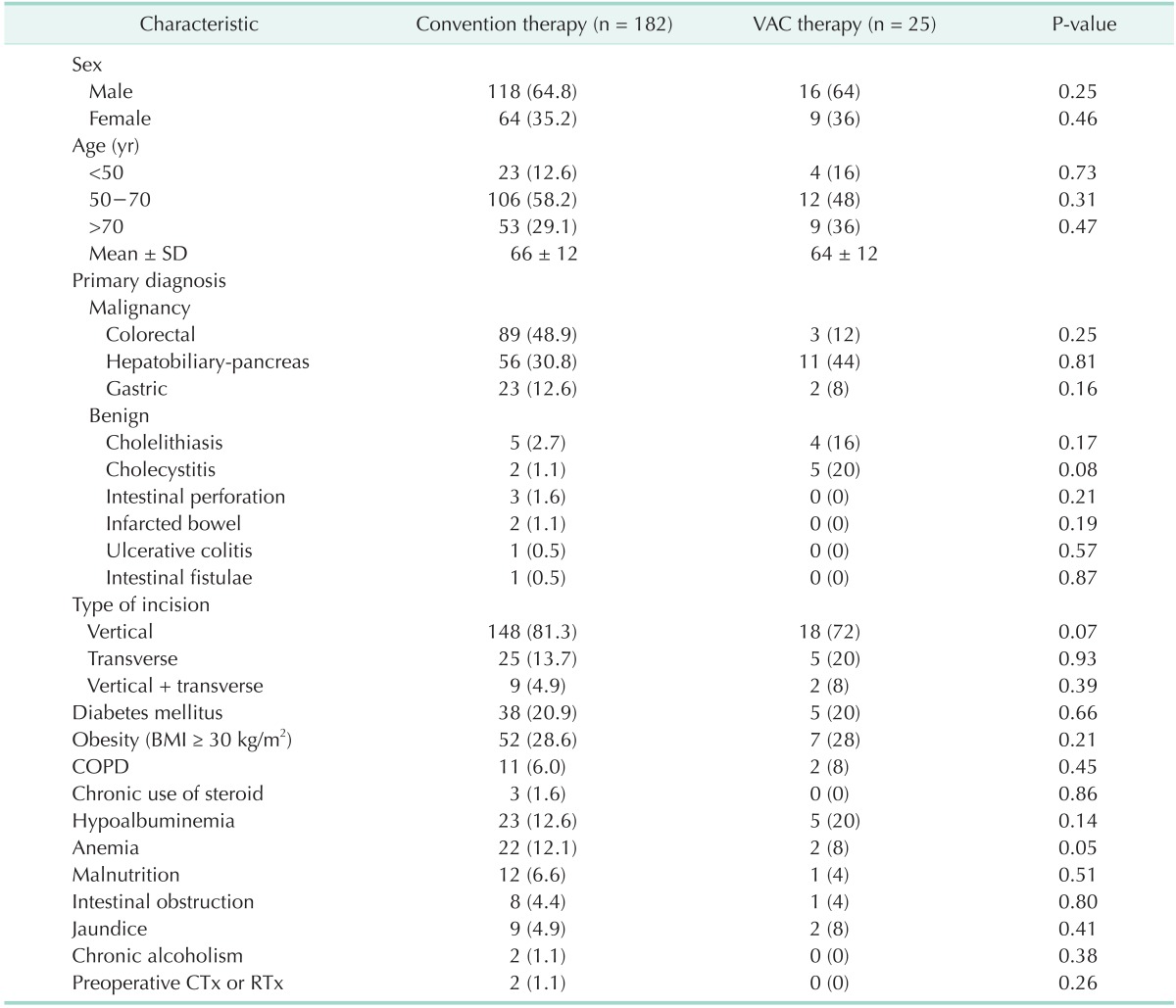
Values are presented as number (%) unless otherwise indicated.
VAC, vacuum-assisted closure; SD, standard deviation; BMI, body mass index; COPD, chronic obstructive pulmonary disease; CTx, chemotherapy; RTx, radiotherapy.
Table 2.
Comparison of conventional therapy and vacuumassisted closure therapy
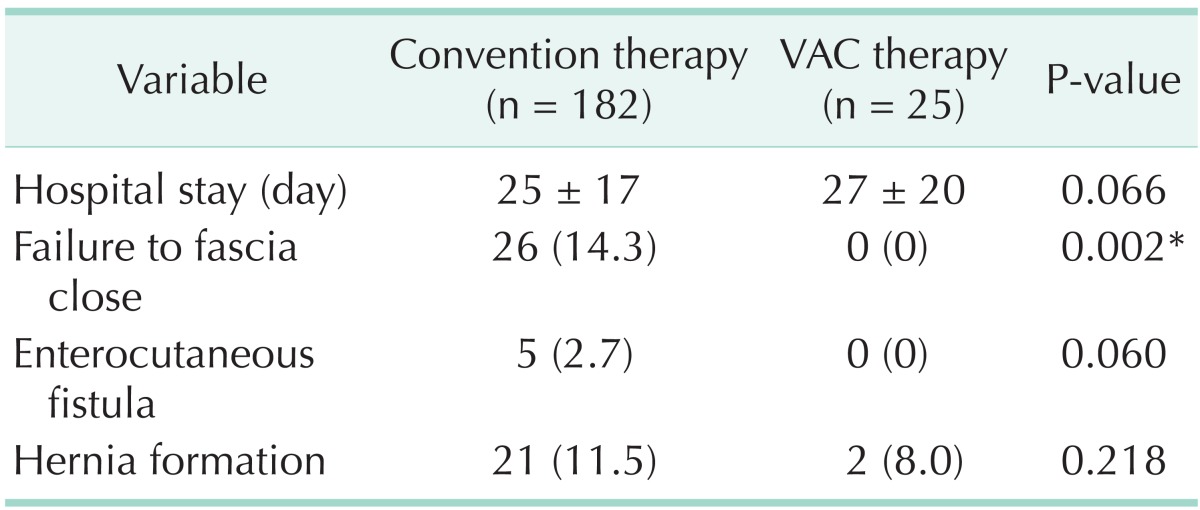
Values are presented as mean ± standard deviation or number (%)
*P < 0.05.
We had found risk factors affecting failure to fascia close with multivariate logistic regression analysis. In multivariate analysis, only conventional therapy was risk factors for failure to fascia close (odds ratio, 2.51; 95% confidence interval, 2.05-6.94; P = 0.04) (Table 3)
Table 3.
Multivariate logistic regression analysis for failure to fascia close
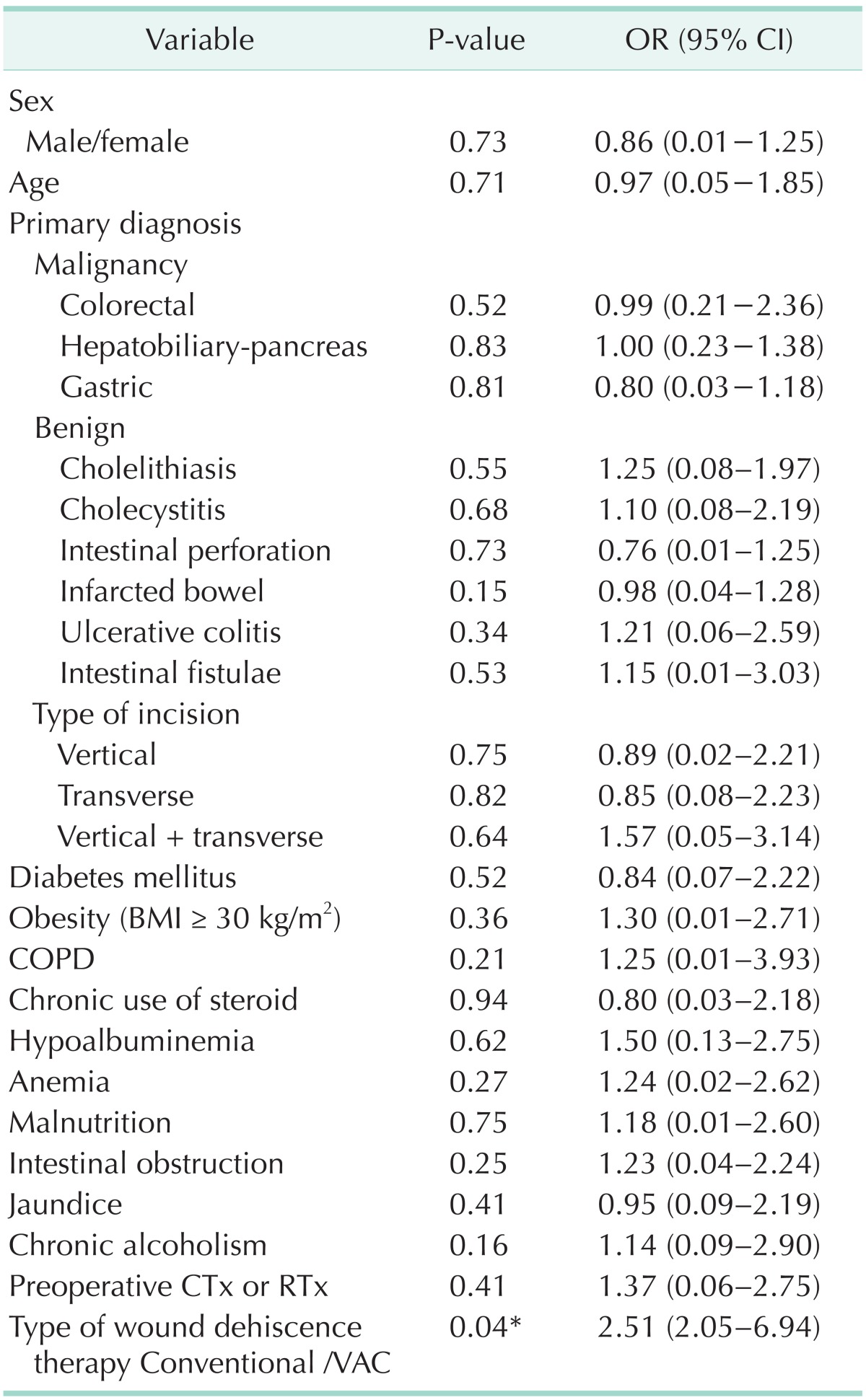
OR, odds ratio; CI, confidence interval; BMI, body mass index; COPD, chronic obstructive pulmonary disease; CTx, chemotherapy; RTx, radiotherapy; VAC, vacuum-assisted closure.
*P < 0.05.
DISCUSSION
Wound dehiscence is a surgical complication in which wounds widen along the surgical suture. Known risk factors for postlaparotomy wound dehiscence are advanced age, diabetes mellitus, malnutrition, obesity, poor knotting or grabbing of stitches, and trauma to the wound after surgery.
As for conventional treatment of wound dehiscence, there are moist dressings, "Bogota bag" applied, towel packs, zipper dressings, debridements, absorbable or permanent meshes, or other synthetic materials such as silicone sheets sutured to the fascial edges [9,10]. Moist wound dressings provide a barrier against bacteria and absorb fluid, allowing aid in reducing pain and reducing the frequency of dressing changes. But, the limitation of moist wound dressing is the wound becomes reversely dry, needs to be changed frequently, and fibers of the gauze may stick to the wound.
VAC is a novel approach in wound-healing management. During the application of this subatmospheric form of treatment, several advantageous features of conventional treatment are combined. VAC allows open drainage that continuously absorbs exudate. This therapy stimulates granulation tissue formation in combination with an increased blood flow in the adjacent tissue [11]. Furthermore, VAC therapy approximates the wound edges and provides a mass filling effect with a low degree of surgical trauma, without establishing a new wound (e.g., abdominal wound in omental flap).
VAC therapy was first used for experimental wounds in pigs in 1988 and the first human patient was treated in 1989. It is a temporary wound cover to improve the local environment of the wound and achieve healing by second intention without recourse to surgical closure techniques in most cases. VAC therapy helps convert an open wound into a controlled closed wound and enhances the body's natural capability to heal. Since then it has been used to treat a variety of wounds, including pressure sores, venous ulcers, dehisced and acute wounds, and diabetic ulcers, and also used to secure skin grafts and flaps, and to manage postoperative ascites and enterocutaneous fistula. VAC therapy facilitates early fascial closure with a decrease in the rate of large ventral hernia.
VAC therapy has been shown to increase local blood perfusion and nutrient delivery to the wound, accelerate the growth of granulation tissue, and decrease wound bacterial concentrations [11]. It can also reduce bowel edema and lower intra-abdominal pressure in abdominal compartment syndrome [12]. The application of mechanical stress to the wound accelerates cellular proliferation and angiogenesis, thus promoting the growth of granulation tissue [11]. It also uses the principle of reverse tissue expansion in the wound whereby shrinkage of the foam dressing exerts a centripetal effect on the wound edges bringing them closer together [13]. However, limitation of the VAC is a sudden increase in the output from the wound, which, while on VAC therapy, should raise the suspicion of an intestinal fistula whereby the therapy should be stopped. It is possible that erosion of underlying tissue by mechanical pressure from the suction tubing, and maceration of skin beneath the VAC may occur.
There are obvious limitations on the results of this study because of its retrospective and nonrandomized design. A randomized study might add further information, but the ideal design is not always feasible in a surgical setting because of practical and ethical reasons. Although there were some limitations in this study, it showed significant results of decreased failure rate to fascia close with VAC therapy compared with conventional method.
In conclusion, the present study demonstrates that properly applied VAC therapy is a safe and reliable option in postlapatomy wound dehiscence, with very low failure rate compared with conventional treatment.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Gislason H, Gronbech JE, Soreide O. Burst abdomen and incisional hernia after major gastrointestinal operations: comparison of three closure techniques. Eur J Surg. 1995;161:349–354. [PubMed] [Google Scholar]
- 2.Haddad V, Macon WL., 4th Abdominal wound dehiscence and evisceration: contributing factors and improved mortality. Am Surg. 1980;46:508–513. [PubMed] [Google Scholar]
- 3.Poole GV., Jr Mechanical factors in abdominal wound closure: the prevention of fascial dehiscence. Surgery. 1985;97:631–640. [PubMed] [Google Scholar]
- 4.Penninckx FM, Poelmans SV, Kerremans RP, Beckers JP. Abdominal wound dehiscence in gastroenterological surgery. Ann Surg. 1979;189:345–352. doi: 10.1097/00000658-197903000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riou JP, Cohen JR, Johnson H., Jr Factors influencing wound dehiscence. Am J Surg. 1992;163:324–330. doi: 10.1016/0002-9610(92)90014-i. [DOI] [PubMed] [Google Scholar]
- 6.Hesselink VJ, Luijendijk RW, de Wilt JH, Heide R, Jeekel J. An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet. 1993;176:228–234. [PubMed] [Google Scholar]
- 7.Poole GV, Jr, Meredith JW, Kon ND, Martin MB, Kawamoto EH, Myers RT. Suture technique and wound-bursting strength. Am Surg. 1984;50:569–572. [PubMed] [Google Scholar]
- 8.Greenburg AG, Saik RP, Peskin GW. Wound dehiscence. Pathophysiology and prevention. Arch Surg. 1979;114:143–146. doi: 10.1001/archsurg.1979.01370260033004. [DOI] [PubMed] [Google Scholar]
- 9.Fernandez L, Norwood S, Roettger R, Wilkins HE., 3rd Temporary intravenous bag silo closure in severe abdominal trauma. J Trauma. 1996;40:258–260. doi: 10.1097/00005373-199602000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Mizrahi S, Deutsch M, Hayes D, Meshkind S, Sorant B, Hussey J, et al. Improved zipper closure of the abdominal wall in patients requiring multiple intra-abdominal operations. Am J Surg. 1993;166:62–63. doi: 10.1016/s0002-9610(05)80585-9. [DOI] [PubMed] [Google Scholar]
- 11.Morykwas MJ, Argenta LC, Shelton-Brown EI, McGuirt W. Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. 1997;38:553–562. doi: 10.1097/00000637-199706000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Suliburk JW, Ware DN, Balogh Z, Mc-Kinley BA, Cocanour CS, Kozar RA, et al. Vacuum-assisted wound closure achieves early fascial closure of open abdomens after severe trauma. J Trauma. 2003;55:1155–1160. doi: 10.1097/01.TA.0000100218.03754.6A. [DOI] [PubMed] [Google Scholar]
- 13.Banwell PE, Teot L. Topical negative pressure (TNP): the evolution of a novel wound therapy. J Wound Care. 2003;12:22–28. doi: 10.12968/jowc.2003.12.1.26451. [DOI] [PubMed] [Google Scholar]


