Abstract
Objective
Posterior accessed lumbar interbody fusion (PALIF) has a clear objective to restore disc height and spinal alignment but surgeons may occasionally face the converse situation and lose lumbar lordosis. We analyzed retrospective data for factors contributing to a postoperative flat back.
Methods
A total of 105 patients who underwent PALIF for spondylolisthesis and stenosis were enrolled. The patients were divided according to surgical type [posterior lumbar inter body fusion (PLIF) vs. unilateral transforaminal lumbar interbody fusion (TLIF)], number of levels (single vs. multiple), and diagnosis (spondylolisthesis vs. stenosis). We measured perioperative index level lordosis, lumbar lordosis, pelvic tilt, sacral slope, pelvic incidence, and disc height in standing lateral radiographs. The change and variance in each parameter and comparative group were analyzed with the paired and Student t-test (p<0.05), correlation coefficient, and regression analysis.
Results
A significant perioperative reduction was observed in index-level lordosis following TLIF at the single level and in patients with spondylolisthesis (p=0.002, p=0.005). Pelvic tilt and sacral slope were significantly restored following PLIF multilevel surgery (p=0.009, p=0.003). Sacral slope variance was highly sensitive to perioperative variance of index level lordosis in high sacral sloped pelvis. Perioperative variance of index level lordosis was positively correlated with disc height variance (R2=0.286, p=0.0005).
Conclusion
Unilateral TLIF has the potential to cause postoperative flat back. PLIF is more reliable than unilateral TLIF to restore spinopelvic parameters following multilevel surgery and spondylolisthesis. A high sacral sloped pelvis is more vulnerable to PALIF in terms of a postoperative flat back.
Keywords: Spinal curvatures, Spinal fusion, Postoperative complication, Flat back
INTRODUCTION
Spinal surgeons previously carried out posterior accessed lumbar fusion (PALIF) with internal instrumentation and bone grafts to stabilize an unstable lumbar spinal segment and reinforce iatrogenic spinal instability3). Thus, many and variously shaped interbody cages have been developed for PALIF. The surgical purposes of PALIF include restoring disc height and establishing quick interbody fusion to correct coronal and sagittal imbalances3). Posterior lumbar interbody fusion (PLIF) or unilateral transforaminal lumbar interbody fusion (TLIF) restores spinal stability and disc height quicker compared with posterolateral lumbar fusion7,8,9,10,18,25,26). Despite establishing the ultimate aim of stable bony fusion, optimal lumbar lordosis could not be achieved with this surgery. Although spinal surgeons often achieve the PALIF objective, they are usually faced with a situation to restore disc height only to lose the original lumbar lordosis and index level lordosis. Thus, we retrospectively analyzed factors that contributed to postoperative flat back in cases of PALIF.
MATERIALS AND METHODS
All patients with severe lumbar spinal stenosis graded C and above and spondylolisthesis and severe foraminal stenosis graded 3 were enrolled and underwent PLIF or TLIF from July 2007 to September 2011. This was a continuous, non-randomized, single center retrospective study of all patients. This study was approved by the Ethics Committee of Eulji University in 2007 and 2011. Patients were operated on by the same surgeon using an identical surgical procedure.
The PLIF includes both sides of hemilaminectomy, the medial and upper resection of superior facet of adjacent lower segment, decompression of relevant nerve roots and thecal sac, the removal of both sides of nucleus pulposus and annulus fibrosus. It allows as broad area of interbody fusion as possible and releases segmental stiffness enough. After the insertion of autologous graft and cage, posterior compressive shortening of screw fixation were conducted. The PLIF in this study was performed not only with the early concept of old type PLIF but also with having the sight of current TLIF, so that preserving superior lamina and spinous process. Whereas TLIF taking unilateral approach inserting the cage in the anterior column of intervertebral space and conducting the interbody fusion with autologous graft and the opposite interfacet bone fusion. In this study, the PLIF is bilateral version of TLIF except cage location.
Inclusion criteria for all patients were severe lower back pain more than a visual analogue scale score of 6, walking with claudication <50 m for >6 months, and pharmaceutical, physical, spinal injection therapy that had failed. No other pain was associated with degenerative arthritis, psychological causes, or degenerative disc disease, as confirmed by magnetic resonance imaging (MRI). General exclusion criteria were : severe osteoporosis [bone mineral density (BMI) : T<-3.5] or metabolic bone disease, local and systemic infection, morbid obesity (body mass index >35), serious psychiatric disorder, symptomatic hip and knee osteoarthritis, adrenal insufficiency due to multiple steroid injection therapy, assist gait, inability to complete a minimum of 6-months follow up.
All patients underwent supine translateral, sitting lateral, and frontal and lateral standing lumbar spine radiography; lateral radiography during flexion and extension; and long-cassette whole-spine radiography. MRI was performed in all cases to analyze the spinal discs, facet joints, vertebral degeneration, neural canal compromise, and paraspinal muscle degeneration. A sacroiliac joint and hip joint MRI study was added to the basic lumbar spinal MRI series in cases of requisition.
The radiographic protocol was standardized. A standing left lateral radiograph including the spine and pelvis was obtained with a long 0.9 m cassette placed 1.8 m from the X-ray tube. Subjects were instructed to stand in a comfortable position with the hips and knees fully extended. Hands were positioned on a support in front of the clavicle instead of the fist on the clavicle. Position was a steady gaze into the distance and upwards 10°.
The following spinopelvic parameters were measured pre-operatively and post-operatively : Index level lordosis (ILL), lumbar lordosis (LL), sacral slope (SS), pelvic tilt (PT), disc height (DH), and pelvic incidence (PI). All spinopelvic parameters were measured using the worldwide principal protocol (lumbar lordosis : angle between the superior endplate of L1 and the endplate of S1; pelvic incidence : angle between the perpendicular to the sacral plate at its midpoint and the line connecting this point to the femoral heads axis; sacral slope : angle between the horizontal and sacral plate; pelvic tilt : angle between the vertical and the line through the midpoint of the sacral plate to femoral heads axis21), ILL was measured as the intersectional angle of the upper most vertebral endplate and lower most vertebral endplate extension but the sacral plate was chosen at the S1 level. Inter- and extra-observer validation for radiographic evaluations was performed with four observers who analyzed the 105 cases. The selected demographic and clinical factors are shown at Table 1. Inter-observer reproducibility was 0.91-0.98, and intra-observer reproducibility was 0.92-0.98.
Table 1.
Patient demographic and clinical data
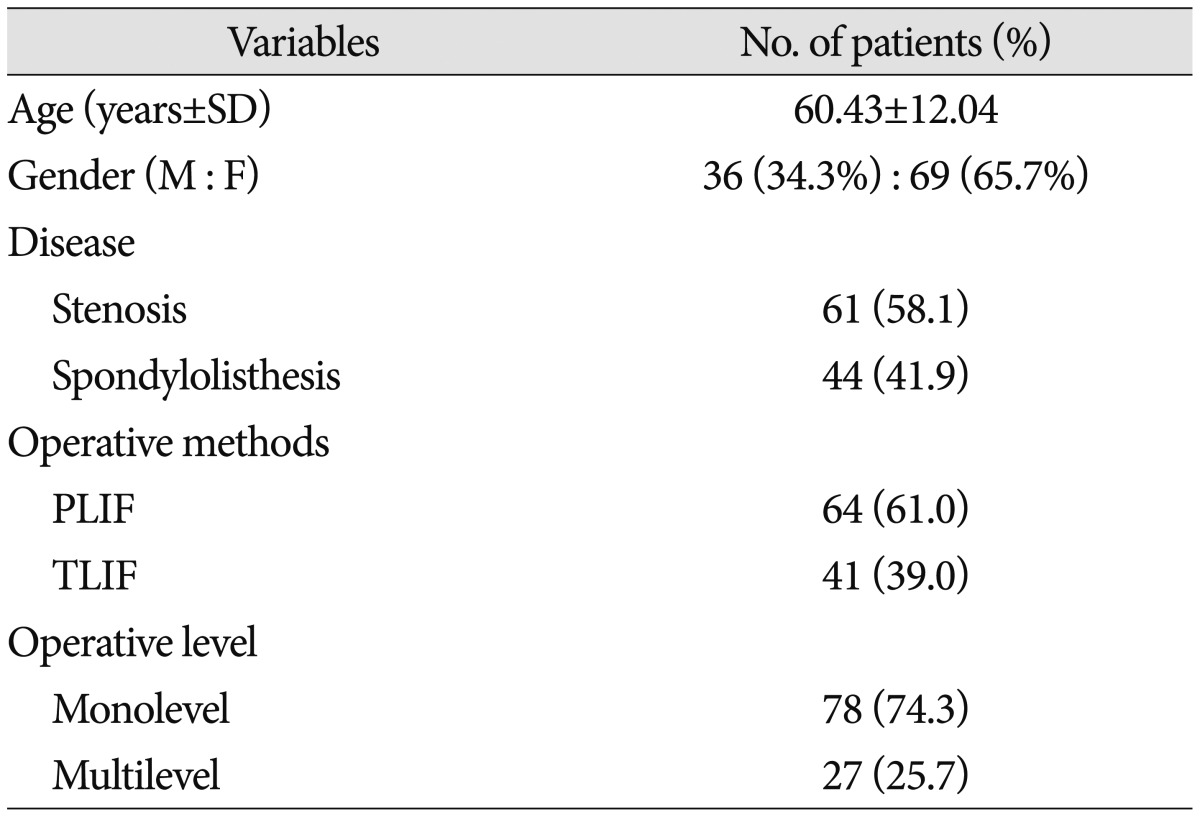
PLIF : posterior lumbar inter body fusion, TLIF : unilateral transforaminal lumbar interbody fusion
Data were entered anonymously using Excel software and processed for analysis with SPSS ver. 13 (SPSS Inc., Chicago, IL, USA). Pre- and post-operative quantitative data were compared using paired t-tests, and each group's data were analyzed with Student's t-test (comparison of means) with a significance level of 0.05 (type I error). A risk analysis was performed with Pearson's chi-square test and correlations between two quantitative variables were determined by Pearson's correlation and linear regression analyses.
Surgical methods
A conventional posterior midline approach was used. Autologous graft materials were harvested from the iliac crest, lamina, and index level facet joints. The average amount of harvest was 20-25 g from the iliac crest and 4-5 g from each laminar and facet joint. Distraction of the disc space was established by hip flexion of the operating table and an Inge laminar distractor. The surgeon limited the use of variable heights of the rimier and disc space elevator to prevent excess endplate damage as well as disc space distraction to prevent graft subsidence and loss of lumbar lordosis. The surgeon preferred to use various kinds of curettes and curved chisels to prepare the disc space. Interbody cage geometry was decided by the manufacturer's design. The PLIF and TLIF cages have 8° and 0° of sagittal angle, respectively. Cage length was 24 mm and 28 mm, respectively. Each cage was placed axial and parallel in cases of PLIF and anterior coronal in cases of TLIF. Interbody bone grafting was an important procedure for compact disc space packing rather than loose filling. The hip flexion surgical posture was returned to a flat prone position to create the original lumbar lordosis at the end of the operation and apply posterior compression force of the pedicle screw locking system to provide a posterior tension bending force and restore ILL.
RESULTS
No significant differences were observed in the demographic or clinical data of the patients except the gender proportion (Table 1). The average amount of discectomy and interbody graft at each level was 13.4±7.4 g and 25.1±10 g for PLIF and 16.4±9.9 g and 24±8.6 g for TLIF (p=0.18 and 0.59). There was no statistical difference of disc height between PLIF and TLIF groups according to this study (p=0.14) (Table 2). The simplest examination of graft contact surface was made by Adobe CS5 extended version and measured as 75% and 65% for PLIF and TLIF, respectively.
Table 2.
The amount of discectomy and bone graft according to surgical method*
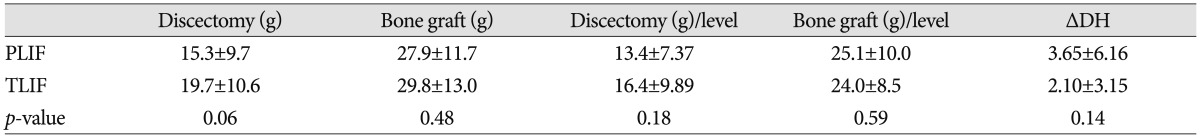
*Data are plotted as means±standard deviations. DH : disc height, PLIF : posterior lumbar interbody fusion, TLIF : unilateral transforaminal lumbar interbody fusion
The risk of postoperative flat back in accordance with diagnosis, operative method, and the number of surgical levels was determined by Pearson's chi-square test. The risk of loss of ILL in the TLIF group was significantly higher than that in the PLIF group (p=0.044). The risk of loss of lumbar lordosis was not significantly different between the groups (Table 3).
Table 3.
The risk of postoperative flat back in accordance with diagnosis, operative method, and the number of surgical levels (Pearson's chi-square)
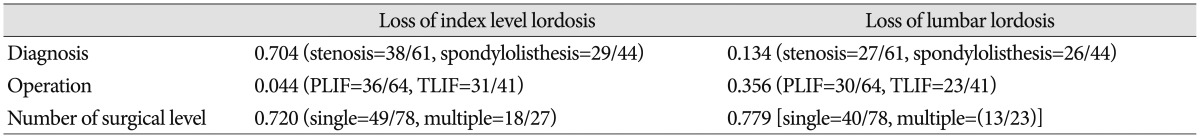
PLIF : posterior lumbar interbody fusion, TLIF : unilateral transforaminal lumbar interbody fusion
No significant perioperative variance in spinopelvic parameters was observed except disc height (Table 4). Sacral angle and pelvic tilt were restored significantly more often in the PLIF group than that in the TLIF group (ΔSS : p=0.02, ΔPT : p=0.03) (Table 5).
Table 4.
Perioperative variance in spinopelvic parameters
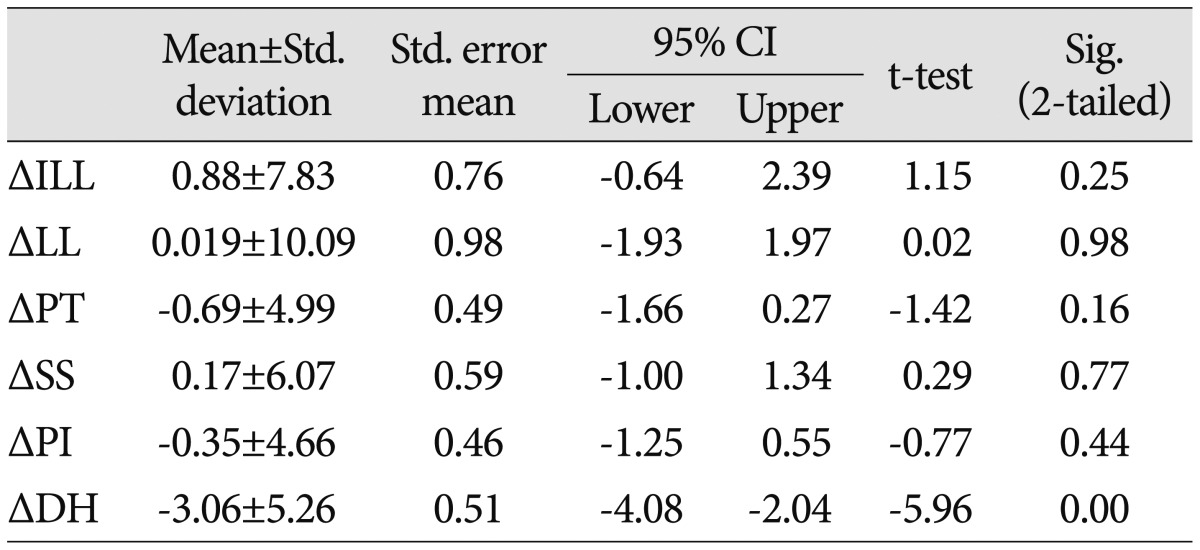
CI : confidence interval, ILL : index level lordosis, LL : lumbar lordosis, PT : pelvic tilt, SS : sacral slope, PI : pelvic incidence, DH : disc height
Table 5.
Comparative analysis in the perioperative variance of spinopelvic parameters according to disease, operative method, and the number of surgical levels*
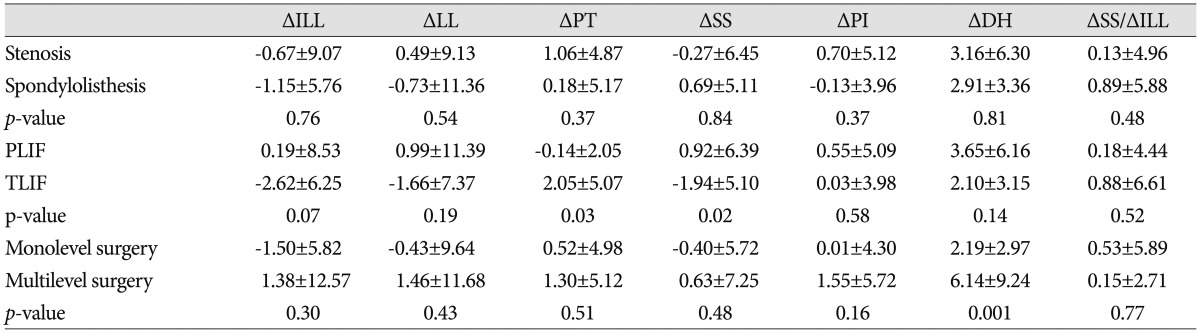
*Data are plotted as means±standard deviations (except, p-value). PLIF : posterior lumbar interbody fusion, TLIF : unilateral transforaminal lumbar interbody fusion, ILL : Index level lordosis, LL : lumbar lordosis, PT : pelvic tilt, SS : sacral slope, PI : pelvic incidence, DH : disc height
The perioperative variance in ILL decreased significantly for the mono-level surgery (p=0.002) and spondylolisthesis (p=0.005) and a significant loss of ILL was observed in the TLIF group compared to that in the PLIF group (PLIF=-0.35±6.27, TLIF=-3.32±4.56, p=0.02) (Table 6, 7). No significant change in perioperative variance of the spinopelvic parameters between stenosis and spondylolisthesis was observed according to surgical method (Table 7).
Table 6.
Paired t-test analysis for perioperative variance in spinopelvic parameters according to surgical method with respect to the number of surgical levels and diagnosis
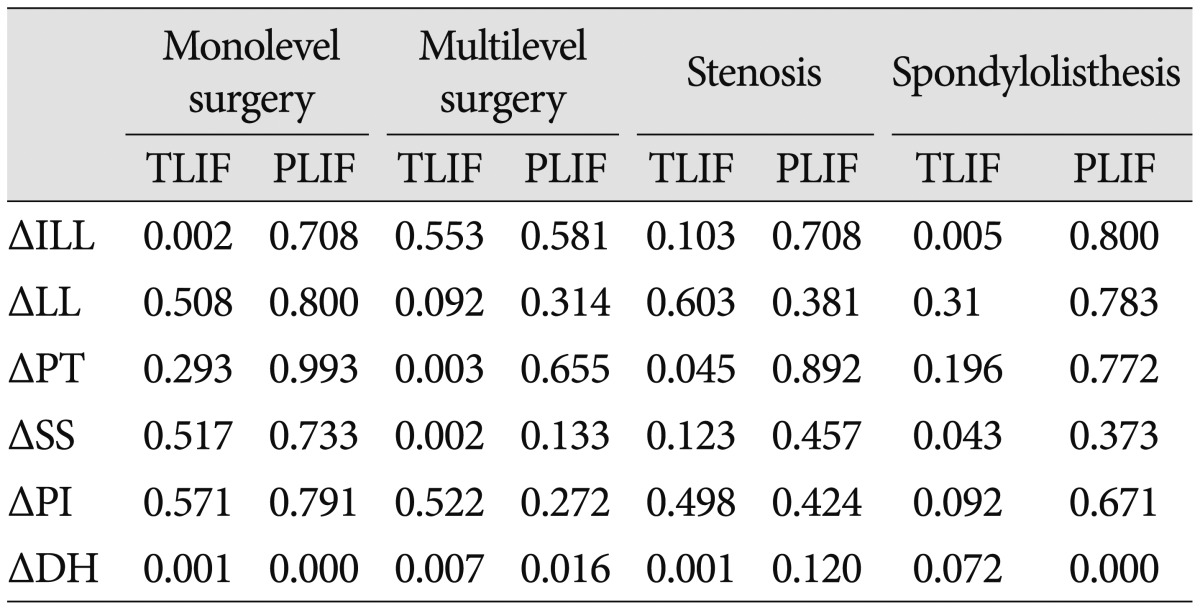
Data are plotted as p-value. PLIF : posterior lumbar interbody fusion, TLIF : unilateral transforaminal lumbar interbody fusion, ILL : index level lordosis, LL : lumbar lordosis, PT : pelvic tilt, SS : sacral slope, PI : pelvic incidence, DH : disc height
Table 7.
Comparative analysis of perioperative variance of spinopelvic parameters according to surgical method in each of operative group and disease*
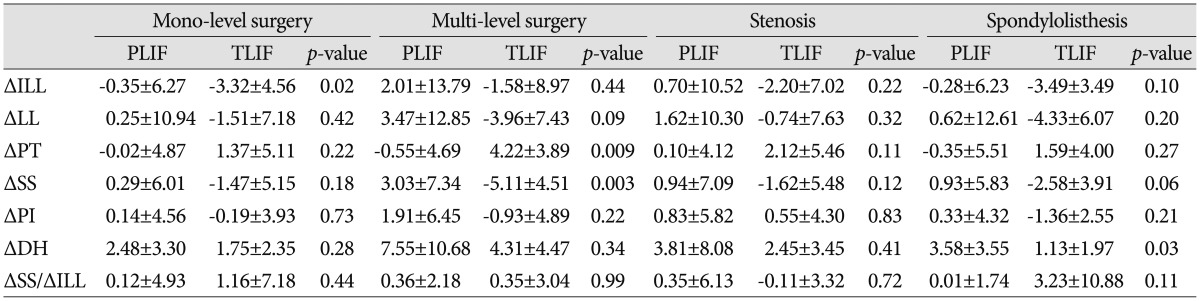
*The data are plotted as means±standard deviation (except, p-value). PLIF : posterior lumbar interbody fusion, TLIF : unilateral transforaminal lumbar interbody fusion, ILL : index level lordosis, LL : lumbar lordosis, PT : pelvic tilt, SS : sacral slope, PI : pelvic incidence, DH : disc height
Based on a 45° of sacral slope, the statistical results get paid attention to perioperative variance of index level lordosis and sacral slope. In patients with a lumbar spine with <45° of sacral slope, the change in sacral slope becomes amplified about 0.13 times in response to the change in index level lordosis. In contrast, in patients with a spine with >45° of sacral slope, the response is approximately 3.1 times. Thus, these results suggest that the change in sacral slope is about 24 times more sensitive to the change of index level lordosis in a spine with >45° of sacral slope compared with a spine with <45° of sacral slope. A high sacral sloped pelvis is more vulnerable to PALIF at the risk of postoperative flat back (Table 8).
Table 8.
Statistical analysis for the perioperative variance of spinopelvic parameters according to the range of preoperative sacral slope (t-test)
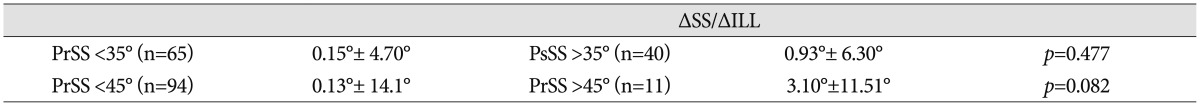
Data are plotted as means±standard deviations. ILL : index level lordosis, LL : lumbar lordosis, PT : pelvic tilt, SS : sacral slope, PI : pelvic incidence, DH : disc height
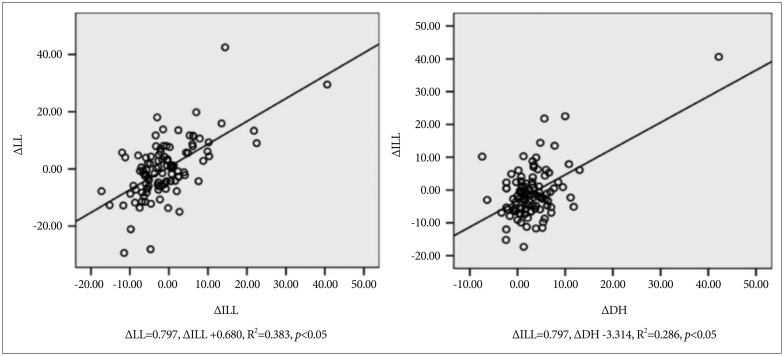
A correlation analysis for perioperative variances showed that ILL and lumbar lordosis were highly positively correlated with disc height variance and sacral slop variance, respectively (correlation coefficients : 0.535 and 0.627) (Table 9). Simple linear regression of the spinopelvic variance in the perioperative state illustrated moderate dependency between perioperative variance of ILL (R squared=0.38), disc height, and ILL (R squared=0.29) (Table 10, Fig. 1). A multiple regression analysis of spinopelvic parameters affecting the perioperative variance of ILL showed that the contribution of perioperative variance of lumbar lordosis and disc height and preoperative lumbar lordosis was important in an ordinal series (lumbar lordosis : p=0.001, disc height : p=0.005, preoperative lumbar lordosis : p=0.007) (Table 11).
Table 9.
Correlations between perioperative variance of spinopelvic parameters and diagnosis
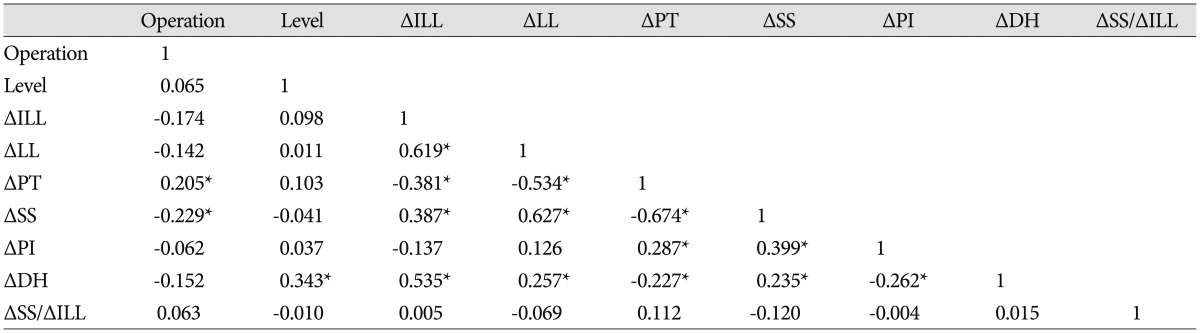
*Correlation was significant at the 0.05 level (two-tailed). ILL : index level lordosis, LL : lumbar lordosis, PT : pelvic tilt, SS : sacral slope, PI : pelvic incidence, DH : disc height
Table 10.
Simple linear regression of spinopelvic variance in the perioperative state
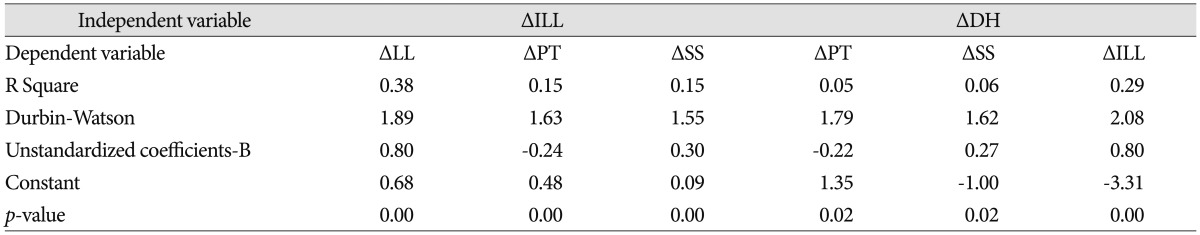
ILL : index level lordosis, LL : lumbar lordosis, PT : pelvic tilt, SS : sacral slope, PI : pelvic incidence, DH : disc height
Fig. 1.
Regression analysis for perioperative variance of the spinopelvic parameters. LL : lumbar lordosis, ILL : index level lordosis, DH : disc height
Table 11.
Multiple regression analysis of spinopelvic parameters affecting the perioperative variance of index level lordosis
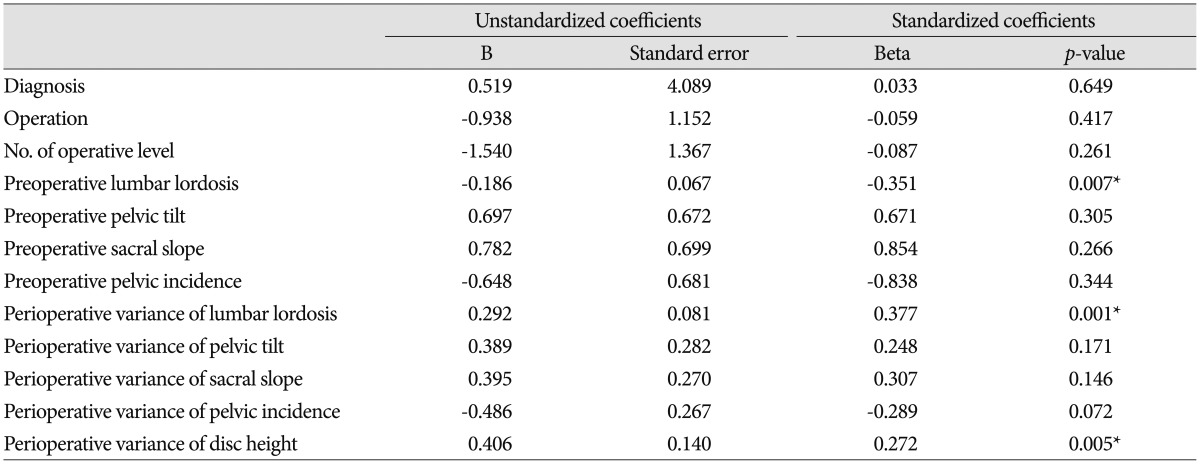
*Correlation was significant. Dependent variable : perioperative variance of index level lordosis
DISCUSSION
The most important factor in spinal surgery is restoring a normal sagittal contour1,3,13,21). Thus, many studies have investigated spinopelvic sagittal balance and changes in spinopelvic parameters in patients with pathologic conditions1,2,3,4,10,12,14,15,16,17,19,20,21,22,23,24). PALIF has the clear objective to restore disc height and lumbar spinal curvature3,5,15). Spine surgeons are careful when restoring disc height with disc space distraction, compact cage insertion, and complete neural decompression in cases of severe lumbar spinal stenosis and spondylolisthesis with foraminal stenosis. However, restoring or maintaining ILL and global spinal balance has received less attention. Postoperative flat back is mostly caused by a careless mistake, and lack of concern for restoring ILL and optimizing spinopelvic and sagittal balance of the patient3) (Fig. 2, 3). Furthermore, studies about postoperative flat back syndrome were reported6,11) and it's cause are known as non-union of graft bone, continuation of neural compression by insufficient decompression of neural canal, chronic back pain, weakness and atrophy of paraspinal muscles, progression of adjust segmental disease, and spinal instability. Also, important causes for postoperative flat back of operative technique include insertion of a lower height cage, excess distraction of the disc space with a too much high cage, not applying a posterior tension bending force of instrumental compression, and loose interbody packing with a small bone graft.
Fig. 2.
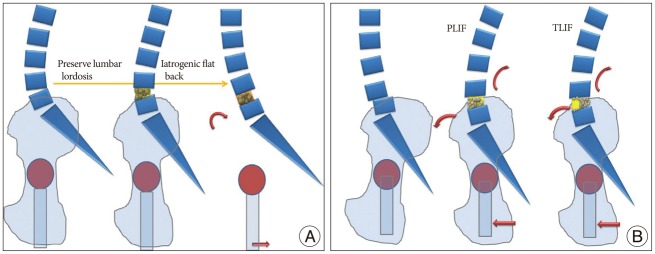
Explanatory illustration for loss of lordosis (A) and dynamic restoration of lumbar lordosis in the posterior accessed lumbar interbody fusion (B). PLIF : posterior lumbar interbody fusion, TLIF : unilateral transforaminal lumbar interbody fusion.
Fig. 3.
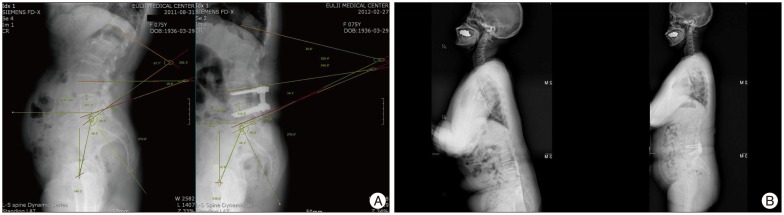
Radiographic illustration of loss of lordosis (A) and restoration of lordosis (B) in patients of posterior accessed lumbar interbody fusion (PALIF).
The solutions are to insert an interbody cage at anterior column of intervertebral space, which as highest as possible, but also complete posterior instrumental compression to restore ILL, and compact the interbody packing with a sufficient bone graft5).
Excess distraction of the disc space with such a high cage, rimmer, and rotatory disc space distractor generates a recoiling force of restitution at the annulus fibrosis and paraspinal muscles and ligaments and leads to damage of vertebral cortical endplate finally potentiating the risk of graft subsidence or screw loosening. Complete posterior instrumental compression with a tension bend force is essential to restore ILL and enhance cage and graft integrity. Loose interbody packing with insufficient bone grafts without iliac bone harvesting usually cannot disperse axial loading force and accomplish early stable interbody fusion.
In addition, lumbar lordosis in accordance with surgical position is very important. The patient's prone position with extending hip joints is set by applying many different-shaped pads to make appropriate lumbar lordosis similar to that of supine just before starting of the operation. Preoperative that position is very important in terms of repositioning the patient before rod's application. On the initial phase of operation start, adjusting the operation table to flex patient's hip joints about 60 degrees is easy for the access to the disc space by fully natural distracting and opening the intervertebral space and intervertebral foramen and facilitate disc space preparation and cage insertion without excessive disc space distraction. And it also preclude overpressure on the facet joint of the adjacent upper segment in accordance with the disc space distraction for cage insertion. After inserting the cage and the autologous graft, the operation table is returned to its former position for making the original lumbar lordosis and binding the cage firmly to the intervertebral space.
In 2011, Rousseoly published an article3) about back type on the base of the sacral slope and distal arch of lumbar lordosis. A type 1 spine has a long thoracolumbar kyphosis and short hyperlordosis and is accompanied with L5 nutcracker spondylolysis and non-harmonious back. A type 2 spine has flat lordosis and a high risk of early disc degeneration of thoracolumbar spine with a harmonious back. A type 3 spine has a harmonious regular back. A type 4 spine has a harmonious hyperlordotic back and is occasionally accompanied with L4-5 spondylolisthesis and L5 isthmic spondylolysis.
Type 4 spines with >45° of sacral slope are about 24 times more sensitive to perioperative variance of sacral slope proportional to the perioperative variance of index level lordosis and more vulnerable to PALIF based on our results. The change in sacral slope is much more sensitive in a patient with a type 4 spine in accordance with the change of perioperative index level lordosis, and accentuates the tendency to compensate the spinopelvic apparatus and a chance for postoperative pelvic retroversion.
In the stage of harmonic regular spine, an iatrogenic flat back compensates by lumbosacral flexibility. However, contact force of disc space increased gradually and paraspinal muscles tired easily. In the stage of harmonic compensatory degeneration, an iatrogenic flat back compensates by pelvic retroversion; however, the contact force increases and disc degeneration accelerates. In the stage of pelvic compensation, further iatrogenic flat back can lead to a disaster. Thus, the surgeon must gain insight into the surgical strategy and complications (Fig. 4).
Fig. 4.
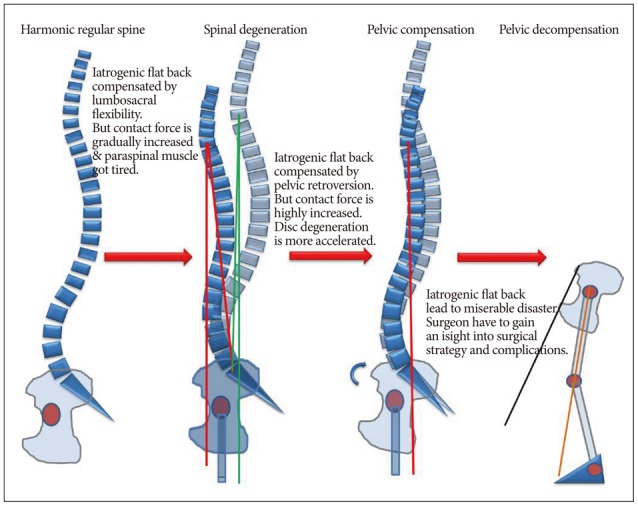
Serial illustrations for the change of spinal and pelvic alignment as a result of compensation mechanism.
In this study, a single surgeon restored disc height and ILL during PALIF with identical surgical protocols after considering flat back and fusion failure in previous surgeries. However, new evidence from this study shows the potential for flat back even though the surgical protocols to restore ILL and optimize spinopelvic parameters were carried out thoroughly. In particular, the perioperative variance of index level lordosis in the case of single level TLIF and spondylolisthesis decreased significantly when compared with single level PLIF and the stenosis group.
PLIF showed less of a tendency for producing postoperative flat back than TLIF but the difference was not significant in statistics. TLIF usually accompanies unilateral foraminolaminectomy on the lesion side and an even compression force may not be applied on the posterior instrumentation. Multilevel PLIF has top priority for restoring lumbar lordosis and scoliosis. Conducting a bilateral foraminolaminectomy and circumferential release of annulus fibrosis and stiff fibroligamentous tissue is mandatory, and the bilateral cages must be snugly placed in a sagittal plan of the anterior and middle disc space. This complete release of the index level disc space optimizes the posterior tension bend mechanism of internal instrumentation with sufficient axial compression force and compact packing of the interbody graft. This is why multilevel PLIF had less of a tendency for flat back and restores spinopelvic parameters in comparison with multilevel TLIF.
Posterior accessed lumbar interbody fusion with a cage unintentionally caused postoperative flat back. The index level lordosis in the case of single level TLIF and spondylolisthesis was significantly reduced compared to that of single level PLIF and stenosis. Multilevel PLIF had less of a tendency for postoperative flat back in comparison with multilevel TLIF. A high sacral sloped pelvis was more vulnerable to PALIF at the risk of postoperative flat back.
The spinopelvic parameter that estimates pelvic retroversion definitely is pelvic tilt value. However, this study adopted SS instead of PT, and it's because in comparison of preoperative and postoperative images of lumbar dynamic series, the center of acetabulum axis cannot correspond exactly in measure of pelvic tilt. Measurement error which can be larger than standard deviation of repeated measurement might be exists as a measurement bias in a retrospective study instead of prospective study. This study thus could indirectly estimate perioperative pelvic compensation through the changes of SS instead of PT for reducing measurement bias.
CONCLUSION
Posterior accessed lumbar interbody fusion with a cage unintentionally caused postoperative flat back. The index level lordosis in the case of single level unilateral TLIF and spondylolisthesis was significantly reduced compared to that of single level PLIF and stenosis. Multilevel PLIF had less of a tendency for postoperative flat back in comparison with multilevel unilateral TLIF. A high sacral sloped pelvis was more vulnerable to PALIF at the risk of postoperative flat back.
Acknowledgements
The abstract of this article was presented at the 53rd annual meeting of the Korean neurosurgical society.
References
- 1.Barrey C, Jund J, Perrin G, Roussouly P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery. 2007;61:981–986. doi: 10.1227/01.neu.0000303194.02921.30. discussion 986. [DOI] [PubMed] [Google Scholar]
- 2.Barrey C, Roussouly P, Perrin G, Le Huec JC. Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J. 2011;20(Suppl 5):626–633. doi: 10.1007/s00586-011-1930-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourghli A, Aunoble S, Reebye O, Le Huec JC. Correlation of clinical outcome and spinopelvic sagittal alignment after surgical treatment of low-grade isthmic spondylolisthesis. Eur Spine J. 2011;20(Suppl 5):663–668. doi: 10.1007/s00586-011-1934-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaléat-Valayer E, Mac-Thiong JM, Paquet J, Berthonnaud E, Siani F, Roussouly P. Sagittal spino-pelvic alignment in chronic low back pain. Eur Spine J. 2011;20(Suppl 5):634–640. doi: 10.1007/s00586-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cole CD, McCall TD, Schmidt MH, Dailey AT. Comparison of low back fusion techniques : transforaminal lumbar interbody fusion (TLIF) or posterior lumbar interbody fusion (PLIF) approaches. Curr Rev Musculoskelet Med. 2009;2:118–126. doi: 10.1007/s12178-009-9053-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farcy JP, Schwab FJ. Management of flatback and related kyphotic decompensation syndromes. Spine (Phila Pa 1976) 1997;22:2452–2457. doi: 10.1097/00007632-199710150-00025. [DOI] [PubMed] [Google Scholar]
- 7.Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991;73:802–808. [PubMed] [Google Scholar]
- 8.Kim CH, Gill SB, Jung MH, Jang YK, Kim SS. Clinical comparison of posterolateral fusion with posterior lumbar interbody fusion. J Korean Neurosurg Soc. 2006;40:84–89. [Google Scholar]
- 9.Kim YT, Lee CS, Na HY, Lee CW. A comparison of surgical treatment in isthmic and degenerative spondylolisthesis. J Korean Orthop Assoc. 1998;33:1627–1634. [Google Scholar]
- 10.Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis : a review and classification. Eur Spine J. 2011;20(Suppl 5):641–646. doi: 10.1007/s00586-011-1932-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lagrone MO, Bradford DS, Moe JH, Lonstein JE, Winter RB, Ogilvie JW. Treatment of symptomatic flatback after spinal fusion. J Bone Joint Surg Am. 1988;70:569–580. [PubMed] [Google Scholar]
- 12.Lazennec JY, Brusson A, Rousseau MA. Hip-spine relations and sagittal balance clinical consequences. Eur Spine J. 2011;20(Suppl 5):686–698. doi: 10.1007/s00586-011-1937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lazennec JY, Ramaré S, Arafati N, Laudet CG, Gorin M, Roger B, et al. Sagittal alignment in lumbosacral fusion : relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Le Huec JC, Aunoble S, Philippe L, Nicolas P. Pelvic parameters : origin and significance. Eur Spine J. 2011;20(Suppl 5):564–571. doi: 10.1007/s00586-011-1940-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Le Huec JC, Charosky S, Barrey C, Rigal J, Aunoble S. Sagittal imbalance cascade for simple degenerative spine and consequences : algorithm of decision for appropriate treatment. Eur Spine J. 2011;20(Suppl 5):699–703. doi: 10.1007/s00586-011-1938-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Le Huec JC, Leijssen P, Duarte M, Aunoble S. Thoracolumbar imbalance analysis for osteotomy planification using a new method : FBI technique. Eur Spine J. 2011;20(Suppl 5):669–680. doi: 10.1007/s00586-011-1935-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Le Huec JC, Roussouly P. Sagittal spino-pelvic balance is a crucial analysis for normal and degenerative spine. Eur Spine J. 2011;20(Suppl 5):556–557. doi: 10.1007/s00586-011-1943-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lombardi JS, Wiltse LL, Reynolds J, Widell EH, Spencer C., 3rd Treatment of degenerative spondylolisthesis. Spine (Phila Pa 1976) 1985;10:821–827. doi: 10.1097/00007632-198511000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur Spine J. 2011;20(Suppl 5):572–577. doi: 10.1007/s00586-011-1923-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morvan G, Mathieu P, Vuillemin V, Guerini H, Bossard P, Zeitoun F, et al. Standardized way for imaging of the sagittal spinal balance. Eur Spine J. 2011;20(Suppl 5):602–608. doi: 10.1007/s00586-011-1927-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Obeid I, Hauger O, Aunoble S, Bourghli A, Pellet N, Vital JM. Global analysis of sagittal spinal alignment in major deformities : correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J. 2011;20(Suppl 5):681–685. doi: 10.1007/s00586-011-1936-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pellet N, Aunoble S, Meyrat R, Rigal J, Le Huec JC. Sagittal balance parameters influence indications for lumbar disc arthroplasty or ALIF. Eur Spine J. 2011;20(Suppl 5):647–662. doi: 10.1007/s00586-011-1933-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roussouly P, Pinheiro-Franco JL. Sagittal parameters of the spine : biomechanical approach. Eur Spine J. 2011;20(Suppl 5):578–585. doi: 10.1007/s00586-011-1924-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sergides IG, McCombe PF, White G, Mokhtar S, Sears WR. Lumbo-pelvic lordosis and the pelvic radius technique in the assessment of spinal sagittal balance : strengths and caveats. Eur Spine J. 2011;20(Suppl 5):591–601. doi: 10.1007/s00586-011-1926-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Suk KS, Jeon CH, Lee HM, Kim NH, Kim HC. Comparison between posterolateral fusion with pedicle screw fixation and anterior interbody fusion with pedicle screw fixation in spondylolytic spondylolisthesis of the lumbar spine. J Korean Soc Spine Surg. 1999;6:397–406. [Google Scholar]
- 26.Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine (Phila Pa 1976) 1997;22:210–219. doi: 10.1097/00007632-199701150-00016. discussion 219-220. [DOI] [PubMed] [Google Scholar]