Abstract
Background
A sentinel lymph node (SLN) biopsy using superparamagnetic iron oxide nanoparticles (SPIOs) as a tracer instead of radioisotopes was first applied successfully in breast cancer. This study determined the feasibility of this new technique using SPIOs and a handheld magnetometer to detect SLNs in prostate cancer (PC).
Methods
Enrolled 20 patients with intermediate and high-risk PC (PSA >10 and/or Gleason score >7) in a prospective study (12/2013–1/2014; DRKS00005473), following an ethics committee approval. After transrectal intraprostatic SPIOs injection a day earlier, patients (19/20) underwent magnetometer-guided sentinel lymphadenectomy (sPLND) and extended PLND, followed by radical prostatectomy. One patient was not operated because of an unrelated coagulation disorder. The ex vivo magnetic activity of all lymph nodes (LNs) removed was measured. The detection rate, rate of in vivo detected SLNs, and sensitivity of sPLND was established.
Results
No adverse events attributable to SPIOs injection were observed. Identified 126 SLNs (median 7, IQR 4–9) and resected 334 LNs (median 17, IQR 14–19); 37 % (7/19) of the patients had LN metastases (median 1, IQR 1–3.5). The detection rate and rate of in vivo detected SLNs were 90 % (17/19) and 94 % (118/126) respectively. Using sPLND, all LN metastases were detected (15/15, sensitivity 100 %) in all patients identified with SLNs. One LN + patient showed no SLNs following transurethral prostate resection.
Conclusions
This is the first study using a magnetic tracer and magnetometer to detect SLNs in PC. Initial data indicate that this simple, radiation-free procedure is safe, feasible, and reliably identifies SLN and LN metastases in most patients.
The lymph node (LN) status serves as a key predictor for clinically localised prostate cancer (PC). In addition, reliable information on the presence or spread of lymphogenous metastasizing is of great importance for optimally directing adjuvant therapy. Pelvic lymph node dissection (PLND) is currently the most accurate LN staging procedure for patients with clinically localised PC. Despite advances in radiologic imaging, none of the available means of radiologic imaging provides an equivalent level of sensitivity for the detection of LN involvement in PC patients. Moreover, the role of PLND as a therapeutic intervention has been the focus of renewed interest. Several reports indicate that PLND improves biochemical relapse-free survival, especially in patients with minimal lymphatic dissemination.1,2
High sensitivity for identification of LN metastases could be demonstrated for a sentinel PLND (sPLND) in PC and other carcinomas.3–5 The procedure offers the advantage of targeted removal of relatively few LNs, which also means lower morbidity.6,7
As established for breast cancer, for example, conventional use involves radioactive marking of SLNs with 99mTechnetium nanocolloid for PC patients and a handheld gamma probe for intraoperative detection.8,9 A radioactive tracer, however, is associated with problems. This procedure depends on the availability of nuclear medicine and radio tracers, which in recent years have been problematic because of cutbacks in production. Furthermore, the main issue is the radioactive exposure of patients and healthcare staff. This calls for the development of new, simpler, radiation-free, but accurate methods, for SLN marking and intraoperative detection—especially those that a urologist can apply independently without the complicated and problematic logistics associated with nuclear medicine.
For the aforementioned reasons, others tested a method for identifying SLNs in breast cancer by using superparamagnetic iron oxide (SPIO) nanoparticles.10 It was shown that after a subcutaneous injection, these particles flow to the SLNs and iron deposition is seen predominantly within sinuses and macrophages.11 This resulted in the development of a system comprising a magnetic tracer (Sienna+®) and a handheld magnetometer (SentiMag®). In two multi-centre and multinational studies, it was possible to demonstrate that for breast cancer, the new procedure is not inferior to the established procedure of marking and detection of SLNs using 99mTechnetium nanocolloid and a gamma probe.12,13 This new radiation-free technology for marking and intraoperative detection of SLNs has not yet been evaluated for the prostate.
This is the first study in which SPIOs were injected transrectally into the prostate to mark SLNs, and a handheld magnetometer was used for intraoperative identification of SLNs. In addition to the safety and functionality of the system for intraoperative detection of SLNs following transrectal injection of Sienna+®, this study also looked at the sensitivity of the method in determining LN metastases versus an extended PLND (ePLND).
Methods
Study Design
The prospective, “SentiMagPro” pilot study applied the concept of a novel technique for intraoperative SLN detection, using SPIO nanoparticles and a handheld magnetometer in PC patients. The protocol (German Clinical Trials Register: DRKS00005473) was approved by the ethics committee of the Medical Chamber of Lower Saxony, Germany. Twenty patients with intermediate or high-risk PC scheduled for open radical retropubic prostatectomy and PLND participated in this study conducted between 3 December 2013 and 27 January 2014. Inclusion criteria were a prostate-specific antigen (PSA) level >10.0 ng/ml and/or a Gleason sum ≥7. Patients excluded were those with known intolerance or hypersensitivity to iron or dextran compounds, with iron overload disease, or with pacemakers or other implantable devices in the chest wall. Patients were informed in writing or orally, and those recruited gave their consent in writing.
The SentiMag® Technique
The SentiMag® system (Endomagnetics Ltd, UK) for marking and identifying SLNs comprises a handheld magnetometer, the SentiMag® unit itself, and the Sienna+® magnet tracer (Endomagnetics Ltd, UK). Both are CE certified as class IIa medical devices. The size of Sienna+® particles (60 nm) is similar to that of 99mTechnetium nanocolloid but more homogeneous. In 99mTechnetium nanocolloid, 95 % of the particles are >80 nm in size, 4 % lie between 80 and 100 nm, and 1 % are >100 nm. Sienna+® has comparable functional properties, because upon injection the tracer flows just like a radio nuclide through the lymph system and gets trapped in the SLNs (Fig. 1). Its characteristic dark brown discolouration could help further identify SLNs (Fig. 2).
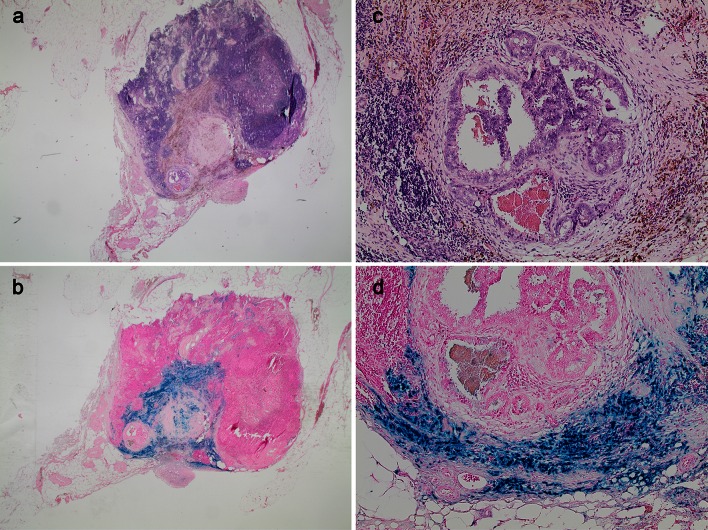
Fig. 1.
Examples of a sentinel lymph node and, in the centre of the image, a 4-mm metastasis of a Gleason 8 prostate cancer after haematoxylin and eosin (H&E) (a and c) and Perl’s Prussian blue (b and d) staining showing the brown and blue discolouration of the absorbed iron oxide nanoparticles in the surrounding lymphatic tissue
Fig. 2.

Brown discoloured sentinel lymph node from the absorbed iron oxide nanoparticles
Tracer Injection
The sentinel technique in PC differs from those in other tumor entities. In breast cancer and malignant melanoma, a well-directed peritumoral injection is only placed to observe the lymphatic drainage of the tumor. In PC, which occurs commonly multifocal, it is not known with absolute certainty from which part of the organ the metastatic spread originates. The currently available imaging or randomized prostate biopsy does not allow a completely reliable localization of all cancer foci in the prostate. Therefore, the goal of prostate lymph scintigraphy must be the imaging of all primary draining LNs of the prostate, under which the SLN of cancer also exist.
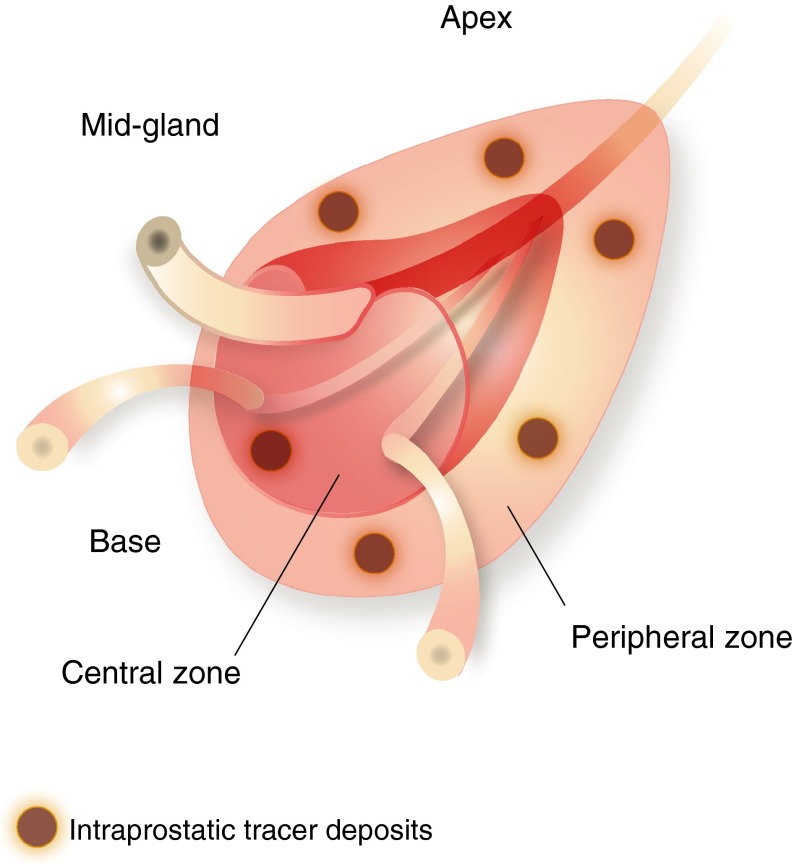
In this study, a urologist injected a total of 2 ml of Sienna+® into prostates of patients 1 day before surgery, on average 20 h before SLN detection (IQR 19–21 h), using transrectal ultrasound guidance. Based on our own examinations and those of others, the tracer was evenly spread as three peripheral deposits on each side (Fig. 3).14,15 Any adverse events, complications, or reactions were noted.
Fig. 3.
Schematic illustration of Sienna+® injection. The magnetic tracer (total of 2 ml) were injected transrectally in three deposits each on both sides of the prostate’s peripheral zone, using ultrasound guidance
Intraoperative Procedures, Histopathology
Patients underwent magnetometer (SentiMag®)-guided sPLND and ePLND, followed by radical retropubic prostatectomy. All cases were performed by two different high-volume surgeons, who applied the same anatomic template during ePLND. The ePLND template included the area along the external iliac vessels, with the distal limit the femoral canal. Proximally, ePLND was performed to and including the bifurcation of the common iliac artery. All lymphatic fatty tissue along the internal iliac artery and within the obturator fossa and the area dorsal of the obturator nerve was removed, as described by Weingärtner et al..16 The lateral limit consisted of the pelvic sidewall and the medial dissection limit was defined by perivesical fat.
During sPLND, all metal retractors were removed from the surgical field and polymer retractors (SUSI®, Aesculap®; B. Braun Melsungen AG, Germany) were used to avoid any kind of interference with the magnetometer when detecting SLNs with the SentiMag® probe. All SLNs detected by the SentiMag® were removed, whereby each magnetically active LN was seen as a SLN. For surgical reasons, LNs other than SLNs directly adjoining and adhering to SLNs also were removed, if an in situ separation was not possible. In this case, the LNs were ex vivo macroscopically detected (tactile and visual) and separated by the surgeon from each other or from the containing fibrofatty tissue. Thereafter, an ePLND was conducted to remove the remaining lymphatic fatty tissue from the above-named regions. Afterwards, the LNs were macroscopically detected and separated by the surgeon from the containing fibrofatty tissue, too.
The magnetic activity of all LNs also was measured ex vivo with the SentiMag® (Fig. 4). This involved separating and registering any directly adjacent SLNs, whose signal could not be differentiated intraoperatively. In addition, we noted the tracer discolouration of SLNs and measured the magnetic activity of the prostate.
Fig. 4.

Ex vivo magnetic activity of a sentinel lymph node measured with a handheld magnetometer (SentiMag®)
Postoperatively, all LNs detected and separated by the surgeon (SLNs and non-SLNs) were initially cut in 3-mm transverse sections, routinely processed and completely embedded in paraffin, whereas 4–5-µm-thick sections were stained with hematoxylin-eosin.
Analysis
A successful procedure was defined as an intraoperative detection of at least one SLN by the SentiMag® magnetometer. This served to determine the detection rate (number of patients with detected SLNs/total number operated). Also computed was the rate of SLNs correctly detected in vivo by the SentiMag® (number of SLNs detected in vivo/number of SLNs detected ex vivo), along with the sensitivity of sPLND (number of positive SLNs/total number of positive LNs).
Results
Table 1 lists the summary of patient characteristics. None of the 20 patients exhibited adverse events attributable to the injection of Sienna+®. One patient could not be operated because of a newly found, unrelated coagulation disorder that was not known during the preliminary examination. A total of 126 SLNs (median 7, IQR 4–9) were identified, and in all 334 LNs (median 17, IQR 14–19) were removed. LN metastases were found in 7 of the 19 patients operated (37 %), with a median of one positive LN (IQR 1–3.5). Of the LN metastases, 25 % each were localised in the area of the obturator fossa and hypogastric region and 50 % in region of the external iliac vessels.
Table 1.
Patient characteristics and number of sentinel lymph nodes detected by using superparamagnetic iron oxide nanoparticles and a handheld magnetometer
| Age [year] | Preoperative PSA [ng/ml] | cT | Preoperative Gleason score | pT | pN | Postoperative Gleason score | LNs removed | SLNs removed | LNs with metastasis | SLNs with metastasis | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 67 | 16.59 | T1c | 7 (4 + 3) | pT3b | N1 | 7 (3 + 4) | 11 | 10 | 5 | 5 |
| 2 | 61 | 17.9 | T2b | 7 (3 + 4) | pT3b | N0 | 7 (4 + 3) | 16 | 3 | 0 | 0 |
| 3 | 63 | 1.31 | T2c | 7 (4 + 3) | pT3b | N0 | 7 (4 + 3) | 23 | 14 | 0 | 0 |
| 4 | 63 | 50.5 | T2b | 7 (3 + 4) | pT2c | N0 | 7 (4 + 3) | 14 | 5 | 0 | 0 |
| 5 | 65 | 4.97 | T1c | 7 (3 + 4) | pT2c | N0 | 7 (3 + 4) | 15 | 0 | 0 | 0 |
| 6 | 53 | 9.16 | T1c | 7 (3 + 4) | pT2a | N0 | 7 (3 + 4) | 13 | 5 | 0 | 0 |
| 7 | 66 | 11.31 | T1c | 7 (3 + 4) | pT3a | N1 | 7 (3 + 4) | 11 | 7 | 1 | 1 |
| 8 | 66 | 7.9 | T1c | 7 (3 + 4) | pT2c | N0 | 7 (3 + 4) | 14 | 5 | 0 | 0 |
| 9 | 55 | 5.86 | T2b | 7 (4 + 3) | pT2c | N0 | 7 (4 + 4) | 17 | 4 | 0 | 0 |
| 10 | 63 | 6.12 | T1c | 7 (3 + 4) | pT2c | N0 | 7 (3 + 4) | 17 | 9 | 0 | 0 |
| 11* | 75 | 12.2 | T2c | 7 (3 + 3) | pT3b | N1 | 7 (4 + 3) | 18 | 0 | 1 | 0 |
| 12 | 67 | 19.63 | T1c | 6 (3 + 3) | pT2a | N0 | 7 (3 + 4) | 19 | 7 | 0 | 0 |
| 13 | 64 | 12.9 | T1c | 6 (3 + 3) | pT2c | N0 | 7 (3 + 4) | 19 | 12 | 0 | 0 |
| 14 | 63 | 48.68 | T3a | 7 (4 + 3) | pT4 | N1 | 9 (4 + 5) | 32 | 2 | 1 | 1 |
| 15 | 68 | 12.1 | T2b | 7 (4 + 3) | pT3b | N1 | 9 (4 + 5) | 15 | 12 | 5 | 5 |
| 16 | 78 | 4.88 | T2c | 8 (4 + 4) | pT3b | N1 | 8 (4 + 4) | 19 | 7 | 2 | 2 |
| 17$ | 72 | 14.5 | T2a | 7 (4 + 3) | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| 18 | 68 | 29.18 | T2c | 10 (5 + 5) | pT3b | N1 | 9 (4 + 5) | 23 | 9 | 1 | 1 |
| 19 | 72 | 30.97 | T2c | 7 (3 + 4) | pT3a | N0 | 7 (4 + 3) | 24 | 8 | 0 | 0 |
| 20 | 53 | 13.98 | T1c | 7 (3 + 4) | pT2c | N0 | 7 (3 + 4) | 14 | 7 | 0 | 0 |
| Median | 65.5 | 12.55 | 17 | 7 | 1§ | 1.5§ |
PSA prostate specific antigen; c clinical values; p pathological values; LN lymph node; SLN sentinel lymph node
* This patient had undergone a transurethral prostate resection in the past
$ This patient did not undergo prostatectomy and lymphadenectomy
§ Patients with lymph node metastases
SLNs were detected in 17 of the 19 patients operated (median 7, IQR 5–9), which equals a detection rate of 90 %. SLNs were not found in either one LN positive patient after transurethral prostate resection, or in a case of long-term transurethral catheter with a relapsing infection. SentiMag® correctly detected 118 (94 %) of SLNs in vivo from among 126 magnetically active LNs identified ex vivo. In one case, a SLN could not be detected in vivo because of an existing hip endoprosthesis. The other (n = 7) undetected SLNs lay mostly close to the prostate.
In all patients with SLNs and positive LNs (6/6), metastases (15/15) were exclusively detected in SLNs identified in vivo by SentiMag®, which means a 100 % sensitivity of magnetometer-guided sPLND. Moreover, a LN metastasis without SLN identification was found in one patient after transurethral prostate resection. See Table 1 for details by patients of the number of LNs and LN metastases removed.
All prostates were magnetically active, with maximum activity measured between 4,143 and >9,999 units. The SLNs showed a median magnetic activity level of 338 units (IQR 127–950), whereby the activity of positive SLNs was a median of 443 units (IQR 127–950). Only 18.3 % (23/126) of the SLNs exhibited macroscopically clearly visible brown discolouration.
Discussion
Based on several thousand patients, radioguided sPLND using 99mTechnetium nanocolloid has been found to be highly sensitive for identifying LN metastases in PC patients.3,4,17 It was possible to demonstrate that for a sPLND, the rate of LN involvement was higher in a sentinel cohort than was expected from the European Association of Urology guideline nomogram.17 In the SentiMag® study, the rate of LN positive patients (37 %) is comparatively high, despite the intermediate and high-risk profile of patients. The possibility of an ePLND overlooking a part of the LN metastases, possibly in the presacral region, is overcome by being able to detect it through the sPLND. Reportedly, Joniau et al. 18 did not detect 13 % of metastatic LNs by applying only conventional standard ePLND.
Moreover, the targeted sentinel procedure has the advantage, versus an ePLND, that relatively few LNs must be removed. This consequently minimizes the intervention and significantly reduces the histopathology. A lower number of LNs can be explored more extensively. For example, more small or micrometastases can be detected by increasing the number of sections.
In the meantime, efforts are underway on targeted removal of LNs in combination with laparoscopic or robot-assisted radical prostatectomies, in order to lower the extensive effort associated with an ePLND.19–21
The morbidity of PLND is still under debate. However, in this context it should be considered that the complications of PLND increase significantly with the number of dissected LNs, as shown previously by different studies.6 In a study of our working group, it was shown that the total and lymphatic complications increased significantly if more than15 LNs have been dissected, and that sPLND, despite the dissection of SLNs in regions with difficult accessibility (e.g., presacral), has a low morbidity.7 Many of these complications are not serious, but in some cases, considerable therapeutic additional effort is required.
Nevertheless, the pros of conventional radioactive marking with 99mTechnetium nanocolloid also come with some cons. For instance, the technology is subject to strict regulations and problems involving the presence of nuclear medicine. Also, there are concerns regarding the availability of 99mTechnetium nanocolloid, because its parent isotope, 99mMo, is produced in only a few reactors worldwide. These have not been fully operational in recent years, which has led to big bottlenecks and interruption of supplies. Worthy of mention are the problems of radiation exposure of patients and healthcare staff, as well as inherent problems with the production and disposal of radioactive materials.
For the above reasons, this is the first study that concentrated on a new, nonradioactive, purely magnetic technology using handheld magnetometers for SLN marking and intraoperative detection in PC patients. Earlier, it was possible to demonstrate that, for breast cancer, this Sienna+®/SentiMag® system was not inferior to the established procedure of marking with 99mTechnetium nanocolloid.12,13
In this prospective pilot study, we were able to show, for the first time, that magnetic marking and intraoperative detection of SLNs and the Sienna+®/SentiMag® system are suited for the prostate. Although this feasibility study was applied for the first time ever to the prostate, the detection rate of 90 % was comparably high. The first examinations of breast cancer detected only 77 % of the SLNs following marking with SPIOs.22 The multi-centre trials of breast cancer came up with a detection rate of 94 and 98 %.12,13 For the prostate, a meta-analysis of 99mTechnetium nanocolloid guided sPLND showed a pooled detection rate of 94 %.4 In contrast, Manny et al. observed a detection rate of only 76 % with indocyanine green (ICG) fluorescence marking, whereas the in vivo detection rate of SLNs with the SentiMag® probe was high (94 %).21 For example, despite application of a hybrid tracer (ICG-99mTechnetium nanocolloid), van der Poel et al. 20 could not detect 15 % of the SLNs intraoperative. In the SentiMagPro study More SLNs (median 7) were detected (median of 2 SLNs) than in our studies with 99mTechnetium nanocolloid (median 5–6 SLNs) or by others with hybrid tracers.9,17,20
In the SentiMagPro study, we were able to identify 100 % of the LN metastases in patients with SLNs detected by magnetometer guided sPLND. One patient, who had undergone transurethral prostate resection and in whom no SLN was detectable, a LN metastasis was resected with ePLND. In a meta-analysis, Sadeghi et al.4 found the pooled sensitivity of radio-guided sPLND to be 94 %.
Beyond the high detection reliability of the SentiMag® system, one should weigh the fact that the radiation-free, magnetometer-guided sPLND procedure is simple and can be performed alone by a urologist. In contrast, in recent years alternatives to the deployment of 99mTechnetium nanocolloid for the prostate have been tested in combination with laparoscopy or robotic radical prostatectomy fluorescence (ICG)-based or coupled procedures (ICG-99mTechnetium nanocolloid) that are either quite extensive or again involve radioactivity.19,21,23 Moreover, these techniques are principally restricted by the limited tissue penetration of near-infrared fluorescence signals (<1 cm) and the functional properties of the free ICG.24,25 Functionally, ICG is a rapidly clearing lymphatic perfusions marker, which does not remain in the SLNs like the radiocolloid and/or is not absorbed there like the latter by macrophages.26 Furthermore, the fluorescence approach for open operations means a much more complex effort and higher costs.24,27,28
Magnetic tracers have another big advantage over other techniques because of the ability to visualise them through magnetic resonance imaging (MRI). Although Sienna+® itself has not been approved as a contrast agent, its properties are comparable with those of other SPIOs deployed as negative contrast agents in MRI for identifying (S)LN metastases.29,30
In addition to limitations related to magnetism, such as the presence of endoprostheses, this new technique also has the same principal limitations of the sentinel method. As with radioactive marking, tissue changes resulting from a transurethral prostate resection or subsided inflammations (as was the situation for both SLN negative patients in this study) could hinder the flow of lymph fluids from the prostate and thereby the SLN marking.3,8,9
In view of the aforementioned issues, and because an ePLND is required in such cases without identification of SLN metastases, these initial findings suggest deployment of the Sienna+®/SentiMag® system or a magnetometer-guided sPLND for prostate carcinomas. This is further underscored by the fact that this procedure offers a level of confidence for identification of LN metastases equivalent to that of conventional radioactive marking. More work is needed to confirm the highly promising findings of this feasibility study and to answer open questions, for example, through direct comparison with conventional radioactive marking or other tracers.
Conclusions
This prospective, clinical, pilot study delivered the first convincing results on magnetic marking and magnetometer-guided sPLND in PC. The procedure appears to be safe, can be performed easily and alone by a urologist, and has the advantage of no radioactive elements. Should these initial findings including the technique’s high sensitivity for identifying metastases be validated in a larger or multicentre study, the new technique could have the potential to achieve targeted improvements in LN surgery in PC—at a comparably low level of effort.
Acknowledgments
None.
Disclosure of Commercial Interest
None of the authors have any conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript.
References
- 1.Withrow DR, DeGroot JM, Siemens DR, Groome PA. Therapeutic value of lymph node dissection at radical prostatectomy: a population-based case-cohort study. BJU Int. 2011;108:209–216. doi: 10.1111/j.1464-410X.2010.09805.x. [DOI] [PubMed] [Google Scholar]
- 2.Schumacher MC, Burkhard FC, Thalmann GN, Fleischmann A, Studer UE. Good outcome for patients with few lymph node metastases after radical retropubic prostatectomy. Eur Urol. 2008;54:344–352. doi: 10.1016/j.eururo.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 3.Holl G, Dorn R, Wengenmair H, Weckermann D, Sciuk J. Validation of sentinel lymph node dissection in prostate cancer: experience in more than 2,000 patients. Eur J Nucl Med Mol Imaging. 2009;36:1377–1382. doi: 10.1007/s00259-009-1157-2. [DOI] [PubMed] [Google Scholar]
- 4.Sadeghi R, Tabasi KT, Bazaz SM, et al. Sentinel node mapping in the prostate cancer. Meta-analysis. Nuklearmedizin. 2011;50:107–115. doi: 10.3413/nukmed-0339-10-07. [DOI] [PubMed] [Google Scholar]
- 5.Straver ME, Meijnen P, van Tienhoven G, et al. Sentinel node identification rate and nodal involvement in the EORTC 10981-22023 AMAROS trial. Ann Surg Oncol. 2010;17(7):1854–1861. doi: 10.1245/s10434-010-0945-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Musch M, Klevecka V, Roggenbuck U, et al. Complications of pelvic lymphadenectomy in 1,380 patients undergoing radical retropubic prostatectomy between 1993 and 2006. J Urol. 2008;179:923–928. doi: 10.1016/j.juro.2007.10.072. [DOI] [PubMed] [Google Scholar]
- 7.Winter A, Vogt C, Weckermann D, Wawroschek F. Complications of pelvic lymphadenectomy in clinically localised prostate cancer: different techniques in comparison and dependency on the number of removed lymph nodes. Aktuelle Urol. 2011;42:179–183. doi: 10.1055/s-0031-1271389. [DOI] [PubMed] [Google Scholar]
- 8.Wawroschek F, Vogt H, Weckermann D, Wagner T, Harzmann R. The sentinel lymph node concept in prostate cancer - first results of gamma probe-guided sentinel lymph node identification. Eur Urol. 1999;36:595–600. doi: 10.1159/000020054. [DOI] [PubMed] [Google Scholar]
- 9.Wawroschek F, Vogt H, Weckermann D, Wagner T, Hamm M, Harzmann R. Radioisotope guided pelvic lymph node dissection for prostate cancer. J Urol. 2001;166:1715–1719. doi: 10.1016/S0022-5347(05)65659-5. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed M, de Rosales RT, Douek M. Preclinical studies of the role of iron oxide magnetic nanoparticles for nonpalpable lesion localization in breast cancer. J Surg Res. 2013;185:27–35. doi: 10.1016/j.jss.2013.05.108. [DOI] [PubMed] [Google Scholar]
- 11.Johnson L, Pinder SE, Douek M. Deposition of superparamagnetic iron-oxide nanoparticles in axillary sentinel lymph nodes following subcutaneous injection. Histopathology. 2013;62:481–486. doi: 10.1111/his.12019. [DOI] [PubMed] [Google Scholar]
- 12.Douek M, Klaase J, Monypenny I, et al. Sentinel node biopsy using a magnetic tracer versus standard technique: the SentiMAG multicentre trial. Ann Surg Oncol. 2014;23:175–179. doi: 10.1245/s10434-013-3379-6. [DOI] [PubMed] [Google Scholar]
- 13.Thill M, Kurylcio A, Welter R, et al. The Central-European SentiMag study: sentinel lymph node biopsy with superparamagnetic iron oxide (SPIO) vs. radioisotope. Breast. 2014;23:175–179. doi: 10.1016/j.breast.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Wawroschek F, Wengenmair H, Senekowitsch-Schmidtke R, et al. Prostate lymphoscintigraphy for sentinel lymph node identification in canines: reproducibility, uptake, and biokinetics depending on different injection strategies. Urol Res. 2003;31:152–158. doi: 10.1007/s00240-003-0307-4. [DOI] [PubMed] [Google Scholar]
- 15.Buckle T. Brouwer OR, Valdés Olmos RA, van der Poel HG, van Leeuwen FW. Relationship between intraprostatic tracer deposits and sentinel lymph node mapping in prostate cancer patients. J Nucl Med. 2012;53:1026–1033. doi: 10.2967/jnumed.111.098517. [DOI] [PubMed] [Google Scholar]
- 16.Weingärtner K, Ramaswamy A, Bittinger A, Gerharz EW, Vöge D, Riedmiller H. Anatomical basis for pelvic lymphadenectomy in prostate cancer: results of an autopsy study and implications for the clinic. J Urol. 1996;156:1969–1971. doi: 10.1016/S0022-5347(01)65406-5. [DOI] [PubMed] [Google Scholar]
- 17.Winter A, Kneib T, Henke RP, Wawroschek F. Sentinel lymph node dissection in more than 1200 prostate cancer cases: rate and prediction of lymph node involvement depending on preoperative tumor characteristics. Int J Urol. 2014;21:58–63. doi: 10.1111/iju.12184. [DOI] [PubMed] [Google Scholar]
- 18.Joniau S, Van den Bergh L, Lerut E, Deroose CM, Haustermans K, Oyen R, Budiharto T, Ameye F, Bogaerts K, Van Poppel H. Mapping of pelvic lymph node metastases in prostate cancer. Eur Urol. 2013;63:450–458. doi: 10.1016/j.eururo.2012.06.057. [DOI] [PubMed] [Google Scholar]
- 19.Jeschke S, Lusuardi L, Myatt A, Hruby S, Pirich C, Janetschek G. Visualisation of the lymph node pathway in real time by laparoscopic radioisotope- and fluorescence-guided sentinel lymph node dissection in prostate cancer staging. Urology. 2012;80:1080–1086. doi: 10.1016/j.urology.2012.05.050. [DOI] [PubMed] [Google Scholar]
- 20.Van der Poel HG, Buckle T, Brouwer OR, Valdés Olmos RA, van Leeuwen FW. Intraoperative laparoscopic fluorescence guidance to the sentinel lymph node in prostate cancer patients: clinical proof of concept of an integrated functional imaging approach using a multimodal tracer. Eur Urol. 2011;60:826–833. doi: 10.1016/j.eururo.2011.03.024. [DOI] [PubMed] [Google Scholar]
- 21.Manny TB, Patel M, Hemal AK. Fluorescence-enhanced robotic radical prostatectomy using real-time lymphangiography and tissue marking with percutaneous injection of unconjugated indocyanine green: the initial clinical experience in 50 patients. Eur Urol. 2013 Nov 21. doi: 10.1016/j.eururo.2013.11.017. [DOI] [PubMed]
- 22.Shiozawa M1, Kobayashi S, Sato Y, et al. Magnetic resonance lymphography of sentinel lymph nodes in patients with breast cancer using superparamagnetic iron oxide: a feasibility study. BreastCancer. 2012 Aug 28. [DOI] [PubMed]
- 23.Van den Berg NS, Valdés-Olmos RA, van der Poel HG, van Leeuwen FW. Sentinel lymph node biopsy for prostate cancer: a hybrid approach. J Nucl Med. 2013;54:493–496. doi: 10.2967/jnumed.112.113746. [DOI] [PubMed] [Google Scholar]
- 24.Van den Berg NS, van Leeuwen FW, van der Poel HG. Fluorescence guidance in urologic surgery. Curr Opin Urol. 2012;22:109–120. doi: 10.1097/MOU.0b013e3283501869. [DOI] [PubMed] [Google Scholar]
- 25.Van Leeuwen AC, Buckle T, Bendle G, et al. Tracer-cocktail injections for combined pre- and intraoperative multimodal imaging of lymph nodes in a spontaneous mouse prostate tumor model. J Biomed Opt. 2011;16:016004. doi: 10.1117/1.3528027. [DOI] [PubMed] [Google Scholar]
- 26.Faries MB, Bedrosian I, Reynolds C, Nguyen HQ, Alavi A, Czerniecki BJ. Active macromolecule uptake by lymph node antigen-presenting cells: a novel mechanism in determining sentinel lymph node status. Ann Surg Oncol. 2000;7:98–105. doi: 10.1007/s10434-000-0098-6. [DOI] [PubMed] [Google Scholar]
- 27.Troyan SL, Kianzad V, Gibbs-Strauss SL, et al. The FLARE intraoperative near-infrared fluorescence imaging system: a first-in-human clinical trial in breast cancer sentinel lymph node mapping. Ann Surg Oncol. 2009;16:2943–2952. doi: 10.1245/s10434-009-0594-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brouwer OR, van den Berg NS, Mathéron HM, et al. A hybrid radioactive and fluorescent tracer for sentinel node biopsy in penile carcinoma as a potential replacement for blue dye. Eur Urol. 2014;65:600–609. doi: 10.1016/j.eururo.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 29.Fortuin AS, Smeenk RJ, Meijer HJ, Witjes AJ, Barentsz JO. Lymphotropic nanoparticle-enhanced MRI in prostate cancer: value and therapeutic potential. Curr Urol Rep. 2014;15:389. doi: 10.1007/s11934-013-0389-7. [DOI] [PubMed] [Google Scholar]
- 30.Motomura K, Ishitobi M, Komoike Y, et al. SPIO-enhanced magnetic resonance imaging for the detection of metastases in sentinel nodes localized by computed tomography lymphography in patients with breast cancer. Ann Surg Oncol. 2011;18:3422–3429. doi: 10.1245/s10434-011-1710-7. [DOI] [PubMed] [Google Scholar]