Abstract
Objective:
To evaluate the effect of a workplace health intervention designed to reduce prolonged occupational sitting on the mean arterial pressure (MAP) of desk-based employees.
Methods:
This randomized controlled trial involved an experimental group who received an e-health intervention and a control group who did not. The 13-week intervention passively prompted participants to stand and engage in short bouts of office-based physical activity by interrupting prolonged occupational sitting time periodically throughout the workday. Mean arterial pressure was measured at pretest and posttest.
Results:
Between pretest and posttest the experimental group significantly reduced their MAP, whereas MAP in the control group did not.
Conclusions:
A workplace e-health intervention designed to reduce prolonged occupational sitting was effective in decreasing MAP in desk-based employees.
Prevalent in Australia are a range of workplace health and wellness interventions designed to reduce or eliminate cardiovascular disease (CVD) risk factors by advocating an increase in physical activity. The inclusion of increased physical activity is largely in response to evidence of an inverse relationship between habitual physical activity and blood pressure (BP).1 Yet, recently, prolonged sitting has been identified as being independent of cardiovascular fitness levels.2–4 Thus, regardless of voluntary exercise levels, desk-based workers who sit for more than 6 hours per day at work5,6 might still be exposed to CVD risk.7,8 In response, there has been an increased effort to regularly break occupational sitting periods9,10 by integrating regular short bursts of non-exercise physical activity (NEPA) throughout the workday.11 There is evidence that increasing NEPA results in positive change to some physiological functions,12 yet there are no data of the effect on BP. Thus, the aim of the researchers in this study was to assess the effect of NEPA on BP within a workplace setting.
Regular moderate-to-vigorous physical activity is widely regarded as a method to reduce hypertension.13,14 The evidence indicates that dynamic physical activity (moderate-to-vigorous) results in BP changes in individuals who are hypertensive. Nevertheless, there is some evidence that lower-intensity physical activity can also reduce BP in borderline hypertensive individuals. Ishikawa-Takata et al15 reported that one session of 30 to 60 minutes per week of physical activity resulted in significant reductions in both systolic and diastolic BP at rest. Similarly, Ross and McGuire12 reported that incidental NEPA accrued sporadically throughout the day was associated with increased levels of cardio-respiratory fitness in inactive, abdominally obese men. Given the difficulties associated with adherence rates in voluntary aerobic exercise programs that use traditional guidelines16 and the lack of data that cardiovascular fitness levels might not reduce CVD,17 the use of NEPA has become an attractive proposition for workplace health and wellness interventions.
On the basis of this, we subjected desk-based employees to a protocol of regular short bursts of NEPA to interfere with prolonged sitting habits to ascertain any effect such activity might have on employees’ BP. Rather than analyze systolic and diastolic BP variables, it was determined that mean arterial pressure (MAP) would be a better measure because it provides a better representation of the average pressure throughout one cardiac cycle.18,19 Among the few studies that have addressed the effect of MAP on CVD, Dyer et al20 and Mitchell et al21 found that MAP was strongly associated with CVD risk and increases in myocardial infarction. Measurements for MAP that are greater than 110 mmHg in adults are considered too high and can impact negatively on individual health.22 We hypothesized that desk-based employee's exposed to regular short bursts of NEPA would significantly reduce their MAP, whereas control participants who were not prompted to perform NEPA during the workday would not.
METHOD
Participant Recruitment
Desk-based employees from the Tasmanian Department of Police and Emergency Management were invited by their occupational health and safety officer to volunteer to participate in the study. These employees were located at eight worksites across the state. Because of limitations in previous field-based studies not using randomized controlled designs,10,23 the sample for this study was recruited for a randomized controlled trial. No a priori data were available for this study; therefore, a power analysis to predict sample size was unable to be conducted. From the initial 80 volunteers, a computer-based random numbers generator was used to select 40 participants for the sample. Once these participants were identified, they were then contacted to determine whether they fit the inclusion criteria. These criteria were being a full-time employee; primarily having desk-based job responsibilities; using a desktop personal computer with Internet access to perform daily work tasks; and being medically cleared to perform short bouts of daily physical activity. On the basis of these criteria, 11 individuals were excluded—seven participants were not primarily desk-based for their daily work; two participants, while desk-based, did not have desktop Internet access; and one person was not medically cleared to participate in workplace physical activity. Moreover, the day before the orientation session one participant was excluded because of a job transfer to another government agency. The occupations of the remaining sample (female = 24, male = 5) varied between roles such as reception duties, administrative support, call center, forensic analysis, community liaison, media liaison, transcription, and sworn duties. All volunteers who were not selected for the study were told that they could receive the workplace health intervention once the experiment was over. All participants in this study provided informed consent according to university ethical guidelines and the Declaration of Helinski before the initiation of any study procedures.
PROCEDURES
After the initial screening for study inclusion, the participants attended an orientation session in a computer laboratory at the Police headquarters. Before this session began, systolic and diastolic BP measurements were collected from each participant by an internationally qualified nurse,24 who was blinded to the participant's group allocation. This registered nurse used a Welch Allyn Sphygmomanometer Platinum Series—DS58–11 inflatable cuff (Welch Allyn Australia Pty. Ltd., New South Wales, Australia) placed around the upper arm of each participant. Before any BP measurements were performed and recorded in this study, all sphygmomanometers were checked and calibrated using a seven-step procedure recommended by Ali and Rouse.25 Each participant had two consecutive seated BP measurements taken with a 1-minute interval between each measurement following the Heart Foundation guidelines to ensure quality and consistency.26 Each participant was seated for a minimum of 5 minutes before each reading was taken.27 Next, participants completed a pretest survey, which included questions from the stages of change questionnaire,28 Short Form–36 health questionnaire,29 and an occupational physical activity questionnaire30 to provide demographic data on our sample.
After the pretest was complete the educational induction session began. The research team provided all participants with an educational lecture on the negative health effects associated with prolonged occupational sitting time (10 minutes), general instructions on performing appropriate workplace physical activity (20 minutes), and an active demonstration on how to use the e-health intervention, as described in the Intervention section (30 minutes). Contamination of the participants was prevented by the research team not divulging the study hypothesis and by providing education on an intervention designed to reduce prolonged sitting in the workplace. During this time, participants were allowed to actively engage with the health intervention and ask any questions related to the information they just received.
Finally, the participants were randomly assigned with replacement either to the experimental group who received the e-health intervention (n = 11; mean = 36.73 ± 12.38 years) or to a control group who did not (n = 18; mean = 42.28 ± 9.59 years). Research staff and participants were not blinded to group allocation. Although the lack of blinding does raise issues with study bias and validity,31,32 participants in the control group were informed at the beginning of this study that they would receive the intervention on the conclusion of the study. This process was completed by using a random numbers generator. There was no significant difference between the mean ages of the two groups (P = 0.22). True randomization to treatment groups was paramount in the research design of this field-based study, and thus groups were purposefully not matched across any demographic variables or pretest data. Participants were informed that the study would take place during their work hours for the next 13 weeks, after which they would attend one more session to collect a final BP measurement. The Tasmanian Department of Police and Emergency Management administration fully supported this research study and granted the participants the time from work to participate in these two data collection sessions.
Experimental Design
A pre-/post-research design was implemented to assess the hypothesis. To assess the effect of the increasing NEPA on MAP, BP measurements were collected at baseline and immediately after exposure to a 13-week experimental period and compared between an experimental and control group. The experimental group received the intervention outlined in the Intervention section, whereas the control group did not. The 13-week experimental period was based on previous research by Lally et al,33 who found that behavior change and habit formation on average take 66 days. A potential threat to validity was the use of self-report data to measure NEPA and the issue of a potential for error in the measurement. We rejected the use of accelerometers because we felt that they might influence behavior because of a surveillance effect.34 Instead, we chose to verify the NEPA reports by contacting participants by telephone throughout the experimental period. The nature of the telephone contact was to ask participants to verify their self-report of occupational physical activity for the given day.
INTERVENTION
Participants in the experimental group were provided an interactive e-health software program, titled Exertime,35 installed on their desktop computer immediately after the pretest. This software was designed to encourage NEPA by prompting employees to break long bouts of sitting by standing up to engage in a brief bout of short-burst physical activity periodically during work hours. This e-health program initiated every 45 minutes as a prompt bubble emanating on the bottom right-hand side of the employees’ computer screen. The 45-minute prompting time was based on national guidelines for office employees,36 which specify that all computer-based employees should remove themselves from a sedentary position for a short period every hour. The prompt indicated that it was time to stand up and engage in a user-selected activity, such as standing while talking on the phone, wall touches while using the photocopier, walking to talk to a colleague, or climbing the office stairs to attend a meeting.
The appearance of the prompt on the computer screen functioned as a passive stimulus in that participants had no choice but to engage with it within a 30-second period. A 30-second countdown measure was included in the prompt, throughout which time participants could select to either engage with the program, postpone the prompt, or simply wait for the 30-second countdown to finish at which time the program would engage automatically. Once the program was engaged, the employees’ computer screen only displayed the Exertime application forcing them to participate before being allowed to have control of their computer. The software featured a postpone function, which enabled participants to temporarily delay the prompt for a selected time period (eg, 10, 15, 30, or 60 minutes) before it reappeared. This function could only be activated for a maximum time of 1 hour. The inclusion of a postpone function was based on the expectation that employees might be involved in a phone conversation, an important meeting, or might need to access computer-based information rapidly; therefore, in a situation such as this employees could choose to postpone the prompt. In the situation where an employee undertook an unscheduled break that was not prompted by the intervention, the software featured a “log additional Exertime” function, which allowed employees to record any NEPA that they had performed while not at their desk. These data were recorded by the software program. These functionality options of the software were thoroughly described to all employees during the orientation session.
Once employees in the experimental group selected an activity, it was their individual decision of how to engage with the prompted opportunity. There was no set requirement placed on participants in terms of activity choice, repetitions, duration, or intensity. At the very least, participants were simply asked to stand during the Exertime sequence. Alternatively, participants in the experimental group could choose from one of 65 office appropriate exercises, such as walking, desk squats, or a wall sit. When participants completed the chosen activity, they were prompted to record the number of repetitions or the amount of time in seconds that they completed so the software could log their daily progress. Their daily progress was graphically presented, indicating the amount of calories expended and the amount of time that they had spent out of their chair to engage in the Exertime activity. This function was incorporated because of research indicating that people who want to change their health habits should be encouraged to regularly monitor their progress in adopting a new behavior.37,38 Once employees’ data were recorded, the Exertime sequence terminated and the employees were able to regain control over their computer screen to continue with their daily work responsibilities. It did not matter which activity was selected, because any time employees were not sitting in their office-based chair during work was considered to require NEPA, and the software was designed to record this progress. For example, if an employee took a break from his or her desk-based work to use the toilet or walk to speak to a colleague, this activity could be logged as NEPA using the software.
During the experimental period, participants received phone calls at random times during the workday from the research team to ensure that they were accurately reporting their participation progress in the program, and if there had been any other changes in their daily routine such as an initiation of leisure time physical activity or a change in eating habits (ie, reduction in salt intake or unhealthy eating) that might have elicited a change in MAP. No participants reported false entries or any such behavior changes during the 13-week trial.
Each participant recorded their activities and levels of engagement (time moving or number of repetitions) for each attempt at NEPA throughout each workday of the 13-week trial. On the basis of an 8-hour workday and incorporating a 1-hour lunch break, each participant was presented with the prompted opportunity to engage with the e-health program on nine separate occasions. Receiving the prompt on nine separate occasions occurred if the participant remained seated at their desk for the entire workday and did not postpone the prompt. Adherence to the e-health intervention in terms of usage per day and duration of each sitting break was measured and reported in the Results section.
CONTROL GROUP
During the 13-week experimental period, the control group was instructed where possible to continue work as normal. To avoid any surveillance or Hawthorne effect, members of the control group were informed during the orientation session that at the end of the study they would receive the e-health software program. Furthermore, each control group participant was contacted by phone on multiple occasions throughout the study to clarify that they had been continuing their workplace behavior as normal. The results of the phone contact confirmed that the control group participants had been continuing normal workplace behavior and had not initiated any new forms of physical activity during or outside of working hours.
STATISTICAL ANALYSES
To arrive at one dependent variable for data analysis of BP, MAP was calculated using the formula (systolic pressure + [2 × diastolic pressure]/3) described as being one third of the distance between the systolic pressure and diastolic pressure.39,40 Descriptive statistics for all three BP variables are presented as means and standard deviations in the Results section. A 2 (group: experimental/control) × 2 (test: pretest/posttest) mixed design analysis of variance was used to test any significant changes in MAP. Alpha was set at α = 0.05. Effect size was reported using partial eta squared (η2p)statistic for comparison to all future related studies. All data were analyzed using SPSS version 21.0 (SPSS, Inc, Chicago, IL).
RESULTS
Demographics
All participants were in one of the following behavior change categories: contemplation, action, or relapse stage.28 In terms of self-reported health,29 the sample was representative of the Australian population,41 with a mean physical component score of 62. This score indicates that the sample perceived their health to be average in relation to the population. Furthermore, the participants worked an average of 39.83 (±11.73) hours per week. This time was spent sitting and standing at work for 34.4 (±7.42) hours per week, and they spent 5.53 (±5.19) minutes per day walking at work.30
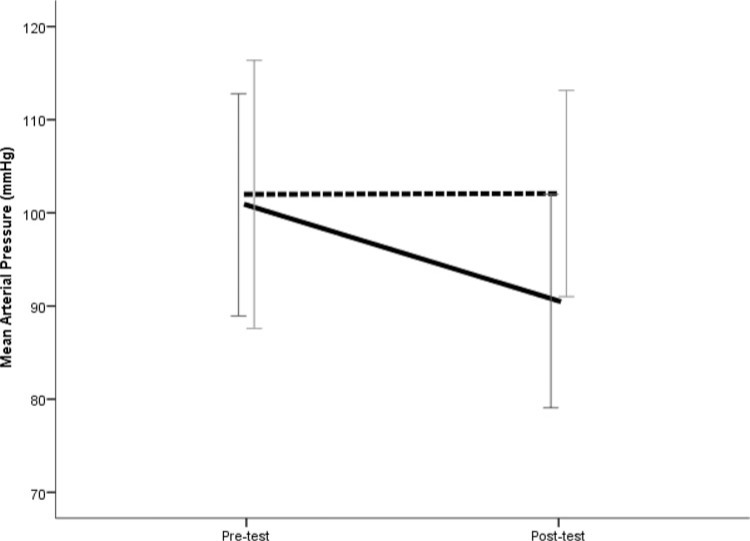
Analysis of the dependent variable indicated a significant interaction between group and test, F(1,27) = 6.85, P < 0.05. As can be seen in Fig. 1, the experimental group significantly decreased their MAP from pretest (mean = 100.85 ± 11.94) to posttest (mean = 90.55 ± 11.46) with a large effect size (η2p = 0.67), whereas the control group marginally increased their MAP from pretest (mean = 101.98 ± 16.60) to posttest (mean = 102.07 ± 10.61) with a small effect size (η2p = 0.01). The latter finding did not reach significance.
FIGURE 1.
Mean arterial pressure (MAP) values of office-based employees in the experimental group and control group at pretest and posttest. Experimental group (-) and control group ( ).
).
The systolic and diastolic BP descriptive values used to calculate MAP are presented in Table 1.
TABLE 1. Participant Systolic Blood Pressure and Diastolic Blood Pressure at Pretest and Posttest by Group.
| Group | Presystolic | Postsystolic | Prediastolic | Postdiastolic |
|---|---|---|---|---|
| Exertime (n = 11) | 132 (15.38) | 127.72 (8.25) | 85.27 (11.13) | 79 (7.88) |
| Control (n = 18) | 137.17 (17.91) | 135.89 (17.28) | 84.39 (14.88) | 85.17 (11.73) |
*Values are means (standard deviations).
For the duration of the trial, no participants withdrew from the study, and all participants’ results were analyzed. In terms of the duration of breaks from sitting, the e-health software prompted participants in the experimental group to engage in NEPA for 7.99 ± 4.44 minutes per day by performing short-burst physical activities 6.28 ± 3.59 times per workday. The average time for each bout of NEPA was 1.34 ± 0.74 minutes.
DISCUSSION
The result of this study gives an indication that increasing movement at work through NEPA can have beneficial health outcomes. Passively prompting desk-based workers to take a regular break from their sitting positions to voluntarily engage in movement resulted in a decrease in MAP over a 13-week period. With the failure to entice large sections of the population to engage in voluntary exercise, alternatives such as NEPA might offer a more salient mechanism to influence population health and associated outcomes.
Our results have several implications. To our knowledge, this is the first study to test the effect of a NEPA intervention on BP. Typically, systolic BP has been the measure of choice when examining sedentary adults who are hypertensive.38,42 We chose to analyze MAP on the basis of evidence indicating an association between MAP and CVD risk factors.20,21 Our finding provides support for Healy et al,43 who found that frequent breaks in sedentary time improved cardio-metabolic profile when compared with uninterrupted sedentary time, independent of moderate-to-vigorous physical activity. Our results should be replicated by other researchers using MAP as the primary means of assessing effect NEPA based interventions on BP on a larger sample of desk-based workers because this population is often overlooked in the occupational health and safety literature.
We suggest that, with a decrease in MAP because of an increase in NEPA, health researchers revise their research interventions to move away from voluntary activity-based programs. Such a move might result in improved compliance to interventions and reach a portion of the population that would have the most benefit. The traditional exercise-based programs (eg, lunchtime exercise classes) tend to recruit those already involved in leisure time physical activity, or those who would like to and then take the opportunity to do so. Nonetheless, the latter group normally finds the behavior change too difficult and drops out before the maintenance stage. Our results suggest a paradigm shift to interventions designed to increase lower–intensity-based movements combined with increased control over the type of movement in workplace health interventions. If health researchers are serious in attempting to help reduce CVD in the population, then the scope of their programs must change. We think that our results provide evidence to support such a paradigm shift.
The efficacy of a passive prompting intervention to change the negative health behavior of prolonged occupational sitting was apparent in this study. The basis of the passive prompt feature meant that the participants had to consciously engage with the software program because it superseded all other active computer-based programs being used at that time and required a response within 30 seconds before the program would automatically initiate. This technique proved valuable in encouraging participants to, first, stand from their seated position and, second, perform 1 to 2 minutes of office-based NEPA regularly throughout the workday. Participation in and adherence to the short-burst office-based physical activities incorporated within the intervention might have also been facilitated by the educational lecture, instructions on performing appropriate workplace physical activity, and information on how to use the intervention software delivered at the initial orientation session.44 Although the control group did receive the educational lecture and instructions on workplace physical activity, MAP levels of the control group marginally increased after the 13-week study period. This further demonstrated the value of the passive prompt in changing the health behavior of desk-based employees. Overall, the use of a passive prompt as a mechanism to reduce prolonged occupational sitting and increase NEPA might offer a solution to reconcile the cardio-metabolic health consequences of prolonged occupational sitting.
Lowering MAP in adults by interrupting prolonged periods of sitting is an important health outcome for workplaces because high MAP levels are related to increased risk of morbidity and mortality rate.45 As previously acknowledged by Seeley et al,22 measurements for MAP that are greater than 110 mmHg in adults are considered too high and can adversely impact on individual health. In individuals with hypertension (greater than 140/90 mmHg; MAP greater than 107), the initial goal of treatment is to reduce MAP to a normotensive pressure.46 Typically, this is treated with prescribed medication and physical activity. Another factor that contributes to hypertension and CVD within the workplace is work-related stress.47 Previous research has shown increases in BP in subjects with high work stress.48 It is possible that desk-based employees who experience high levels of work-related stress are reluctant to remove themselves from their office-based chair throughout the workday. By failing to do this, they might be adding to their cardiovascular risk by not only not standing from their chairs and moving to increase energy expenditure, but also by not capitalizing on a potentially valuable mental break that 1 to 2 minutes of physical activity might provide. On the basis of these factors, workplace health interventions framed on regular short bouts of movement throughout the workday offer a viable and practical option for improving employee cardio-metabolic health indicators such as MAP and might also influence nervous system reactivity to work-related stress.
The objective clinical measurement of BP, randomized group allocation, and field-based study duration were key strengths of this study. Moreover, a good built in feature of the software was the ability to record the duration and frequency of the NEPA breaks. Similarly, the ability to record the NEPA breaks that occurred at un-scheduled times was effective in capturing employee movement when not at their desks. Limitations of this study included the small sample size, and not matching group participants across demographic variables. Considering that the majority of participants were female (83%), the findings should be treated with for limited generalizability. The possibility that MAP could change as a result of age did exist, with previous research indicating age-associated increases in both systolic and diastolic BP.49–51 To address these limitations, future trials should incorporate larger sample sizes that can detect health and work-related benefits or adverse effects to improve generalizability, and group participants should be matched across the demographic variables outlined previously in this article.
CONCLUSIONS
This is the first study to examine the effect of an intervention designed to reduce prolonged occupational sitting on the MAP of a cohort of desk-based employees. The major finding was that an intervention based on prompting desk-based employees to stand and perform NEPA significantly decreased MAP in the experimental group compared with a control group. This indicates that desk-based employees might not need to rely on purposeful physical activity that is set in duration and intensity to improve their health. A key feature of the intervention was the passive nature of the prompt and how this functioned to consciously engage the participants in the decision-making process of standing and being physically active. In conjunction with the potential health implications that breaking prolonged occupational sitting in the workplace can contribute, our findings offer scope for practical application in home environments, school environments, and whenever sitting might occur for prolonged periods.
Footnotes
The views expressed in this article are those of the authors and not an official position of any institution or funding organization. The study was approved by the University of Tasmania Ethics Committee (Hobart, Australia, #00002624).
This study was funded in part by a Tasmanian Government (Australia) Healthy at Work grant (www.healthyatwork.tas.gov.au). Study design, data collection, analysis and interpretation, writing of the report, and submission of the results were not influenced by the funding source. The authors declare that there were no conflicts of interest in this experiment.
The authors of this original article have read and approved the manuscript, and believe that the manuscript represents honest work.
REFERENCES
- 1.Nelson L, Esler MD, Jennings G, Korner P. Effect of changing levels of physical activity on blood-pressure and haemodynamics in essential hypertension. Lancet. 1986;2:473–476. [DOI] [PubMed] [Google Scholar]
- 2.Dunstan DW, Thorp AA, Healy GN. Prolonged sitting: is it a distinct coronary heart disease? Curr Opin Cardio. 2011;26:412–419. 10.1097/HCO.0b013a3283496605. [DOI] [PubMed] [Google Scholar]
- 3.Healy GN, Lawler SP, Thorp AA, et al. Reducing prolonged sitting in the workplace: an evidence review: full report. Melbourne, Australia: Victorian Health Promotion Foundation; 2012. Available at: http://www.vichealth.vic.gov.au/∼/media/ResourceCentre/PublicationsandResources/Economic%20participation/2012%20workplace/CHW_Sitting_Full_Web_Final.ashx. Accessed December 12, 2013. [Google Scholar]
- 4.Van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman AE. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med. 2012;172:494–500. 10.1001/archinternmed.2011.2174. [DOI] [PubMed] [Google Scholar]
- 5.Pronk NP, Katz AS, Lowry M, Payfer JR. Reducing occupational sitting time and improving worker health: the take a stand project 2011. Prev Chronic Dis. 2012;9:110323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thorp AA, Dunstan DW, Clark B, et al. Stand up Australia: Sedentary Behaviour in Workers. Australia: Baker IDI Heart and Diabetes Institute, Medibank Private; 2009. [Google Scholar]
- 7.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–2667. [DOI] [PubMed] [Google Scholar]
- 8.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behaviour. Exer Sport Sci Rev. 2010;38:105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Evans RE, Fawole HO, Sheriff SA, Dall PM, Ryan CG. Point of choice prompts to reduce sitting at work: a randomised trial. Am J Prev Med. 2012;43:293–297. [DOI] [PubMed] [Google Scholar]
- 10.Healy GN, Eakin EG, LaMontagne AD, et al. Reducing sitting time in office workers: short-term efficacy of a multicomponent intervention. Prev Med. 2013;57:43–48. [DOI] [PubMed] [Google Scholar]
- 11.Ekblom-Bak E, Ekblom B, Vikström M, de Faire U, Hellénius M. The importance of non-exercise physical activity for cardiovascular health and longevity. Br J Sports Med. 2014;48:233–238. 10.1136/bjsports-2012–092038. [DOI] [PubMed] [Google Scholar]
- 12.Ross R, McGuire KA. Incidental physical activity is positively associated with cardiorespiratory fitness. Med Sci Sports Exer. 2011;43:2189–2194. 10.1249/MSS.0b013e31821e4ff2. [DOI] [PubMed] [Google Scholar]
- 13.Blair SN, LaMonte MJ, Nichaman MZ. The evolution of physical activity recommendations: How much is enough? Am J Clin Nutr. 2004;79:913S–920S. [DOI] [PubMed] [Google Scholar]
- 14.Warburton DER, Nicol CW, Bredin SD. Health benefits of physical activity: the evidence. Can Med Assoc. 2006;174:801–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ishikawa-Takata K, Ohta T, Tanaka H. How much exercise is required to reduce blood pressure in essential hypertensives: a dose–response study. Am J Hyper. 2003;16:629–633. [DOI] [PubMed] [Google Scholar]
- 16.McGillivray D. Health promotion in the workplace; a missed opportunity? Health Promot. 2002;102:60–67. [Google Scholar]
- 17.Blair SN. Taking a Stand on Sitting Down. USA: The Wellness Council of America; 2010. [Google Scholar]
- 18.Oblouck G. Haemodynamic Monitoring. Philadelphia, PA: WB Saunders; 1987. [Google Scholar]
- 19.Meaney E, Alva F, Moguel R, Meaney A, Alva J, Webel R. Formula and nomogram for the sphygmomanometric calculation of the mean arterial pressure. Heart. 2000;84:64. 10.113/heart.84.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dyer AR, Stamler J, Shekelle RB, et al. Pulse pressure, III: prognostic significance in four Chicago epidemiologic studies. J Chronic Dis. 1982;35:283–294. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell GF, Moye LA, Braunwald E, et al. Sphygmomanometrically determined pulse pressure is a powerful independent predictor of recurrent events after myocardial infarction in patients with impaired left ventricular function. Circulation. 1997;96:4254–4260. [DOI] [PubMed] [Google Scholar]
- 22.Seeley RR, Stephens TD, Tate P. Anatomy and Physiology. 3rd ed. USA: C.V. Mosby; 1995. [Google Scholar]
- 23.Schulz KF, Grimes DA. Blinding in randomised trials: hiding who got what. Lancet. 2002;359:696–700. [DOI] [PubMed] [Google Scholar]
- 24.Australian Nursing and Midwifery Accreditation Council. Review of Accreditation Standards: Registered Nurse Re-entry to the Register Programs and Entry Programs for Internationally Qualified Registered Nurses Seeking Registration in Australia: Second Consultation Paper. Canberra, Australia: Australian Nursing and Midwifery Accreditation Council; 2013. [Google Scholar]
- 25.Ali S, Rouse A. Practice audits: reliability of sphygmomanometers and blood pressure recording bias. J Hum Hypertens. 2002;16:359–361. [DOI] [PubMed] [Google Scholar]
- 26.Heart Foundation. Your Blood Pressure. Australia: Heart Foundation Australia; 2011. Available at: http://www.heartfoundation.org.au/SiteCollectionDocuments/A_Hypert_Guidelines2008_ISC_YourBloodPressure.pdf. Accessed June 3, 2013. [Google Scholar]
- 27.Vidt GD, Lang RS, Seballos RJ, Misra-Hebert A, Campbell J, Bena JF. Taking blood pressure: too important to trust to humans? Cleveland Clin J Med. 2010;77:683–688. [DOI] [PubMed] [Google Scholar]
- 28.Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Heal Psych. 1992;11:386–395. 10.1037/0278–6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- 29.Ware JE, Sherbourne CD. The MOS 36 item short-form health status (SF–36). Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 30.Reis JP, Dubose KD, Ainsworth BE, Macera CA, Yore MM. Reliability and validity of the occupational physical activity questionnaire. Amer Coll Spor Med. 2005;37:2075–2083. [DOI] [PubMed] [Google Scholar]
- 31.Karanicolas PJ, Farrokhyar F, Bhandari M. Blinding: who, what, when, why, how? Can J Surg. 2010;53:345–348. [PMC free article] [PubMed] [Google Scholar]
- 32.Chau JY, der Ploeg HP, van Uffelen JG, et al. Are workplace interventions to reduce sitting effective? A systematic review. Prev Med. 2010;51:352–256. [DOI] [PubMed] [Google Scholar]
- 33.Lally P, van Jaarsveld CHM, Potts HWW, Wardle J. How habits are formed: modelling habit formation in the real world. Eur J Soc Psych. 2010;40:998–1009. 10.1002/ejsp.674. [Google Scholar]
- 34.Reilly JJ, Penpraze V, Hislop J, Davies G, Grant S, Paton JY. Objective measurement of physical activity and sedentary behaviour: review with new data. Arch Dis Child. 2008;93:614–619. 10.1136/adc.2007.133272. [DOI] [PubMed] [Google Scholar]
- 35.Cooley PD, Pedersen SJ. A pilot study of increasing nonpurposeful movement breaks at work as a means of reducing prolonged sitting. J Environ Public Health. 2013;2013:128376. 10.1155/2013/128376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Worksafe Australia. Guidance Note for the Prevention of Occupational Overuse Syndrome in Keyboard Employment. National Occupational Health and Safety Commission. Canberra, Australia: National Government Publishing Service; 1996. [Google Scholar]
- 37.Yon BA, Johnson RK, Harvey-Berino J, Gold BC, Howard AB. Personal digital assessments are comparable to traditional diaries for dietary self-monitoring during a weight-loss program. Behav Med. 2007;30:165–175. [DOI] [PubMed] [Google Scholar]
- 38.Black HR, Weltin G, Jaffe CC. The limited echocardiogram: a modification of standard echocardiography for use in the routine evaluation of patients with systemic hypertension. Am J Cardiol. 1991;67:1027–1030. [DOI] [PubMed] [Google Scholar]
- 39.Cywinski J. The Essentials in Pressure Monitoring. Boston, MA: Martinus Nijhoff Publishers; 1980. [Google Scholar]
- 40.Ira S. Human Physiology. 5th ed. Iowa: William C Brown Publishers; 1996. [Google Scholar]
- 41.National Health Survey: SF36 Population Norms. Australia: Australian Bureau of Statistics; 1995. [Google Scholar]
- 42.Carretero OA, Oparil S. Essential hypertension. Part I: definition and etiology. Circulation. 2000;101:329–335. [DOI] [PubMed] [Google Scholar]
- 43.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes. 2008;31:661–666. [DOI] [PubMed] [Google Scholar]
- 44.Smith L, Pedersen SJ, Cooley PD. The effect of education on compliance to a workplace health and wellbeing intervention: closing the loop. Universal J Public Health. 2013;1:97–102. 10.13189/ujph.2013.010308. [Google Scholar]
- 45.Grossman E. Blood pressure: the lower the better. The con side. Diabetes. 2011;34:S308–S312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smithburger PL, Kane-Gill SL, Nestor BL, Seybert AL. Recent advances in the treatment of hypertensive emergencies. Crit Care Nurs. 2010;30:24–30. 10.4037/ccn2010664. [DOI] [PubMed] [Google Scholar]
- 47.Vrijkotte TGM, van Doornen LJP, de Gues EJC. Effects of work stress on ambulatory blood pressure, heart rate, and hear rate variability. Hypertension. 2000;35:880–886. [DOI] [PubMed] [Google Scholar]
- 48.Schnall PL, Schwartz JE, Landsbergis KW, Pickering TG. A longitudinal study of job strain and ambulatory blood pressure: results from a three-year follow-up. Psychosom Med. 1998;60:697–706. [DOI] [PubMed] [Google Scholar]
- 49.Boe J, Humerfelt S, Wedervang F. The blood pressure in a population. Acta Med Scand. 1957;321:1–336. [PubMed] [Google Scholar]
- 50.McDonough JR, Garrison GE, Hames CG. Blood pressure and hypertensive disease among Negroes and whites. Ann Int Med. 1964;61:208–227. [DOI] [PubMed] [Google Scholar]
- 51.Wills AK, Lawlor DA, Matthews FE, et al. Life course trajectories of systolic blood pressure using longitudinal data from eight UK cohorts. PLOS Med. 2011;8:e1000440. 10.1371/journal.pmed.1000440. [DOI] [PMC free article] [PubMed] [Google Scholar]