Abstract
There were nearly 12 million admissions to U.S. jails in 2011, the majority of them Black or Hispanic. We analyzed data on men’s health screenings from the last Bureau of Justice Statistics Survey of Inmates in Local Jails. Black and Hispanic men had the same or higher odds of reporting nearly all types of screenings compared to White male inmates. Because many prisoners are medically underserved, jails can be crucial public health partners in reducing disparities by identifying men in need of health care. The anticipated expansion of Medicaid eligibility in 2014 constitutes an important opportunity for correctional and public health authorities to work together to ensure linkage to care following release from incarceration.
Keywords: jail, incarceration, screening, disparities, men’s health
Incarceration in the U.S. appears to have plateaued, but the U.S. still incarcerates a higher percentage of its population than any other nation (Rich, Wakeman, & Dickman, 2011). The vast majority of inmates in the U.S. are male, and about 2/3 are Black or Hispanic (Minton, 2012; West, Sabol, & Greenman, 2010). Evidence is mounting regarding incarceration’s adverse effects on life trajectories and family wellbeing (Freudenberg, 2001; London & Myers, 2006; D. Roberts, 2004; Wildeman & Western, 2010). At the same time, most inmates come from low-resource communities and lack employment, health insurance, and stable housing at higher rates than the general population. As a result, for some inmates incarceration provides their only access to non-emergency healthcare. Jails present a number of ethical dilemmas to providers and public health practitioners, but they are an underutilized public health opportunity to screen and test the medically underserved and to provide treatment for conditions that may have previously been undiagnosed. We present evidence on racial/ethnic patterns in screening inmates and discuss how jail-based medical screening provides one path to decreasing disparities in healthcare access among men in the community.
Background
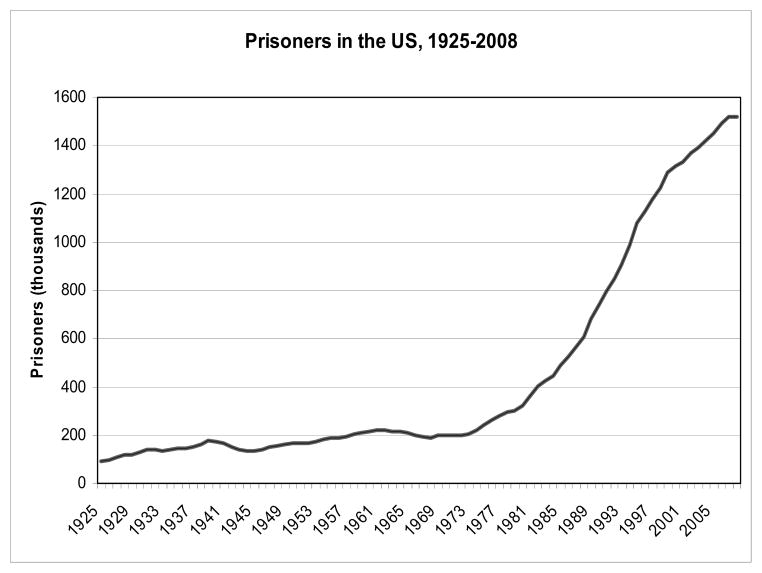
Incarceration rates in the U.S. escalated rapidly beginning in the 1970s and only stopped rising in the middle of the last decade (see Figure 1). During this time, the gap between White incarceration rates and Black/Hispanic incarceration rates also grew rapidly. In 1926, at the height of Jim Crow racial segregation, 21% of admissions to prisons were Black; by 1986, Blacks represented 44% and continued to rise (Langan, 1991). By comparison, Blacks represented less than 10% of the population in 1926 and fewer than 14% through the most recent censuses. The epidemic of incarceration resulted less from rampant criminality among Americans than a confluence of structural changes, such as the increased use of incarceration for minor offences, inadequate funding of community-based mental health services, and adoption of “tough on crime” political rhetoric. More recent studies suggest that well over 50% of inmates have a mental illness and/or addiction, reflecting insufficient community-based treatment for these conditions (Baillargeon, Binswanger, Penn, Williams, & Murray, 2009; Baillargeon, Hoge, & Penn, 2010; Lamb & Weinberger, 2005; Taxman, Byrne, & Pattavina, 2005). A substantial number of admissions, and a large percentage of the racial/ethnic disparities, stemmed directly from the war on drugs. Although Blacks, Whites, and Hispanics use drugs at about equal rates, Blacks are 13 times more likely to be imprisoned on drug charges than Whites (Moore & Elkavich, 2008; SAHMSA, 2010). Several legal scholars have identified features of the law enforcement, legal, and criminal justice systems (for example, stop-and-frisk practices in which police target young men of color) that account for these discrepancies (Alexander, 2010; Fellner, 2009; HRW, 2009; Provine, 2007).
Figure 1.
U.S. incarceration trends, 1925–2008. Source: Bureau of Justice Statistics.
Research studies and interventions involving inmates tend to focus on prisons, but about 17 times as many people pass through jail, an initial and more temporary placement. In 2011 there were about 11.8 million jail admissions—87.3% of them male—though many of these represented individuals who cycled through more than once in that year (Minton, 2012). Jail inmates tend to be younger and have less education than prison inmates, and like prison inmates, they carry a higher disease burden than the general population (Binswanger, Krueger, & Steiner, 2009). An estimated 17% of all Americans living with HIV pass through a correctional facility annually. This includes 22–28% of all Black men with HIV and 22–33% of all Hispanic men with HIV (Spaulding et al., 2009). Because injection drug use is a common route of transmission for both infections, co-infection with hepatitis C (HCV) is especially common; in one study, 65% of prisoners with HIV also had HCV (Solomon, Flynn, Muck, & Vertefeuille, 2004). Chronic diseases such as hypertension, asthma and diabetes have only recently become a substantial focus for researchers in correctional health, but chronic health problems now constitute a growing percentage of correctional healthcare needs due to a confluence of trends, especially the increase in chronic disease among younger Americans and the aging of the correctional population (Harzke et al., 2010; Williams, Stern, Mellow, Safer, & Greifinger, 2012).
Jails are the entry point to the entire incarceration experience, and as such they can capture many people without prior contact with the healthcare system. But from a healthcare perspective they are more problematic than prisons in a number of ways. Prisons house people who have been convicted and sentenced to over a year. Jails hold a combination of those awaiting charges, trial, or sentencing, and people sentenced to less than a year. This division is blurred in some places. In California in particular, as a result of the 2011 Supreme Court decision in Brown v Plata, many longer-term inmates are being shifted to jails in order to comply with the court’s orders to relieve overcrowding in the state prisons. Even so, jails experience constant turnover and although the mean length of stay is 38 days, the median is 2 days, with the 25th quartile released at 1 day (Spaulding et al., 2011). Thus any effort to screen the majority of inmates must capture them in the first 48 hours or so of arrival. However, the window may be even smaller if inmates arrive too intoxicated or otherwise unable to provide clear answers or consent (Spaulding, et al., 2011).
It is also difficult to describe the “typical” jail. There are almost 3300 jails in the U.S. (Stephan & Walsh, 2011). The largest jail (Los Angeles County) holds over 15,000, but about 40% of them have fewer than 50 beds. Jails with over 1000 beds are likely to have a full range of medical facilities and services, but the smaller ones are far more likely to rely on arrangements with local providers. In addition, all types of correctional facilities have turned increasingly from public employees to private contractors for some or all of their medical services, often contracting with more than one company. Because jails are under the jurisdiction of local rather than state or federal authorities, it is difficult to compile a national overview of jails’ medical services or even their regulatory oversight. The American Public Health Association and the National Commission on Correctional Health Care both provide standards and, in the case of the latter, accreditation for correctional health services, but these are voluntary. Despite all of these logistical difficulties, jails may provide a distinctive infrastructure in which disparities in access to health screening can be reduced. In this study, we examined men’s screenings and medical exams as reported in the 2002 Bureau of Justice Statistics national survey of jail inmates (the most recent available) for racial and ethnic patterns.
Methods
The Bureau of Justice Statistics and US Census Bureau conduct the Survey of Inmates in Local Jails (SILJ) every few years, and the last was conducted in 2002 (separate surveys are conducted among inmates in state prisons and federal prisons, most recently in 2004). The survey employs a stratified two-stage sample design selecting jails in the first stage and inmates in the second (BJS, 2002). In the first stage, 465 of the 3365 jails in the 1999 Census of Jails were selected, of which 9 had closed and 39 refused to participate, leaving 417 facilities in the sample. Inmates at those facilities were then randomly selected for interviews regarding their criminal, incarceration, personal, and health histories. Of the 605,997 unique individuals, 529,084 of whom were adult males, a total of 7750 names were drawn for the sample and 6982 interviews were completed. Two hundred sixty-three inmates refused to participate, 407 were released or transferred after sampling, and 98 could not be interviewed due to medical, security, or other reasons. The nonresponse rate for the second stage was 9.9% (BJS, 2002). Interviews were conducted using computer-assisted personal interviewing (CAPI).
The independent variable of interest was race/ethnicity as self-reported by inmates. Responses were categorized as non-Hispanic White, non-Hispanic Black, Hispanic, and “other.” The latter were included in analyses (except where stratified by race/ethnicity) but are not reported separately. Analyses were run separately for several dependent variables. Inmates were asked about three types of screening upon admission to jail: whether correctional staff checked to see if the inmate was sick, injured, or intoxicated; whether staff asked about health or medical history; and whether staff asked about suicidal thoughts or prior suicide attempts. Additional questions included whether the inmate had received a medical exam since admission; whether they had received a blood test; and whether they had been tested for TB and HIV. All dependent variables were recoded to become binary, with responses of “Don’t know” and refusals removed from the analysis. “Don’t know” responses were then tested separately for racial/ethnic patterns. We ran logistic regressions separately for each outcome variable, controlling for age (categorized as 16–34; 35–49; and 50 or more years), and education level (no high school; some high school; high school degree or GED; and any post-secondary), and the length of time the respondent had been incarcerated in the current incarceration episode. Income was tested but not included in the final model due to the high number of missing responses. Analyses were conducted in STATA version 11, using survey commands to account for the complex sampling.
Results
Nearly 44% of the male inmates surveyed lacked a high school degree (Table 1). Compared to White male inmates, Black and Hispanic men were more likely to be younger than 35 years old (56.7% compared to 63.6% and 71.6%, respectively; Table 1) and less likely to have a high school diploma. Black and Hispanic men were also in jail longer at the time of interview: 22.3% of Black men, 19.9% of Hispanic men, and 14.3% of White men had been in jail over 180 days.
Table 1.
Demographics of Male Jail Inmates by Race/Ethnicity, 2002 (n/weighted %)
| Non-Hispanic Black men N = 2,044 (40.5%a) | Hispanic men 978 (19.1%) | Non-Hispanic White men 1,684 (35%) | p | |
|---|---|---|---|---|
| Age | < .0001 | |||
| 35 years and younger | 1355 (63.6%) | 719 (71.6%) | 989 (56.7%) | |
| 35–49 years | 601 (31.8%) | 220 (24.3%) | 592 (36.6%) | |
| 50 years and older | 88 (4.6%) | 39 (4.1%) | 103 (6.7%) | |
| Education | < .0001 | |||
| Under 9th grade | 225 (9.3%) | 270 (27.3%) | 159 (8.9%) | |
| Some high school | 818 (38.0%) | 315 (31.2%) | 446 (25.8%) | |
| High school or GED | 769 (41.1%) | 309 (33.5%) | 830 (50.7%) | |
| Some college or degree | 216 (11.7%) | 71 (8.0%) | 234 (14.7%) | |
| Duration of current incarceration at time of interview | < .0001 | |||
| < 7 days | 231 (11.6%) | 116 (11.8%) | 246 (14.9%) | |
| 1–2 weeks | 155 (7.7%) | 81 (8.3%) | 158 (10.0%) | |
| 2–4 weeks | 273 (14.1%) | 133 (14.2%) | 261 (15.8%) | |
| 1–2 months | 328 (16.1%) | 152 (15.7%) | 270 (16.1%) | |
| 2–6 months | 575 (28.2%) | 294 (30.0%) | 484 (28.8%) | |
| > 6 months | 422 (22.3%) | 183 (19.9%) | 241 (14.3%) |
Men other than Blacks, Whites, and Hispanics were excluded from analysis due to low numbers.
Among male jail inmates, 81% reported being asked about their medical history and 79.3% were asked about prior suicidal thoughts/attempts at admission; rates did not vary by race/ethnicity (Table 2). Following admission, Black men were more likely to have a medical exam (45.7%, compared to 41.2% of White men and 40.3% of Hispanic men; p = .018). Both Black men (41%) and Hispanic men (36.6%) were more likely to report getting a blood test than White men (25.8%; p < .0001).
Table 2.
Prevalence of Screening Among Male Jail Inmates (Weighted Percentage)
| Black | White | Hispanic | p-values | |
|---|---|---|---|---|
| At intake | ||||
| Medical history taken | 79.7% | 81.4% | 83.5% | p = .107 |
| Checked for suicidal thoughts/attempts | 78.3% | 80.9% | 78.4% | p = .283 |
| Checked for injury, illness, or intoxication | 47.3% | 46.2% | 53.1% | p = .007 |
| Post-admission | ||||
| Received a medical exam | 45.7% | 41.2% | 40.3% | p = .018 |
| Received a blood test | 41.0% | 25.8% | 36.6% | p < .001 |
| Tested for TB | 67.3% | 56.9% | 63.8% | p < .001 |
| Tested for HIVa | 76.3%% | 70.5% | 69.4% | p = .065 |
Of those who reported receiving a blood test.
For almost all types of screening we examined, Black, White, and Hispanic men had similar odds after controlling for age, education, and length of time in jail (Table 3). Compared to Whites, both Blacks and Hispanics had higher odds of receiving a blood test (AORs 1.92 and 1.65 respectively) and being tested for TB (AORs 1.48 and 1.31 respectively; p ≤ .005 for both outcomes). Hispanics also had higher odds than Whites of being screened for illness, injury, or intoxication at admission (AOR 1.31; 95% CI 1.10–1.57). Differences were not statistically significant for any other outcome. To test whether results differed among younger versus older men, we ran separate models stratified by age group; results followed the same pattern (results not shown).
Table 3.
Odds Ratios of Men in Jail Adjusted for Time Since Admission, Age, and Education Level (White Males As Reference Group)a
| Black | Hispanic | |
|---|---|---|
| At intake | ||
| Medical history taken | .92 (.77–1.10) | 1.25 (.99–1.58) |
| Checked for suicidal thoughts/attempts | .88 (.73–1.05) | .94 (.75–1.17) |
| Checked for injury, illness, or intoxication | 1.04 (.91–1.2) | 1.31 (1.10–1.57) |
| Post-admission | ||
| Received a medical exam | 1.14 (.99–1.33) | 1.00 (.83–1.20) |
| Received a blood test | 1.92 (1.63–2.25) | 1.65 (1.36–2.00) |
| Tested for TB | 1.48 (1.27–1.73) | 1.31 (1.08–1.58) |
| Tested for HIVb | 1.29 (.95–1.76) | .90 (.62–1.32) |
Boldface indicates statistical significance.
Of those who reported receiving a blood test.
Inmates were only asked if they had been tested for HIV if they indicated they had received a blood test (in the ten years since the last jail survey, rapid HIV testing which may not require a blood sample has become more common). A follow-up question allows estimates of how many had ever received an HIV test, though it does not permit identification of how many of those were conducted during a previous incarceration. For all three races/ethnicities, a higher percentage of inmates said they had ever been tested for HIV than men in the general population (see Table 4). However, inmates who said they did not get a blood test since their latest admission were also less likely to report having ever been tested.
Table 4.
Percentage of Men Reporting Ever Being Tested for HIV
| General male population* | Among all jail inmates | Among jail inmates not reporting a blood test during the current incarceration episode | |
|---|---|---|---|
| Black men | 61.8 | 71.5 | 59.8 |
| Hispanic men | 47.6 | 54.8 | 47.6 |
| White men | 40.9 | 64.1 | 40.9 |
Discussion
Jails present a rare opportunity to provide medically underserved men with access to screening and treatment for conditions that may have been previously undiagnosed. All attempts to capitalize on this opportunity must start by recognizing that it is a counterproductive solution to the problem of insufficient access to community-based healthcare for low-income men. As a disruptive life event experienced disproportionately by young Black and Hispanic men, incarceration may well be contributing to health disparities in the U.S., especially by virtue of its adverse effects on employment, homelessness, marriage, and other primary social determinants of health (Binswanger, Redmond, Steiner, & Hicks, 2012; Iguchi, Bell, Ramchand, & Fain, 2005; London & Myers, 2006; Mallik-Kane & Visher, 2008; Massoglia, 2008a, 2008b; Pager, Western, & Sugie, 2009). There is also evidence that parental incarceration is contributing to disparities in childhood development (Wakefield & Wildeman, 2011; Western & Wildeman, 2009; Wildeman, 2009). Still, jails are one of few ways to access a population that is largely poor in the social and economic resources that permit regular contact with healthcare providers. Our results show that Black and Hispanic men in jail had equal or higher odds of being screened for medical conditions compared to White men. Although Black and Hispanic men were more likely to be in jail for longer periods of time than White men at the time of the interview, regressions controlling for incarceration duration show that the existence of a longer period when screening might occur does not explain these screening patterns.
All inmates are supposed to be screened at intake for immediate risk and need. Based on the Survey of Inmates, about 80% of male inmates reported being screened for suicide risk and having a medical history taken, but significantly fewer answered affirmatively to the question, “When you were admitted, did staff check you to see if you were sick, injured, or intoxicated?”. This may indicate either that staff evaluations gave lower priority to this question or that respondents did not realize they had been evaluated for injury, illness, or intoxication. It is notable, however, that Hispanics had higher adjusted odds of reporting this screening than Whites did, suggesting that language barriers were not a likely source of lack of communication on this point.
Because the same screens (e.g. being checked for injury, illness, or intoxication) are not common among the general population, it is difficult to compare jail screening rates to racial/ethnic patterns among men at large. However, a 2012 Institute of Medicine workshop noted the persistence of racial disparities identified in its 2002 report Unequal Treatment (Anderson, 2012), and the AHRQ indicates that 72.3% of non-Hispanic White males in the general population had an outpatient visit in the past year, compared to 56.1% of Black males and 54.8% of Hispanic males (AHRQ, 2012). Among jail inmates, Black and Hispanic men had the same or higher odds of receiving screens compared to White men. Odds differed most in TB and blood testing. TB remains one of the most basic and traditional concerns of correctional health, as the presence of large numbers of people in enclosed, poorly-ventilated spaces is highly conducive to its spread. One survey of large jails found that 85% had policies for universal TB screening, and over 70% of those had a policy to place a skin test within 24 hours (C.A. Roberts et al., 2006). In our study, only among inmates who had been in jail over 6 months did TB testing reach 75% (results not shown). Thus, even among long-term inmates, at least 25% remained untested. Blacks and Hispanics overall are at higher risk for TB in the U.S. (CDC, 2012) and it appears that in jails they are tested for TB at higher rates than White men. It is unclear whether this results from jails’ perceptions of relative risk or from some other factor.
There is a substantial literature on HIV detection and treatment in correctional facilities and their implications for the community HIV burden. HIV is also the subject of interventions and clinical studies on linkage to community-based health care following release from incarceration (Baillargeon et al., 2009; Binswanger & Wortzel, 2009; Nunn et al., 2010; Springer, Spaulding, Meyer, & Altice, 2011). As such, HIV can serve as a bellwether and template for capitalizing on even brief periods of incarceration as an opportunity to diagnose and treat the medically underserved for other conditions as well.
A number of studies attest to the important role correctional facilities have played in detecting community-wide rates of HIV and STIs. In the 1990s, for instance, a third of all HIV cases in Rhode Island were identified in correctional facilities (Beckwith, Zaller, Fu, Montague, & Rich, 2010; Desai, Latta, Spaulding, Rich, & Flanigan, 2002). Estimates of the prevalence of HIV among inmates, and the proportion of community- and state-wide cases reported by correctional facilities, vary substantially across facilities and states depending on testing policies and practices. Facilities that test primarily upon inmate request may under-diagnose HIV, since those who are most at risk are less likely to request testing. Facilities with opt-out testing (i.e. testing is automatic unless the inmate refuses, but is not mandatory in order to protect patients’ rights) are most likely to capture previously-undiagnosed cases before return to the community. When the Washington state prison system changed its policy from testing on inmate request to opt-out testing, the percent of male inmates tested rose from 5% to 90%. Our analysis was not able to control for the type of HIV testing policy implemented at the facilities. There appears to have been some reduction in the number of facilities with universal HIV testing between 2000 and 2004 (Sykes & Piquero, 2009), but to our knowledge there is no current review of policies across facilities. It bears noting that a review of STD testing policies found that even jails with a universal testing policy tested fewer than 50% of inmates; other facility features, such as size and public vs. private providers, also predicted testing prevalence (Parece, Herrera, Voigt, Middlekauff, & Irwin, 1999).
There are at least three critical questions the data do not address. First, it is difficult to know why some inmates were tested but not others. Since our analysis controlled for how long the inmate had been incarcerated, it does not appear to be the case that some had not been in long enough to be tested prior to the interview. One possible explanation is that inmates who were unable to answer questions upon arrival (e.g. because under the influence of drugs or alcohol) were not captured later. Because all data are self-reported, there is also the possibility of recall or response bias. With the present data, we are unable to identify whether racial/ethnic patterns in post-admission medical exams result primarily from inmate request or facility capacity or decisions.
Second, the national averages may hide significant within-facility differences in screening patterns, in addition to the expected between-facility variation. Recent studies on racial disparities in the Veterans Administration found that disparities do occur within facilities and cannot be attributed solely to differences between facilities (Trivedi, Grebla, Wright, & Washington, 2011). A study of the North Carolina prison system found substantial variation among facilities in the same state system: although the state-wide prison HIV testing rate was 34% prior to the implementation of opt-out testing, individual prisons ranged from 1% to 84% (Rosen et al., 2009). Jails under local jurisdiction presumably differ even more widely in their screening policies and practices. We were not able to analyze within-facility versus between-facility patterns with the publicly available jail data.
Finally, it is critical to underscore that the data do not allow us to evaluate whether disparities exist in the amount and appropriateness of care provided subsequent to these screenings, although Rosen et al. found that Black prison inmates were slightly more likely to utilize healthcare services for specific conditions than Whites were (Rosen, Hammond, Wohl, & Golin, 2012). Further information is also needed on the systems, protocols, and decisions determining screening. Post-intake screenings presumably rely more on inmate initiative (i.e. whether they requested a medical exam). However, no data are available on sick call procedures in jails overall. Anecdotal evidence indicates that when inmates submit sick call slips to request access to a healthcare provider, they often encounter substantial wait periods before the request is filled. In the worst of cases, as testimony in the 2011 Brown v Plata Supreme Court decision revealed, overcrowding has contributed to widespread systemic failures in basic medical services. In addition, many correctional facilities have implemented copays which, though low, have been shown to deter inmates from seeking medical appointments (Awofeso, 2005; Fisher & Hatton, 2010).
Practical Solutions to Addressing Health Disparities in Men
Since nearly all prisoners eventually return to the community, prisoner health is inseparable from community health. Much of the community health impact occurs through economic pathways (e.g. the cumulative impact of the removal of income-earners on family wellbeing) but there is growing evidence of more direct associations between correctional health and community health. Several studies have documented STI/HIV transmission associated with incarceration’s disruption of sex ratios and relationships (Johnson & Raphael, 2009; Khan et al., 2011; Khan et al., 2008; Rogers et al., 2012; Thomas, Levandowski, Isler, Torrone, & Wilson, 2008). Jail screening policies, especially the introduction or elimination of universal STI screening, have also been linked to STI rates in the community (Broad et al., 2009; Pathela et al., 2009).
These and other links between correctional and community health suggest that the criminal justice system is an important partner in combatting health disparities in the U.S., but it is also a problematic one. Healthcare providers and public health practitioners should always be cognizant of the adverse health consequences endemic in incarceration and the potential ethical dilemmas of working with correctional systems (Allen, Wakeman, Cohen, & Rich, 2010; Metzner & Fellner, 2010). Even so, we suggest three points at which healthcare providers and public health practitioners can work towards the reduction of health disparities among men by engaging with the correctional population.
First, health professionals should use their considerable authority to advocate for alternatives to incarceration where appropriate. This is especially the case for the high percentage of inmates whose untreated mental illness and/or substance dependence led them to the attention of the criminal justice system. Especially by working through professional associations (e.g. the American Medical Association, American Nurses Association, or American Public Health Association) the health fields have in the past proved highly effective advocates, and their support for diversion programs that redirect people from jail to treatment could carry a great deal of weight with policymakers. Health professionals must also be willing to accept formerly incarcerated adults as clients. The expansion of healthcare coverage under the Affordable Care Act (ACA) will have substantial implications for the correctional population, both by expanding Medicaid eligibility and by ensuring broad coverage for behavioral health. There is less certainty that community providers will accept large numbers of new patients who are seen as high-need or high-risk, especially in settings like community health clinics that are already strained. Shifting away from the criminalization of addiction and mental illness, though, is a crucial step towards addressing these conditions that disproportionately affect poor men.
That said, the current reality is that jails are likely to remain the healthcare providers of last resort for large numbers of low-income men, and they may be a unique locus for identifying health needs among this population. Despite the great potential of the ACA, it is unlikely that in the foreseeable future community providers will be able to access and screen the numbers of medically underserved men who pass through jails. The racial/ethnic parity in screening men in jail also offers a rare opportunity to redress community-level disparities among men. Only about 4% of jail inmates continue on to prison, where nearly everyone undergoes some type of screening, so a large number of people leave jail and return to the community without ever being screened for potential health problems. It is thus crucial to increase overall screening rates during short-term stays. Our second recommendation is that community providers and public health practitioners reduce existing barriers to screening all inmates by actively collaborating with correctional health providers as colleagues and partners, rather than a distinct and removed workforce. In practical terms, this might include the following:
improve communication and active partnership between jails and Departments of Health
increase external oversight of jail health services, e.g. via standardized reporting and on-site visits whenever possible, to identify the specific reasons that not all inmates are screened
advocate for adequate funding for jail medical facilities and staff
employ professional associations to increase communication between correctional and community health professionals
Third, health professionals can play a major role in increasing linkage to community-based treatment upon release from jail, potentially interrupting the cycle of recidivism and reincarceration at the same time. The fact that jails are local institutions and thus more open to local influence than state and federal prisons is especially important here, though recommendations for nationwide action on incarceration and health have been made elsewhere (Gibbons & Katzenbach, 2006). Prisoners returning to the community frequently struggle to reestablish housing, employment, and relationships. In this context, attention to health needs often falls by the wayside and high-risk behaviors such as unsafe sex and relapse to drug use are common. Still, numerous initiatives have shown that it is possible to improve the odds that releasees will link to community-based treatment (Wang et al., 2010; Wang et al., 2012). Even if jails cannot provide treatment themselves (e.g. when inmates are released after only a few days), jail-based screenings can identify which inmates require discharge planning and community-based intervention. Discharge planning broadly refers to the process of helping prisoners to prepare to make the transition from incarceration back into the community. With rising demand and declining resources, even prisons are able to provide discharge planning to only a fraction of releasees (Mellow & Greifinger, 2005) and jails provide even less. Community providers and public health departments, though, could work with jails to ensure that more inmates with health problems identified by jail-based screening are provided with referrals and other local resources necessary to increase access to follow-up care.
This is an unusually propitious moment for public health-correctional partnerships. With the Supreme Court’s reaffirmation of the legality of the Affordable Care Act, most states are planning for the expansion of Medicaid eligibility. Starting in 2014, male releasees who were previously ineligible will be able to receive Medicaid, thereby removing a significant financial barrier to accessing care in the community (although it is unclear at this time how many states are working on plans for enrollment outreach specifically to this population). Other barriers to community-based care will continue, but now more than ever it may be possible to link low-resource men, particularly Blacks and Hispanics, to community-based treatment. Given the continuing epidemic of incarceration in the U.S., jails are likely to continue to provide access to the medically underserved for years to come. And while some correctional facilities have required continuous litigation and public scandal to improve the care they provide, health authorities and practitioners will find that many correctional individuals and facilities are deeply committed to any potential social good they can provide in the course of their duties.
Acknowledgments
This work was supported by NIDA K24DA022112 (Dr. Rich) and CFAR P30AI042853. Dr. Redmond was supported by a Minority Investigator Research Supplement to NHLBI grant (R01 HL080477-07S1) and a Center for Medicaid and Medicare Innovation Health care innovation (CFDA 93.610) award (sub recipient).
References
- AHRQ. National Healthcare Disparities Report 2011. Washington, DC: U.S. Department of Health & Human Services; 2012. [Google Scholar]
- Alexander M. The new Jim Crow: Mass incarceration in the age of colorblindness. New York, NY: The New Press; 2010. [Google Scholar]
- Allen S, Wakeman S, Cohen L, Rich J. Physicians in US prisons in the era of mass incarceration. International Journal of Prison Health. 2010;6(3):100–106. [PMC free article] [PubMed] [Google Scholar]
- Anderson KA. Progress since 2000. Washington, DC: National Academies of Sciences; 2012. How far have we come in reducing health disparities? [PubMed] [Google Scholar]
- Awofeso N. Making prison health care more efficient. BMJ. 2005;331(7511):248–249. doi: 10.1136/bmj.331.7511.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baillargeon J, Binswanger IA, Penn JV, Williams BA, Murray OJ. Psychiatric disorders and repeat incarcerations: The revolving prison door. American Journal of Psychiatry. 2009;166(1):103–109. doi: 10.1176/appi.ajp.2008.08030416. [DOI] [PubMed] [Google Scholar]
- Baillargeon J, Giordano TP, Rich JD, Wu ZH, Wells K, Pollock BH, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301(8):848–857. doi: 10.1001/jama.2009.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baillargeon J, Hoge SK, Penn JV. Addressing the challenge of community reentry among released inmates with serious mental illness. American Journal of Community Psychology. 2010;46(3–4):361–375. doi: 10.1007/s10464-010-9345-6. [DOI] [PubMed] [Google Scholar]
- Beckwith CG, Zaller ND, Fu JJ, Montague BT, Rich JD. Opportunities to diagnose, treat, and prevent HIV in the criminal justice system. Journal of Acquired Immune Deficiency Syndrome. 2010;55(Suppl 1):S49–55. doi: 10.1097/QAI.0b013e3181f9c0f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger IA, Krueger PM, Steiner JF. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. Journal of Epidemiology and Community Health. 2009;63(11):912–919. doi: 10.1136/jech.2009.090662. [DOI] [PubMed] [Google Scholar]
- Binswanger IA, Redmond N, Steiner JF, Hicks LS. Health disparities and the criminal justice system: An agenda for further research and action. Journal of Urban Health. 2012;89(1):98–107. doi: 10.1007/s11524-011-9614-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger IA, Wortzel HS. Treatment for individuals with HIV/AIDS following release from prison. JAMA. 2009;302(2):147. doi: 10.1001/jama.2009.919. author reply 148. [DOI] [PubMed] [Google Scholar]
- BJS. Survey of inmates in local jails, 2002 Codebook. Ann Arbor, MI: Interuniversity Consortium for Political and Social Research; 2002. [Google Scholar]
- Broad J, Cox T, Rodriguez S, Mansour M, Mennella C, Murphy-Swallow D, et al. The impact of discontinuation of male STD screening services at a large urban county jail: Chicago, 2002–2004. Sexually Transmitted Diseases. 2009;36(2 Suppl):S49–S52. doi: 10.1097/OLQ.0b013e318156159a. [DOI] [PubMed] [Google Scholar]
- CDC. Reported tuberculosis in the United States, 2011. Atlanta (GA): U.S. Department of Health and Human Services; 2012. [Google Scholar]
- Desai AA, Latta ET, Spaulding A, Rich JD, Flanigan TP. The importance of routine HIV testing in the incarcerated population: The Rhode Island experience. AIDS Education & Prevention. 2002;14(5 Suppl B):45–52. doi: 10.1521/aeap.14.7.45.23867. [DOI] [PubMed] [Google Scholar]
- Fellner J. Race, drugs, and law enforcement in the United States. Stanford Law Review. 2009;20(2):257–291. [Google Scholar]
- Fisher AA, Hatton DC. A study of women prisoners’ use of co-payments for health care: Issues of access. Women’s Health Issues. 2010;20(3):185–192. doi: 10.1016/j.whi.2010.01.005. [DOI] [PubMed] [Google Scholar]
- Freudenberg N. Jails, prisons, and the health of urban populations: A review of the impact of the correctional system on community health. Journal of Urban Health. 2001;78(2):214–235. doi: 10.1093/jurban/78.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons J, Katzenbach N. Confronting confinement: A report of The Commission on Safety and Abuse in America’s Prisons. Washington University Journal of Law and Policy. 2006;22:385–560. [Google Scholar]
- Harzke AJ, Baillargeon JG, Pruitt SL, Pulvino JS, Paar DP, Kelley MF. Prevalence of chronic medical conditions among inmates in the Texas prison system. Journal of Urban Health. 2010;87(3):486–503. doi: 10.1007/s11524-010-9448-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HRW. Decades of disparity: Drug arrests and race in the United States. New York, NY: Human Rights Watch; 2009. [Google Scholar]
- Iguchi MY, Bell J, Ramchand RN, Fain T. How criminal system racial disparities may translate into health disparities. Journal of Health Care for the Poor and Underserved. 2005;16(4 Suppl B):48–56. doi: 10.1353/hpu.2005.0114. [DOI] [PubMed] [Google Scholar]
- Johnson R, Raphael S. The effects of male incarceration dynamics on Acquired Immune Deficiency Syndrome Infection rates among African American women and men. Journal of Law and Economics. 2009;52:251–293. [Google Scholar]
- Khan MR, Epperson MW, Mateu-Gelabert P, Bolyard M, Sandoval M, Friedman SR. Incarceration, sex with an STI- or HIV-infected partner, and infection with an STI or HIV in Bushwick, Brooklyn, NY: A social network perspective. American Journal of Public Health. 2011;101(6):1110–1117. doi: 10.2105/AJPH.2009.184721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan MR, Miller WC, Schoenbach VJ, Weir SS, Kaufman JS, Wohl DA, et al. Timing and duration of incarceration and high-risk sexual partnerships among African Americans in North Carolina. Annals of Epidemiology. 2008;18(5):403–410. doi: 10.1016/j.annepidem.2007.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb HR, Weinberger LE. The shift of psychiatric inpatient care from hospitals to jails and prisons. Journal of the American Academy of Psychiatry and Law. 2005;33(4):529–534. [PubMed] [Google Scholar]
- Langan P. Race of prisoners admitted to state and federal institutions, 1926–86. 1991 Retrieved from https://www.ncjrs.gov/pdffiles1/nij/125618.pdf.
- London A, Myers N. Race, incarceration, and health: A life-course approach. Research on Aging. 2006;28(3):409–422. [Google Scholar]
- Mallik-Kane K, Visher C. Health and prisoner reentry: How physical, mental, and substance abuse conditions shape the process of reintegration. Washington, DC: Urban Institute; 2008. [Google Scholar]
- Massoglia M. Incarceration as exposure: The prison, infectious disease, and other stress-related illnesses. Journal of Health and Social Behavior. 2008a;49(1):56–71. doi: 10.1177/002214650804900105. [DOI] [PubMed] [Google Scholar]
- Massoglia M. Incarceration, health, and racial disparities in health. Law & Society Review. 2008b;42(2):275–305. [Google Scholar]
- Mellow J, Greifinger R. Sucessful reentry: The perspective of private correctional health care providers. Journal of Urban Health. 2005;84(1):85–98. doi: 10.1007/s11524-006-9131-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzner JL, Fellner J. Solitary confinement and mental illness in U.S. prisons: A challenge for medical ethics. Journal of the American Academy of Psychiatry and Law. 2010;38(1):104–108. [PubMed] [Google Scholar]
- Minton T. Jail inmates at midyear 2011 - Statistical tables. Washington, DC: Bureau of Justice Statistics; 2012. [Google Scholar]
- MMWR. Vital signs: HIV testing and diagnosis among adults—United States, 2001–2009. Morbidity and Mortality Weekly Report (MMWR) 2010;59(47):1550–1555. [PubMed] [Google Scholar]
- Moore LD, Elkavich A. Who’s using and who’s doing time: Incarceration, the war on drugs, and public health. American Journal of Public Health. 2008;98(5):782–786. doi: 10.2105/AJPH.2007.126284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunn A, Cornwall A, Fu J, Bazerman L, Loewenthal H, Beckwith C. Linking HIV-positive jail inmates to treatment, care, and social services after release: results from a qualitative assessment of the COMPASS Program. Journal of Urban Health. 2010;87(6):954–968. doi: 10.1007/s11524-010-9496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pager D, Western B, Sugie N. Sequencing disadvantage: Barriers to employment facing young black and white men with criminal records. Annals of the American Academy of Political and Social Science. 2009;623:195–210. doi: 10.1177/0002716208330793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parece MS, Herrera GA, Voigt RF, Middlekauff SL, Irwin KL. STD testing policies and practices in U.S. city and county jails. Sexually Transmitted Diseases. 1999;26(8):431–437. doi: 10.1097/00007435-199909000-00003. [DOI] [PubMed] [Google Scholar]
- Pathela P, Hennessy RR, Blank S, Parvez F, Franklin W, Schillinger JA. The contribution of a urine-based jail screening program to citywide male Chlamydia and gonorrhea case rates in New York City. Sexually Transmitted Diseases. 2009;36(2 Suppl):S58–S61. doi: 10.1097/OLQ.0b013e31815615bb. [DOI] [PubMed] [Google Scholar]
- Provine D. Unequal under law: Race in the war on drugs. Chicago, IL: University of Chicago Press; 2007. [Google Scholar]
- Rich JD, Wakeman SE, Dickman SL. Medicine and the epidemic of incarceration in the United States. New England Journal of Medicine. 2011;364(22):2081–2083. doi: 10.1056/NEJMp1102385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts CA, Lobato MN, Bazerman LB, Kling R, Reichard AA, Hammett TM. Tuberculosis prevention and control in large jails: A challenge to tuberculosis elimination. American Journal of Preventive Medicine. 2006;30(2):125–130. doi: 10.1016/j.amepre.2005.10.018. [DOI] [PubMed] [Google Scholar]
- Roberts D. The social and moral cost of mass incarceration in African American communities. Stanford Law Review. 2004;56:1272–1305. [Google Scholar]
- Rogers SM, Khan MR, Tan S, Turner CF, Miller WC, Erbelding E. Incarceration, high-risk sexual partnerships and sexually transmitted infections in an urban population. Sexually Transmitted Infections. 2012;88(1):63–68. doi: 10.1136/sextrans-2011-050280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen DL, Hammond WP, Wohl DA, Golin CE. Disease prevalence and use of health care among a national sample of black and white male state prisoners. Journal of Health Care for the Poor and Underserved. 2012;23(1):254–272. doi: 10.1353/hpu.2012.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen DL, Schoenbach VJ, Wohl DA, White BL, Stewart PW, Golin CE. An evaluation of HIV testing among inmates in the North Carolina prison system. American Journal of Public Health. 2009;99(Suppl 2):S452–459. doi: 10.2105/AJPH.2007.133124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAHMSA. Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010. [Google Scholar]
- Solomon L, Flynn C, Muck K, Vertefeuille J. Prevalence of HIV, syphilis, hepatitis B, and hepatitis C among entrants to Maryland correctional facilities. Journal of Urban Health. 2004;81(1):25–37. doi: 10.1093/jurban/jth085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaulding AC, Perez SD, Seals RM, Hallman MA, Kavasery R, Weiss PS. Diversity of release patterns for jail detainees: Implications for public health interventions. American Journal of Public Health. 2011;101(Suppl 1):S347–352. doi: 10.2105/AJPH.2010.300004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: Declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications for adequate transitional care for HIV-infected prisoners: five essential components. Clinical Infectious Diseases. 2011;53(5):469–479. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan J, Walsh G. Census of jail facilities, 2006. Washington, DC: Bureau of Justice Statistics; 2011. [Google Scholar]
- Sykes B, Piquero A. Structuring and re-creating inequality: Health testing policies, race, and the criminal justice system. Annals of the American Academy of Political and Social Science. 2009;623(1):214–227. [Google Scholar]
- Taxman FS, Byrne JM, Pattavina A. Racial disparity and the legitimacy of the criminal justice system: Exploring consequences for deterrence. Journal of Health Care for the Poor and Underserved. 2005;16(4 Suppl B):57–77. doi: 10.1353/hpu.2005.0119. [DOI] [PubMed] [Google Scholar]
- Thomas JC, Levandowski BA, Isler MR, Torrone E, Wilson G. Incarceration and sexually transmitted infections: A neighborhood perspective. Journal of Urban Health. 2008;85(1):90–99. doi: 10.1007/s11524-007-9231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi AN, Grebla RC, Wright SM, Washington DL. Despite improved quality of care in the Veterans Affairs health system, racial disparity persists for important clinical outcomes. Health Affairs (Millwood) 2011;30(4):707–715. doi: 10.1377/hlthaff.2011.0074. [DOI] [PubMed] [Google Scholar]
- Wakefield S, Wildeman C. Mass imprisonment and racial disparities in childhood behavioral problems. American Society of Criminology. 2011;10(3):793–817. [Google Scholar]
- Wang EA, Hong CS, Samuels L, Shavit S, Sanders R, Kushel M. Transitions clinic: Creating a community-based model of health care for recently released California prisoners. Public Health Reports. 2010;125(2):171–177. doi: 10.1177/003335491012500205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang EA, Hong CS, Shavit S, Sanders R, Kessell E, Kushel MB. Engaging individuals recently released from prison into primary care: A randomized trial. American Journal of Public Health. 2012;102(9):e22–e29. doi: 10.2105/AJPH.2012.300894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West H, Sabol W, Greenman S. Prisoners in 2009. Washington, DC: U.S. Department of Justice Bureau of Justice Statistics; 2010. [Google Scholar]
- Western B, Wildeman C. The black family and mass incarceration. Annals of the American Academy of Political and Social Science. 2009;621:221–242. [Google Scholar]
- Wildeman C. Parental incarceration, the prison boom, and the concentration of childhood disadvantage. Demography. 2009;46(2):265–280. doi: 10.1353/dem.0.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildeman C, Western B. Incarceration in fragile families. The Future of Children. 2010;20(2):157–177. doi: 10.1353/foc.2010.0006. [DOI] [PubMed] [Google Scholar]
- Williams BA, Stern MF, Mellow J, Safer M, Greifinger RB. Aging in correctional custody: Setting a policy agenda for older prisoner health care. American Journal of Public Health. 2012;102(8):1475–1481. doi: 10.2105/AJPH.2012.300704. [DOI] [PMC free article] [PubMed] [Google Scholar]