Abstract
Background
Trauma centers are an effective but costly element of the US health care infrastructure. Some level I and II trauma centers regularly incur financial losses when these high fixed costs are coupled with high burdens of uncompensated care for disproportionately young and uninsured trauma patients. As a result, they are at risk of reducing their services or closing. The impact of these closures on patient outcomes, however, has not been previously assessed.
Methods
We performed a retrospective study of all adult patient visits for injuries at Level I and II, non-federal trauma centers in California between 1999–2009. Within this population, we compared the in-hospital mortality of patients whose drive time to their nearest trauma center increased as the result of a nearby closure to those whose drive time did not increase using a multivariate logit-linked generalized linear model. Our sensitivity analysis tested whether this effect was limited to a two-year period following a closure.
Results
The odds of inpatient mortality increased by 21%(OR 1.21, 95% CI 1.04–1.40) among trauma patients who experienced an increased drive time to their nearest trauma center as a result of a closure. The sensitivity analyses showed an even larger effect in the two years immediately following a closure, during which patients with increased drive time had 29% higher odds of inpatient death (OR 1.29, 95% CI 1.11, 1.51).
Conclusions
Our results show a strong association between closure of trauma centers in California and increased mortality for patients with injuries who have to travel further for definitive trauma care. These adverse impacts were intensified within two years of a closure.
Level of Evidence
Level III, Prognostic and Epidemiological
Background
Unintentional injuries are the leading cause of death among Americans aged 1–44, accounting for 29.5 million emergency department (ED) visits,1,2 and two thirds of all injury deaths in 2009.1 Studies have documented a 25% decrease in mortality among severely injured patients treated at trauma centers (TCs) compared to those treated in non-TC hospitals.3,4 Although many members of the public do not recognize the difference between a TC and a hospital ED,5 trauma centers are especially staffed and equipped to provide surgical and non-operative care to the most severely injured, and are regularly inspected and verified as such by the American College of Surgeons (ACS) or state agencies.
Providing the highly specialized services of a trauma center does not come without cost; one survey-based study estimated the annual cost of readiness per TC at $2.7 million.6 The high fixed costs of trauma centers, coupled with low rates of reimbursement from uninsured and under-insured patients, create financial pressures that sometimes lead to closure.7–9
Due to rising numbers of uninsured and under-insured patients, coupled with falling levels of public support, many trauma centers are struggling to keep their doors open.8,10,11 The trend is not new. In fact, trauma center closures have been accelerating over the past two decades; between 1999 and 2005, 390 of the 1,125 US trauma centers (30%) closed.9,10,12
The Institute of Medicine (IOM), among other organizations, has voiced concern that closure of safety net facilities such as trauma centers may adversely affect patient care.13,14 Given the link between time to definitive care and survival in trauma patients,15,16 trauma center closures could logically lead to worse outcomes for patients with injuries. In 2006, Buchmueller et al. reported that the wave of hospital closures in Los Angeles County between 1997–2003 increased distance to care for large numbers of patients, and the increase was associated with a higher rate of mortality from unintentional injury.17 It is not known, however, whether the closure of trauma centers specifically produces similar effects, and if so, whether it is evident in a larger geographic area than a single county.
To determine whether trauma center closures adversely affect inpatient mortality, we performed a retrospective cohort study of all adult injury admissions to Level I and II non-federal trauma centers in California between January 1, 1999 and December 31, 2009, a period when three (11%)level I and II trauma centers closed their doors in the state.
Methods
Data Sources
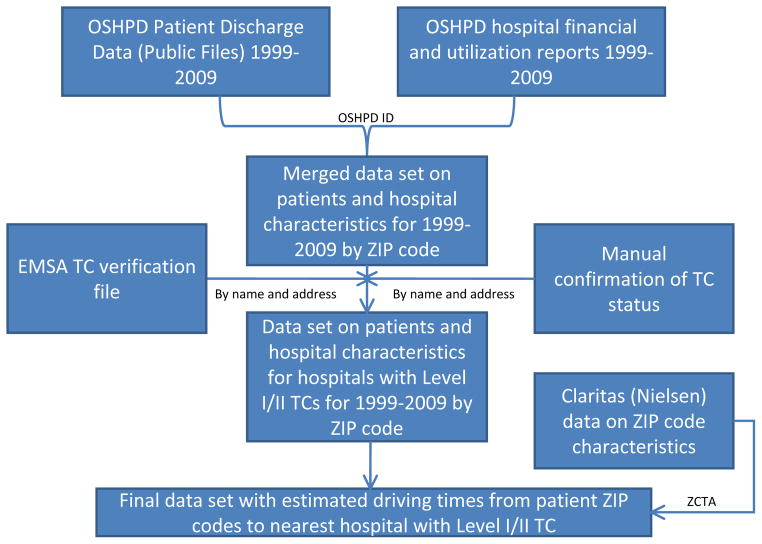
To examine the relationship between TC closures and inpatient mortality, we combined several datasets (Figure 1). We used data from the California Emergency Medical Services Authority,18 to determine which adult TCs were open as of January 1, 1999 and confirm closures that happened between then and December 31, 2009.
Figure 1.
Data sources
For the patient database we used the publicly available California Office of Statewide Health Planning and Development (OSHPD) patient discharge database (PDD) for the years of 1999–2009. Our key variable from this data was patient ZIP code, which was used to compute the distance to the patient’s nearest TC. These records also contained patient-level demographics and clinical information such as date of admission, discharge diagnosis (primary and up to 24 secondary), and disposition (including in-hospital death).
We merged the PDD with the OSHPD 1999–2009 hospital financial and utilization reports using OSHPD’s unique hospital ID. We also incorporated ZIP code-level median household income using a demographic database by Claritas (Nielsen, Claritas, NY) for 2004 to account for socioeconomic neighborhood effects.
Patient Population
We defined adult patients with acute trauma as those age20 or older with ICD-9 diagnosis codes 800–904.9, 910–929.9, and 950–959.9 in either the principal or any of the 24 secondary diagnoses, as outlined in previous literature, excluding visits with ICD-9 codes indicating drowning, bites and stings, overexertion, poisonings, foreign body, suffocation, or late effects of injury, as well as those with a sole traumatic ICD-9 diagnosis of strains and sprains, or contusions with intact skin surface.19,20 We also excluded patients with isolated hip fractures (ICD-9 codes 820–820.9; ISS=9),21 as there is no evidence that they benefit from TC care. In addition, we excluded patients with missing e-codes, without which we could not reliably determine the mechanism of injury that we adjusted for in our models. To further exclude very minor injuries, we excluded those patients who had a calculated injury severity score of zero. In addition, we excluded patients with burn injuries because in California, burn victims are treated at specialized burn centers. Moreover, we eliminated scheduled and elective admissions, since these patients would be less affected by longer drive times. We also excluded patients who were not taken to their nearest TC, as our goal was to evaluate how changes in drive time to the nearest TC affected outcomes for those who received care in those facilities. Finally, we excluded patients who lived in ZIP codes greater than 100 miles away from the nearest TC as well as out of state patients, as done previously.22
Predictor
In this study, our key variable of interest was each patient’s estimated time to their nearest TC and more specifically, whether patients resided in locations where the drive time to the nearest TC increased during the study period as a result of trauma center closure or decreased as a result of an opening. We first used the latitude and longitude coordinates of each TC’s physical address or heliport to calculate the straight-line distance between the population-weighted central location of each ZIP code and the nearest TC. The straight-line distance is highly correlated with actual driving distance, and has been used in previous literature.23,24 We computed these distances separately for each year, and computed the change in distance between each year and the base year of 1999 for each ZIP code. To provide clarity in presenting the multivariate results, we translated changes in distance to changes in drive time, using the formula developed by Phibbs and Luft.24,25 Since we specifically used changes in drive time as our predictor, we did not add in the constant time to response by the ambulance and scene time used in other studies,26,27 because it would not change our results.
Outcome
The outcome variable in our models was in-hospital mortality due to acute trauma or its complications.
Covariates
We adjusted for several potential confounders in each of our models, including patient age (categorized as 20–44 years, 45–64, 65–74, 75–84, and 85+ years), gender, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and other), insurance status (uninsured, Medicaid, Medicare, privately insured, and other). We also included income, which is known to be associated with trauma mortality,28 using the median household income of the patient ZIP code. For comorbidity adjustment, we used Elixhauser29 categorizations (Distribution of Elixhauser comorbidities in Supplemental Digital Content Table 1; Regression results for comorbitdities in Supplemental Digital Content Table 2).
To control for severity of injury, we calculated Injury Severity Score (ISS) using ICD-9 codes with software by Tri-Analytics (Bel Air, Maryland),30 and stratified the patient according to previously suggested categories of mild (ISS 1–4) moderate (ISS 5–15), and severe (ISS>15).4 We also included mechanism of injury based on e-codes, categorized into penetrating injury, falls, burns, motor vehicle crashes, and other.31
In a small number of cases, certain covariates were masked by OSHPD to protect patient identities. To compensate for this, we incorporated masked data as separate categories for each variable (cf. Table 1 for the proportion of masked variables). We also included hospital-level characteristics that have been shown to be associated with access to TCs and mortality, including whether or not there is a TC available within a patient’s county, urbanicity, and case-mix adjustment for patient severity.19,32 Finally, we included year as a covariate to account for secular trends in trauma care.
Table 1.
Distribution of patient and hospital characteristics by change in drive timea
| No increase in drive
time N=266,023 |
Increase in drive
time N=5,122 |
p-valueb | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
|
Gender
| |||||
| Male | 138353 | 52.0 | 3024 | 59.0 | <0.01 |
| Female | 89176 | 33.5 | 1332 | 26.0 | |
| (Masked) | 38494 | 14.5 | 766 | 15.0 | |
|
| |||||
|
Age Category
| |||||
| 20–44 years | 109591 | 41.2 | 2488 | 48.6 | <0.01 |
| 45–64 years | 59909 | 22.5 | 1325 | 25.9 | |
| 65–74 years | 20445 | 7.7 | 371 | 7.2 | |
| 75–84 years | 29357 | 11.0 | 266 | 5.2 | |
| > 85 years | 24110 | 9.1 | 208 | 4.1 | |
| (Masked) | 22611 | 8.5 | 464 | 9.1 | |
|
| |||||
|
Race/Ethnicity
| |||||
| Non-Hispanic White | 113550 | 42.7 | 845 | 16.5 | <0.01 |
| Black | 14216 | 5.3 | 471 | 9.2 | |
| Hispanic | 46606 | 17.5 | 1853 | 36.2 | |
| Other (Asian, Pacific Islander, Native American) | 7609 | 2.9 | 232 | 4.5 | |
| (Masked) | 84042 | 31.6 | 1721 | 33.6 | |
|
| |||||
|
Insurance
| |||||
| Medicare | 75665 | 28.4 | 936 | 18.3 | <0.01 |
| Medi-Cal | 38931 | 14.6 | 1081 | 21.1 | |
| Private | 69055 | 26.0 | 1641 | 32.0 | |
| Uninsured | 63752 | 24.0 | 1641 | 32.0 | |
| Other | 18620 | 7.0 | 457 | 8.9 | |
|
| |||||
|
Mechanism of Injury
| |||||
| Penetrating injury | 32874 | 12.4 | 866 | 16.9 | <0.01 |
| Falls | 102419 | 38.5 | 1526 | 29.8 | |
| Burns | 300 | 0.1 | 9 | 0.2 | |
| MVC | 85831 | 32.3 | 1838 | 35.9 | |
| Other | 44599 | 16.8 | 883 | 17.3 | |
|
| |||||
|
Year
| |||||
| 1999 | 18911 | 7.1 | 0 | 0.0 | <0.01 |
| 2000 | 20836 | 7.8 | 0 | 0.0 | |
| 2001 | 23069 | 8.7 | 0 | 0.0 | |
| 2002 | 24794 | 9.3 | 0 | 0.0 | |
| 2003 | 25706 | 9.7 | 0 | 0.0 | |
| 2004 | 26118 | 9.8 | 0 | 0.0 | |
| 2005 | 26485 | 10.0 | 445 | 8.7 | |
| 2006 | 26028 | 9.8 | 375 | 7.3 | |
| 2007 | 22965 | 8.6 | 1389 | 27.1 | |
| 2008 | 24959 | 9.4 | 1456 | 28.4 | |
| 2009 | 26152 | 9.8 | 1457 | 28.5 | |
|
| |||||
|
ISS severity
| |||||
| Mild | 62754 | 23.6 | 1470 | 28.7 | <0.01 |
| Moderate | 34059 | 12.8 | 920 | 18.0 | |
| Severe | 169210 | 63.6 | 2732 | 53.3 | |
|
| |||||
|
Median household income
| |||||
| $14999 – 35599 | 66031 | 24.8 | 2007 | 39.2 | <0.01 |
| $35600 – 48709 | 66178 | 24.9 | 1380 | 26.9 | |
| $48710 – 65453 | 68614 | 25.8 | 311 | 6.1 | |
| >$65454 | 65200 | 24.5 | 1424 | 27.8 | |
|
| |||||
| Trauma center in county | 238514 | 89.7 | 4433 | 86.6 | <0.01 |
|
| |||||
|
Beale categories (urbanicity)
| |||||
| 1 (most urban) | 218787 | 82.2 | 3103 | 60.6 | <0.01 |
| 2 (next urban) | 34252 | 12.9 | 1735 | 33.9 | |
| 3 (next) | 10042 | 3.8 | 284 | 5.5 | |
| 4 (middle) | 1772 | 0.7 | 0 | 0.0 | |
| 5 (rural) | 146 | 0.1 | 0 | 0.0 | |
| 6 (rural) | 510 | 0.2 | 0 | 0.0 | |
| 7 (most rural) | 514 | 0.2 | 0 | 0.0 | |
|
| |||||
|
Case mix index
| |||||
| 1st quartile (0.87–1.09) | 65413 | 24.6 | 2522 | 49.2 | <0.01 |
| 2nd quartile (1.09–1.20) | 66150 | 24.9 | 592 | 11.6 | |
| 3rd quartile (1.20–1.34) | 67300 | 25.3 | 1816 | 35.5 | |
| 4th quartile (>1.34) | 67160 | 25.3 | 192 | 3.8 | |
|
| |||||
| Mortality | 8982 | 3.4 | 205 | 4.0 | 0.014 |
|
| |||||
| Case mix index mean (SD) | 1.24 | 0.2 | 1.11 | 0.1 | <0.01 |
|
| |||||
| LOS mean (SD) | 5.3 | 7.7 | 5.7 | 9.0 | <0.01 |
Comorbidities included in Supplemental Digital Content Table 1
p-value for chi-square (categorical variables), difference in proportion (binary variables), or means (continuous variables) test.
Statistical Analysis
We used a generalized linear model framework with a log it link to determine the odds of death from injury at a TC for patients living in a specific ZIP code as a function of the change in drive time to the nearest Level I or II trauma center relative to the baseline year (1999). We used generalized estimating equations with clustering at the ZIP code level to accommodate the hierarchical nature of the dataset.
In our primary model, the treatment group consisted of all adult trauma patients who experienced an increase in drive time relative to 1999, whereas the control group consisted of all adult patients who did not. Our secondary analysis compared patients in ZIP codes that experienced (1) a decrease in drive time, (2) no change in drive time, and (3) an increase in drive time. Finally, to determine if the negative impact of TC closures is only temporary as nearby TCs adapt to increasing demand, we conducted sensitivity analyses with both our primary and secondary models to include only patients within two years of experiencing a change in driving distance to their nearest TC, based on the effect window from literature on ED closures.22 All models were run in SAS v. 9.2 (Cary, NC).
Results
Between 1999 and 2009, three level I and II adult trauma centers (11% of the initial number of TCs) in California closed. In the same 10-year interval, 271, 145 patients in our sample received care for injuries at a California level I or II TC. Of those patients, 1.9% (n=5,122) lived in a ZIP code that had an increase in drive time to the nearest TC. Of the remaining patients, 84.2% (n=228,236) lived in a ZIP code that had no change in TC drive time, while 13.9 % (n=37,787) experienced a decrease due to the opening of a trauma center. The average drive time to the nearest TC was 47 minutes [IQR 27, 52] for patients who experienced an increase in drive time, and 34 minutes [IQR 23, 35] for those who did not (Supplemental Digital Content Table 3). Patients who faced an increase in drive time to the nearest TC relative to 1999tended to be younger, lower income, more likely to have Medi-Cal insurance, and more likely to be a member of a racial minority group than patients who did not face an increased drive time (Table 1).
After adjusting for covariates, patients who faced an increase in drive time were 21% (1.21, 95% CI 1.04, 1.40) more likely to die of trauma in a level I or II California TC than otherwise similar Californians who did not face increased drive time (Table 2). In our secondary analysis, we found that compared to patients with no change in drive time to the nearest TC, the adjusted odds of inpatient mortality were 17% lower (0.83, 95% CI 0.75–0.92) for patients who experienced a decrease in drive time, and 14% higher (1.14, 95% CI 0.98–1.33) for those who experienced an increase (Table 3).
Table 2.
Primary model – Multivariate regression of increase in drive time on inpatient mortality
| In-hospital mortality Odds Ratio (95% CI) | |
|---|---|
| Decrease or no change in drive time to nearest TC (n= 266,023, 98.1%) | ref |
|
| |
| Increase in drive time to nearest TC (n=5,122, 1.9%) | 1.21 (1.04, 1.40) |
|
| |
| COVARIATESa | |
|
| |
|
Gender
| |
| Male | 1.41 (1.33, 1.49) |
| Female | ref |
|
| |
|
Age Category
| |
| 20–44 years | ref |
| 45–64 years | 1.61 (1.50, 1.72) |
| 65–74 years | 2.11 (1.89, 2.37) |
| 75–84 years | 2.78 (1.48, 3.11) |
| > 85 years | 3.71 (3.28, 4.18) |
|
| |
|
Race/Ethnicity
| |
| Non-Hispanic White | ref |
| Black | 0.98 (0.87, 1.10) |
| Hispanic | 0.95 (0.87, 1.03) |
| Other (Asian, Pacific Islander, Native American) | 0.90 (0.77, 1.04) |
|
| |
|
Insurance
| |
| Medicare | 1.54 (1.39, 1.69) |
| Medi-Cal | 1.69 (1.54, 1.86) |
| Private | ref |
| Uninsured | 0.91 (0.82, 1.02) |
| Other | 0.74 (0.65, 0.84) |
|
| |
|
Injury category
| |
| Penetrating injury | 1.76 (1.62, 1.91) |
| Falls | ref |
| Burns | 3.63 (2.25, 5.87) |
| MVC | 0.84 (0.79, 0.91) |
| Other | 0.62 (0.57, 0.68) |
|
| |
|
ISS severity
| |
| Mild | ref |
| Moderate | 2.64 (1.23,1.37) |
| Severe | 14.01 (13.07, 15.01) |
|
| |
|
Median household income
| |
| $14999 – 35599 | 1.15 (1.05, 1.27) |
| $35600 – 48709 | 1.12 (1.03, 1.22) |
| $48710 – 65453 | 1.07 (0.99, 1.16) |
| >$65454 | ref |
|
| |
|
Trauma center in county
| |
| None | ref |
| Present | 1.04 (0.94, 1.14) |
|
| |
|
Urbanicity
| |
| Beale=1 (most urban) | ref |
| Beale=2 | 1.07 (0.96, 1.02) |
| Beale=3 | 1.07 (0.90, 1.27) |
| Beale=4 | 0.75 (0.57, 0.98) |
| Beale=5 | 0.68 (0.25, 1.86) |
| Beale=6 | 0.81 (0.47, 1.38) |
| Beale=7 (most rural) | 0.36 (0.15, 0.84) |
|
| |
|
Case mix index
| |
| 1st quartile (0.87–1.09) | ref |
| 2nd quartile (1.09–1.20) | 0.90 (0.83, 0.98) |
| 3rd quartile (1.20–1.34) | 0.90 (0.82, 0.98) |
| 4th quartile (>1.34) | 0.80 (0.74, 0.87) |
|
| |
|
Year
|
0.96 (0.95, 0.97) |
Odds ratios for patient comorbidities included in Supplemental Digital Content Table 2
Table 3.
Secondary model – Multivariate regression of increase in drive time on inpatient mortality compared with no change and decreasea
| In-hospital mortality Odds Ratio (95% CI) | |
|---|---|
| Decrease in drive time to nearest TC (n=37,787, 13.9%) | 0.83 (0.75, 0.92) |
| No change in drive time to nearest TC (n=228,236, 84.2%) | ref |
| Increase in drive time to nearest TC (n=5,122, 1.9%) | 1.14 (0.98, 1.33) |
Adjusted for all covariates shown in Table 2 and comorbidities in Supplemental Digital Content Table 2
In our sensitivity analyses limiting the affected sample to patients experiencing increased drive time within two years of a closure, we found that these adverse effects were intensified; patients whose drive time increased had 29% higher odds of inpatient mortality (OR 1.29, 95% CI, 1.11, 1.51) compared with those whose drive time did not increase (Supplemental Digital Content Table 4). Our results were robust when patients were categorized according to our secondary model; the increased drive time group had 26% higher odds of inpatient mortality (OR 1.26, 95% CI 1.06, 1.49) compared with the reference group of no change, and the reduced drive time group had16% lower odds of inpatient death (OR 0.84, 95% CI 0.76, 0.93) (Supplemental Digital Content Table 5).
Discussion
Although overall rates of trauma mortality in California declined over the study interval, we observed that patients living in ZIP codes with longer drive times as a result of trauma center closure faced 21% higher odds of dying in their nearest TC as a result of injury than those in ZIP codes with no increase in drive times. Our secondary model showed that reducing drive time to the nearest TC may be protective; the 13.9% of Californians in our sample (n=37,787) who enjoyed a net decrease in drive time to the nearest TC had 17% lower odds of dying in the TC from trauma than those with no change in drive times. Those from ZIP codes with an increase in drive time had 14% higher odds of dying in the TC compared to patients with no change in drive time.
To our knowledge, ours is the first study to investigate the direct effects of trauma center closure on the health outcomes of affected patients. Overall, past research on changes in outcomes due to trauma center closures is indirect, through anecdotal evidence33 or results of hospital closures rather than trauma centers specifically.17 In addition, while others have noted the detrimental effects of longer travel times on survival,17,34 we are the first to our knowledge to identify a positive survival benefit to lowering drive time.
Importantly, our study used as its outcome in-hospital mortality, an admittedly narrow but unambiguous outcome. Obviously, TC closures could adversely affect patients in many other ways, including inpatient morbidity and lower quality of life. The loss of a TC also puts pressure on those that remain, straining infrastructure and professional resources.35 This may compromise the care of all patients who seek care at the next available trauma center, whether or not they personally face an increase in drive time. Therefore, our findings should be considered conservative estimates of the negative effects of trauma center closure.
The implications of these findings are clear: trauma centers do definitively benefit the communities they serve. Decreased distance to these centers is associated with lower inpatient mortality, and increased distance to the nearest trauma center is associated with higher inpatient mortality. Though dedicating extensive resources for trauma care is not inexpensive, the data show that trauma centers are still cost-effective. A prospective cohort study of over 5,000 patients by MacKenzie et al found that the added cost of treatment at a level I TC was $36,319 per life year gained -- much lower than the estimated value of a year of life, which ranges between $50,000–$200,000.14 The decisions about how to sustain trauma services for all populations must be undertaken methodically and strategically, with careful attention toward equity and efficiency. Future research should clarify who is impacted most by trauma center closure and evaluate potential interventions regarding their effects on high-risk groups.
Limitations
Our study is subject to several limitations. First, some demographic variables in our public dataset were masked to protect the identity of a limited number of patients. If the masked variables disguised covariates differentially in the different drive time groups, this could affect the risk-adjustment of our main findings. However, the percentages of patients with masked variables were similar in the different groups. Therefore we doubt that masked variables affected our overall results.
Second, we only studied patients who received inpatient care at a level I or level II TC. Although this criterion should capture the most severely injured patients - who would be most affected by TC closure - a large body of literature has identified significant under-triage of trauma patients. This means that our analysis missed some severely injured patients who were affected by TC closure never reached a TC. If these patients had worse outcomes at non-TCs, their absence from our analysis would bias our results to favor the null hypothesis.
Third, though injuries most commonly occur at home,36 drive time from a patient’s home ZIP code to the nearest TC is not a perfect predictor of actual transport time from the location of injury to the nearest TC. For instance, it is possible that a patient with a home ZIP code that experienced an increase in drive time to the nearest TC was actually injured in a different location, and thus in practice was unaffected by the closure. We limited the extent of this possible misclassification by excluding patients who were not transported to the TC nearest to their home ZIP code. Further, given the paucity of large-scale data linkages between pre-hospital and hospital records, as well as the lack of any injury location records for patients who walk in, we feel that in order to understand the relationship between TC closures and mortality from a population perspective this is a necessary estimation.
Fourth, our dataset does not include patients who died in the ED. As a result, it is possible that patients who previously would have died in their nearest ED, which then closed, could have been transported to a further but higher quality TC, survived the initial resuscitation in the ED, and died as an inpatient. This would falsely inflate the odds of mortality due to closure. At the same time, however, if these patients were so severely injured as to die in the ED, it is also likely that they would have died en route to the further hospital. This competing effect significantly mitigates the potential for Type I error.
Finally, we made no effort to control for trauma center quality, which certainly affects patient outcomes. If patients in ZIP codes with longer drive times were more likely to be treated at worse TCs than those who experienced no change in drive times, this would tend to inflate our measures of risk. However, if, as it has been suggested, the three TCs that closed in California during the study period did so as a result of poor quality of care, it would tend to attenuate our findings.
Conclusions
Our findings indicate that trauma center closure, and the resulting increase in drive times to trauma care for patients, is associated with increased odds of inpatient mortality from injury. In addition, injured patients who enjoyed a decrease in drive time to their nearest trauma center had lower odds of inpatient mortality. These results present compelling data that access to trauma care matters. However, given their cost and the relationship between volume and outcomes, it is not feasible to put a trauma center on every street corner.37–40 Our findings affirm the importance of health administrators and policymakers working strategically to ensure equitable access to trauma care nationwide.
Supplementary Material
SDC Table 1. Distribution of comorbidities by change in drive time.
SDC Table 2. Association of patient comorbidities with likelihood of inpatient mortality (Primary Model).
SDC Table 3. Descriptive statistics of drive time to nearest TC for study patients.
SDC Table 4. Sensitivity Analysis with Primary model – Multivariate regression of increase in drive time (limited to 2-year period after change) on inpatient mortality
SDC Table 5. Sensitivity Analysis with Secondary model – Multivariate regression of increase in drive time (limited to 2-year period after change) on inpatient mortality compared with no change and decrease
Acknowledgments
We especially thank Olga Saynina, MS, for technical assistance, and Julia Brownell, BA for her administrative and editorial support.
Footnotes
Author Contributions:
RYH: Study design, data interpretation, writing, critical revision
TS: Study design, data analysis, data interpretation, critical revision
JM: Data analysis, data interpretation, critical revision
MC: Data interpretation, critical revision
CM: Study design, data analysis, data interpretation, critical revision
ALK: Data interpretation, critical revision
Disclosures: This publication was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number KL2 TR000143 (R.Y.H.), and the Robert Wood Johnson Foundation Physician Faculty Scholars Program (R.Y.H.). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of any of the funding agencies. No authors have any conflicts of interest to report.
Contributor Information
Renee Y. Hsia, Email: renee.hsia@emergency.ucsf.edu.
Tanja Srebotnjak, Email: tanja.srebotnjak@eius.org.
Judith Maselli, Email: jmaselli@medicine.ucsf.edu.
Marie Crandall, Email: macranda@nmh.org.
Charles McCulloch, Email: CMcCulloch@epi.ucsf.edu.
Arthur L. Kellermann, Email: Arthur_Kellermann@rand.org.
References
- 1.Kochanek K, Xu J, Murphy S, Minino A, Kung H. National Vital Statisics Reports. 3. Vol. 60. National Center for Health Statistics; 2011. Deaths: Final Data for 2009. [PubMed] [Google Scholar]
- 2.National Center for Health Statistics. National Hospital Ambulatory Medical Care Survey: 2009 Emergency Department Summary Tables. Table 16. Injury-related ED visits by intent and mechanism: United States, 2009. [Google Scholar]
- 3.Chiara O, Cimbanassi S. Organized trauma care: does volume matter and do trauma centers save lives? Curr Opin Crit Care. 2003;9:510–514. doi: 10.1097/00075198-200312000-00008. [DOI] [PubMed] [Google Scholar]
- 4.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 5.Champion HR, Mabee MS, Meredith JW. The state of US trauma systems: public perceptions versus reality--implications for US response to terrorism and mass casualty events. J Am Coll Surg. 2006;203:951–961. doi: 10.1016/j.jamcollsurg.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 6.Taheri PA, Butz DA, Lottenberg L, Clawson A, Flint LM. The cost of trauma center readiness. Am J Surg. 2004;187:7–13. doi: 10.1016/j.amjsurg.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 7.Eastman AB, Bishop GS, Walsh JC, Richardson JD, Rice CL. The economic status of trauma centers on the eve of health care reform. J Trauma. 1994;36:835–844. [PubMed] [Google Scholar]
- 8.Eastman AB, Rice CL, Bishop G, Richardson JD. An analysis of the critical problem of trauma center reimbursement. J Trauma. 1991;31:920–925. doi: 10.1097/00005373-199107000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Dailey JT, Teter H, Cowley RA. Trauma center closures: a national assessment. J Trauma. 1992;33:539–546. [PubMed] [Google Scholar]
- 10.Shen Y-C, Hsia RY, Kuzma K. Understanding the risk factors of trauma center closures: do financial pressure and community characteristics matter? Med Care. 2009;47:968–978. doi: 10.1097/MLR.0b013e31819c9415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zuckerman S, Bazzoli G, Davidoff A, LoSasso A. How did safety-net hospitals cope in the 1990s? Health Aff (Millwood) 2001;20:159–168. doi: 10.1377/hlthaff.20.4.159. [DOI] [PubMed] [Google Scholar]
- 12.Bazzoli GJ, Meersman PJ, Chan C. Factors that enhance continued trauma center participation in trauma systems. J Trauma. 1996;41:876–885. doi: 10.1097/00005373-199611000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Lewin ME, Baxter RJ. America’s health care safety net: revisiting the 2000 IOM report. Health Aff (Millwood) 2007;26:1490–1494. doi: 10.1377/hlthaff.26.5.1490. [DOI] [PubMed] [Google Scholar]
- 14.MacKenzie EJ, Weir S, Rivara FP, et al. The value of trauma center care. J Trauma. 2010;69:1–10. doi: 10.1097/TA.0b013e3181e03a21. [DOI] [PubMed] [Google Scholar]
- 15.Sampalis JS, Denis R, Lavoie A, et al. Trauma Care Regionalization: A Process-Outcome Evaluation. J Trauma. 1999;46:565–581. doi: 10.1097/00005373-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Sampalis JS, Lavoie A, Williams JI, Mulder DS, Kalina M. Impact of on-Site Care, Prehospital Time, and Level of in-Hospital Care on Survival in Severely Injured Patients. J Trauma. 1993;34:252–261. doi: 10.1097/00005373-199302000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Buchmueller TC, Jacobson M, Wold C. How far to the hospital? The effect of hospital closures on access to care. J Health Econ. 2006;25:740–761. doi: 10.1016/j.jhealeco.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 18.California Emergency Medical Services Authority. [Accessed Aug 7, 2013];2008 http://www.emsa.ca.gov/
- 19.Hsia RY, Wang E, Torres H, Saynina O, Wise PH. Disparities in trauma center access despite increasing utilization: data from California, 1999 to 2006. J Trauma. 2010;68:217–224. doi: 10.1097/TA.0b013e3181a0e66d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McLoughlin E, Annest JL, Fingerhut LA, et al. Recommended framework for presenting injury mortality data. MMWR Morb Mortal Wkly Rep. 1997;46:1–32. [PubMed] [Google Scholar]
- 21.Shinoda-Tagawa T, Clark DE. Trends in hospitalization after injury: older women are displacing young men. Injury Prevention. 2003;9:214–219. doi: 10.1136/ip.9.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shen Y-C, Hsia RY. Does decreased access to emergency departments affect patient outcomes? Analysis of AMI population 1996–2005. Health Serv Res. 2012;471:188–210. doi: 10.1111/j.1475-6773.2011.01319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Love RF, Morris JG. Mathematical models of road travel distances. Manage Sci. 1979;252:130–139. [Google Scholar]
- 24.Phibbs C, Luft H. Correlation of travel time on roads versus straight line distance. Med Care Res Rev. 1995;52:532–542. doi: 10.1177/107755879505200406. [DOI] [PubMed] [Google Scholar]
- 25.Phibbs C. [Accessed June 11, 2009];Patient Incurred Cost - How do I estimate travel costs? 2008 http://www.herc.research.va.gov/resources/faq_h02.asp.
- 26.Branas CC, MacKenzie EJ, Williams JC, et al. Access to trauma centers in the United States. JAMA. 2005;293:2626–2633. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 27.Branas CC. No time to spare: improving access to trauma care. LDI Issue Brief. 2005;11:1–4. [PubMed] [Google Scholar]
- 28.Newgard CD, Schmicker RH, Sopko G, et al. Trauma in the neighborhood: a geospatial analysis and assessment of social determinants of major injury in North America. Am J Public Health. 2011;101:669–677. doi: 10.2105/AJPH.2010.300063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Mackenzie E, Sacco WJ. ICDMAP-90 Software and Users Guide. Baltimore: Johns Hopkins University and Trianalytics; 1997. [Google Scholar]
- 31.Centers for Disease Control and Prevention. Table 1. Recommended framework of E-code groupings for presenting injury mortality and morbidity data (August 10, 2011) [Accessed December 3, 2013];Matrix of E-code Groupings. 2011 http://www.cdc.gov/injury/wisqars/ecode_matrix.html.
- 32.Hsia RY, Wang E, Saynina O, Wise P, Perez-Stable EJ, Auerbach A. Factors associated with trauma center use for elderly patients with trauma: a statewide analysis, 1999–2008. Arch Surg. 2011;146:585–592. doi: 10.1001/archsurg.2010.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Time matters when transporting critically injured to trauma centers. Rep Med Guidel Outcomes Res. 2000;11(7):7. [PubMed] [Google Scholar]
- 34.Innes G, Grafstein E, McGrogan J. Do Emergency Physicians Know the Costs of Medical Care? CJEM. 2000;2:95–102. doi: 10.1017/s148180350000467x. [DOI] [PubMed] [Google Scholar]
- 35.Acosta JA, Yang JC, Winchell RJ, et al. Lethal injuries and time to death in a level I trauma center. J Am Coll Surg. 1998;186:528–533. doi: 10.1016/s1072-7515(98)00082-9. [DOI] [PubMed] [Google Scholar]
- 36.Chen L, Warner M, Fingerhut L, Makuc D. Injury Episodes and Circumstances: National Health Interview Survey, 1997–2007. National Center for Health Statistics, Vital Health Stat. 2009:10. [PubMed] [Google Scholar]
- 37.Demetriades D, Martin M, Salim A, Rhee P, Brown C, Chan L. The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg. 2005;242(4):512–517. doi: 10.1097/01.sla.0000184169.73614.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nathens AB, Jurkovich GJ, Maier RV, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285:1164–1171. doi: 10.1001/jama.285.9.1164. [DOI] [PubMed] [Google Scholar]
- 39.Chowdhury MM, Dagash H, Pierro A. A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg. 2007;94:145–161. doi: 10.1002/bjs.5714. [DOI] [PubMed] [Google Scholar]
- 40.Thiemann DR, Coresh J, Oetgen WJ, Powe NR. The association between hospital volume and survival after acute myocardial infarction in elderly patients. N Engl J Med. 1999;340:1640–1648. doi: 10.1056/NEJM199905273402106. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SDC Table 1. Distribution of comorbidities by change in drive time.
SDC Table 2. Association of patient comorbidities with likelihood of inpatient mortality (Primary Model).
SDC Table 3. Descriptive statistics of drive time to nearest TC for study patients.
SDC Table 4. Sensitivity Analysis with Primary model – Multivariate regression of increase in drive time (limited to 2-year period after change) on inpatient mortality
SDC Table 5. Sensitivity Analysis with Secondary model – Multivariate regression of increase in drive time (limited to 2-year period after change) on inpatient mortality compared with no change and decrease