Abstract
IMPORTANCE
In asthma and other diseases, vitamin D insufficiency is associated with adverse outcomes. It is not known if supplementing inhaled corticosteroids with oral vitamin D3 improves outcomes in patients with asthma and vitamin D insufficiency.
OBJECTIVE
To evaluate if vitamin D supplementation would improve the clinical efficacy of inhaled corticosteroids in patients with symptomatic asthma and lower vitamin D levels.
DESIGN, SETTING, AND PARTICIPANTS
The VIDA (Vitamin D Add-on Therapy Enhances Corticosteroid Responsiveness in Asthma) randomized, double-blind, parallel, placebo-controlled trial studying adult patients with symptomatic asthma and a serum 25-hydroxyvitamin D level of less than 30 ng/mL was conducted across 9 academic US medical centers in the National Heart, Lung, and Blood Institute’s AsthmaNet network, with enrollment starting in April 2011 and follow-up complete by January 2014. After a run-in period that included treatment with an inhaled corticosteroid, 408 patients were randomized.
INTERVENTIONS
Oral vitamin D3 (100 000 IU once, then 4000 IU/d for 28 weeks; n = 201) or placebo (n = 207) was added to inhaled ciclesonide (320 µg/d). If asthma control was achieved after 12 weeks, ciclesonide was tapered to 160 µg/d for 8 weeks, then to 80 µg/d for 8 weeks if asthma control was maintained.
MAIN OUTCOMES AND MEASURES
The primary outcome was time to first asthma treatment failure (a composite outcome of decline in lung function and increases in use of β-agonists, systemic corticosteroids, and health care).
RESULTS
Treatment with vitamin D3 did not alter the rate of first treatment failure during 28 weeks (28%[95% CI, 21%-34%] with vitamin D3 vs 29% [95% CI, 23%–35%] with placebo; adjusted hazard ratio, 0.9 [95% CI, 0.6–1.3]). Of 14 prespecified secondary outcomes, 9 were analyzed, including asthma exacerbation; of those 9, the only statistically significant outcome was a small difference in the overall dose of ciclesonide required to maintain asthma control (111.3 µg/d [95% CI, 102.2–120.4 µg/d] in the vitamin D3 group vs 126.2 µg/d [95% CI, 117.2–135.3 µg/d] in the placebo group; difference of 14.9 µg/d [95% CI, 2.1–27.7 µg/d]).
CONCLUSIONS AND RELEVANCE
Vitamin D3 did not reduce the rate of first treatment failure or exacerbation in adults with persistent asthma and vitamin D insufficiency. These findings do not support a strategy of therapeutic vitamin D3 supplementation in patients with symptomatic asthma.
TRIAL REGISTRATION
clinicaltrials.gov Identifier: NCT01248065
In children and adults with asthma, serum 25-hydroxyvitamin D levels of less than 30 ng/mL have been linked to airway hyperresponsiveness, impaired lung function, increased exacerbation frequency, and reduced corticosteroid responsiveness.1–3 Although the underlying mechanisms are not yet known, it has been suggested that vitamin D enhances anti-inflammatory functions of corticosteroids in asthma, either by enhancing the ability of T cells to produce IL-104 or through inhibition of TH17 cytokine production.5,6 Low vitamin D levels also create a proinflammatory state, and vitamin D signaling pathways and receptor polymorphisms7–9 can influence the balance between TH1 and TH2,9,10 airway smooth muscle contraction, and airway remodeling,11,12 all of which have been implicated in asthma pathogenesis and severity. These data suggesting that vitamin D supplementation could modify steroid response and reduce airway inflammation have led to open questions about whether treatment with vitamin D might improve outcomes in patients with asthma.4,5
National and international guidelines recommend inhaled corticosteroids as the primary anti-inflammatory controller therapy for persistent asthma; however, there is significant variability in the responses of patients to inhaled corticosteroids, with clinical studies demonstrating that up to 45% of patients do not have a clinical or physiological response to these agents.13,14 An element of this variability may be explained by vitamin D status, with studies suggesting that vitamin D may augment the effects of corticosteroids.4 We hypothesized that vitamin D supplementation would improve the clinical efficacy of inhaled corticosteroids in patients with asthma as measured by exacerbations, lung function, and the dose of inhaled corticosteroids required to maintain asthma control.
Methods
Participants
Eligible participants were aged 18 years or older with asthma and a serum 25-hydroxyvitamin D level of less than 30 ng/mL. Asthma entry criteria included (1) physician-diagnosed disease and (2) evidence of either bronchodilator reversibility (forced expiratory volume in the first second of expiration [FEV1≥12% following 180 µg [4 puffs] of levalbuterol) or airway hyperresponsiveness (provocative concentration of methacholine at which FEV1 decreased by 20% [PC20] <8 mg/mL if not receiving inhaled corticosteroids or ≤16 mg/mL if receiving inhaled corticosteroids). All participants received stable asthma controller therapy for 2 weeks or longer and had a predicted FEV1 of 50% or greater. The VIDA (Vitamin D Add-on Therapy Enhances Corticosteroid Responsiveness in Asthma) study protocol was approved by the institutional review board at each participating institution, all participants provided written informed consent, and a data and safety monitoring board monitored the study. The full study protocol and additional information appears in e Methods, e Appendix 1, and e Appendix 2 in the Supplement.
Study Design and Treatment
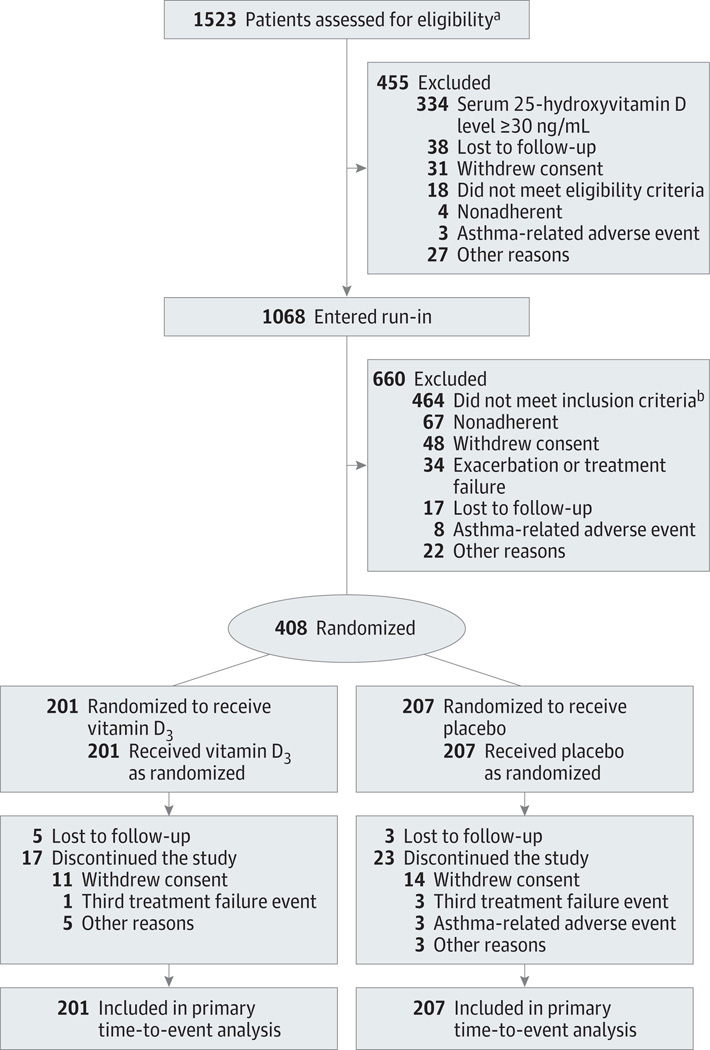
The study was a randomized, double-masked, parallel group trial (e Figure 1 in Supplement), with each eligible participant randomly assigned to either placebo or high-dose vitamin D3 (100 000 IUonce, followed by 4000 IU/dfor28 weeks) (Bio Tech Pharmacal) added to inhaled ciclesonide (320 µg/d; 2 puffs twice daily) and levalbuterol. Eligible participants were screened from April 2011 to May 2013 and enrolled if they met the inclusion criteria. After completing a 4-week run-in period of treatment with only ciclesonide and levalbuterol (prior asthma treatments were discontinued), participants were randomized. Participants were excluded if they did not meet study criteria at entry or during run-in (Figure 1).
Figure 1. Participant Flow of VIDA Trial.
VIDA indicates Vitamin D Add-on Therapy Enhances Corticosteroid Responsiveness in Asthma. Postrandomization dropouts were included in the analysis as censored observations.
a Details for those screened but ineligible were not collected.
bThe most common reasons were predicted forced expiratory volume in the first second of expiration (FEV1) greater than 90% (n = 286; a subsequent protocol modification removed this criteria), did not have a provocative concentration of methacholine at which FEV1 decreased by 20% or did not qualify for challenge (n = 60), too few symptoms (n = 52), and predicted FEV1 of less than 50% (n =41).
Computer-generated randomization was stratified by clinical center, body mass index (BMI, calculated as weight in kilograms divided by height in meters squared; ≤25 vs >25), and race (blacks vs all others), with treatment assignments made in random permuted blocks of size 2. The placebo vitamin D soft gelatin capsules matched in appearance those containing vitamin D3. To assess responsiveness to corticosteroids, 40 mg of prednisone was added to each participant’s daily regimen for 1 week at the end of the run-in; a change in FEV1 of 5% or greater was considered significant.15,16
After randomization, participants entered a 12-week inhaled corticosteroids stability phase, in which they continued to receive 320 µg/d of ciclesonide. This was followed up by 2 phases in which inhaled corticosteroids were tapered by 50% if the participant’s asthma symptoms were controlled. During the first phase at 12 weeks, patients were tapered to 160 µg/d of ciclesonide for 8 weeks, and during the second phase at 20 weeks, patients were tapered to 80 µg/d for 8 weeks. Participants were terminated or withdrawn from the study if they had more than 2 treatment failures or exacerbations. The last participant completed follow-up in January 2014.
Adherence to dosing with ciclesonide and vitamin D capsules was monitored electronically (DOSER device [MediTrack] for ciclesonide and MEMS 6 monitor [Aardex] for capsules), and symptoms and peak expiratory flows were recorded in a device that was both an electronic diary and a peak flow meter (Spirotel [Medical International Research]).
Outcome Measures
The primary end point was time to first asthma treatment failure during the 28-week study period. Treatment failure was defined as 1 or more of the following: peak expiratory flow of 65% or less of baseline measurement on 2 of 3 consecutive measurements; FEV1 of 80% or less of baseline measurement on 2 consecutive measurements; increase in levalbuterol dose of 8 puffs/d or more for 48 hours (vs baseline); additional use of inhaled corticosteroids or use of oral or parenteral corticosteroids for asthma; emergency department or hospitalization for asthma with systemic corticosteroid use; participant lack of satisfaction with treatment; and physician clinical judgment for safety reasons.17–19
There were 14 prespecified secondary outcomes. Of these, 9 have been analyzed and are presented herein: asthma exacerbations, lung function, airway hyperresponsiveness, asthma symptoms, asthma control,20 asthma-specific quality of life,21 achieving vitamin D sufficiency (25-hydroxyvitamin D level ≥ 30 ng/mL), total inhaled corticosteroids dose, and airway inflammation (e Table 1 in Supplement). Asthma exacerbations were defined by meeting criteria for treatment failure and 1 or more of the following: failure to respond to rescue algorithm within 48 hours; FEV1 of less than 50% of baseline measurement on 2 consecutive measurements; FEV1of less than 40% of predicted level on 2con-secutive measurements; use of 16 puffs/d or more of as-needed levalbuterol for 48 hours; experiencing an exacerbation of asthma according to physician opinion; and use of oral or parenteral corticosteroids due to asthma.18,19,22
Asthma symptoms were measured using an electronic diary and the Asthma Symptom Utility Index (ASUI).23 Participants were instructed to complete the electronic diary every morning and evening and asked to grade the following symptoms: shortness of breath, chest tightness, wheezing, cough, and phlegm or mucus. Symptoms were graded as 0 (absent; no symptom present), 1 (mild; symptom was minimally troublesome or not sufficient to interfere with normal daily activity or sleep), 2 (moderate; symptom was sufficiently troublesome to interfere with normal daily activity or sleep), or 3 (severe; symptom was so severe as to prevent normal activity or sleep, or both). The scores on the ASUI range from 0 to 1; a higher score indicates better symptom control (0.88, mild; 0.64, moderate; and 0.47, severe asthma) and the minimal clinically important difference is 0.09.24
Asthma control was measured using the Asthma Control Test (ACT).20 The proportion of days in which a participant had no asthma symptoms or use of levalbuterol was recorded in the electronic diary. The scores on the ACT range from 5 to 25; higher scores indicate better asthma control and the minimal clinically important difference is 3.25 Asthma-specific quality of life was measured using the Asthma Bother Profile questionnaire.26 The scores on the Asthma Bother Profile range from 0 to 75 and higher scores indicate poorer quality of life. Serum 25-hydroxyvitamin D level was measured at baseline and at the end of each ciclesonide treatment phase using the DiaSorin LIAISON vitamin D assay. Vitamin D responder status was defined as vitamin D3–treated participants who achieved a 25-hydroxyvitamin D level of 30 ng/mL or greater. Airway inflammation was measured by performing a differential cell count from induced sputum samples collected at the end of the 4-week run-in and at 12 weeks. Race was assessed by participant self-report, using National Institutes of Health race/ethnicity reporting standards and categories.
Statistical Analysis
The primary analysis was intent-to-treat, comparing treatment groups in a Cox proportional hazards regression model that estimated a hazard ratio (HR) for events across the entire 28-week treatment period, as well as with in each of the treatment phases. The trial was designed to have a sample size of 400 for 90% power to detect an HR for treatment failures of 0.56 (a reduction from 40.0% in the placebo group and 24.5% in the vitamin D3 group based on data from the Asthma Clinical Research Network Salmeterol or Corticosteroids18 and Salmeterol ± Inhaled Corticosteroids19 trials), assuming an overall α level of .05, 2-sided test, and 15% withdrawal. The model included dropouts as censored observations, and was adjusted for clinical center, BMI, and race. An additional model incorporated the ability to taper inhaled corticosteroids during the treatment phases as a time-dependent covariate. The overall rates of treatment failures and exacerbations were evaluated in proportional hazards regression models for recurrent events.27
Repeated-measures analysis of covariance models were used for secondary outcomes, with adjustment for the baseline stratification factors of clinical center, BMI, and race. Total inhaled corticosteroids dose was compared between the treatment groups in a repeated-measures analysis of variance model. The difference in inhaled corticosteroids dose was evaluated for each of the 2 taper phases with a Bonferroni correction applied to the significance criterion. The ability to taper was evaluated with χ2 tests. Prespecified subgroup analyses involving BMI and race were evaluated using interaction terms in the relevant models. A prespecified exploratory responder analysis was performed that evaluated outcomes in those participants treated with vitamin D3 who achieved a serum 25-hydroxyvitamin D level of 30 ng/mL or greater vs placebo. Baseline 25-hydroxyvitamin D level was evaluated as a predictor of achieving 25-hydroxyvitamin D of 30 ng/mL or greater in a logistic regression model. All tests were 2-sided and based on a significance criterion of P < .05. Without formal adjustment for the number of secondary analyses that were performed, the secondary results should be considered exploratory. All analyses were performed using SAS version 9.3 (SAS Institute Inc).
Results
Enrollment and Study Completion
A total of 1523 participants were enrolled and 408 were randomized (n = 201 in the vitamin D3 group and n = 207 in the placebo group). Overall, the completion rate was similar in both groups(89%[95%CI,85%–93%] in the vitamin D3 groupvs87% [95% CI, 83%–92%] in the placebo group), with a median duration of follow-up of 28.1 weeks (interquartile range [IQR], 27.6–28.7 weeks). The most common reasons for study discontinuation post randomization were withdrawal of consent and loss to follow-up (Figure 1).
Baseline Characteristics
At baseline, there were no significant differences in participant characteristics between the groups (Table 1). The study enrolled adult participants with symptomatic asthma (median asthma control days, 0% [IQR, 0%–31%]; median ACT score, 20 [IQR, 17–22]) and mild spirometric impairment. Health care use, corticosteroid courses, and days of school or work missed due to asthma did not differ significantly between groups. The mean baseline 25-hydroxyvitamin D level was 18.8 ng/mL (95% CI, 18.2–19.5 ng/mL). Of the participants, 54 (13%) had 25-hydroxyvitamin D levels of less than 10 ng/mL and 217 (53%) had levels of less than 20 ng/mL. Of the participants, 13% in the vitamin D3 group and 18% in the placebo group reported taking supplements containing vitamin D at baseline. Of the participants, 18% met FEV1 criteria for oral corticosteroid response. Following the run-in with inhaled ciclesonide, participants reported a small improvement in asthma control that was not clinically significant (mean change in ACT score, 1.00 [95% CI, 0.65–1.35]; mean change in ASUI score, 0.03 [95% CI, 0.02–0.05]).
Table 1.
Baseline Characteristics of Randomized Participants
| Placebo (n = 207) |
Vitamin D3 (n = 201) |
|
|---|---|---|
| No. (%) of Participantsa | ||
| Men | 66 (31.9) | 64 (31.8) |
| Race/ethnicity | ||
| Asian/Pacific Islander | 7 (3.4) | 7 (3.5) |
| Black | 68 (32.9) | 63 (31.3) |
| White | 111 (53.6) | 105 (52.2) |
| Hispanic | 19 (9.2) | 20 (10.0) |
| Otherb | 2 (1.0) | 6 (2.0) |
| Previous year | ||
| ED or unscheduled office visit | 65 (31.4) | 75 (37.3) |
| Hospitalizations | 12 (5.8) | 7 (3.5) |
| Systemic corticosteroid therapy | 62 (30.0) | 69 (34.3) |
| Missed work or school or not able to do housework |
50 (24.2) | (n = 200) 59 (29.5) |
| Leukotriene receptor antagonist or 5-lipoxygenase inhibitor use |
(n = 206) 53 (25.7) | 48 (23.9) |
| Steroid use | ||
| Oral | 59 (28.5) | 67 (33.3) |
| Inhaled | 82 (39.6) | 95 (47.3) |
| Plus long-acting bronchodilator | 132 (63.8) | (n = 200) 119 (59.5) |
| Level of 25-hydroxyvitamin D <20 ng/mL | 116 (56.0) | 101 (50.2) |
| Change in FEV1 ≥5% with prednisonec | (n = 176) 32 (18.2) |
(n = 167) 30 (18.0) |
| Season of enrollment | ||
| Spring | 68 (32.9) | 63 (31.3) |
| Summer | 60 (29.0) | 51 (25.4) |
| Fall | 37 (17.9) | 46 (22.9) |
| Winter | 42 (20.3) | 41 (20.4) |
| Mean (SD)a | ||
| Age, y | 39.5 (12.7) | 39.9 (13.1) |
| Asthma, y | 25.0 (12.8) | 24.9 (13.5) |
| Body mass indexd | 31.53 (9.51) | 32.00 (8.19) |
| Positive skin test, median (IQR) | 3.0 (2.0 to 6.0) |
3.0 (2.0 to 6.0) |
| Symptom scoree | ||
| Morning | 0.41 (0.36) | 0.41 (0.34) |
| Afternoon and evening | 0.43 (0.40) | 0.44 (0.35) |
| Asthma Symptom Utility Index scoref | 0.82 (0.12) | 0.83 (0.11) |
| Asthma control, median (IQR) | ||
| Test scoreg | 20.0 (17.0 to 22.0) |
19.0 (17.0 to 22.0) |
| Proportion of daysh | 7 (0 to 31) | 0 (0 to 29) |
| Asthma-related quality of life, median (IQR)i |
18.0 (12.0 to 28.0) |
19.0 (12.0 to 26.0) |
| Level of 25-hydroxyvitamin D, median (IQR), ng/mL |
18.8 (13.4 to 23.7) |
19.9 (14.5 to 25.0) |
| Peak flow, L/min | ||
| Morning | 393.6 (107.0) | 394.4 (103.2) |
| Afternoon and evening | 399.4 (109.2) | 399.2 (103.9) |
| FEV1 before albuterol use | ||
| Level, L | 2.62 (0.83) | 2.63 (0.78) |
| % Predicted | 80.5 (14.2) | 80.7 (13.8) |
| Ratio of FEV1 to forced vital capacity | 0.71 (0.09) | 0.72 (0.09) |
| After prednisone, % changec | −0.49 (8.25) | −0.88 (7.14) |
| FEV1 after albuterol use, % predicted | 92.09 (13.65) | 91.32 (13.83) |
| Maximum albuterol reversibility, % change |
18.41 (11.84) | 16.63 (11.56) |
| Methacholine PC20,, geometric mean (CV), mg/mL |
1.85 (1.67) | 2.05 (1.61) |
| Sputum eosinophils, median (IQR), % | 0.40 (0 to 1.30) |
0.30 (0 to 1.30) |
Abbreviations: CV, coefficient of variation; ED, emergency department; FEV1, forced expiratory volume in the first second of expiration; IQR, interquartile range; PC20, provocative concentration at which FEV1 decreased by 20%.
Unless otherwise indicated.
Included American Indian, Alaskan Native, or participant-selected “other” category.
Dosage of 40 mg for 5 to 7 days.
Calculated as weight in kilograms divided by height in meters squared.
Indicates the average score for shortness of breath, chest tightness, wheezing, cough, and phlegm or mucus (0 = absent, 1 = mild, 2 = moderate, 3 = severe).
Score range is 0 to 1 (a higher score indicates better symptom control).
Score is sum of questions 1 through 5 (score range for individual questions is 1 to 5; higher values indicate better asthma control).
Based on use of levalbuterol or any symptoms reported during the 14 days prior to the end of run-in.
Score is sum of scores across 18 questions on the Asthma Bother Profile Scale (score range, 0–5; response range, “no bother” to “makes my life a misery”).
Serum 25-Hydroxyvitamin D Levels
In the vitamin D3 treatment group, 82% of participants achieved a serum25-hydroxyvitamin D level of 30 ng/mL or greater. The mean serum 25-hydroxyvitamin D level in the vitamin D3 group was 41.9 ng/mL (95% CI, 40.1–43.7 ng/mL) at 12 weeks (range, 6.3–97.3 ng/mL), an effect which persisted at 20 weeks (42.6 ng/mL; 95% CI, 40.8–44.3 ng/mL) and 28 weeks (41.8 ng/mL; 95% CI, 39.8–43.7 ng/mL) (e Figure 2 in Supplement).Mean serum 25-hydroxyvitamin D levels remained less than 20 ng/mL in the placebo group, although 9% of participants treated with placebo were observed to have 25-hydroxyvitamin D levels of 30 ng/mL or greater at 12 weeks (range, 4.4–52.2 ng/mL). Of the participants, 13% in the vitamin D3 group and 15% in the placebo group reported taking supplements containing vitamin D at the end of the trial. In those treated with vitamin D3, baseline serum 25-hydroxyvitamin D level was associated with vitamin D sufficiency at 12 weeks (odds ratio, 2.1; 95% CI, 1.2–3.8) for achieving 25-hydroxyvitamin D level of 30 ng/mL or greater observed for each 10-ng/mL increment. Median adherence was 96% (IQR, 90%-99%) in those receiving vitamin D3 and 96% (IQR, 89%-99%) in those receiving placebo (P = .85). Median ciclesonide adherence was 95%(IQR, 90%–98%) in the vitamin D3 group and 94%(IQR,90%–98%)in the placebo group (P = .56).
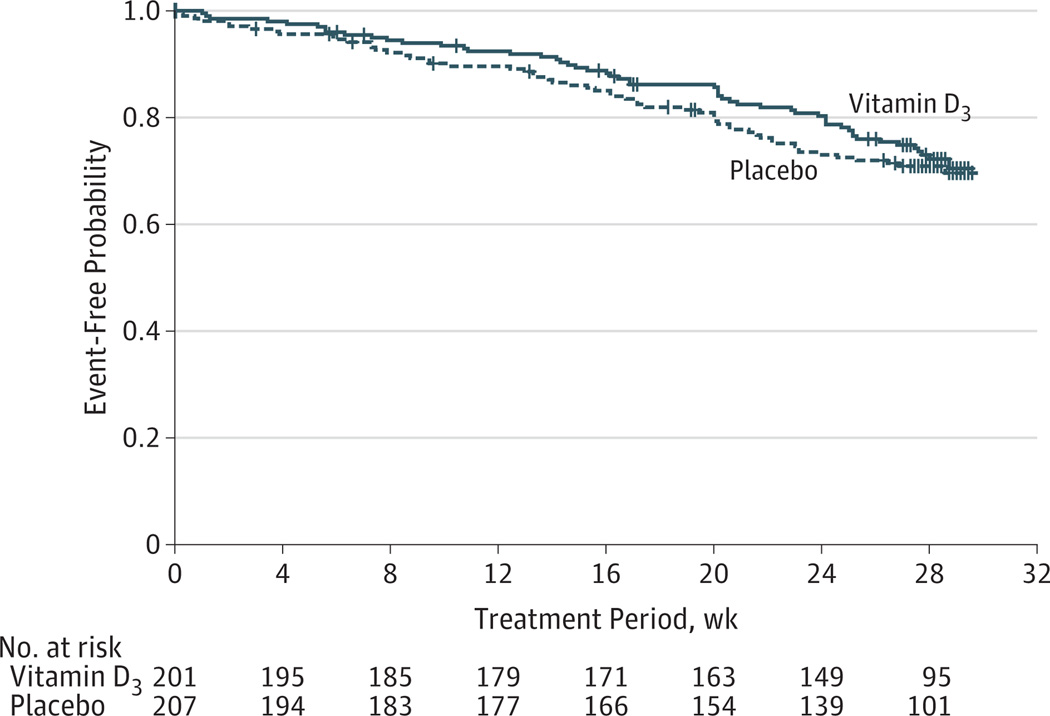
Primary Outcome of Asthma Treatment Failures
The addition of vitamin D3 to ciclesonide did not significantly reduce the rate of first treatment failure compared with placebo; 28% (95% CI, 21%–34%) and 29% (95% CI, 23%–35%) of participants in each group, respectively, experienced at least 1 treatment failure during 28 weeks (adjusted HR, 0.9 [95% CI, 0.6–1.3], P = .54; Figure 2). The overall treatment failure rate was not reduced in the vitamin D3 group at 0.58/person-year (95% CI, 0.47–0.69/person-year) vs 0.74/person-year (95% CI, 0.61–0.87/person-year) in the placebo group (adjusted HR, 0.8 [95% CI 0.6–1.1], P = .17; Table 2). These estimates did not change significantly when taper status was included in the model (e Table 2 in Supplement). Participants most commonly achieved treatment failure due to the need for increased inhaled or systemic steroids (58%) or by experiencing an exacerbation (46%) (e Table 3 in Supplement). Baseline serum 25-hydroxyvitamin D level was not associated with treatment failure (HR, 0.9 per 10-ng/mL increment [95% CI, 0.7–1.1 per 10-ng/mL increment], P = .32).
Figure 2. Primary Treatment Failure Outcome.
Vertical bars represent censored events. The adjusted hazard ratio for time from randomization to first treatment failure was 0.9 (95% CI, 0.6–1.3) for the vitamin D3 vs placebo treatment groups (P = .54).
Table 2.
Primary Treatment Failure and Exacerbation for Intent-to-Treat Vitamin D3 vs Placebo
| Vitamin D3 (n = 201) | Placebo (n = 207) | Unadjusted HR (95% CI) |
P Value |
Adjusted HR (95% CI)a |
P Value |
|
|---|---|---|---|---|---|---|
| Treatment failureb | ||||||
| First, No. of events (%) [95% CI] | 53 (28) [21–34] | 58 (29) [23–35] | 0.9 (0.6–1.3) | .57 | 0.9 (0.6–1.3) | .54 |
| Overall, No. of events (rate/person-year) [95% CI]c |
63 (0.58) [0.47–0.69] | 83 (0.74) [0.61–0.87] | 0.8 (0.5–1.1) | .17 | 0.8 (0.6–1.1) | .17 |
| Exacerbationd | ||||||
| First, No. of events (%) [95% CI] | 28 (13) [8–18] | 37 (19) [13–24] | 0.7 (0.5–1.2) | .24 | 0.7 (0.4–1.2) | .21 |
| Overall, No. of events (rate/person-year) [95% CI]c |
28 (0.26) [0.18–0.33] | 45 (0.40) [0.30–0.50] | 0.6 (0.4–1.0) | .06 | 0.63 (0.39–1.01) | .05 |
Abbreviation: HR, hazard ratio.
Adjusted for center, black race, and body mass index greater than 25.
Defined as 1 or more of the following: peak expiratory flow of 65% or less of baseline measurement on 2 of 3 consecutive measurements; forced expiratory volume in the first second of expiration (FEV1) of 80% or less of baseline measurement on 2 consecutive measurements; increase in levalbuterol dose of 8 or more puffs/day for 48 hours (vs baseline dose); additional use of inhaled corticosteroid, or use of oral or parenteral corticosteroids for asthma; emergency department or hospitalization for asthma with systemic corticosteroid use; participant lack of satisfaction with treatment; or physician clinical judgment for safety reasons.
Total person-years in analysis: 103.9 person-years for vitamin D3 group and 106.4 person-years for placebo group.
Defined as meeting criteria for treatment failure listed in footnote “b” plus 1 or more of the following: failure to respond to rescue algorithm within 48 hours; FEV1 of less than 50% of baseline measurement on 2 consecutive measurements; FEV1 of less than 40% of predicted on 2 consecutive measurements; increase in levalbuterol dose of 16 or more puffs/day for 48 hours (vs baseline dose); experiencing an exacerbation of asthma according to physician; use of oral or parenteral corticosteroid due to asthma.
Secondary Outcomes
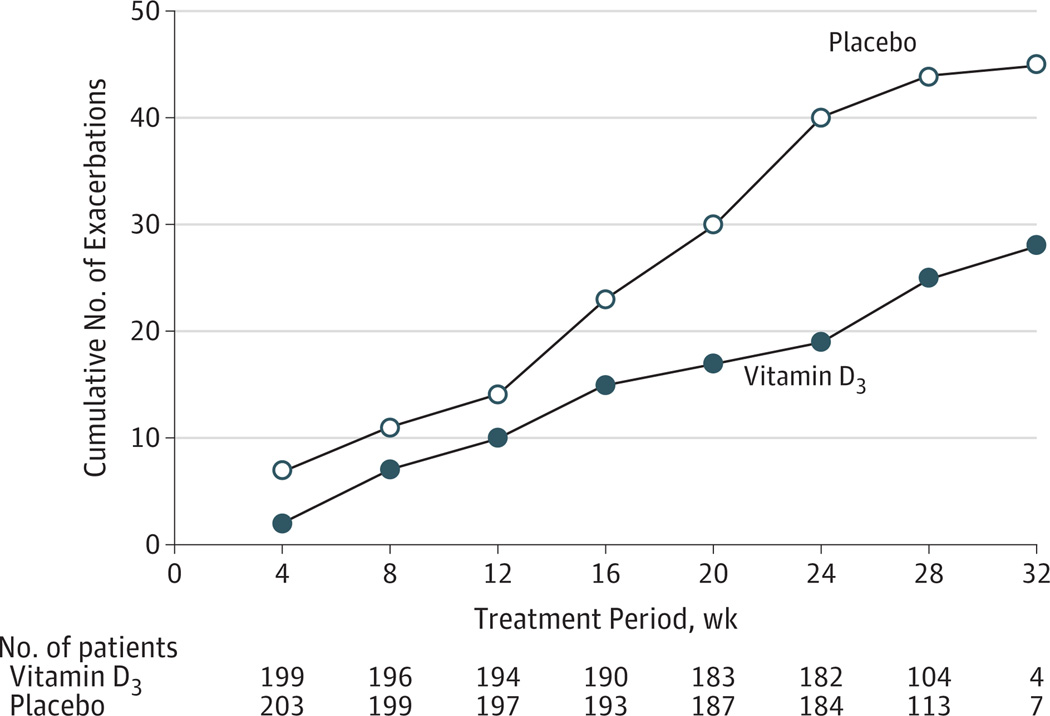
Asthma Exacerbations
The addition of vitamin D3 to ciclesonide did not significantly reduce the rate of first asthma exacerbation compared with placebo; 13% (95% CI, 8%–18%) and 19% (95% CI, 13%– 24%) of participants in each group, respectively, experienced at least 1 exacerbation during 28 weeks (adjusted HR, 0.7 [95% CI, 0.4–1.2], P = .21). The addition of vitamin D3 also did not significantly reduce the overall exacerbation rate (0.26/person-year [95% CI, 0.18–0.33/person-year] in the vitamin D3 group vs 0.40/person-year [95% CI, 0.30–0.50/person-year] in the placebo group; adjusted HR, 0.63 [95% CI, 0.39–1.01], P = .05; Table 2 and Figure 3). These estimates did not change significantly when taper status was included in the model (e Table 2 in Supplement).
Figure 3. Secondary Exacerbation Outcome.
The first data point corresponds to the number of exacerbations that occurred during the first 4 weeks of treatment. The adjusted hazard ratio for cumulative number of exacerbations that occurred over the course of the trial was 0.63 (95% CI, 0.39–1.01; P = .05).
Ciclesonide Dosing
Ultimately, 96% (95% CI, 93%–99%) of the vitamin D3 group and 91% (95% CI, 87%–95%) of the placebo group achieved a 50% reduction in the starting dose of ciclesonide (P = .07); 89% (95% CI, 84%–93%) vs 80% (95% CI, 75%–86%), respectively, achieved a 75% reduction in the starting dose of ciclesonide (P = .03). During the third treatment phase (phase 2b), a difference of 14.9 µg/d (95% CI 2.1–27.7 µg/d) in cumulative ciclesonide dosing was observed between the 2 groups (the vitamin D3 group received 111.3 µg/d [95% CI, 102.2–120.4 µg/d] of ciclesonide and the placebo group received 126.2 µg/d [95% CI, 117.2–135.3 µg/d]) (P = .02; Bonferroni-adjusted P = .03 for the 2 taper phases).
Other Secondary Outcomes and Subgroup Comparisons
Treatment with vitamin D3 had no significant effect on lung function or airway hyperreactivity (e Table 4 and e Figure 3 in Supplement). Neither asthma quality of life nor asthma control improved with vitamin D3 (e Table 4 in Supplement). Sputum eosinophilia did not change after treatment with vitamin D3.
Black race was associated with lower baseline 25-hydroxyvitamin D levels, with a mean of 15.6 ng/mL (95% CI, 14.4–16.8 ng/mL) vs 20.4 ng/mL (95% CI, 19.6–21.1 ng/mL) in all other races (P < .001). Although non black participants demonstrated a significant reduction in the rate of first asthma exacerbation with vitamin D3 (HR, 0.49 [95% CI, 0.25–0.96], P = .04), there was no significant interaction between race and treatment for this outcome (P = .07) or any other outcomes (e Table 5 in Supplement). Increased BMI was not associated with an increased risk of treatment failures or exacerbations in either treatment group, and no interactions were significant.
Exploratory Vitamin D3 Responder Analyses
When vitamin D3–treated participants who achieved a 25-hydroxyvitamin D level of 30 ng/mL or greater (n = 157 of 201) were compared with all placebo-treated participants (n = 207), the rate of first treatment failure was not reduced: 25% (95% CI, 18%-32%) vs 29% (95% CI, 23%-35%), respectively, during 28 weeks (adjusted HR, 0.8 [95% CI, 0.5–1.2], P = .20; e Table 6 in Supplement). The rate of first exacerbation was lower for the vitamin D3 group (11%; 95% CI, 6%-16%) compared with the placebo group (19%; 95% CI, 13%-24%) (adjusted HR, 0.57 [95% CI, 0.33–0.99], P = .05). Among participants who responded to treatment, the overall rates were lower for treatment failures (adjusted HR, 0.6 [95% CI, 0.4–0.9], P = .03) and exacerbations (adjusted HR, 0.5 [95% CI, 0.3–0.8], P = .01). The change in serum 25-hydroxyvitamin D level from baseline to 12 weeks was significantly associated with the rate of treatment failures and exacerbations. Each 10-ng/mL increase in serum 25-hydroxyvitamin D level was associated with a reduction in the overall rate of treatment failures (HR, 0.88 [95% CI, 0.78–0.99], P = .04) and overall rate of exacerbations (HR, 0.80 [95% CI, 0.67–0.96], P = .02).
Adverse Events
Nonasthma adverse events did not differ significantly between the treatment groups. The ratio of urine calcium to creatinine exceeded 0.37 in 14 participants, all of which resolved on repeat measurement. No instances of nephrolithiasis were reported.
Discussion
In this randomized clinical trial of vitamin D3 added to ciclesonide in patients with symptomatic asthma, supplemental vitamin D3 did not result in a significant reduction in the rate of first treatment failure or exacerbation. There was also no significant reduction in the secondary end points related to asthma control, airway function, quality of life, or airway inflammation.
Of the 9 secondary end points assessed, the only significant association observed was with dose of inhaled corticosteroids. Vitamin D3 allowed participants to taper inhaled corticosteroids to as little as 25% of the original dose, but the absolute difference in inhaled corticosteroids dose was small (14.9 µg/d). Given that concern has been raised with the safety of both long-acting β-agonists and anticholinergics28,29 (these agents are commonly added when inhaled corticosteroids are not optimally efficacious), this small effect of add-on vitamin D3 might be important over time, but this would require further investigation. Because of the large number of secondary outcomes and lack of adjustment for multiple comparisons, this finding needs to be considered exploratory and interpreted with caution.
Our study must be interpreted in the context of a number of potential limitations. First, although vitamin D3 did not reduce the treatment failure rate, it is possible that the failure to observe an effect is attributable to inadequate power. There was a lower than expected event rate (29%) in the control group, which could have limited the ability to detect a significant difference. The study was powered appropriately for detecting relatively moderate size population effects, but it was not designed for establishing the existence of smaller effects. Thus, it is possible that studies of larger sample size and longer duration will be needed to fully resolve the question of vitamin D3 efficacy on asthma. Second, although we demonstrated significant increases in serum 25-hydroxyvitamin D level after 12 weeks, there was a wide range of observed 25-hydroxyvitamin D levels in the study population at this time point, suggesting that variable response to vitamin D3 may have occurred. If associated with delayed onset of maximal 25-hydroxyvitamin D level in some participants, this may have underestimated the effect of vitamin D3 and could explain the differences we observed between time-dependent outcomes and total numbers of treatment failures or exacerbations.
Third, during the course of designing and conducting the VIDA trial, consensus definitions of asthma exacerbations have changed, resulting in our primary outcome of treatment failure being different from the currently recommended definition of an asthma exacerbation for asthma clinical trials.22 Although this does not directly affect the internal validity of the trial, it does affect the generalizability of our findings. Fourth, although vitamin D insufficiency mayinduce a proinflammatory state, we did not observe any association between the sputum differential cell counts and vitamin D status and do not have data to determine whether vitamin D3 treatment altered sputum inflammatory biomarkers; thus, the effect of vitamin D3 treatment on airway inflammation in asthma remains unknown. Fifth, al though we did not observe any adverse events associated with vitamin D3 treatment in the context of our trial, we cannot generalize beyond what was observed with regard to the long-term safety of vitamin D3 treatment in asthma. Long-term risks of vitamin D3 could be similar, less than, or greater than what we observed, and long-term studies will be needed to shed further light on this issue.
Conclusions
In adults with persistent asthma and lower vitamin D levels, treatment with vitamin D3 did not reduce the rate of first treatment failure or exacerbation. These findings do not support a strategy of therapeutic vitamin D3 supplementation in patients with symptomatic asthma.
Supplementary Material
Acknowledgments
Funding/Support: This study was conducted with the support of grants HL098102, U10HL098096, UL1TR000150, UL1TR000430, UL1TR000050, HL098075, UL1TR001082, HL098090, HL098177, UL1TR000439, HL098098, UL1TR000448, HL098107, HL098112, HL098103, UL1TR000454, and HL098115 that were awarded by the National Heart, Lung, and Blood Institute. Ciclesonide and levalbuterol were provided without cost by Sunovion Pharmaceuticals Inc.
Role of the Sponsor: The National Institutes of Health (NIH) program officers participated in the design and conduct of the study; did not participate in the collection, management, analysis, and interpretation of the data; the NIH data and safety monitoring board participated in the preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We acknowledge the study participants, the AsthmaNet clinical research coordinators, and the data coordinating center. Rick Kelley (University of Wisconsin, Madison) received compensation for spirometry overreading; Carlos Bernal-Mizrachi, MD (Washington University), Neil Binkley, MD (University of Wisconsin, Madison), Michael Holick, MD (Boston University), and Augusto Litonjua, MD (Brigham and Women’s Hospital), did not receive compensation as vitamin D consultants; and Michael E. Hyland, PhD, FBPS (University of Plymouth), did not receive compensation for creation of AsthmaNet version of Asthma Bother Profile.
Footnotes
Group Information: A list of the National Heart, Lung, and Blood Institute’s AsthmaNet executive steering committee is included in the Supplement.
Author Contributions: Dr Castro had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Drs Castro and Sutherland contributed equally to the article.
Study concept and design: Castro, King, Kunselman, Cabana, Denlinger, Holguin, Kazani, Moore, Moy, Sorkness, Avila, Bacharier, Bleecker, Boushey, Fitzpatrick, Israel, Kraft, Lazarus, Lemanske, Martin, Mauger, Peters, Phipatanakul, Smith, Solway, Sumino, Wechsler, White, Sutherland.
Acquisition, analysis, or interpretation of data: Castro, King, Kunselman, Cabana, Denlinger, Kazani, Moore, Moy, Sorkness, Avila, Bacharier, Boushey, Chmiel, Fitzpatrick, Gentile, Hundal, Israel, Krishnan, LaForce, Lazarus, Lemanske, Lugogo, Martin, Mauger, Naureckas, Peters, Phipatanakul, Que, Sheshadri, Smith, Solway, Vedder, Sumino, Wechsler, Wenzel, White, Sutherland.
Drafting of the manuscript: Castro, King, Kunselman, Cabana, Holguin, Moy, Bleecker, Gentile, Hundal, Israel, Kraft, LaForce, Peters, Wechsler, Sutherland.
Critical revision of the manuscript for important intellectual content: Castro, King, Kunselman, Cabana, Denlinger, Holguin, Kazani, Moore, Moy, Sorkness, Avila, Bacharier, Boushey, Chmiel, Fitzpatrick, Gentile, Israel, Kraft, Krishnan, Lazarus, Lemanske, Lugogo, Martin, Mauger, Naureckas, Peters, Phipatanakul, Que, Sheshadri, Smith, Solway, Vedder, Sumino, Wechsler, Wenzel, White, Sutherland.
Statistical analysis: Castro, King, Kunselman, Hundal, Mauger, Sutherland.
Obtained funding: Holguin, Bacharier, Boushey, Kraft, Lemanske, Martin, Peters, Phipatanakul, Smith, Solway, Wechsler, Wenzel, Sutherland.
Administrative, technical, or material support: Castro, Holguin, Kazani, Moore, Avila, Bleecker, Boushey, Chmiel, Fitzpatrick, Gentile, Kraft, Krishnan, Martin, Naureckas, Peters, Que, Sheshadri, Smith, Solway, Vedder, Sumino, Wechsler, White.
Study supervision: Castro, Denlinger, Kazani, Moore, Moy, Sorkness, Avila, Boushey, Chmiel, Fitzpatrick, Gentile, Israel, LaForce, Lazarus, Mauger, Peters, Phipatanakul, Smith, Solway, Wechsler, Wenzel.
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Castro reported receiving grants from the National Institutes of Health, Boston Scientific, Amgen, Ception/Cephalon/Teva, Genetech, Medimmune, Merck, Novartis, GlaxoSmithKline, sanofi-aventis, Vectura, NextBio, and KaloBios; and receiving personal fees from Asthmatx, Boston Scientific, IPS/Holaria, Genentech, Merck, GlaxoSmithKline, Genentech, Boehringer Ingelheim, Elsevier, and Sparo Inc. Dr King reported receiving personal fees from KaloBios and Pearl Therapeutics. Ms Kunselman reported receiving grants from the National Heart, Lung, and Blood Institute and the National Institutes of Health. Drs Cabana, Holguin, Sorkness, Hundal, Naureckas, Phipatanakul, Que, Sheshardri, and Sullivan-Vedder reported no disclosures. Dr Denlinger reported receiving grants from the National Institutes of Health and personal fees from Novartis. Dr Kazani reported receiving income from Novartis Institutes for Biomedical Research. Drs Moore and Moy reported receiving grants from the National Institutes of Health. Drs Avila and Lazarus reported receiving grants from the National Heart, Lung, and Blood Institute and the National Institutes of Health. Dr Bacharier reported receiving personal fees from Aerocrine, AstraZeneca, Genentech/Novartis, GlaxoSmithKline, Merck, Schering, and Teva. Dr Bleecker reported receiving grants from the National Heart, Lung, and Blood Institute and the National Institutes of Health; and personal fees from AstraZeneca, Boehringer Ingelheim-Pfizer, Janssen-Johnson & Johnson, Genentech-Novartis, GlaxoSmithKline, Merck, sanofi/Regeneron, Amgen, AstraZeneca-MedImmune, Boehringer Ingelheim-Pfizer, Cephalon, Forest, Genentech-Roche, Novartis, and Pearl. Dr Boushey reported receiving a grant from Genentech. Dr Chmiel reported receiving personal fees from Genentech, Boehringer Ingelheim, CSL Behring, Gilead Sciences, KaloBios Pharmaceuticals, the American College of Chest Physicians, and the American Board of Pediatrics; and receiving grants from the National Institutes of Health and the Cystic Fibrosis Foundation. Dr Fitzpatrick reported receiving personal fees from MedImmune Inc Consulting, Merck, GlaxoSmithKline, Genentech, and Boehringer Ingelheim. Dr Gentile reported receiving personal fees from Teva and Merck. Dr Israel reported receiving personal fees from Cowen & Co, Infinity Pharmaceuticals, Merck, Regeneron Pharmaceuticals, Teva Specialty Pharmaceuticals, and UpTable 1ToDate; and receiving grants from Amgen and i3 Research (Biota). Dr Kraft reported receiving grants from the National Institutes of Health, GlaxoSmithKline, Chiesi, AstraZeneca, and Genentech. Dr Krishnan reported receiving a grant and support for travel from the National Heart, Lung, and Blood Institute. Dr LaForce reported receiving personal fees from Novartis Pharmaceuticals Corp. Dr Lemanske reported receiving grants from the National Heart, Lung, and Blood Institute and Pharmaxis; receiving grants, board membership, and personal fees from the University of Wisconsin; and receiving personal fees from Merck, Sepracor, SA Boney and Associates, GlaxoSmithKline, the American Institute of Research, Genentech, Double Helix Development, Boerhinger Ingelheim, Michigan Public Health, Allegheny General Hospital, American Academy of Pediatrics, West Allegheny Health, California Chapter 4, Colorado Allergy Society, Pennsylvania Allergy Society, Howard Pilgrim Health, California Society of Allergy, NYC Allergy Society, World Allergy Organization, Asia Pacific Association of Pediatric Allergy, Respirology and Immunology, Western Society of Allergy, Asthma, and Immunology, American Academy of Allergy, Asthma and Immunology, Elsevier, and UpToDate. Dr Lugogo reported receiving a grant from the National Institutes of Health. Dr Martin reported receiving grants from the National Institutes of Health and MedImmune; personal fees and nonfinancial support from Teva; and personal fees from UpToDate. Dr Mauger reported receiving grants from the National Heart, Lung, and Blood Institute; nonfinancial support from Sunovion and Teva; and personal fees and nonfinancial support from GlaxoSmithKline, Merck, and Boehringer Ingelheim. Dr Peters reported receiving grants from the National Institutes of Health and the National Heart, Lung, and Blood Institute; other from Johns Hopkins University and the American Lung Association-Asthma Clinical Research Center; personal fees from AstraZeneca, Aerocrine, Airsonett AB, Boehringer Ingelheim, GlaxoSmithKline, Merck, Novartis, Ono Pharmaceuticals, Pfizer, PPD Development, Quintiles, Sunovion, Targacept, Teva, Integrity CE, Merck, and UpToDate; and personal fees and other from Respiratory Medicine for serving as an associate editor in respiratory research, the Journal of Allergy for serving as an associate editor in case reports in medicine, and as an associate editor in US respiratory disease for the Journal of Pulmonary Respiratory Medicine, Clinical Experimental Medical Sciences, and the Journal of Allergy and Clinical Immunology: In Practice. Dr Smith reported receiving grants from the National Heart, Lung, and Blood Institute and the National Institutes of Health and other support from Merck. Dr Solway reported receiving grants from the National Heart, Lung, and Blood Institute, National Center for Advancing Translational Sciences, the National Institutes of Health, and AstraZeneca; nonfinancial support from Sunovion Pharmaceuticals Inc; personal fees from PulmOne Advanced Medical Devices, Hollister Inc, Cytokinetics Inc, Novartis Institute for Biomedical Research, and Boston Scientific; and holds US patent Nos. 6 090 618, 6 114 311, 6 284 743, 6 291 211, 6 297 221, 6 331 527, and 7 169 764. Dr Sumino reported receiving grants and speaker fees from the National Institues of Health. Dr Wechsler reported receiving grants from the National Heart, Lung, and Blood Institute; and personal fees from GlaxoSmithKline, Novartis, Cephalon/Teva, Sepracor/Sunovion, NKT Therapeutics, Asthmatx/Boston Scientific, Genzyme, MapPharma, Genentech, Boehringer Ingelheim, Merck, Regeneron, and MedImmune. Dr Wenzel reported receiving personal fees from AstraZeneca, Gilead, Boeringer Ingelheim, Teva, Sterna, and ICON Medical Imaging; grants and personal fees from GlaxoSmithKline, Amgen, Merck, and MedImmune; and grants from sanofi-aventis and Array. Dr White reported receiving grants from the National Heart, Lung, and Blood Institute and the National Institute of Allergy and Infectious Diseases; and personal fees from Boehringer Ingelheim and GlaxoSmithKline. Dr Sutherland reported being a current employee of sanofi; however, all trial-related activities were performed and completed while he was an employee of National Jewish Health.
REFERENCES
- 1.Wu AC, Tantisira K, Li L, et al. Effect of vitamin D and inhaled corticosteroid treatment on lung function in children. Am J Respir Crit Care Med. 2012;186(6):508–513. doi: 10.1164/rccm.201202-0351OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sutherland ER, Goleva E, Jackson LP, Stevens AD, Leung DY. Vitamin D levels, lung function, and steroid response in adult asthma. Am J Respir Crit Care Med. 2010;181(7):699–704. doi: 10.1164/rccm.200911-1710OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brehm JM, Schuemann B, Fuhlbrigge AL, et al. Serum vitamin D levels and severe asthma exacerbations in the Childhood Asthma Management Program study. J Allergy Clin Immunol. 2010;126(1):52–58. doi: 10.1016/j.jaci.2010.03.043. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xystrakis E, Kusumakar S, Boswell S, et al. Reversing the defective induction of IL-10-secreting regulatory T cells in glucocorticoid-resistant asthma patients. J Clin Invest. 2006;116(1):146–155. doi: 10.1172/JCI21759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nanzer AM, Chambers ES, Ryanna K, et al. Enhanced production of IL-17A in patients with severe asthma is inhibited by 1α,25-dihydroxyvitamin D3 in a glucocorticoid-independent fashion. J Allergy Clin Immunol. 2013;132(2):297–304. doi: 10.1016/j.jaci.2013.03.037. e3. [DOI] [PubMed] [Google Scholar]
- 6.Joshi S, Pantalena LC, Liu XK, et al. 1,25-dihydroxyvitamin D(3) ameliorates Th17 autoimmunity via transcriptional modulation of interleukin-17A. Mol Cell Biol. 2011;31(17):3653–3669. doi: 10.1128/MCB.05020-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poon AH, Laprise C, Lemire M, et al. Association of vitamin D receptor genetic variants with susceptibility to asthma and atopy. Am J Respir Crit Care Med. 2004;170(9):967–973. doi: 10.1164/rccm.200403-412OC. [DOI] [PubMed] [Google Scholar]
- 8.Raby BA, Lazarus R, Silverman EK, et al. Association of vitamin D receptor gene polymorphisms with childhood and adult asthma. Am J Respir Crit Care Med. 2004;170(10):1057–1065. doi: 10.1164/rccm.200404-447OC. [DOI] [PubMed] [Google Scholar]
- 9.Wittke A, Chang A, Froicu M, et al. Vitamin D receptor expression by the lung micro-environment is required for maximal induction of lung inflammation. Arch Biochem Biophys. 2007;460(2):306–313. doi: 10.1016/j.abb.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cantorna MT. Vitamin D and its role in immunology. Prog Biophys Mol Biol. 2006;92(1):60–64. doi: 10.1016/j.pbiomolbio.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 11.Banerjee A, Damera G, Bhandare R, et al. Vitamin D and glucocorticoids differentially modulate chemokine expression in human airway smooth muscle cells. Br J Pharmacol. 2008;155(1):84–92. doi: 10.1038/bjp.2008.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song Y, Qi H, Wu C. Effect of 1,25-(OH)2D3 (a vitamin D analogue) on passively sensitized human airway smooth muscle cells. Respirology. 2007;12(4):486–494. doi: 10.1111/j.1440-1843.2007.01099.x. [DOI] [PubMed] [Google Scholar]
- 13.Malmstrom K, Rodriguez-Gomez G, Guerra J, et al. Oral montelukast, inhaled beclomethasone, and placebo for chronic asthma. Ann Intern Med. 1999;130(6):487–495. doi: 10.7326/0003-4819-130-6-199903160-00005. [DOI] [PubMed] [Google Scholar]
- 14.Szefler SJ, Martin RJ, King TS, et al. Significant variability in response to inhaled corticosteroids for persistent asthma. J Allergy Clin Immunol. 2002;109(3):410–418. doi: 10.1067/mai.2002.122635. [DOI] [PubMed] [Google Scholar]
- 15.Szefler SJ, Phillips BR, Martinez FD, et al. Characterization of within-subject responses to fluticasone and montelukast in childhood asthma. J Allergy Clin Immunol. 2005;115(2):233–242. doi: 10.1016/j.jaci.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 16.Martin RJ, Szefler SJ, King TS, et al. The predicting response to inhaled corticosteroid efficacy (PRICE) trial. J Allergy Clin Immunol. 2007;119(1):73–80. doi: 10.1016/j.jaci.2006.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peters SP, Anthonisen N, Castro M, et al. Randomized comparison of strategies for reducing treatment in mild persistent asthma. N Engl J Med. 2007;356(20):2027–2039. doi: 10.1056/NEJMoa070013. [DOI] [PubMed] [Google Scholar]
- 18.Lemanske RF, Jr, Sorkness CA, Mauger EA, et al. Inhaled corticosteroid reduction and elimination in patients with persistent asthma receiving salmeterol. JAMA. 2001;285(20):2594–2603. doi: 10.1001/jama.285.20.2594. [DOI] [PubMed] [Google Scholar]
- 19.Lazarus SC, Boushey HA, Fahy JV, et al. Long-acting β2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma. JAMA. 2001;285(20):2583–2593. doi: 10.1001/jama.285.20.2583. [DOI] [PubMed] [Google Scholar]
- 20.Schatz M, Sorkness CA, Li JT, et al. Asthma Control Test. J Allergy Clin Immunol. 2006;117(3):549–556. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 21.Hyland ME, Ley A, Fisher DW, Woodward V. Measurement of psychological distress in asthma and asthma management programmes. Br J Clin Psychol. 1995;34(pt 4):601–611. doi: 10.1111/j.2044-8260.1995.tb01494.x. [DOI] [PubMed] [Google Scholar]
- 22.Reddel HK, Taylor DR, Bateman ED, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations. Am J Respir Crit Care Med. 2009;180(1):59–99. doi: 10.1164/rccm.200801-060ST. [DOI] [PubMed] [Google Scholar]
- 23.Revicki DA, Leidy NK, Brennan-Diemer F, et al. Integrating patient preferences into health outcomes assessment. Chest. 1998;114(4):998–1007. doi: 10.1378/chest.114.4.998. [DOI] [PubMed] [Google Scholar]
- 24.Bime C, Wei CY, Holbrook JT, Sockrider MM, Revicki DA, Wise RA. Asthma Symptom Utility Index. J Allergy Clin Immunol. 2012;130(5):1078–1084. doi: 10.1016/j.jaci.2012.07.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schatz M, Kosinski M, Yarlas AS, et al. The minimally important difference of the Asthma Control Test. J Allergy Clin Immunol. 2009;124(4):719–723. doi: 10.1016/j.jaci.2009.06.053. e1. [DOI] [PubMed] [Google Scholar]
- 26.Hyland ME, Ley A, Fisher DW, Woodward V. Measurement of psychological distress in asthma and asthma management programmes. Br J Clin Psychol. 1995;34(pt 4):601–611. doi: 10.1111/j.2044-8260.1995.tb01494.x. [DOI] [PubMed] [Google Scholar]
- 27.Lin D, Wei L, Yang I, Ying Z. Semiparametric regression for the mean and rate functions of recurrent events. J Royal Stat Soc Series B. 2000;62:711–730. [Google Scholar]
- 28.Drazen JM, O’Byrne PM. Risks of long-acting beta-agonists in achieving asthma control. N Engl J Med. 2009;360(16):1671–1672. doi: 10.1056/NEJMe0902057. [DOI] [PubMed] [Google Scholar]
- 29.Wise RA, Anzueto A, Cotton D, et al. Tiotropium Respimat inhaler and the risk of death in COPD. N Engl J Med. 2013;369(16):1491–1501. doi: 10.1056/NEJMoa1303342. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.