Abstract
Purpose:
To determine the incidence and density of Demodex species on the eyelashes of subjects with normal eyelids, anterior blepharitis (AB), meibomian-gland dysfunction (MGD), and mixed blepharitis (MB).
Materials and Methods:
One hundred and fifty consecutive patients diagnosed with AB, MGD, and MB were recruited. An additional 50 individuals were recruited who were free of lid and margin disease to serve as a control group. All patients underwent a standard eye examination. Data on ocular symptomatology were gathered. Digital photography was performed of the lid margins. Lash sampling was performed by epilating the lashes and the lashes were checked for Demodex based on morphology using light microscopy. The total number of mites were tabulated for each eye. Comparison between the affected eyes and the control eyes was performed. Data were analyzed using the Chi-square test.
Results:
A total of 200 patients were included. Twenty percenth had AB, 40% had MGD, and 40% had MB. The incidence of Demodex infestation was 90% in cases of AB, 60% in MGD cases, and 90% in MB cases. The incidence of Demodex in control subjects was 18%.
Conclusions:
The incidence and density of Demodex infestation was highest in patients with AB and MB. Lid irritation and presence of cylindrical dandruff were indicative of a high-density infestation. These signs should alert the clinician to treat concomitant Demodex infestation.
Keywords: Blepharitis, Demodex, Eyelash, Tea Tree Oil
INTRODUCTION
Demodex mite is an external parasite that belongs to the Phylum Arthropoda and can infest the meibomian and sebaceous glands. Although they normally inhabit the hair and eyelash follicles in low numbers, an over-proliferation may lead to lid-margin infection causing ocular-surface irritation and symptoms of ocular discomfort such as itching, foreign-body, or stinging sensation. It may also exacerbate coexisting lid-margin diseases such as anterior blepharitis (Staphylococcal and sebaceous) and posterior blepharitis (meibomian-gland dysfunction). Demodex infestation is an often overlooked in the clinical investigation of blepharitis and may be a cause of treatment failure. The adult Demodex mite is cigar-shaped, with several pairs of legs, and has a mouth with a biting apparatus [Figure 1a and b]. Demodex infestation is diagnosed by identification of the parasite at the root of the lashes with light microscopy.1 This study determined the incidence and density of Demodex species found on the eyelashes of subjects with normal eyelids, anterior blepharitis, meibomian gland dysfunction, and mixed blepharitis. Specifically, it determined the relationship of the incidence and density of Demodex with patient demographics, ocular symptoms related to blepharitis, and clinical lid-margin findings (dandruff-like material, collarette or cylindrical dandruff, scurf, plugged meibomian gland orifices, crust) [Figure 2a and b].
Figure 1.
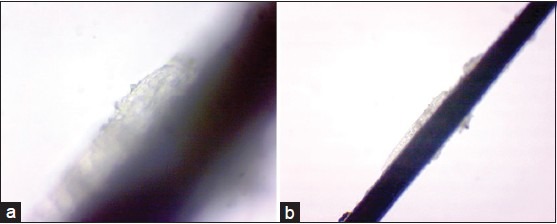
(a) Adult demodex (b) Adult demodex on lash on light microscopy
Figure 2.
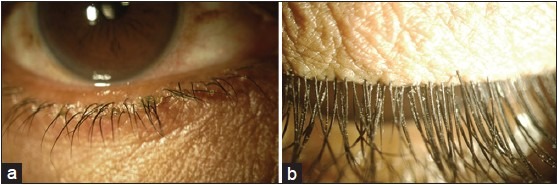
(a) Patient with cylindrical dandruff (b) Cylindrical dandruff
MATERIALS AND METHODS
Consecutive patients who presented to the Sankara eye center, a tertiary care eye center in Coimbatore, Tamil Nadu, India, over a period of 3 months with the diagnosis of meibomian-gland dysfunction (MGD), anterior blepharitis (AB), or mixed blepharitis (MB) were recruited for the study. This study was registered with the institutional review board approved by the ethics committee of the hospital. The authors established the diagnosis based on preset criteria of clinical findings1 using a slit lampbiomicroscopy (Topcon Corp., Tokyo, Japan). Exclusion criteria were use of topical ophthalmic medications (except artificial tears) over the previous 3 months before the study started, a history of ocular or eyelid trauma and surgery, previous diagnosis of chemical burns, Stevens-Johnson syndrome, ocular cicatricial pemphigoid, with eyelid malpositions such as entropion, ectropion, and distichiasis, signs of active ocular infection, or inflammation other than blepharitis. After the recruitment of patients with MGD, AB, and MB, 50 age-matched patients who presented at the hospital for other eye complaints were recruited to serve as the (normal lid/lashes) control group. All patients underwent standard eye examinations. Data were collected on ocular symptoms and clinical findings. Digital photographs of the lid margins were performed using the digital camera of the same slit lamp biomicroscope. Lash sampling was performed by epilating the lashes. The collected lashes were inspected for Demodex based on morphology [Figure 3a and b] using a light microscope. The total number of Demodex mites were tabulated for each eye per lash. The main outcome measure was the incidence of Demodex infestation, [Video] taken as the percentage of patients per group (control group, MGD, AB, MB) that had lashes with mites identified with light microscopy. The data were collected and tabulated using Microsoft Excel (Microsoft Corp., Redmond, WA, USA) and Word (Microsoft Corp., Redmond, WA, USA) and were analyzed using the Chi-square test. Statistical software used in the study included Statistical Analysis System (SAS) 9.2 (SAS Inc., Cary, NC, USA), Statistical Package for the Social Sciences (SPSS) 15.0 (SPSS Inc. Chicago, IL, USA), Stata 10.1 (StataCorp LP, College Station, Tx, USA), MedCalc 9.0.1 (MedCalc Software bvba, Ostend, Belgium), Systat 12.0 (Cranes Software Inc., Bangalore, India), and R environment ver. 2.11.1 (free online software) and Microsoft Word and Excel were used to generate graphs and Tables.
Figure 3.
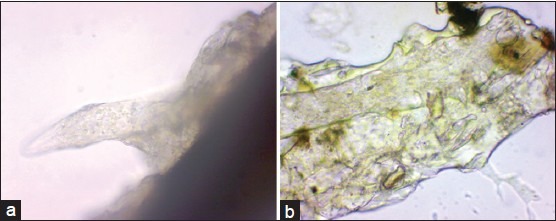
(a) Adult demodex body on microscopy (b) Detailed microscopy of the head of demodex
RESULTS
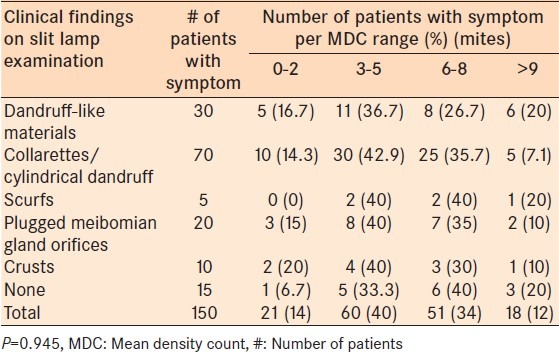
A total of 200 subjects were included, 150 symptomatic patients and 50 control patients. In the symptomatic group 33% were in 40-60 year age-group and 44% in 60-80 year age-group [Table 1]. In the control group, 40% were in 40-60 year age-group and 30% were in 60-80 year age-group. The gender distribution in both groups was 60% males and 40% females. The incidence of Demodex sp infestation in the symptomatic group was 78.7% and 18% in the asymptomatic group [Table 1]. There was a statistically significantly greater incidence of Demodex associated with symptomatic patients (P < 0.001). The incidence of Demodex infestation was statistically significantly higher in cases of anterior blepharitis and mixed blepharitis (P < 0.001, both groups) [Table 2]. The mean Demodex count was between 3-5 mites (38.9%), 6-8 mites (44.4%) were associated with irritation as the symptom [Table 3]. The mean Demodex count in the symptomatic group was high in patients with cylindrical dandruff, 3-5 mites in 42.9% and 6-8 mites in 35.7% [Table 4].
Table 1.
Incidence of Demodex in symptomatic patients: A control group of patients
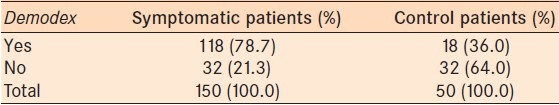
Table 2.
Incidence of Demodex based on diagnosis in symptomatic patients
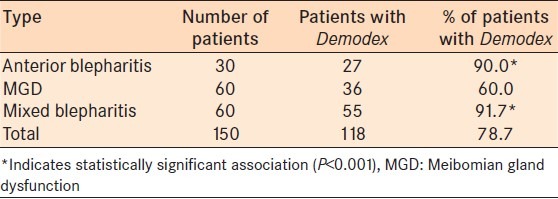
Table 3.
Comparison of ocular symptomatology and density of Demodex
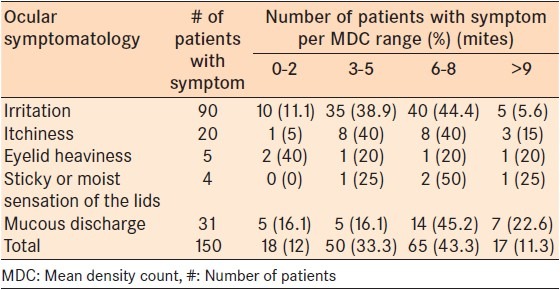
Table 4.
Comparison of clinical findings and density of Demodex
DISCUSSION
The conventional method of counting Demodex involves random epilation of four non-adjacent lashes per lid and addition of a drop of oil (peanut oil is preferred) before mounting with a coverslip. However, this method can lead to erroneous results for a number of reasons. First, as the chance of detecting Demodex is much higher by sampling those with cylindrical dandruff compared with those without cylindrical dandruff, random epilation of lashes may result in a lower count if lashes without cylindrical dandruff are epilated. Secondly, addition of oil before mounting the coverslip may result in a decreased incidence by allowing non-adherent mites to float away, especially in lashes without retained cylindrical dandruff fragments. Third, even if lashes with cylindrical dandruff are intentionally epilated, different amounts of cylindrical dandruff fragments are actually retained. Fourth, Demodex embedded in compact cylindrical dandruff fragments could not be counted with accuracy without adding alcohol. Lastly, even if only lashes with clinically evident cylindrical dandruff were epilated, some cylindrical dandruff fragments that harbor Demodex still adhere to the lid skin. These potential errors collectively explain why use of the conventional method could lead to miscounting of Demodex.2 In the current study, we followed a modified method of epilating the lashes. We epilated lashes with cylindrical dandruff and used a carrier slide with a concavity, put a drop of saline and placed a cover slip [Figure 4]. This prevented Demodex from floating away resulting in more accurate count. The incidence of Demodex in our study was 68%, which included controls. In the symptomatic group the incidence was 78.7% which is higher than reported by Venecia and Siong.1 There was statistically significantly greater incidence of Demodex in case of anterior blepharitis and mixed blepharitis (P < 0.001 both groups). Demodex infestation in humans was once thought to be of no clinical significance due to its non-pathogenic nature. Several authors, however, have concluded that Demodex infestation or demodecosis is related to blepharitis.3,4,5 However, the exact pathogenic potential of Demodex mites remains unclear because a low number of Demodex mites are found in the skin and lashes of asymptomatic individuals. It is postulated that Demodex becomes pathogenic when it multiplies to cause or exacerbate ocular symptoms and lid-margin changes. No prior research has convincingly demonstrated whether a minimal number of mites must be present to produce symptoms. Of the ocular symptoms investigated, only lid irritation correlated with a high Demodex count. The etiology of lid irritation in Demodex infestation is an interplay of different factors. First, the biting apparatus of the mitealone may cause lid irritation. Second, lid irritation is also caused by the lipolytic enzymes produced by the parasite to digest sebum, and by the accumulation of parasite excreta, resulting in the blockage of sebaceous glands that may lead to infection or the stimulation of the host's humoral responses and cell-mediated reaction. Third, secondary or concomitant microbial blepharitis is common in Demodex infestation, as the micro-organisms may cling to the integuments of the parasites.6 This study demonstrated the highest incidence and density in patients with mixed blepharitis, followed by anterior blepharitis. MGD patients have the lowest incidence and density among the three. This can be explained by the fact that patients with mixed and anterior blepharitis have involvement of the eyelashes because Demodex mites tend to be clustered at the roots of lashes. The incidence and density of Demodex infestation were highest among patients with both anterior blepharitis and meibomian-gland dysfunction. Symptom of lid irritation and presence of cylindrical dandruff are indicative of a high-density count. These diagnosis and eye findings should alert the clinician to Demodex infestation of the eyelashes, especially in the elderly. Patients with recurrent blepharitis not responsive to current blepharitis treatment regimen should be investigated and treated for Demodex infestation.
Figure 4.

Carrier slide
Video on available at: www.meajo.org
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Venecia AB, Siong RL. Demodex sp. infestation in anterior blepharitis, meibomian-gland dysfunction, and mixed blepharitis. Philipp J Ophthalmol. 2011;36:15–22. [Google Scholar]
- 2.Gao Y, Di Pascuale MA, Li W. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46:3089–94. doi: 10.1167/iovs.05-0275. [DOI] [PubMed] [Google Scholar]
- 3.Pena GP, de Souza J, Filho A. Is Demodex really non-pathogenic? Rev Ins Med Trop S Paulo. 2000;42:171–3. doi: 10.1590/s0036-46652000000300012. [DOI] [PubMed] [Google Scholar]
- 4.Liu J, Sheha H, Fu Y, Tseng SC. Demodex blepharitis. Adv Ocular Care. 2010:37–9. [Google Scholar]
- 5.Czeptia D, Kuzna-Grgiel W, Czepita M, Grobelmy A. Demodex folliculorum and Demodex brevis as a cause of chronic marginal blepharitis. Ann Acad Meu Stein. 2007;53:63–7. [PubMed] [Google Scholar]
- 6.English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol. 1981;91:362–72. doi: 10.1016/0002-9394(81)90291-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


