Abstract
Objectives
To examine the impact of a successful 12 month behavioral intervention to improve diabetes control on healthcare utilization in American Samoa.
Methods
A cluster randomized design was used to assign 268 diabetes patients to a nurse-community health worker (CHW) intervention or usual care. Hospitalizations, emergency department (ED) and primary care physician (PCP) visits were collected retrospectively for one year prior to, and during, the intervention to assess changes in healthcare utilization. The association of utilization changes with change in HbA1c during the intervention was assessed.
Results
Adjusted incidence rate ratios (RR) for PCP visits were significantly higher in the CHW relative to the usual care group (RR= 1.71; 95% CI, 1.25–2.33). There was no main intervention effect on ED utilization, but visits in the prior year modified the intervention effect on ED visits. Increased PCP utilization was associated with greater decreases in HbA1c (b=−0.10, se=0.04, p=0.01).
Conclusions
A culturally adapted CHW diabetes intervention in American Samoa significantly increased PCP visits, and decreased ED visits among those with high ED usage in the prior year. These changes suggest important and beneficial impacts on health system utilization from the diabetes intervention in a low resource and high-risk population.
INTRODUCTION
American Samoans have high type 2 diabetes levels, approximately 21.5% among those >18 years, due to nutritional transitions and the rise in obesity and hypertension over the last thirty years.1–4 Health inequalities among American Samoans especially in non-communicable diseases (NCDs) and their risk factors such as dietary intake, sedentariness and low health literacy are associated with rapid modernization and the health transition, relative geographic isolation and an underdeveloped health care system with a health care professional shortage.5,6 American Samoa (AS) is located in the central South Pacific, approximately 2400 miles Southwest of Hawaii, has a population of 55,519, and 58% of families are below the US poverty level.7,8 These AS individual and social structural characteristics are broadly similar to other US low income and ethnic minority communities, such as Native Americans, Hispanic and African-American groups, as well as to low and middle income countries experiencing health transitions. Thus, research in this setting may be generalized outside of contemporary Polynesian settings.
Community health worker (CHW) interventions have been shown to improve biomarkers of diabetes control and reduce high utilization of health care from emergency visits and hospitalizations.9,10 There have been observational and non-randomized diabetes studies among Pacific Islanders,11–14 and in Torres Strait islanders.15,16
Diabetes Care in American Samoa (DCAS) is the first randomized controlled trial (RCT) for diabetes in American Samoa and assessed the effects on diabetic control of a 12 month nurse-community health worker (CHW) team intervention, compared to usual care.17,18 We found significant improvement in glycosolated hemoglobin (HbA1c) in the CHW group compared with usual care.18 Adjusted HbA1c among CHW participants was 0.53 units less at the end of the intervention compared with the usual care group, and the odds of reporting a change of at least 0.5% in HBA1c from baseline to end of treatment for the CHW group was 2.07 times greater than among the usual care group.18 DCAS culturally translate done of the few well-designed RCTs with a CHW model, Project Sugar, which examined a nurse-CHW team model for diabetes management among African Americans on Medicare in West Baltimore.19,10 Project Sugar found significant decreases over 2-years in emergency department (ED) visits in the CHW group.10 An earlier CHW program for West Baltimore type 2 diabetes patients conducted a retrospective evaluation of Medicaid claims and found a 40% reduction in ED visits and a 33% reduction in hospital admissions.20
This report describes the impact of the DCAS behavioral intervention on healthcare utilization, including ED visits, hospitalizations, and primary care physician (PCP) visits, as well as the association of utilization with change in HbA1c among Samoan adults with type 2 diabetes. Based on prior studies and the design of our intervention17,18 we hypothesized that those receiving the CHW intervention would show reduced ED visits and hospitalizations, and increased PCP visits during the intervention year, compared to those in the usual care group.
METHODS
Study Design, Setting and Participants
More detail about methods can be found elsewhere, but we provide a brief overview here, as it relates to the present hypotheses.18 DCAS was a cluster RCT conducted on the main island of Tutuila in American Samoa. Study participants were drawn from patient records of the Tafuna Clinic (TC), a federally qualified community primary health care center.18 Villages within TC’s catchment area were randomized to the CHW intervention or usual care/wait-list control arms with six villages assigned to the 12-month CHW intervention and six to 12-months of usual care.18 Villages were matched by size and different location to avoid intervention and usual care villages being adjacent to one another to limit potential contamination.
Health center staff enrolled patients on a rolling basis with eligibility criteria kept broad to test real-world effectiveness. Eligible patients were adults who self-identified as Samoan, had type 2 diabetes diagnosed by a physician, were mentally competent and willing to give informed consent, were unlikely to leave American Samoa for 4 months during the study, and were free of comorbid conditions likely to lead to death in the next year. Patients had to be willing to receive care at TC, where the CHW intervention was based. While some patients had sought primary care at the hospital prior to the study, they were able to enroll if they moved their primary care or used both sites.
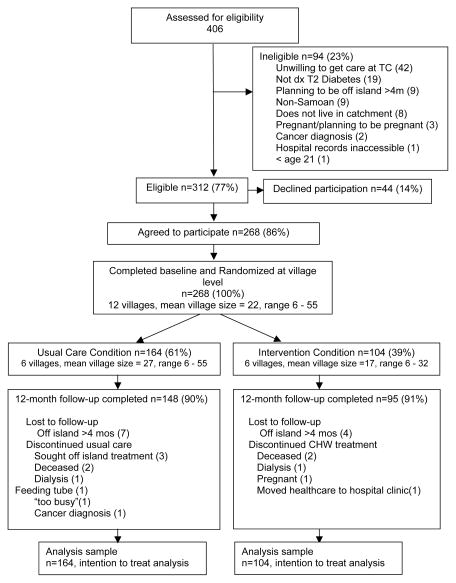
The sample for the healthcare utilization study consisted of all 268 participants enrolled in DCAS.18 Of the 268 participants from 12 villages, 104 (93 households) were assigned to the CHW intervention and 164 (148 households) were assigned to the usual care group (Figure 1). This imbalance was due to differential recruitment efforts on the part of the field staff as they strove to meet enrollment targets.
Figure 1.
CONSORT diagram of recruitment
The study design for assessment of healthcare utilization was based on a comparison between the CHW and the usual care trial arms of the changes in utilization during the 12-months in the intervention trial relative to utilization in the year before trial entry. The primary outcome measures were the numbers of ED visits, overnight hospitalizations, and PCP visits during the intervention year, based on medical chart records. ED visits and hospitalizations were considered to reflect poor diabetes control, while PCP visits reflected good adherence to diabetes management guidelines. In addition we sought to detect an association between changes in ED and PCP visits and changes in HbA1c during the intervention. All study protocols and informed consent procedures were approved by Institutional Review Boards of the American Samoa Department of Health, and Brown University.
Intervention
DCAS project staff included a nurse case manager (NCM) and four CHWs. Intervention content included a menu of eight topics, including basic diabetes information and seven diabetes-related behaviors (healthy eating, physical activity, medication adherence, monitoring, risk reduction, healthy coping, and problem solving).18,22,23 During their visits, CHWs used flipcharts modeled on the National Diabetes Education Program flipcharts for diabetes prevention to facilitate their teaching of basic diabetes education.21 These flipcharts included eight sections corresponding to the aforementioned diabetes-related behaviors and were adapted to the local context by incorporating cultural features that had been identified through formative focus groups with diabetes patients and in-depth interviews with health care providers.17
The specific content of each participant’s intervention was guided by patient risk and patient self-directed goals from the menu of eight topics listed above. Risk profiles were determined by data collected at the baseline assessment and included HbA1c, BP, smoking status, alcohol use, and depression scores on PHQ-9. Higher risk patients were seen weekly, moderate risk patients were seen monthly by CHWs, and lower risk patients were seen every three months.18 The intervention encouraged participants to have regular doctors’ appointments for diabetes care, following American Diabetes Association guidelines.24 Blood glucose (BG) and BP were monitored at each intervention visit. When urgent levels (defined as BG≥400mg/dL and BP≥200/120mmHg) were detected, patients were referred immediately to the TC physician (if during clinic hours) or to the hospital emergency department (if outside of clinic hours).
Data Collection
The baseline assessment included information on sociodemographics, personal beliefs about diabetes control, diet and exercise, and clinical indicators such as BMI, BP, BG, and HbA1c. Using this information, CHW group patients were assigned one of three risk profiles as explained above. Following the baseline assessment, the usual care group patients continued receiving primary care for their diabetes based on their regularly scheduled and any self-initiated appointments for one year.18 The follow-up assessment was conducted in both groups 12 months after baseline. After follow-up the usual care group received the CHW intervention.
Glycemic control was measured as HbA1c to reflect BG over a 3-month period, using DCA 2000®+ analyzer.25,26 The DCA 2000 reports only “>14” for HbA1c values greater than 14; we had eight such values, 5 in the usual care and 3 in the CHW group; these were coded as 14, thus the mean HbA1c is conservative.
The healthcare utilization data collected were the number of ED visits, overnight hospitalizations, and PCP visits during the year before and one year after enrollment, or until ineligibility due to pregnancy, dialysis, or off-island travel of a duration exceeding four months. Data were abstracted from the Computerized Patient Record System (CPRS) at LBJ Tropical Medical Center, the hospital in American Samoa. Supplementary data on PCP visits (including visit dates and reasons) at TC were abstracted from their paper medical records. As noted, some patients had used LBJ doctors for primary care and may have used both sites for care during the study. It is possible that individuals obtained primary care at one of the outlying community health centers but very unlikely given the greater distance between facilities. Thus, data obtained from their records provide the best measure of health care visits on the island. It was not possible to obtain care utilization data outside American Samoa.
Statistical Analysis
Baseline variables were compared between the CHW intervention and usual care groups using t-tests for continuous variables and χ2 tests for categorical variables. As the healthcare utilization data did not follow a normal distribution, nonparametric tests were used to detect utilization differences between groups (whether the difference between the year prior to baseline and the year after baseline were statistically different between the 2 groups) and within group changes. Specifically, the Wilcoxon two-sample test was used to detect baseline differences in ER and PCP visits between groups and the signed-rank test was used to detect within group changes in ER and PCP visits from the year before study enrollment to the 12 month follow up. Hospitalizations were analyzed as a dichotomous variable (any/none) and within group changes were analyzed using McNemar’s test.
The main outcome variables were number of ED visits and number of PCP visits with intervention status as the exposure variable. Negative binomial regression was used to account for multiple visits censored for death and loss to follow up. Estimates are absolute rate differences (RDs) and ratios of utilization rates (RRs) in the two groups. Three interactions were examined to investigate whether baseline risk level, the number of ER visits in the year before enrollment, or the number of PCP visits in the year before enrollment modified the effect of the intervention. In subsidiary analyses, adjustment was made for age, gender, and baseline characteristics (location of doctor (TC, LBJ, both), risk level, personal perception of diabetes control as measured by response to the single item, “my diabetes in is good control” (5=strongly agree, 1=strongly disagree)27 pre-baseline utilization, and the interaction of pre-baseline utilization with treatment group). Analyses controlled for the clustering of participants in villages and households through the use of generalized estimating equations (GEEs).
As a subsequent step, we tested the association between changes in HbA1c during the 12 month intervention and PCP and ED visits, using a series of mixed effects regression models, controlling for baseline outcome values, as well as covariates (indicators of potential contamination by church, co-morbidities, perceived diabetes control, gender, age, baseline risk level). Models included random intercepts to account for within subject correlation between repeated outcomes over time and standard errors accounted for two levels of clustering: households and villages. Estimation is likelihood based and thus makes use of all available data (intent to treat analysis).
All analyses were conducted using SAS statistical software (version 9.2 SAS Institute Inc., Cary, NC, USA).
RESULTS
Baseline characteristics
Patients were enrolled between February 2009 and May 2010 and all participants completed the follow-up assessment by June 2011. Roughly two-thirds of participants were women and their mean age was 55 years (Table 1). More than half were unemployed, reflecting the age of the sample and high level of unemployment in American Samoa. Clinical characteristics, including body mass index, HbA1c, and BP of the groups were similar. Baseline differences in risk levels based on clinical indicators and self-reported health behaviors were not statistically significant between the two groups. Although there was no statistically significant utilization difference in the year prior to baseline between the two groups in terms of the frequency of ED and PCP visits (Table 1), patients in the CHW group were more likely than usual care patients to receive their primary care at TC. Patients assigned to intervention and usual care groups also differed in the language spoken during the baseline interview, with more patients in the usual care arm speaking Samoan only. Compared to those in the usual care group, patients in the CHW group were more likely to believe at baseline that their diabetes was in good control. There was no difference in loss-to-follow-up between groups, with 91% retention overall. Losses occurred primarily due to death, initiation of dialysis, and off-island travel of a duration exceeding four months. In the CHW group there were three deaths and seven losses to follow up and in the usual care group there were two deaths and twelve losses to follow up.
Table 1.
Selected Baseline characteristics of the study population by randomization groupa
| CHW Intervention Group (n=104) | Usual Care Group (n=164) | Total Study Group (n=268) | P value b | |
|---|---|---|---|---|
| Sociodemographics | ||||
| Female | 60(58) | 108(66) | 168(63) | 0.178 |
| Age (years) | 56 12 | 54 13 | 55 13 | 0.386 |
| Marital status | 0.100 | |||
| Married | 82(79) | 129(79) | 211(78) | |
| Widow/separated/divorced | 13(13) | 30(18) | 43(16) | |
| Never been married | 9(9) | 5(3) | 14(5) | |
| Employed | 46(44) | 76(46) | 122(46) | 0.798 |
| Language on Interview | <0.001 | |||
| Samoan only | 69(66) | 132(80) | 201(75) | |
| English only | 0 | 7(4) | 7(3) | |
| English and Samoan | 35(34) | 25(15) | 60(22) | |
| Healthcare utilization (prior 12 months) | ||||
| Hospitalization (yes/no) | 11(11) | 15(9) | 26(10) | 0.700 |
| ED visits | 0.144 | |||
| None | 45(43) | 71(43) | 116(43) | |
| 1–3 | 54(52) | 74(45) | 128(48) | |
| 4+ | 5(5) | 19(12) | 24(9) | |
| Primary care visits | 0.265 | |||
| None | 11(11) | 29(18) | 40(15) | |
| 1–3 | 47(45) | 65(40) | 112(42) | |
| 4+ | 46(44) | 70(43) | 116(43) | |
| Location of doctor | <0.001 | |||
| Hospital | 49(47) | 81(49) | 130(49) | |
| Primary Care Clinic | 52(50) | 62(38) | 114(43) | |
| Both/Other | 0 | 19(12) | 19(7) | |
| Health Beliefs c (My diabetes is well controlled) | <0.001 | |||
| Strongly disagree | 2(2) | 0 | 2(1) | |
| Disagree | 11(11) | 22(13) | 33(12) | |
| Not sure | 19(18) | 54(33) | 73(27) | |
| Agree | 31(30) | 59(36) | 90(34) | |
| Strongly agree | 37(36) | 27(16) | 64(24) | |
| Health Behaviors | ||||
| Smoking | 0.028 | |||
| Never | 84(81) | 147(90) | 231(86) | |
| Former | 3(3) | 1(1) | 4(1) | |
| Current | 15 (14) | 11(7) | 26(10) | |
| Medication Adherence(yes) | 43(41) | 93(57) | 136(51) | 0.145 |
| Clinical characteristics | ||||
| BMI, kg/m2 | 36±7.3 | 37±7.9 | 37±7.7 | 0.876 |
| Systolic BP (mmHg) | 131±16 | 134±17 | 132±17 | 0.247 |
| Diastolic BP (mmHg) | 84±9.3 | 84±11 | 84±10 | 0.924 |
| HbA1c, % | 9.6±2.1 | 10±2.3 | 9.8±2.3 | 0.151 |
| Risk Leveld | 0.210 | |||
| Lower Risk | 10(9.6) | 20(12.2) | 30(11) | |
| Moderate Risk | 50(48.1) | 61(37.2) | 111(41) | |
| High Risk | 44(42.3) | 83(50.6) | 127(47) |
Abbreviations: BMI, body mass index (weight (kg)/height (m2); BP, blood pressure; ED, emergency department; HbA1c, hemoglobin A1c. NB. Numbers may not add up to total due to missing data
Results are shown as number (percentage) or mean ± SD
P-values based on Chi-square test or Fisher’s exact test for categorical variables, t-test for continuous variables, Wilcoxon two-sample test for count variables
Health Beliefs: based on degree of subject agreement with the statement “My diabetes is well controlled.”
Risk level: based on HbA1c, blood pressure, smoking status, alcohol consumption, and depression (PHQ-9 score).
ED visits, hospitalizations, and PCP visits at 12 months
Unadjusted analyses using nonparametric methods showed no change in hospital utilization in the CHW and usual care groups from baseline to 12-month follow-up. An unadjusted comparison of within group changes in ED visits and PCP visits between the intervention and usual care groups is presented in Table 2. These results indicate a statistically significant increase in PCP visits in the CHW group during the intervention year. There was a temporal decline in emergency care visits in the CHW group but this did not reach statistical significance (p=0.087). No significant changes from the prior year in ED or PCP visits occurred in the usual care group during the 12 month study period. A comparison of CHW and usual care groups in terms of median changes scores (the difference between numbers of pre-intervention and post-intervention visits) for PCP visits and ED visits showed no significant difference (p-values for the Wilcoxon rank sum test were 0.591 and 0.086 for ED visits and PCP visits respectively).
Table 2.
Comparison of healthcare utilization, one year before and after enrollment
| Healthcare Utilization | One Year Before | One Year After | Within Group Change | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Median | IQ Range | Median | IQ Range | Median | IQ Range | P value | |
| Intervention Group | |||||||
| ED visits | 1.0 | 0.0–2.0 | 0 | 0.0–1.5 | 0 | −1.0 – 0.0 | 0.087 |
| Primary care visits | 3.0 | 1.0–4.0 | 3.5 | 2.0–5.0 | 0 | −1.0 – 3.0 | 0.041 |
| Control Group | |||||||
| ED visits | 1.0 | 0.0–2.0 | 0 | 0.0–2.0 | 0 | −1.0 – 1.0 | 0.879 |
| Primary care visits | 3.0 | 1.0–5.0 | 3.0 | 1.0–5.0 | 0 | −1.0 – 1.0 | 0.570 |
Abbreviations: IQ, Interquartile; ED, Emergency Department.
Median within group change refers to the median change in the number of visits in the year before study enrollment to the number of visits in the intervention year.
Results are based on signed-rank test.
Unadjusted incidence rate ratios for ED visits showed a decrease in ED visits and an increase in PCP visits in the intervention group relative to the usual care group (Table 3). The observed increase in PCP visits in the CHW group remained statistically significant (adjusted RR, 1.71; 95% CI, 1.25–2.33; rate increase 71%) in analyses that controlled for the effect of clustering of patients in villages and households, age, sex, pre-baseline utilization, baseline risk level, as well as self-reported physician location and perceived diabetes control. However, no significant difference between the two groups in ED visits (adjusted RR, 1.04; 95% CI, 0.69–1.57; rate increase 4%) was detected in analyses controlling for these same variables. As expected, the numbers of ED and PCP visits in the year before study enrollment were significant predictors of visits during the intervention year (p<0.001). Baseline risk level did not appear to modify the effect of the intervention on ED visits (p-value for interaction term = 0.50) or PCP visits (p-value for interaction term = 0.34).
Table 3.
ED Visits and Primary Care Visits at 12-Months
| Group | No. | Counts | Person-Years (py) | Rate per 100 py | RD per 100 py | Unadjusted RR | Unadjusted RD % | Adjusted RR (95% CI) | Adjusted RD % |
|---|---|---|---|---|---|---|---|---|---|
| ED visits | |||||||||
| Control | 164 | 237 | 163 | 146.0 | [ref] | 1.00 | [ref] | 1.00 | [ref] |
| CHW | 104 | 91 | 100 | 91.3 | 54.7 | 0.63(0.49,0.80) | 37 | 1.04(0.69,1.57) | 4 |
| Primary Care visits | |||||||||
| Control | 164 | 495 | 163 | 304.4 | [ref] | 1.00 | [ref] | 1.00 | [ref] |
|
|
|||||||||
| CHW | 104 | 416 | 100 | 417.4 | 113 | 1.37(1.20,1.56) | 37 | 1.71(1.25,2.33) | 71 |
Abbreviations: CHW, community health worker; CI, confidence interval; RD, rate difference; RR, rate ratio.
Adjusted for age, sex, and baseline characteristics (doctor location, risk level, health beliefs, pre-baseline utilization, and the interaction of pre-baseline utilization with treatment group) with over-dispersion parameter and control for the effect of clustering in villages and households. The natural log of person-years at risk was included as an offset in the model. The coefficient of interaction term for pre-baseline ED visits with treatment group is −0.2126 (p=0.0179) and coefficient for interaction term of pre-baseline primary visits with treatment group is −0.0520 (p=0.0670).
There was a significant interaction (p=0.018) between group and the number of ED visits during the year before study enrollment. Analyses indicated the CHW intervention had a greater effect in reducing ED visits in those who had more ED visits before study enrollment; each additional ED visit before enrollment was associated with a 20% (95% CI: 12%, 26%) reduction in the relative risk of ED visits during the intervention year. The interaction between the intervention and the number of PCP visits in the year before study enrollment was marginally significant (p=0.067).
Effect of ED and PCP visits on changes in HbA1c from baseline to 12-months
There was not a significant association between ED visits and changes in HbA1c (b=−0.08, se=0.04, p=0.08). However, PCP visits were significantly and inversely associated with changes in HbA1c, even after adjusting for trial group, potential confounders and baseline values (b=−0.10, se=0.04, p=0.01). Specifically, the mean difference in HbA1c at the end of the intervention was 0.10 units less for every one-unit increase in PCP visits over the treatment period in the entire study sample.
DISCUSSION
In this low-income American Samoan setting a 12-month CHW diabetes intervention increased primary care utilization by 71% in the CHW group compared to the usual care group, adjusting for PCP visits in the year before the intervention. Based on the underdeveloped health care system currently in American Samoa related to NCDs, especially type 2 diabetes,6,17 and the design of our intervention to increase understanding and ability to improve self-management,23 we expected the diabetes control intervention would increase primary care services during that 12 month period.16 CHW smonitored when patients were due to be seen and during their home visits specifically encouraged, reminded and assisted participants to make and keep regular PCP appointments.23 Based on standards of care for type 2 diabetes, PCP visits offer opportunities to monitor diabetes control and adjust medication management if needed, (refill/change prescriptions), order timely lab-work to monitor lipids and kidney function and encourage other self-management behaviors.17,22,24
The finding of no reduction in ED visits in the CHW group was surprising and may be understood given differences between the American Samoan health care system and those where similar interventions found ED visit declines.10, 16, 20 American Samoa’s primary care facilities were few in number at the time of the research and frequently understaffed so patients seeking non-emergency care, including prescription refills, may choose to visit the ED to receive care that should be provided at a primary care facility.6 The only pharmacy is located adjacent to the ED at the one hospital. Patients needing medications might have opted for ED care and refills rather than making two trips: one to TC to visit their PCP and another to the pharmacy. Despite not detecting a main effect, our results suggest the intervention’s impact on ED visits was modified by use of ED care before enrollment. The CHW intervention seemed to have a greater effect on reducing ED visits among higher ED users in the prior year.
Several studies have examined the impact on healthcare utilization of CHW interventions with diabetes patients.10,15,16,20 The Project Sugar 2 study, a CHW intervention among African American diabetes patients in Baltimore, found significant ED visit reductions in the CHW group but no effect on hospitalizations.10 Another study in Baltimore African Americans with diabetes using a CHW intervention found reductions in ED visits and hospitalizations in the CHW group, as well as reduced health system expenditures.20 Neither of these two studies reported data on PCP visits. The study in Torres Strait Islanders using indigenous health workers to improve diabetes control and care showed significant reductions in hospital admissions for diabetes-related conditions over the study period, which were sustained three years later.15,16 No data on PCP visits were reported.
The improved diabetes control with increases in PCP visits is consistent with the overall intervention effect of improved control in the CHW arm18, and supports the fundamental mechanism of receiving primary care for diabetes on improved biomedical control. Further mediation analyses will examine participants’ behavioral changes resulting from the CHW intervention visits and permit causal inferences about their effects and strengths on influencing improved diabetic control.
Our and others’ results support the use of CHWs, or similar outreach staff, from the same culture and society as diabetes patients in order to improve utilization of the health system.28–31 The relationships among PCP and ED visits, hospitalizations and lengths of stay need further study to provide evidence for comparative effectiveness of CHW interventions with diabetes patients. Certainly, PCP visits are less costly than ED visits and hospitalizations in all health care systems and we can assume that optimal use of PCP visits will reduce excessive ED use and overnight hospital stays. However, increases in PCP visits represent non-trivial health system expenditures and there is a possibility that excessive PCP visits do not improve diabetes control and lead to high costs. The emphasis of future research should be to determine for each society the most efficacious and cost-effective mix of increased PCP visits that lead to improved diabetes control. Strengths of this study that lend weight to these findings include the randomized controlled design, 86% enrollment of eligible individuals, 91% retention and follow-up, and adjustment for baseline healthcare utilization levels, age, and follow-up time. Using members of the same community and culture as CHWs assured compatibility between the intervention message and the messengers. The CHWs, Samoans recruited from the community, were seen as trustworthy by their patients and thus were able to communicate meaningfully with them, including messages to make and keep appointments with their doctors for diabetes care.
Several limitations of the study deserve mention. Recruitment depended on a positive diagnosis of type 2 diabetes. Individuals who were not aware of their diabetes status, do not regard diabetes as important, or in general have low health literacy about NCDs did not have an opportunity to be recruited, despite our community screening activities.18 It is possible that selection bias could affect the results because of the way in which participants were selected into the sample. Nonetheless we believe the findings are generalizable to other diabetes patients in resource poor and high-risk populations. The 12-month evaluation period evaluation is relatively short, suggesting further follow-up assessments. However, since the usual care group received the intervention after 12 months, further longitudinal assessment of the intervention is not possible. In addition, the utilization data is only as complete as the hospital’s electronic record and paper charts at TC; there may have been undocumented visits. Unfortunately, there was no means of determining the accuracy of these record systems although an examination of the paper ED log and several paper hospital charts indicated that the electronic record contained more complete utilization information. These data do not include healthcare received off-island but this was likely uncommon due to costs and travel. Furthermore, participants who traveled off-island for periods exceeding four months were censored from the data. Our measurement of HbA1c had a maximum of 14 but the eight individuals with these values were evenly distributed, with 5 in the usual care and 3 in the CHW group.
In conclusion the CHW group’s increase in PCP visits, their apparent decrease in ED visits among those with high ED usage in the prior year, and the overall association between increased number of PCP visits and lower Hba1C levels suggest important and beneficial impacts on utilization. Future work should include cost effectiveness analysis of healthcare utilization, and use of longer follow up periods for evaluation of long-term impacts of CHW interventions on utilization. To have the greatest impact of utilization and its costs, future interventions might focus on high risk patients with frequent ED utilization.
Acknowledgments
Financial support: US, NIH, National Institute of Diabetes, Digestive, and Kidney Disorders Grant # R18-DK075371, (PI: ST McGarvey), and Downs Fellowship, Yale School of Public Health (SH).
References
- 1.McGarvey ST. Obesity in Samoans and a perspective on its etiology in Polynesians. Am J Clin Nutr. 1991;53(6):1586S–1594S. doi: 10.1093/ajcn/53.6.1586S. [DOI] [PubMed] [Google Scholar]
- 2.Galanis DJ, McGarvey ST, Quested C, Sio B, Afele-Fa’amuli SA. Dietary intake of modernizing Samoans: Implications for risk of cardiovascular disease. J Am Diet Assoc. 1999;99(2):184–190. doi: 10.1016/s0002-8223(99)00044-9. [DOI] [PubMed] [Google Scholar]
- 3.Keighley ED, McGarvey ST, Turituri P, Viali S. Farming and Adiposity in Samoan Adults. Am J Hum Biol. 2006;18:112–121. doi: 10.1002/ajhb.20469. [DOI] [PubMed] [Google Scholar]
- 4.DiBello JR, Baylin A, Viali S, Tuitele J, Bausserman L, McGarvey ST. Adiponectin and type 2 diabetes in Samoan Adults. Am J Hum Biol. 2009;21:389–391. doi: 10.1002/ajhb.20858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keighley ED, McGarvey ST, Quested C, McCuddin C, Viali S, Maga U. Nutrition and health in modernizing Samoans: temporal trends and adaptive perspectives. In: Ohtsuka R, Ulijaszek SJ, editors. Health Change in the Asia-Pacific Region: Biocultural and Epidemiological Approaches. Cambridge University Press; 2007. pp. 147–191. [Google Scholar]
- 6.Henry M, Ichiho HM, Roby FT, Ponausuia ES, Aitaoto N. An Assessment of Non-Communicable Diseases, Diabetes, and Related Risk Factors in the Territory of American Samoa: A Systems Perspective. Haw Jl Med Pub Hlth. 2013;72 (5, Suppl 1):10–18. [PMC free article] [PubMed] [Google Scholar]
- 7.Census US. [Accessed 15 March 2012];2010 census population counts for American Samoa. Available from http://2010.census.gov/news/releases/operations/cb11-cn177.html.
- 8.American Samoa Department of Commerce. [Accessed 15 March 2012];American Samoa at-a-glance. 2006 Available from www.spc.int/prism/country/as/stats/At_A_Glance_2006.pdf.
- 9.Hawthorne K, Robles Y, Cannings-John R, Edwards AG. Culturally appropriate health education for type 2 diabetes in ethnic minority groups: A systematic and narrative review of randomized controlled trials. Diabet Med. 2010;27(6):613–623. doi: 10.1111/j.1464-5491.2010.02954.x. [DOI] [PubMed] [Google Scholar]
- 10.Gary TL, Batts-Turner M, Yeh HC, et al. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: A randomized controlled trial. Arch Intern Med. 2009;169(19):1788–1794. doi: 10.1001/archinternmed.2009.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beckham S, Bradley S, Washburn A, Taumua T. Diabetes management: Utilizing community health workers in a Hawaiian/Samoan population. J Health Care Poor Underserved. 2008;19(2):416–427. doi: 10.1353/hpu.0.0012. [DOI] [PubMed] [Google Scholar]
- 12.Mau MK, Glanz K, Severino R, Grove JS, Johnson B, Curb JD. Mediators of lifestyle behavior change in Native Hawaiians: Initial findings from the Native Hawaiian diabetes intervention program. Diabetes Care. 2001;24(10):1770–1775. doi: 10.2337/diacare.24.10.1770. [DOI] [PubMed] [Google Scholar]
- 13.Bell AC, Swinburn BA, Amosa H, Scragg RK. A nutrition and exercise intervention program for controlling weight in samoan communities in new zealand. Int J Obes Relat Metab Disord. 2001;25(6):920–927. doi: 10.1038/sj.ijo.0801619. [DOI] [PubMed] [Google Scholar]
- 14.Simmons D, Fleming C, Voyle J, Fou F, Feo S, Gatland B. A pilot urban church-based programme to reduce risk factors for diabetes among Western Samoans in New Zealand. Diabet Med. 1998;15(2):136–142. doi: 10.1002/(SICI)1096-9136(199802)15:2<136::AID-DIA530>3.0.CO;2-P. 2-P. [DOI] [PubMed] [Google Scholar]
- 15.McDermott RA, Schmidt BA, Sinha A, Mills P. Improving diabetes care in the primary healthcare setting: A randomised cluster trial in remote indigenous communities. Med J Aust. 2001;174(10):497–502. doi: 10.5694/j.1326-5377.2001.tb143397.x. [DOI] [PubMed] [Google Scholar]
- 16.McDermott R, Tulip F, Schmidt B, Sinha A. Sustaining better diabetes care in remote indigenous Australian communities. BMJ. 2003;327(7412):428–430. doi: 10.1136/bmj.327.7412.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DePue JD, Rosen RK, Batts-Turner M, et al. Cultural translation of interventions: Diabetes care in American Samoa. Am J Public Health. 2010;100(11):2085–2093. doi: 10.2105/AJPH.2009.170134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DePue JD, Dunsiger S, Seiden AD, Blume J, Rosen RK, Goldstein MG, Nu’solia O, Tuitele J, McGarvey ST. Nurse-community health worker team improves diabetes care in American Samoa: results of a randomized controlled trial. Diabetes Care. 2013;36(7):1947–53. doi: 10.2337/dc12-1969. Epub 2013 Feb 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gary TL, Batts-Turner M, Bone LR, et al. A randomized controlled trial of the effects of nurse case manager and community health worker team interventions in urban African-Americans with type 2 diabetes. Control Clin Trials. 2004;25(1):53–66. doi: 10.1016/j.cct.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 20.Fedder DO, Chang RJ, Curry S, Nichols G. The effectiveness of a community health worker outreach program on healthcare utilization of west Baltimore City Medicaid patients with diabetes, with or without hypertension. Ethn Dis. 2003;13(1):22–7. [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. The road to health toolkit. Atlanta, GA: U.S.: Department of Health and Human Services, Centers for Disease Controland Prevention; 2010. [Google Scholar]
- 22.AADE. AADE7 Self-Care Behaviors. Diabetes Educ. 2008;34:445–449. doi: 10.1177/0145721708316625. [DOI] [PubMed] [Google Scholar]
- 23.DePue JD, Rosen RK, Seiden A, Bereolos N, Chima ML, Goldstein MG, Nu’usolia O, Tuitele J, McGarvey ST. Implementation of a culturally tailored diabetes intervention with community health workers in American Samoa. Diabetes Educ. 2013 doi: 10.1177/0145721713504630. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Diabetes Association. Standards of medical care in diabetes--2011. Diabetes Care. 2011;34 (Suppl 1):S11–61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DCA 2000TM+ analyzer. West Haven, CT: Bayer Diagnostics Division; [Accessed 5 Sept 2005]. 2000. Available from http://www.bayerdiag.com. [Google Scholar]
- 26.Carter JS, Houston CA, Gilliland SS, et al. Rapid HbA1c testing in a community setting. Diabetes Care. 1996;19:764–767. doi: 10.2337/diacare.19.7.764. [DOI] [PubMed] [Google Scholar]
- 27.Brown SA, Becker HA, Garcia AA, Barton SA, Hanis CL. Measuring health beliefs in Spanish-speaking Mexican Americans with type 2 diabetes: Adapting an existing instrument. Res Nurs Health. 2002;25(2):145–158. doi: 10.1002/nur.10023. [DOI] [PubMed] [Google Scholar]
- 28.Norris SL, Chowdhury FM, Van Le K, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;23(5):544–556. doi: 10.1111/j.1464-5491.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- 29.Hill-Briggs F, Batts-Turner M, Gary TL, et al. Training community health workers as diabetes educators for urban African Americans: value added using participatory methods. Prog Community Health Partnersh. 2007;1(2):185–193. doi: 10.1353/cpr.2007.0008. [DOI] [PubMed] [Google Scholar]
- 30.Gibbons MC, Tyus NC. Systematic review of U.S.-based randomized controlled trials using community health workers. Prog Community Health Partnersh. 2007;1(4):371–381. doi: 10.1353/cpr.2007.0035. [DOI] [PubMed] [Google Scholar]
- 31.Davidson MB. The effectiveness of nurse- and pharmacist-directed care in diabetes disease management: a narrative review. Curr Diabetes Rev. 2007;3(4):280–286. doi: 10.2174/157339907782330058. [DOI] [PubMed] [Google Scholar]