Abstract
Objectives To investigate the effects of Helicobacter pylori infection and its eradication on heartburn and gastro-oesophageal reflux.
Design Cross sectional study, followed by a randomised placebo controlled trial.
Setting Seven general practices in Bristol, England.
Participants 10 537 people, aged 20-59 years, with and without H pylori infection (determined by the 13C-urea breath test).
Main outcome measures Prevalence of heartburn and gastro-oesophageal acid reflux at baseline and two years after treatment to eradicate H pylori infection.
Results At baseline, H pylori infection was associated with increased prevalence of heartburn (odds ratio 1.14, 95% confidence interval 1.05 to 1.23) but not reflux (1.05, 0.97 to 1.14). In participants with H pylori infection, active treatment had no effect on the overall prevalence of heartburn (0.99, 0.88 to 1.12) or reflux (1.04, 0.91 to 1.19) and did not improve pre-existing symptoms of heartburn or reflux.
Conclusions H pylori infection is associated with a slightly increased prevalence of heartburn but not reflux. Treatment to eradicate H pylori has no net benefit in patients with heartburn or gastro-oesophageal reflux.
Introduction
Infection with Helicobacter pylori usually causes antral gastritis, with increased acid secretion and risk of duodenal ulcer.1,2 Pangastritis sometimes occurs, with a net suppression of acid secretion.2 Eradication of the infection might therefore result in variable effects on acid related symptoms.
An increase in reflux oesophagitis after treatment to eradicate H pylori was first reported in 1991.3 Later studies, with varying methods, have produced conflicting results; some showed an increase or unmasking of reflux oesophagitis,4-6 others reported no effect,7-9 and some even found a benefit.10-13
Randomised controlled trials generally provide more reliable information than observational studies. We carried out a large community based study of the effects of H pylori infection on heartburn and acid reflux.
Methods
This study was part of a large trial of the effects of H pylori infection and its eradication on the symptoms, treatment, and costs of dyspepsia in the community—the Bristol helicobacter project.14 All people aged 20-59 years registered with seven general practices in northeast Bristol (total 26 203) were invited to participate. Of these, 10 537 (40.2%) gave informed consent to take part in the study and had a 13C-urea breath test for active H pylori infection administered by using an orange juice and citric acid test meal.14,15
All participants completed a validated questionnaire describing the frequency and severity of any epigastric pain, heartburn, and gastro-oesophageal reflux. Details are described in the methods paper for the Bristol helicobacter project.14 We compared the symptoms of all 1634 participants whose 13C-urea breath test was positive for H pylori infection with those of twice that number (3268) of randomly selected H pylori negative controls (total 4902).
We randomised participants whose 13C-urea breath test showed H pylori infection in equal numbers to receive 500 mg clarithromycin and 400 mg ranitidine bismuth citrate twice daily for two weeks or placebo. The 13C-urea breath test was repeated six months later, but the results were not revealed until after the two year follow up. We recorded consultations with the general practitioner for dyspepsia after scrutiny of the participants' primary care notes.
We used SPSS version 10 to do the statistical analysis. We analysed symptoms two years after treatment on an intention to treat basis.
Results
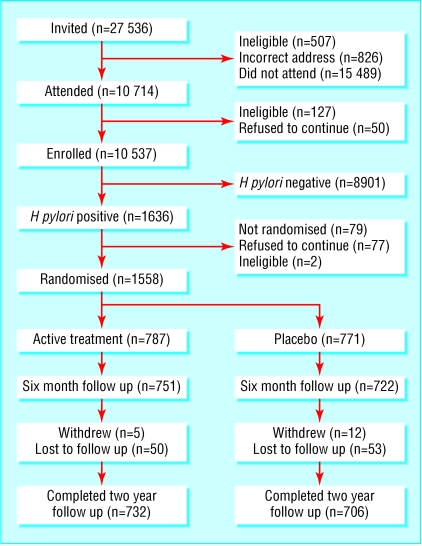
Of the 10 537 participants who had a 13C-urea breath test, 1634 (15.5%) were positive for H pylori infection (figure). Of those with a positive test result, 1558 (95.3%) were randomised to receive either active treatment (787) or placebo (771). The characteristics of the two groups were similar (table 1).
Figure 1.
Trial profile
Table 1.
Baseline characteristics of two groups of participants with Helicobacter pylori infection who entered the prospective double blind study. Values are numbers (percentages)
| Characteristic | Active treatment (n=787) | Placebo treatment (n=771) |
|---|---|---|
| Age (years): | ||
| <40 | 120 (15.2) | 110 (14.3) |
| 41-54 | 452 (57.5) | 451 (58.5) |
| ≥55 | 215 (27.3) | 210 (27.2) |
| Sex: | ||
| Male | 385 (48.9) | 378 (49.0) |
| Female | 402 (51.1) | 393 (51.0) |
| Lifestyle: | ||
| Smoking | ||
| never | 405/767 (52.8) | 389/764 (50.9) |
| past | 179/767 (23.3) | 190/764 (24.9) |
| current | 183/767 (23.9) | 185/764 (24.2) |
| Alcohol consumption* | 140 (17.8) | 195 (25.3) |
| NSAIDs (any in past 3 months) | 177/732 (24.2) | 191/720 (26.5) |
| BMI >30 kg/m2 | 221 (28.1) | 195 (25.3) |
| Pretreatment symptoms†: | ||
| Any epigastric pain | 298/760 (39.2) | 302/730 (41.4) |
| Monthly epigastric pain | 185/760 (24.3) | 194/730 (26.6) |
| Any heartburn | 378/756 (50.0) | 368/734 (50.1) |
| Monthly heartburn | 213/756 (28.2) | 202/734 (27.5) |
| Any acid reflux | 301/760 (39.6) | 298/732 (40.7) |
| Monthly acid reflux | 144/760 (18.9) | 133/732 (18.2) |
NSAID=non-steroidal anti-inflammatory drug; BMI=body mass index.
The slight differences in the denominators are due to incomplete data for some participants.
Current alcohol intake at least one unit per week.
Any=any in past three months; monthly=at least once in past month.
Six months after treatment, the 13C-urea breath test was negative in 659/727 (90.7%) of participants after active treatment (60 non-attenders) and in 99/706 (14.0%) of those given placebo (65 non-attenders). Two year follow up was complete in 1433/1558 (92.0%) participants. The unexpectedly high apparent loss of H pylori infection in the placebo group was mainly due to our use of δ3.5 rather than δ5.0 as a cut-off point to define infection in the 13C-urea breath test. In 75 of the 99 instances of apparent eradication by placebo, the initial breath test reading was between δ3.5 and δ5.0. Such participants probably never had H pylori infection.
H pylori infection was associated with a small difference in the prevalence of heartburn (“any heartburn in the past month” 28.1% v 25.2%, χ2 = 4.51, P = 0.034) (table 2), but not gastro-oesophageal reflux (“any reflux in the past month” 18.6% v 17.4%, χ2 = 1.0, P = 0.32) (table 3).
Table 2.
Effect of Helicobacter pylori infection on prevalence of heartburn. Values are numbers (percentages) unless stated otherwise
| Frequency of heartburn | H pylori infection (n=1560)* | No infection (n=3164)* | Unadjusted odds ratio (95% CI) for H pylori positive participants |
|---|---|---|---|
| Any in past three months | 781 (50.1) | 1490 (47.1) | 1.14 (1.05 to 1.23) |
| At least monthly | 438 (28.1) | 797 (25.2) | 1.21 (1.11 to 1.32) |
Incomplete data for 178/4902 (3.6%) participants.
Table 3.
Effect of Helicobacter pylori infection on prevalence of acid reflux. Values are numbers (percentages) unless stated otherwise
| Frequency of reflux | H pylori infection (n=1566)* | No infection (n=3167)* | Unadjusted odds ratio (95% CI) for H pylori positive participants |
|---|---|---|---|
| Any in past three months | 627 (40.0) | 1184 (37.4) | 1.05 (0.97 to 1.14) |
| At least monthly | 291 (18.6) | 551 (17.4) | 1.05 (0.95 to 1.17) |
Incomplete data for 178/4902 (3.6%) participants.
Heartburn was significantly associated with epigastric pain, acid reflux, obesity, regular consumption of non-steroidal anti-inflammatory drugs or proton pump inhibitors, smoking, and chest pain induced by exercise (table 4). Age, sex, alcohol intake, and socioeconomic status were not risk factors for heartburn.
Table 4.
Factors associated with a significantly increased risk of heartburn. Values are numbers (percentages) unless stated otherwise
|
Heartburn
|
Unadjusted odds ratio (95% CI)
|
||
|---|---|---|---|
| Factor | No | Yes | |
| Epigastric pain*: | |||
| No | 3085 (88.2) | 411 (37.2) | 1.0 |
| Yes | 423 (11.8) | 714 (62.8) | 12.67 (10.54 to 15.28) |
| Acid reflux*: | |||
| No | 3201 (93.3) | 623 (51.4) | 1.0 |
| Yes | 231 (6.7) | 590 (48.6) | 7.25 (6.29 to 8.26) |
| Use of proton pump inhibitor: | |||
| No | 3443 (98.3) | 984 (87.9) | 1.0 |
| Yes | 59 (1.7) | 136 (12.1) | 8.07 (5.85 to 11.13) |
| Non-steroidal anti-inflammatory drugs:
|
|
|
|
| <1/month | 2906 (84.2) | 825 (76.7) | 1.0 |
| ≥1/month | 545 (15.8) | 251 (23.3) | 1.62 (1.37 to 1.92) |
| Obesity†: | |||
| No | 2902 (81.8) | 644 (70.4) | 1.0 |
| Yes | 817 (18.2) | 343 (29.6) | 1.89 (1.31 to 2.21) |
| Chest pain on exertion: | |||
| No | 3512 (98.9) | 1115 (96.0) | 1.0 |
| Yes | 41 (1.2) | 47 (4.0) | 3.61 (2.36 to 5.53) |
| Smoking: | |||
| Never | 1421 (48.3) | 303 (32.5) | 1.0 |
| Ever | 1521 (51.7) | 629 (67.5) | 1.94 (1.66 to 2.27) |
Age over 50, sex, alcohol intake, and socioeconomic status were not risk factors for heartburn.
At least monthly.
Body mass index ≥30.0 kg/m2.
H pylori eradication treatment had no significant effect on the prevalence of either heartburn (odds ratio 0.99, 95% confidence interval 0.88 to 1.12) or gastro-oesophageal reflux (1.04, 0.91 to 1.19) two years after treatment (table 5). Treatment had no impact on the development of heartburn (0.90, 0.78 to 1.04) or reflux (1.05, 0.90 to 1.21) in previously asymptomatic participants. In participants who had these symptoms at baseline, no significant improvement occurred in either heartburn (0.90, 0.71 to 1.14) or reflux (0.89, 0.62 to 1.29).
Table 5.
Effect of Helicobacter pylori eradication treatment on prevalence of heartburn and reflux at two years. Values are numbers (percentages) unless stated otherwise
| Measure | Placebo (n=787) | Active treatment (n=771) | Unadjusted odds ratio (95% CI) for active treatment |
|---|---|---|---|
| Prevalence of heartburn* (n=1410) | 170/702 (24.2) | 169/708 (23.9) | 0.99 (0.88 to 1.12) |
| Prevalence of reflux† (n=1419) | 124/704 (17.6) | 135/715 (18.9) | 1.04 (0.91 to 1.19) |
Defined as heartburn at least once a month.
Defined as reflux at least once a month.
In those participants who had gastro-oesophageal reflux without heartburn before treatment (n = 248), H pylori eradication treatment had a protective effect against the development of heartburn over the two year period (0.56, 0.35 to 0.90). The number of general practice consultations for heartburn or reflux over the two years after active treatment was not significantly greater than after placebo (1.63, 0.94 to 2.87).
Discussion
The most obvious mechanism by which H pylori infection might affect reflux oesophagitis is by affecting secretion of gastric acid. H pylori infection usually causes a predominantly antral gastritis, which results in a net increase in acid secretion.16 In people with an incompetent antireflux mechanism, this would increase exposure of the lower oesophagus to acid, increasing the prevalence of heartburn.4,5 Our findings that H pylori is associated with an increased prevalence of heartburn and that H pylori eradication treatment reduces the risk of patients with acid reflux developing heartburn support this hypothesis. Acid reflux depends more on the integrity of the lower oesophageal sphincter, hence the insignificant effect of H pylori infection on reflux. Patients with severe reflux oesophagitis are less likely to have H pylori infection,17-26 possibly because corpus gastritis caused by helicobacter infection limits maximum acid output in these patients,27-32 thus protecting them against the more severe forms of reflux oesophagitis. Such people might theoretically be at risk of increased exposure of the lower oesophagus to acid after eradication of H pylori infection.29,31 However, our study suggests that no significant worsening of heartburn or reflux occurs after eradication of H pylori in patients in the community.
Our study has weaknesses. As it was community based, we had no direct information (from endoscopy, for example) as to the actual pathology underlying the symptoms of our participants. The randomised double blind design, the large numbers of participants, the high rate of H pylori eradication, the avoidance of prolonged acid suppression as part of the treatment, and the length and completeness of the two year period of follow up are compensating strengths.
What is already known on this topic
Heartburn and gastro-oesophageal reflux are common symptoms in the population
Helicobacter pylori gastritis is also very common and might influence these symptoms by altering gastric acid secretion
Previous studies have reached differing conclusions about the effect of H pylori eradication on gastro-oesophageal reflux disease
What this study adds
In a general practice population, people with Helicobacter pylori infection had a slightly higher prevalence of heartburn (but not reflux) than other people
Helicobacter pylori eradication had no net effect on symptoms of gastro-oesophageal reflux disease
We thank the participants in the Bristol helicobacter project and the general practitioners and health centre staff; the nursing team of Lynne Bradshaw, Julie Watson, Tina Critchley, Jo Lee, Carol Everson-Coombe, Penny Nettlefield, and Joanne Smith; Judy Millward, Helen Davies, Amy Hawkins, and Sarah Pike for secretarial support; and Erwin Brown, Paul Thomas, Nick Pope, and Phil Hedges of the microbiology department and Peter Spurr, Martin Bullock, and Fiona Greenwood of the pharmacy department, Frenchay Hospital, for help with the breath tests.
Contributors: RFH initiated the study, helped to plan the project, analysed the results, wrote the initial draft of the paper, and is the guarantor. JAL ran the Bristol helicobacter project from day to day and helped with analysis of the data and the final version of the paper. PN helped to set up the project. LJM, IMH, and JLD helped to plan the project, analyse the results, and produce the final version of the paper.
Funding: This study was funded jointly by the NHS South and West Regional Research and Development Directorate and GlaxoSmithKline UK. The Department of Social Medicine is the lead centre for the MRC Health Services Research Collaboration.
Competing interests: RFH and JAL were reimbursed by GlaxoSmithKline for attending the AGA symposium in 2000.
Ethical approval: The local research ethics committee approved the study.
References
- 1.Tarpila S, Kekki M, Samloff IM, Sipponen P, Siurala M. Morphology and dynamics of the gastric mucosa in duodenal ulcer patients and their first-degree relatives. Hepatogastroenterology 1983;30: 198-201. [PubMed] [Google Scholar]
- 2.Calam J. Clinicians' guide to Helicobacter pylori. London: Chapman & Hall Medical, 1996: 39-77.
- 3.Labenz J, Blum AL, Bayerdorffer E, Meining A, Stolte M, Borsch G. Curing Helicobacter pylori infection in patients with duodenal ulcer may provoke reflux esophagitis. Gastroenterology 1997;112: 1442-7. [DOI] [PubMed] [Google Scholar]
- 4.Hamada H, Haruma K, Mihara M, Kamada T, Yoshihara M, Sumii K, et al. High incidence of reflux oesophagitis after eradication therapy for Helicobacter pylori: impacts of hiatal hernia and corpus gastritis. Aliment Pharmacol Ther 2000;14: 729-35. [DOI] [PubMed] [Google Scholar]
- 5.Manes G, Mosca S, De Nucci C, Lombardi G, Lioniello M, Balzano A. High prevalence of reflux symptoms in duodenal ulcer patients who develop gastro-oesophageal reflux disease after curing Helicobacter pylori infection. Dig Liver Dis 2001;33: 665-70. [DOI] [PubMed] [Google Scholar]
- 6.Veldhuyzen van Zanten SJ. Treatment of Helicobacter pylori infection unmasks rather than induces symptoms of gastro-oesophageal reflux disease. Dig Liver Dis 2001;33: 647-8. [DOI] [PubMed] [Google Scholar]
- 7.Befrits R, Sjostedt S, Odman B, Sorngard H, Lindberg G. Curing Helicobacter pylori infection in patients with duodenal ulcer does not provoke gastroesophageal reflux disease. Helicobacter 2000;5: 202-5. [DOI] [PubMed] [Google Scholar]
- 8.Moayyedi P, Bardhan C, Young L, Dixon MF, Brown L, Axon AT. Helicobacter pylori eradication does not exacerbate reflux symptoms in gastroesophageal reflux disease. Gastroenterology 2001;121: 1120-6. [DOI] [PubMed] [Google Scholar]
- 9.Laine L, Sugg J. Effect of Helicobacter pylori eradication on development of erosive esophagitis and gastroesophageal reflux disease symptoms: a post hoc analysis of eight double blind prospective studies. Am J Gastroenterol 2002;97: 2992-7. [DOI] [PubMed] [Google Scholar]
- 10.Schwizer W, Thumshirn M, Dent J, Guldenschuh I, Menne D, Cathomas G, et al. Helicobacter pylori and symptomatic relapse of gastro-oesophageal reflux disease: a randomised controlled trial. Lancet 2001;357: 1738-42. [DOI] [PubMed] [Google Scholar]
- 11.Stuart RC, Craig CF, Morran C, Burns H, Harden K, Power A, et al. A beneficial effect of H. pylori eradication in reflux patients in the community. Gastroenterology 2001;120(suppl 1): A48. [Google Scholar]
- 12.Moayyedi P, Feltbower R, Brown J, Mason S, Mason J, Nathan J, et al. Effect of population screening and treatment for Helicobacter pylori on dyspepsia and quality of life in the community: a randomized controlled trial. Lancet 2000;355: 1665-9. [DOI] [PubMed] [Google Scholar]
- 13.Wildner-Christensen M, Moller Hansen J, Schaffalitzky de Muckadell OB. Rates of dyspepsia one year after Helicobacter pylori screening and eradication in a Danish population. Gastroenterology 2003;125: 372-9. [DOI] [PubMed] [Google Scholar]
- 14.Lane JA, Harvey RF, Murray L, Harvey IM, Nair P, Egger M, et al. A placebo-controlled randomized trial of eradication of Helicobacter pylori in the general population: study design and response rates of the Bristol helicobacter project. Control Clin Trials 2002;23: 321-32. [DOI] [PubMed] [Google Scholar]
- 15.Dominguez-Munoz JE, Leodolter A, Sauerbruch T, Malfertheiner P. A citric acid solution is an optimal test drink in the 13C-urea breath test for Helicobacter pylori infection. Gut 1997;40: 459-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El Omar EM, Penman ID, Ardill JE, Chittajallu RS, Howie C, McColl KE. Helicobacter pylori infection and abnormalities of acid secretion in patients with duodenal ulcer disease. Gastroenterology 1995;109: 681-91. [DOI] [PubMed] [Google Scholar]
- 17.Koike T, Ohara S, Sekine H, Iijima K, Kato K, Shimosegawa T, et al. Helicobacter pylori infection inhibits reflux esophagitis by inducing atrophic gastritis. Am J Gastroenterol 1999;94: 3468-72. [DOI] [PubMed] [Google Scholar]
- 18.Haruma K, Hamada H, Mihara M, Kamada T, Yoshihara M, Sumii K, et al. Negative association between Helicobacter pylori infection and reflux esophagitis in older patients: case-control study in Japan. Helicobacter 2000;5: 24-9. [DOI] [PubMed] [Google Scholar]
- 19.Labenz J, Jaspersen D, Kulig M, Leodolter A, Lind T, Lindner D, et al. Risk factors for the development of erosive reflux disease: a multivariate analysis based on the proGERD initiative. Gastroenterology 2002; W1163.
- 20.Shirota T, Kusano M, Kawamura O, Horikoshi T, Mori M, Sekiguchi T. Helicobacter pylori infection correlates with severity of reflux esophagitis: with manometry findings. J Gastroenterol 1999;34: 553-9. [DOI] [PubMed] [Google Scholar]
- 21.Varanasi RV, Fantry GT, Wilson KT. Decreased prevalence of Helicobacter pylori infection in gastroesophageal reflux disease. Helicobacter 1998;3: 188-94. [DOI] [PubMed] [Google Scholar]
- 22.Werdmuller BF, Loffeld RJ. Helicobacter pylori infection has no role in the pathogenesis of reflux esophagitis. Dig Dis Sci 1997;42: 103-5. [DOI] [PubMed] [Google Scholar]
- 23.Weston AP, Badr AS, Topalovski M, Cherian R, Dixon A, Hassanein RS. Prospective evaluation of the prevalence of gastric Helicobacter pylori infection in patients with GERD, Barrett's esophagus, Barrett's dysplasia, and Barrett's adenocarcinoma. Am J Gastroenterol 2000;95: 387-94. [DOI] [PubMed] [Google Scholar]
- 24.Loffeld RJ, Werdmuller BF, Kuster JG, Perez-Perez GI, Blaser MJ, Kuipers EJ. Colonization with cagA-positive Helicobacter pylori strains inversely associated with reflux esophagitis and Barrett's esophagus. Digestion 2000;62: 95-9. [DOI] [PubMed] [Google Scholar]
- 25.Warburton-Timms VJ, Charlett A, Valori RM, Uff JS, Shepherd NA, Barr H, et al. The significance of cagA+ Helicobacter pylori in reflux oesophagitis. Gut 2001;49: 341-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fallone CA, Barkun AN, Gottke MU, Best LM, Loo VG, Veldhuyzen van Zanten S, et al. Association of Helicobacter pylori genotype with gastroesophageal reflux disease and other upper gastrointestinal diseases. Am J Gastroenterol 2000;95: 659-69. [DOI] [PubMed] [Google Scholar]
- 27.El Omar EM, Oien K, El Nujumi A, Gillen D, Wirz A, Dahill S, et al. Helicobacter pylori infection and chronic gastric acid hyposecretion. Gastroenterology 1997;113: 15-24. [DOI] [PubMed] [Google Scholar]
- 28.El Serag HB, Sonnenberg A, Jamal MM, Inadomi JM, Crooks LA, Feddersen RM. Corpus gastritis is protective against reflux oesophagitis. Gut 1999;45: 181-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu JC, Chan FK, Wong SK, Lee YT, Leung WK, Sung JJ. Effect of Helicobacter pylori eradication on oesophageal acid exposure in patients with reflux oesophagitis. Aliment Pharmacol Ther 2002;16: 545-52. [DOI] [PubMed] [Google Scholar]
- 30.Iijima K, Ohara S, Sekine H, Koike T, Kato K, Asaki S, et al. Changes in gastric acid secretion assayed by endoscopic gastrin test before and after Helicobacter pylori eradication. Gut 2000;46: 20-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koike T, Ohara S, Sekine H, Iijima K, Kato K, Toyota T, et al. Increased gastric acid secretion after Helicobacter pylori eradication may be a factor for developing reflux oesophagitis. Aliment Pharmacol Ther 2001;15: 813-20. [DOI] [PubMed] [Google Scholar]
- 32.Yamaji Y, Mitsushima T, Ikuma H, Okamoto M, Yoshida H, Kawabe T, et al. Inverse background of Helicobacter pylori antibody and pepsinogen in reflux oesophagitis compared with gastric cancer: analysis of 5732 Japanese subjects. Gut 2001;49: 335-40. [DOI] [PMC free article] [PubMed] [Google Scholar]