Understanding the pathophysiology of a burn injury is important for effective management. In addition, different causes lead to different injury patterns, which require different management. It is therefore important to understand how a burn was caused and what kind of physiological response it will induce.
The body's response to a burn
Burn injuries result in both local and systemic responses.
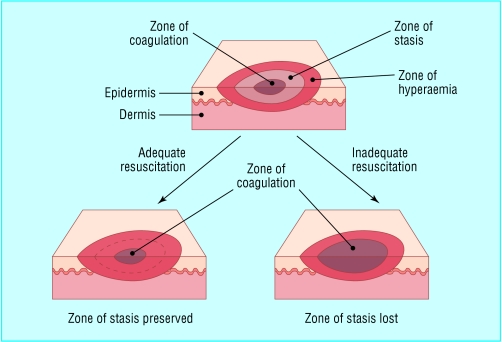
Figure 1.

Clinical image of burn zones. There is central necrosis, surrounded by the zones of stasis and of hyperaemia
Local response
The three zones of a burn were described by Jackson in 1947.
Zone of coagulation—This occurs at the point of maximum damage. In this zone there is irreversible tissue loss due to coagulation of the constituent proteins.
Zone of stasis—The surrounding zone of stasis is characterised by decreased tissue perfusion. The tissue in this zone is potentially salvageable. The main aim of burns resuscitation is to increase tissue perfusion here and prevent any damage becoming irreversible. Additional insults—such as prolonged hypotension, infection, or oedema—can convert this zone into an area of complete tissue loss.
Zone of hyperaemia—In this outermost zone tissue perfusion is increased. The tissue here will invariably recover unless there is severe sepsis or prolonged hypoperfusion.
These three zones of a burn are three dimensional, and loss of tissue in the zone of stasis will lead to the wound deepening as well as widening.
Figure 2.
Jackson's burns zones and the effects of adequate and inadequate resuscitation
Systemic response
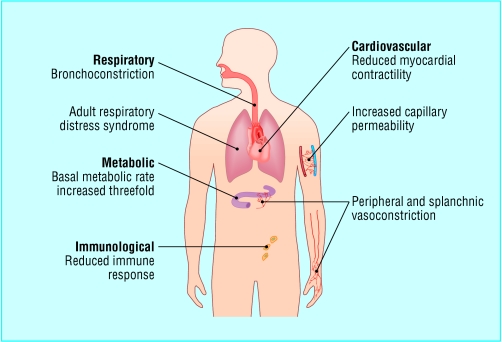
The release of cytokines and other inflammatory mediators at the site of injury has a systemic effect once the burn reaches 30% of total body surface area.
Cardiovascular changes—Capillary permeability is increased, leading to loss of intravascular proteins and fluids into the interstitial compartment. Peripheral and splanchnic vasoconstriction occurs. Myocardial contractility is decreased, possibly due to release of tumour necrosis factor α. These changes, coupled with fluid loss from the burn wound, result in systemic hypotension and end organ hypoperfusion.
Respiratory changes—Inflammatory mediators cause bronchoconstriction, and in severe burns adult respiratory distress syndrome can occur.
Metabolic changes—The basal metabolic rate increases up to three times its original rate. This, coupled with splanchnic hypoperfusion, necessitates early and aggressive enteral feeding to decrease catabolism and maintain gut integrity.
Immunological changes—Non-specific down regulation of the immune response occurs, affecting both cell mediated and humoral pathways.
Figure 3.
Systemic changes that occur after a burn injury
Mechanisms of injury
Thermal injuries
Scalds—About 70% of burns in children are caused by scalds. They also often occur in elderly people. The common mechanisms are spilling hot drinks or liquids or being exposed to hot bathing water. Scalds tend to cause superficial to superficial dermal burns (see later for burn depth).
Flame—Flame burns comprise 50% of adult burns. They are often associated with inhalational injury and other concomitant trauma. Flame burns tend to be deep dermal or full thickness.
Figure 4.


Examples of a scald burn (left) and a contact burn from a hot iron (right) in young children
Contact—In order to get a burn from direct contact, the object touched must either have been extremely hot or the contact was abnormally long. The latter is a more common reason, and these types of burns are commonly seen in people with epilepsy or those who misuse alcohol or drugs. They are also seen in elderly people after a loss of consciousness; such a presentation requires a full investigation as to the cause of the blackout. Burns from brief contact with very hot substances are usually due to industrial accidents. Contact burns tend to be deep dermal or full thickness.
Electrical injuries
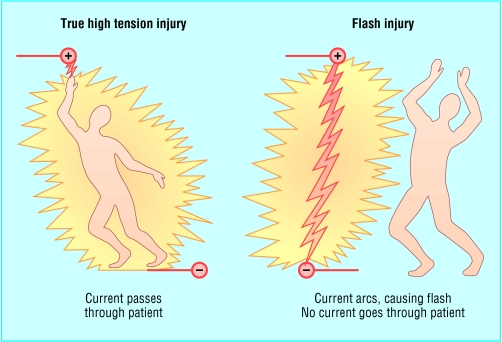
Some 3-4% of burn unit admissions are caused by electrocution injuries. An electric current will travel through the body from one point to another, creating “entry” and “exit” points. The tissue between these two points can be damaged by the current. The amount of heat generated, and hence the level of tissue damage, is equal to 0.24×(voltage)2×resistance. The voltage is therefore the main determinant of the degree of tissue damage, and it is logical to divide electrocution injuries into those caused by low voltage, domestic current and those due to high voltage currents. High voltage injuries can be further divided into “true” high tension injuries, caused by high voltage current passing through the body, and “flash” injuries, caused by tangential exposure to a high voltage current arc where no current actually flows through the body.
Figure 6.
Differences between true high tension burn and flash burn
Domestic electricity—Low voltages tend to cause small, deep contact burns at the exit and entry sites. The alternating nature of domestic current can interfere with the cardiac cycle, giving rise to arrhythmias.
“True” high tension injuries occur when the voltage is 1000 V or greater. There is extensive tissue damage and often limb loss. There is usually a large amount of soft and bony tissue necrosis. Muscle damage gives rise to rhabdomyolysis, and renal failure may occur with these injuries. This injury pattern needs more aggressive resuscitation and debridement than other burns. Contact with voltage greater than 70 000 V is invariably fatal.
“Flash” injury can occur when there has been an arc of current from a high tension voltage source. The heat from this arc can cause superficial flash burns to exposed body parts, typically the face and hands. However, clothing can also be set alight, giving rise to deeper burns. No current actually passes through the victim's body.
Figure 7.
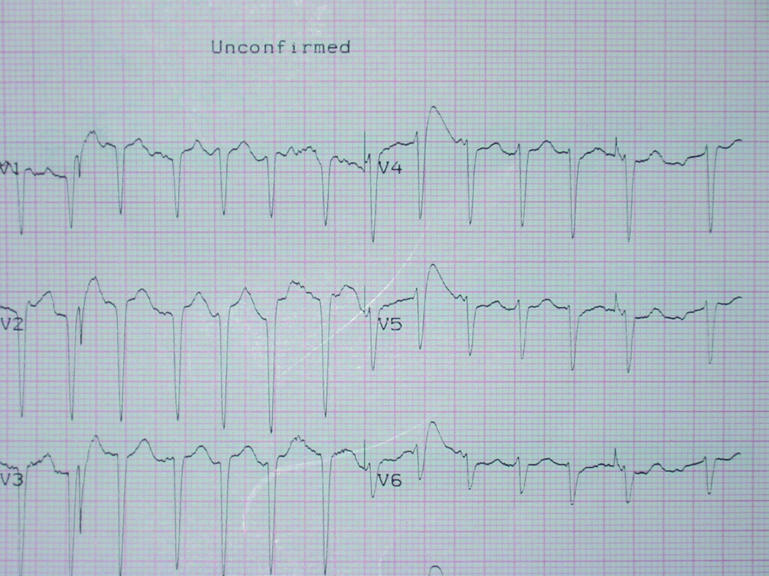
Electrocardiogram after electrocution showing atrial fibrillation
A particular concern after an electrical injury is the need for cardiac monitoring. There is good evidence that if the patient's electrocardiogram on admission is normal and there is no history of loss of consciousness, then cardiac monitoring is not required. If there are electrocardiographic abnormalities or a loss of consciousness, 24 hours of monitoring is advised.
Chemical injuries
Chemical injuries are usually as a result of industrial accidents but may occur with household chemical products. These burns tend to be deep, as the corrosive agent continues to cause coagulative necrosis until completely removed. Alkalis tend to penetrate deeper and cause worse burns than acids. Cement is a common cause of alkali burns.
Figure 8.

Chemical burn due to spillage of sulphuric acid
Certain industrial agents may require specific treatments in addition to standard first aid. Hydrofluoric acid, widely used for glass etching and in the manufacture of circuit boards, is one of the more common culprits. It causes a continuing, penetrating injury and must be neutralised with calcium gluconate, either applied topically in a gel or injected into the affected tissues.
The initial management of all chemical burns is the same irrespective of the agent. All contaminated clothing must be removed, and the area thoroughly irrigated. This is often best achieved by showering the patient. This has been shown to limit the depth of the burn. Litmus paper can be used to confirm removal of alkali or acid. Eye injuries should be irrigated copiously and referred to an ophthalmologist.
Table 1.
Specific chemical burns and treatments
| Chromic acid—Rinse with dilute sodium hyposulphite |
| Dichromate salts—Rinse with dilute sodium hyposulphite |
| Hydrofluoric acid—10% calcium gluconate applied topically as a gel or injected |
Non-accidental injury
An estimated 3-10% of paediatric burns are due to non-accidental injury. Detecting these injuries is important as up to 30% of children who are repeatedly abused die. Usually young children (< 3 years old) are affected. As with other non-accidental injuries, the history and the pattern of injury may arouse suspicion. A social history is also important. Abuse is more common in poor households with single or young parents. Such abuse is not limited to children: elderly and other dependent adults are also at risk. A similar assessment can be made in these scenarios.
Table 2.
Injury pattern of non-accidental burns
| • Obvious pattern from cigarettes, lighters, irons |
| • Burns to soles, palms, genitalia, buttocks, perineum |
| • Symmetrical burns of uniform depth |
| • No splash marks in a scald injury. A child falling into a bath will splash; one that is placed into it may not |
| • Restraint injuries on upper limbs |
| • Is there sparing of flexion creases—that is, was child in fetal position (position of protection) when burnt? Does this correlate to a “tide line” of scald—that is, if child is put into a fetal position, do the burns line up? |
| • “Doughnut sign,” an area of spared skin surrounded by scald. If a child is forcibly held down in a bath of hot water, the part in contact with the bottom of the bath will not burn, but the tissue around will |
| • Other signs of physical abuse—bruises of varied age, poorly kempt, lack of compliance with health care (such as no immunisations) |
It is natural for non-accidental injury to trigger anger among healthcare workers. However, it is important that all members of the team remain non-confrontational and try to establish a relationship with the perpetrators. The time around the burn injury is an excellent opportunity to try to break the cycle of abuse. In addition, it is likely that the patient will eventually be discharged back into the care of the individuals who caused the injury. As well as treating the physical injury, the burn team must try to prevent further abuse by changing the relationship dynamics between victim and abuser(s).
Table 3.
History of non-accidental burns
| • Evasive or changing history |
| • Delayed presentation |
| • No explanation or an implausible mechanism given for the burn |
| • Inconsistency between age of the burn and age given by the history |
| • Inadequate supervision, such as child left in the care of inappropriate person (older sibling) |
| • Lack of guilt about the incident |
| • Lack of concern about treatment or prognosis |
Any suspicion of non-accidental injury should lead to immediate admission of the child to hospital, irrespective of how trivial the burn is, and the notification of social services.
The team should carry out the following:
Examine for other signs of abuse
Photograph all injuries
Obtain a team opinion about parent-child interaction
Obtain other medical information (from general practitioner, health visitor, referring hospital)
Interview family members separately about the incident (check for inconsistencies) and together (observe interaction).
It should be remembered that the injury does not have to be caused deliberately for social services to intervene; inadequate supervision of children mandates their involvement.
Figure 9.

“Doughnut sign” in a child with immersion scalds. An area of spared skin is surrounded by burnt tissue. The tissue has been spared as it was in direct contact with the bath and protected from the water. This burn pattern suggests non-accidental injury
Table 4.
Key points
| • A burn results in three distinct zones—coagulation, stasis, and hyperaemia |
| • The aim of burns resuscitation is to maintain perfusion of the zone of stasis |
| • Systemic response occurs once a burn is greater than 30% of total body surface area |
| • Different burn mechanisms lead to different injury patterns |
| • Identification of non-accidental burn injury is important |
Shehan Hettiaratchy is specialist registrar in plastic and reconstructive surgery, Pan-Thames Training Scheme, London; Peter Dziewulski is consultant burns and plastic surgeon, St Andrews Centre for Plastic Surgery and Burns, Broomfield Hospital, Chelmsford.
The ABC of burns is edited by Shehan Hettiaratchy; Remo Papini, consultant and clinical lead in burns, West Midlands Regional Burn Unit, Selly Oak University Hospital, Birmingham; and Peter Dziewulski. The series will be published as a book in the autumn.
Competing interests: See first article for series editors' details.
Further reading and resources
- • Kao CC, Garner WL. Acute burns. Plast Reconstr Surg 2000;105: 2482-93 [PubMed] [Google Scholar]
- • Andronicus M, Oates RK, Peat J, Spalding S, Martin H. Non-accidental burns in children. Burns 1998;24: 552-8 [DOI] [PubMed] [Google Scholar]
- • Herndon D. Total burn care. 2nd ed. London: WB Saunders, 2002
- • Luce EA. Electrical burns. Clin Plast Surg 2000;27: 133-43 [PubMed] [Google Scholar]
- • Kirkpatrick JJR, Enion DS, Burd DAR. Hydrofluoric acid burns; a review. Burns 1995;21: 483-93 [DOI] [PubMed] [Google Scholar]
- • Burnsurgery.org. www.burnsurgery.org