Abstract
Individuals with spinal cord injuries (SCIs) often face a number of barriers in family planning and pregnancy. These barriers can be structural (i.e. inaccessible health care provider offices and providers unfamiliar with fertility, pregnancy, and SCI) or social (i.e. friends, family, and even providers suggesting that individuals with SCI should not have children), and can affect both men and women. Additionally, much of the information about SCI and pregnancy is from a medical perspective and the psychosocial aspects of pregnancy for individuals with SCI have not been considered. 253 men and women with SCI were asked about the information they received about SCI and pregnancy, where they received this information, and how their SCI affected their family planning. The responses shared in this study can be used to inform individuals who work with people with SCI to better assist their clients or patients who have sustained SCI and are considering pregnancy.
Keywords: Pregnancy, Fertility, Spinal Cord Injury, Family Planning, United States
Introduction
People with disabilities are commonly viewed as asexual or sexually innocent (1–4), which often results in them being excluded from sex education (5) and leads to lower levels of sexual knowledge (6–9). Healthcare professionals and other service providers may have negative attitudes towards sex and disability (2,3,10), which can result in the omission of sexual education and counseling (11–13). This may lead to these topics not being discussed with people with disabilities, communicating a clear message to people with disabilities about social norms with respect to reproduction.
Women with disabilities encounter many other barriers to reproduction and reproductive health, as well. Women with disabilities have significantly higher rates of hysterectomies, may not know how their disability will affect their ability to have children, may encounter providers who urge them to terminate their pregnancy because of their disability, and may have difficulty finding providers who are capable of managing both their pregnancy and medical issues associated with their disabilities (14). Women with spinal cord injuries (SCI) are confronted with similar barriers, despite the fact that SCI often does not affect a woman’s ability to carry a child (15). Women with SCI often encounter difficulty in finding wheelchair accessible healthcare provider offices as well as offices that have accessible exam tables, stirrups, and examining instruments needed for reproductive health care (14,16). In addition, women with SCI often encounter providers who are not knowledgeable about pregnancy and SCI (14,16), and providers often incorrectly assume that women with SCI have high risk pregnancies (14).
As SCI is more common in men, there is often less information about the effects of SCI in women (17). Issues such as fertility in SCI often focus on men (18,19), and much of the research on pregnancy and SCI is purely medical (15,20,21). While all of this information is important, the family planning experiences of men and women with SCI continue to be a missing piece of the discourse on pregnancy and fertility in SCI. This paper addresses both family planning and pregnancy in individuals with SCI by identifying personal factors that influence decisions about pregnancy and SCI, concerns about pregnancy and child rearing for people with SCI, and where people with SCI get their information about family planning and pregnancy in SCI.
Methods
The data for this survey were collected at the fourth time-point in a longitudinal study on pain and fatigue in individuals with spinal cord injury. Participants were recruited through the University of Washington (Seattle, Washington), the Shepherd Center at the Virginia Crawford Research Institute (Atlanta, Georgia), and both print and web advertisements. At the fourth point of the survey, paper surveys were mailed to the 272 participants who had participated in the previous surveys, and 253 individuals completed the survey, resulting in a 93% response rate. While this survey was included as part of a larger longitudinal study, questions about SCI and pregnancy were only asked during the fourth time-point of data collection. Participants (both men and women) were asked about family planning, the effect of SCI on their family planning, and where they received advice and information about SCI and pregnancy. Questions about fertility and pregnancy were initially developed and used with a sample of individuals with multiple sclerosis, and were modified for use with individuals with SCI.
Results
The sample consisted of individuals who had sustained a spinal cord injury. Demographic information about their age and years since SCI diagnosis are presented in Table 1. Demographic data on sex, race, marital status, employment status, and injury related data are presented in Table 2.
Table 1.
Participants ages and years since diagnosis
| Minimum | Maximum | Mean | Standard Deviation |
|
|---|---|---|---|---|
| Age – Male | 19 | 85 | 48.74 | 14.81 |
| Age – Female | 21 | 75 | 44.32 | 13.12 |
| Years Since Diagnosis – Male | 2 | 57 | 13.75 | 10.53 |
| Years Since Diagnosis – Female | 2 | 43 | 12.79 | 9.63 |
Table 2.
Participant demographics
| Frequency | Percent | |
|---|---|---|
| Sex | ||
| Male | 159 | 62.8% |
| Female | 94 | 37.2% |
| Race | ||
| Non-Hispanic White | 196 | 77.5% |
| Non-Hispanic Black | 28 | 11.1% |
| Non-Hispanic Native American/Alaska Native | 3 | 1.2% |
| Non-Hispanic Asian | 5 | 2% |
| Non-Hispanic Native Hawaiian/Pacific Islander | 1 | .4% |
| Hispanic | 11 | 4.3 |
| Hispanic and Other Race | 1 | .4% |
| More than one race | 7 | 2.8% |
| Marital Status | ||
| Married/living with partner | 118 | 46.6% |
| Separated | 7 | 2.8% |
| Divorced | 51 | 20.2% |
| Never married | 20 | 7.9% |
| Widowed | 5 | 2% |
| Single | 45 | 17.8% |
| Other | 7 | 2.8% |
| Employment Status | ||
| Not Employed | 171 | 67.6% |
| Employed | 82 | 32.4% |
| Cause of Spinal Cord Injury | ||
| Motor Vehicle Accident | 121 | 47.8% |
| Fall | 50 | 19.8% |
| Sport Accident (excluding diving) | 15 | 5.9% |
| Gunshot/Wound | 14 | 5.5% |
| Diving | 10 | 4% |
| Other | 43 | 17% |
| Level of Spinal Cord Injury | ||
| C1-C4 | 47 | 18.6% |
| C5-C8 | 63 | 24.9% |
| T1-T5 | 33 | 13% |
| T6-T12 | 92 | 36.4% |
| L1-L-5, S4-S5 | 17 | 6.7% |
Approximately half of the 94 women (N=51, 54.3%) and the 159 men (n=78, 49.1%) surveyed were diagnosed with SCI prior to having completed family planning. Over half of the women in the sample had not spoken with a physician or healthcare provider about SCI and pregnancy (n=58, 61.7). Also, just over 60% of the women in the sample had been pregnant at some point in their lives (n=57, 60.6%), and just over half of the men (n=85, 53.5%) had fathered a child. Approximately one-third of these men (30.5%, n=26) and women (35.1%, n=20) who had been pregnant or fathered a child were diagnosed with SCI prior to completing family planning.
When asked about fertility, 13.4% of the sample (n=34) reported that they or their partner had discussed fertility issues with a fertility specialist, 7.1% (n=18) reported that they or their partner had taken part in an infertility evaluation, and 4.3% (n=11) reported that either they or their partner had received fertility treatment. With regards to unplanned pregnancies, 13.4% of the sample (n=34, 19 women and 15 men) stated that either they or their partner had experienced an unplanned pregnancy, 8.7% of the sample (n=22, 9 women and 13 men) stated that either they or their partner had experienced a miscarriage. Finally, two women and one man reported that they or their partner had an abortion partially because of their SCI.
A majority of both the women (n= 57, 60.6%) and men (n=83, 52.2%) had completed their family planning decisions prior to completing the survey, while 19.1% of women (n=18) and 17% of men (n=27) were in the process of decision making, and 18.1% of women (n=17) and 26.4% of men (n=42) reported that they had not thought much about family planning.
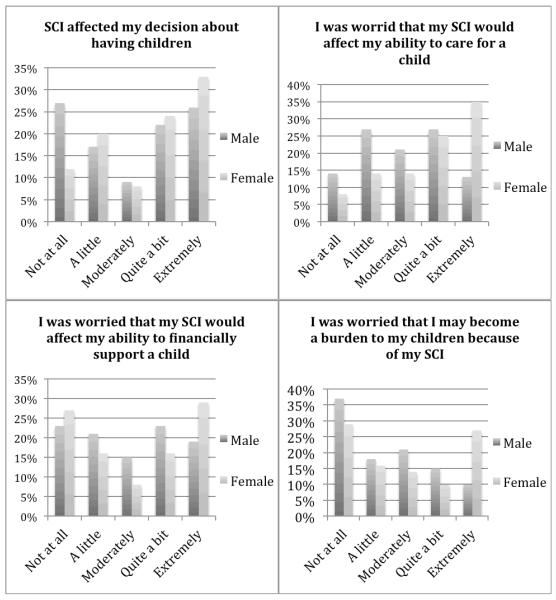
Participants were asked about how sustaining an SCI affected their attitudes towards having children. These data are reported using data from the 51 women and 78 men who were diagnosed with SCI before they had completed all of their family planning decisions. One-third (n=17, 33%) of these women reported that having an SCI factored “extremely” into their decisions about having children, with one-fourth of the men (n=20, 26%) having the same feelings. However, 27% of men (n=21) had the opposite feelings, and stated that their SCI had no effect on their decisions about having children. When asked if they felt that an SCI would affect their ability to have a child, men tended to have a more moderate response, responding “a little” (n=13, 17%), “moderately” (n=9, 7%), and “quite a bit” (n=17, 22%), as opposed to “not at all” or “extremely.” However, 25% (n=13) of women reported that their SCI affected their feelings on how they would be able to care for a child “moderately,” and 35% “extremely” (n=18). Women were more stratified on their concerns about their SCI affecting their ability to financially support a child, with 29% (n=15) reporting that they would be extremely concerned and 27% (n=14) reporting that they would not be concerned at all. Men were similarly split, with 23% (n=18) reporting that they were not concerned at all and 23% (n=18) reporting that they were “quite a bit” concerned (albeit not “extremely” concerned, as nearly one third (n=15, 29%) of the women were). Finally, when asked about their concerns that their SCI would lead them to possibly become burdens to their children, 37% of men (n=29) reported not being concerned that they would become a burden, while women had a more varied response, with 29% (n=15) not being concerned, but also 27% (n=14) being extremely concerned that they would become a burden to their children after sustaining their SCI. The results are presented in figure 1.
Fig. 1.
Concerns about childbearing
The 51 women and 78 men who were diagnosed with SCI prior to completing their family planning were asked about the advice they received about SCI and pregnancy from different sources. Two of these women (3.9%) were advised not to have children because of their SCI by a healthcare provider, while 18 had healthcare providers advise them that it was ok (35.3%). None of these men were advised not to have children by a healthcare provider, and 14 of them were advised by a healthcare provider that it was ok to have children (17.9%). Four of these women (7.8%) and none of the men were advised not to have children by their SCI physician, while 19 of the 51 women (37.3%) and 18 of the78 men (23.1%) were advised that it was ok to have children by their SCI physician. When asked about the input of their families, one of these women (2%) and none of the men were advised not to have children by their family, while 19 of the women (37.3%) and 10 of the men (12.8%) received advice from their families that it was ok to have children. One of these women (2%) and none of the men received advice from a friend not to have children because of their SCI, while 7 of these women (13.7%) and 8 of the men (10.3%) were advised that it was ok to have children by their friends. Few of the participants received advice from others with SCI, however one man (no women) was advised not to have children by someone with an SCI, while 10 of these women (19.6%) and 13 of the men (16.7%) were advised by others with SCI that it was ok to have children. Only one woman (and no men) found information in medical journals or on the internet that advised her not to have children, while 4 women (7.8%) and 5 men (6.4%) found information that advised them it was ok to have children. These results are presented in table 3.
Table 3.
Advice received about pregnancy
| FEMALE (n=94) |
MALE (n=159) |
|||||
|
| ||||||
| No | Yes | Missing | No | Yes | Missing | |
| I was diagnosed with SCI after I was finished with family planning |
51 54.3% |
42 44.7% |
1 1.1% |
78 49.1% |
78 49.1% |
3 1.9% |
|
| ||||||
| Because of SCI, I was advised NOT to have children by: |
FEMALE (n=51) |
MALE (n=78) |
||||
|
| ||||||
| A healthcare provider | 48 94.1% |
2 3.9% |
1 2% |
75 96.2% |
0 0% |
3 3.8% |
| My SCI physician | 46 90.2% |
4 7.8% |
1 2% |
75 96.2% |
0 0% |
3 3.8% |
| My family | 49 96.1% |
1 2% |
1 2% |
75 96.2% |
0 0% |
3 3.8% |
| My friends | 49 96.1% |
1 2% |
1 2% |
75 96.2% |
0 0% |
3 3.8% |
| Others with SCI | 50 98% |
0 0% |
1 2% |
74 94.9% |
1 1.3% |
3 3.8% |
| Information on the internet or in medical journals |
49 96.1% |
1 2% |
1 2% |
75 96.2% |
0 0% |
3 3.8% |
|
| ||||||
| Because of SCI, I as advised it was OK to have children by: |
FEMALE (n=51) |
MALE (n=78) |
||||
|
| ||||||
| A healthcare provider | 30 58.8% |
18 35.3% |
3 5.9% |
62 79.5% |
14 17.9% |
2 2.6% |
| My SCI physician | 29 56.9% |
19 37.3% |
3 5.9% |
58 74.4% |
18 23.1% |
2 2.6% |
| My family | 29 76.5% |
19 37.3 |
3 5.9% |
66 84.6% |
10 12.8% |
2 2.6% |
| My friends | 41 80.4% |
7 13.7% |
3 5.9% |
68 87.2% |
8 10.3% |
2 2.6% |
| Others with SCI | 38 74.5% |
10 19.6% |
3 5.9% |
63 80.8% |
13 16.7% |
2 2.6 |
| Information on the internet or in medical journals |
44 86.3% |
4 7.8% |
3 5.9% |
71 91% |
5 6.4% |
2 2.6% |
When the entire sample was asked about where they received most of their information about fertility and SCI, participants were given a list of options and were able to pick as many of the options as applied. The largest source of information about SCI and pregnancy in this sample were specialists (i.e. an SCI doctor) (n=50, 19.8%), followed by national organizations (i.e. National Spinal Cord Injury Association) (n=38, 15%). These were followed by primary care physicians (n=31, 12.3%), the internet (n=26, 10.3%), others with SCI (n=25, 9.9%), friends and family (n=10, 4%), medical journals (n=10, 4%), TV or radio (n-8, 3.2%), and finally, newspapers (n=5, 2%). However, 53 individuals (20.9%) reported that they did not seek information about fertility and SCI. These results are presented in table 4.
Table 4.
Sources of information on pregnancy and SCI
| Yes - N, (%) | |
|---|---|
| Specialists (i.e. SCI Physician) | 50, (19.8%) |
| SCI organizations (i.e. National SCI Association) | 38, (15%) |
| Primary care physician | 31, (12.3%) |
| The internet | 26, (10.3%) |
| Others with SCI | 25, (9.9%) |
| Medical journals | 10, (4%) |
| Friends and family | 10, (4%) |
| TV or radio | 8, (3.2%) |
| Newspaper | 5, (2%) |
| I did not seek information about fertility | 53, (20.9%) |
Fourteen women (14.9%) had been pregnant after their SCI diagnosis. Of these 14 women, 7 of them (50%) felt that their first pregnancy post SCI diagnosis influenced their attitudes about having more children. These seven women were asked how their first pregnancy post-SCI influenced their feelings about having more children. Four of these women (57% of the seven women who felt influenced by their first pregnancy post SCI) felt reassured that they could have children despite their SCI, and 2 women (28%) chose not to become pregnant again. One respondent declined to answer this question. None of the participants reported that they chose to adopt due to their experiences with their first pregnancy post SCI. These results are presented in table 5.
Table 5.
Experiences of pregnancy post-SCI
| No | Yes | |
|---|---|---|
| I have been pregnant since being diagnosed with SCI. | 79 84% |
14 14.9% |
| Did the experience of your first pregnancy after being diagnosed with SCI influence your attitude about having more children? (Out of 14 who had been pregnant since diagnosis). |
0 0% |
7 50% |
| My partner and/or I felt reassured that we can have children despite SCI (out of the 7 whose attitudes were influenced). |
3 42.9% |
4 57.1% |
| My partner and I were more concerned but still attempted to have more children (out of the 7 whose attitudes were influenced). |
7 100% |
0 0% |
| My partner and/or I chose not to become pregnant again (out of the 7 whose attitudes were influenced). |
5 71.4% |
2 28.6% |
| My partner and/or I chose to adopt (out of the 7 whose attitudes were influenced). |
7 100% |
0 0% |
Discussion
Pregnancy and fertility for people with SCI have been studied, however personal factors that influence family planning decisions have not previously been identified. Concerns about pregnancy and child rearing from the perspective of individuals who have sustained SCI remain under-researched, and similarly, data on where people who have sustained SCI find their information about family planning has not previously been presented.
Knowing that people who have sustained SCI get their information about pregnancy from specialists, SCI organizations, and primary care physicians can lead these healthcare providers and organizations to recognize their important roles in assisting people with SCI make decisions about pregnancy, which is consistent with previous research (22). Recognizing this importance can allow for information about pregnancy for women with SCI to be disseminated through the most accessible and commonly used channels. This demonstrates the need for these healthcare providers and consumer organizations to have up-to-date information about SCI and pregnancy and the need for these providers to be prepared to discuss pregnancy with their patients/consumers with SCI.
Understanding the effect of SCI on perceptions about pregnancy is important. The fact that sustaining a SCI affects both men’s and women’s decisions about having children, including the concerns of women about their ability to care for a child and financially support a child, indicates that this is an important topic that service providers and rehabilitation professionals (especially SCI specialists, primary care physicians, and SCI organizations) should be prepared to discuss. Finally, knowing that experiences from one’s first pregnancy after SCI influences attitudes towards future pregnancies suggest that it may be helpful for health care workers to counsel with women with SCI following the birth of a child to evaluate their satisfaction with the process, and address barriers or issues they confront in rearing the child.
This study has several limitations. First, all of the data are self-report, and in many cases participants reported on events (their pregnancies) that occurred many years ago. This may lead to a less accurate representation of how respondents thought or felt at the time. Also, the total sample size was 253, but the sub groups are smaller. For example, only 14 respondents had become pregnant since their SCI. Because no sampling strategy was used, the results cannot be generalized to a larger population of people with SCI. Nevertheless, the results of this study may at least inform clinicians the perspectives of some people living with SCI, and can serve as a basis for further qualitative and quantitative research.
Supplementary Material
Acknowledgements
This work was supported by the grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institute of Health number U01AR052171 (Amtmann, PI).
Bibliography
- 1.Anderson P, Kitchin R. Disability, space and sexuality: Access to family planning services. Social Science & Medicine. 2000;51:10. doi: 10.1016/s0277-9536(00)00019-8. [DOI] [PubMed] [Google Scholar]
- 2.Di Giulio G. Sexuality and people living with physical or developmental disabilities: A review of key issues. The Canadian Journal of Human Sexuality. 2003;12(1):53–68. [Google Scholar]
- 3.Kempton W, Kahn E. Sexuality and people with intelectual disabilities: A historical perspective. Sexuality and Disability. 1991;9(2):93–112. [Google Scholar]
- 4.O’Toole CJ, Bregante JL. Lesbians with disabilities. Sex Disabil. 1992 Sep 1;10(3):163–72. [Google Scholar]
- 5.Tilley CM. Sexuality in women with physical disabilities: A social justice or health issue? Sex Disabil. 1996 Jun 1;14(2):139–51. [Google Scholar]
- 6.McCabe MP, Cummins RA, Deeks AA. Sexuality and quality of life among people with physical disabilities. Sexuality and Disability. 2000;18(2):115–23. [Google Scholar]
- 7.McCabe MP. Sexual knowledge, experience and feelings among people with disability. Sexuality and Disability. 1999;17(2):157–70. [Google Scholar]
- 8.Murphy GH, O’Callaghan A. Capacity of adults with intellectual disabilities to consent to sexual relationships. Psychological Medicine. 2004;34:1347–57. doi: 10.1017/s0033291704001941. [DOI] [PubMed] [Google Scholar]
- 9.Szollos AA, McCabe MP. The sexuality of people with mild intellectual disability: Perceptions of clients and caregivers. Australia & New Zealand Journal of Developmental Disabilities. 1995;20(3):205–23. [Google Scholar]
- 10.Wolfe PS. The influence of personal values on issues of sexuality and disability. Sexuality and Disability. 1997;15(2):69–90. [Google Scholar]
- 11.Haboubi NHJ, Lincoln N. Views of health professionals on discussing sexual issues with patients. Disability and Rehabilitation. 2003;25(6):291–6. doi: 10.1080/0963828021000031188. [DOI] [PubMed] [Google Scholar]
- 12.Kendall M, Booth S, Fronek P, Miller D, Geraghty T. The development of a scale to assess the training needs of professionals in providing sexuality rehabilitation following spinal cord injury. Sexuality and Disability. 2003;21(1):49–64. [Google Scholar]
- 13.Verschuren JEA, Enzlin P, Geertzen JHB, Dijkstra PU, Dekker R. Sexuality in people with a lower limb amputation: a topic too hot to handle? Disability and Rehabilitation. 2013 Jan 25;:1–7. doi: 10.3109/09638288.2012.751134. [DOI] [PubMed] [Google Scholar]
- 14.Nosek MA, Howland CA, Rintala DH, Young ME, Chanpong GF. National study of women with physical disabilities: Final report. Sexuality and Disability. 2001;19(1):5–39. [Google Scholar]
- 15.Charlifue SW, Gerhart KA, Menter RR, Whiteneck GG, Manley MS. Sexual issues of women with spinal cord injuries. International Medical Society of Paraplegia. 1992;30:192–9. doi: 10.1038/sc.1992.54. [DOI] [PubMed] [Google Scholar]
- 16.Becker H, Stuifbergen A, Tinkle M. Reproductive health care experiences of women with physical disabilities: A qualitative study. Archives of Physical Medicine and Rehabilitation. 1997;78:7. doi: 10.1016/s0003-9993(97)90218-5. [DOI] [PubMed] [Google Scholar]
- 17.Singh R, Sharma SC. Sexuality and women with spinal cord injury. Sexuality and Disability. 2005;23(1):21–33. [Google Scholar]
- 18.Heruti RJ, Katz H, Menashe Y, Weissenberg R, Raviv G, Madjar I, et al. Treatment of male infertility due to spinal cord injury using rectal probe electroejaculation: the Israeli experience. Spinal Cord. 2001 Mar;39(3):168–75. doi: 10.1038/sj.sc.3101120. [DOI] [PubMed] [Google Scholar]
- 19.Monga M, Bernie J, Rajasekaran M. Male infertility and erectile dysfunction in spinal cord injury: A review. Archives of Physical Medicine and Rehabilitation. 1999 Oct;80(10):1331–9. doi: 10.1016/s0003-9993(99)90039-4. [DOI] [PubMed] [Google Scholar]
- 20.Cross LL, Meythaler JM, Tuel SM, Cross AL. Pregnancy following spinal cord injury. West J Med. 1991 May;154(5):607–11. [PMC free article] [PubMed] [Google Scholar]
- 21.Cross LL, Meythaler JM, Tuel SM, Cross AL. Pregnancy, labor and delivery post spinal cord injury. Spinal Cord. 1992;30(12):890–902. doi: 10.1038/sc.1992.166. [DOI] [PubMed] [Google Scholar]
- 22.Matter B, Feinberg M, Schomer K, Harniss M, Brown P, Johnson K. Information Needs of People With Spinal Cord Injuries. J Spinal Cord Med. 2009 Oct;32(5):545–54. doi: 10.1080/10790268.2009.11754556. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.