Abstract
Depressive symptoms are common among the U.S. population, yet research into prospective risk factors of depression among men is limited. Distorted body image is also prevalent among adolescent boys, and may be linked with elevated depression; however, longitudinal associations have rarely been measured. Thus, the aim of the current study was to assess the prospective relationship between forms of body image distortion and depressive symptoms among adolescent boys, into adulthood. Data were extracted from the National Longitudinal Study of Adolescent Health. Participants were 2,139 U.S. adolescent boys (M age = 16) who were followed prospectively over 13-years (1996 to 2009), into adulthood. Longitudinal mixed-level modeling was employed to assess the temporal prediction of body image distortion on symptoms of depression. Results revealed that boys who were average weight and viewed themselves as either very underweight (very underweight distorted; Cohen's d = .47) or overweight (overweight distorted; Cohen's d = .29) reported significantly higher levels of depressive symptoms compared to boys who accurately viewed their weight as average; this effect remained constant over the 13-year study period. These findings indicated that distortions in body image, particularly extreme distortions, are risk factors for elevated depressive symptoms among adolescent boys, and persist into early adulthood.
Keywords: Body image distortion, Body Mass Index, Depression, Males, Weight
Body image is a broad construct that comprises multiple components, including perceptions, attitudes, feelings, and behaviors toward one's body (Cash, 2004). One aspect of body image—body image distortion—is the degree to which an individual has a distorted perception regarding his or her objective appearance (Thompson & Gardner, 2004). For instance, an undistorted body image may be defined as holding perceptual and/or attitudinal beliefs which are consistent with objective data (i.e., an individual with a body mass index in the average range who views his or her weight as average). Conversely, a distorted body image represents divergence between subjective and objective data (i.e., an individual with a body mass index in the average range who views his or her weight as underweight or overweight). Although both males and females report body image distortions, there appears to be differing patterns between the genders (Cohen & Adler, 1992; Fallon & Rozin, 1985; McCreary & Sasse, 2000).
Females tend to internalize a thin appearance ideal (Striegel-Moore & Franko, 2004; Thompson & Stice, 2001), whereas males emphasize a mesomorphic (i.e., muscular) body (McCreary, 2007; McCreary & Sasse, 2000; Olivardia, Pope, Borowiecki, & Cohane, 2004). Due to varied sociocultural pressures toward ideal bodies for females versus males, it is likely that there are gender differences in the directionality of body image distortions (e.g., McCreary & Sadava, 1999). The “ideal” male physique promoted in many Western cultures is one of lean muscularity, perhaps due to beliefs that muscularity is an explicit representation of masculinity (Powlishta, Watterson, Blashill, & Kinnucan, 2008; Wienke, 1998). Indeed, muscularity and masculinity are highly related constructs (Blashill, 2011; McCreary, Saucier, & Courtenay, 2005), and concerns about desiring lean muscularity are common among adolescent and young adult males (e.g., Calzo, Corliss, Blood, Field, & Austin, 2013).
Empirically, the data bear out these gender differences in the directionality of body distortions. Between 17% and 41% of females with a normal weight body mass index (BMI) perceived themselves as being overweight (Kaplan, Busner, & Pollack, 1988; Park, 2011; ter Bogt et al., 2006). In contrast, normal weight males tend to perceive themselves as being underweight, with between 19% and 25% reporting this form of distortion (McCreary & Sadava, 2001; Park, 2011; Schiefelbein et al., 2012; ter Bogt et al., 2006). Body image distortions are not only prevalent among males, but they are also associated with maladaptive outcomes.
Males who report body image distortion are more likely to experience increased psychological distress compared to their peers who possess an undistorted view of self (e.g., McCreary, 2007). Males who reported a perceived lack of muscularity had elevated levels of body dysmorphia—characterized by a preoccupation with an imagined or slight defect in appearance (Phillips & Diaz, 1997), muscle dysmorphia (a subtype of body dysmorphic disorder)—a pathological preoccupation that one's body is not sufficiently lean and muscular (Maida & Armstrong, 2005), and depressive symptoms (Olivardia et al., 2004). Regarding depressive symptoms, some studies sampling adolescent boys have found a positive association with a distorted perception of being underweight (Lo et al., 2011; Schiefelbein et al., 2012; ter Bogt et al., 2006), while, others reported that distorted perceptions of being overweight were predictive of depressive symptoms (Al Mamun et al., 2007; Kaplan, Busner, & Pollack, 1988; Xie et al., 2006). Consequently, the literature to date on this topic has revealed that inaccurately perceiving oneself as an extreme weight has been associated with elevated levels of depression.
Depression is an important public health problem in the U.S. Depression, and depressive symptoms are common, with 12-month prevalence rates roughly 7% and 20% for major depressive disorder, and depressive symptoms, respectively (e.g., Hasin, Goodwin, Stinson, & Grant, 2005; Richards, 2011; Shim, Baltrus, Ye, & Rust, 2011). Developmentally, adolescence to early adulthood has emerged as a particularly important timeframe in which depression is likely to develop, as the ages of 15 to 29 appears to be a critical lifestage for psychopathology to emerge (Craighead, Sheets, Brosse, & Ilardi, 2007; Kessler, Berglund, Demler, Jin, Merikangas, & Walters, 2005). Moreover, not only are depressive symptoms common, they are associated with poor quality of life, morbidity, mortality, economic strain, and increased healthcare costs (e.g., Donohue & Pincus, 2007). Although it has been well documented that women are roughly twice as likely as men to be diagnosed with depression, Addis (2008) offers several points as to why studying depression among men is needed, including “masked” symptoms (perhaps as a function of conformity to male role norms), and a narrowing of the depression gender gap. Thus, identifying risk factors for the development of depression, particularly among this age group of males, has the potential to yield useful information in developing prevention interventions.
Although the literature reviewed above highlighted the association between body distortion and depression, a number of methodological factors have limited the generalization of these findings. The vast majority of studies in this area have been cross-sectional designs (Kaplan et al., 1988; Lo et al., 2011; Schiefelbein et al., 2012; ter Bogt et al., 2006; Xie et al., 2006), with only one (Al Mamun et al., 2007) employing a longitudinal methodology. Further, only two studies were conducted in the United States (Kaplan et al., 1988; Schiefelbein et al., 2012), and only two studies were based on nationally-representative samples (ter Bogt et al., 2006; Xie et al., 2006). The preponderance of cross-sectional designs precludes inferences regarding temporal prediction, and the only longitudinal study (Al Mamun et al., 2007) utilized two time points, a design that is considered limited in assessing growth over time, as two wave studies cannot describe individual trajectories of change and can confound true change with measurement error (Singer & Willett, 2003). Among studies conducted in the U.S., none have utilized a nationally-representative sample, leaving generalizations about the nature of body image distortion and depression among the population of U.S. males unclear.
With these limitations in mind, the current study sought to expand on the methodology employed by previous studies. Specifically, a secondary data analysis from a nationally-representative sample of U.S. adolescent boys, followed over 13-years (1996 to 2009), into early adulthood was utilized. In doing so, three waves of data were included, assessing body image distortion and depression from roughly age 16 to 29. This methodological design allows for analysis of true longitudinal change, with results that can be generalized to the entire U.S. population of males who fall within this age cohort. It was hypothesized that boys with body image distortion would report elevated depression, over time. No specific hypothesis regarding the directionality of the distortion (i.e., overestimation vs. underestimation of weight) was made, given the previous findings in the literature. Further, interactions between body image distortion and time in predicting depression were also explored; however, no specific hypotheses were generated.
Method
Participants
Participants were 2,139 males, whose average age was 16 (SD = 1.6, Wave 2), 22 (SD = 1.7, Wave 3), and 29 (SD = 1.6, Wave 4). The sample was 11% (n = 235) Hispanic, and the following races were identified, White (n = 1,433; 67%), Black (n = 513; 24%), Other (n = 85; 4%), Asian/Pacific Islander (n = 86; 4%), and Native American (n = 21; 1%).
Procedure
Data were extracted from Wave 2 through Wave 4 of the National Longitudinal Study of Adolescent Health (Add Health; Harris et al., 2009), a nationally-representative, longitudinal dataset of U.S. adolescents, including data from 1996 to 2009. Data from Wave 1 was not included, as objectively measured BMI was not introduced until Wave 2 of the Add Health study. Initially, a sample of 80 high schools and 52 middle schools from the U.S. was selected with unequal probability of selection. Incorporating systematic sampling methods and implicit stratification into the Add Health study design ensured this sample was representative of U.S. schools with respect to region of country, urbanicity, school size, school type, and ethnicity. Only male participants were included in the current study, and the final sample was: Wave 2 (age 16) n = 2,139; Wave 3 (age 22) n = 1,768; and Wave 4 (age 29) n = 1,786, with 83% of the sample being retained at ages 22 and 29.
Measures
Depressive symptoms
The Add Health study included items from the Center for Epidemiological Studies Depression Scale (CESD; Radloff, 1977) in each of the data collection time points. However, the number of items varied (9 to 19) between the waves as a function of the methodological design. Thus, the same core nine CESD items, which were assessed at each wave, were included in the creation of the depression variable. These nine items were: “I was bothered by things that usually don't bother me;” “I felt that I could not shake off the blues even with help from my family or friends;” “I had trouble keeping my mind on what I was doing;” “I felt depressed;” “I felt everything I did was an effort;” “I felt sad;” “I felt that people dislike me;” “I enjoyed life;” and “I felt I was just as good as other people.” Participants responded to items via a 4-point scale ranging from 0 “never/rarely” to 3 “most/all of the time.” The average of each set of nine items was computed, after accounting for reverse scoring, with higher scores denoting increased depressive symptoms. Internal consistency from the current study was: α = .75 (age 16), α = .76 (age 22), and α = .77 (age 29).
Body image distortion
To assess participants' body image distortion, seven orthogonal categories were created (at age 16) as a function of participants' subjective perception of their weight and their objectively measured BMI. Participants reported their perceived weight to be “very underweight,” “underweight,” “average,” “overweight,” or “very overweight.” For participants who were 21 year of age or older, the following categories were created: underweight (BMI < 18.5), average (BMI ≥ 18.5 and < 25), overweight (BMI ≥ 25 and < 30), and obese (BMI ≥ 30). The same BMI categories were also created for participants who were 20 years of age and younger, utilizing specific growth charts for cut points based on the CDC's (2000) guidelines for assessing BMI in children and adolescents. The following body image distortion groups were created: very underweight distortion (average or higher BMI and perceived very underweight), underweight distortion (average or higher BMI and perceived underweight), overweight distortion (average or lower BMI and perceived overweight or very overweight), average undistorted (average BMI and perceived average weight), underweight undistorted (underweight BMI and perceived underweight or very underweight), average distorted (underweight, overweight, or obese BMI and perceived average weight) and overweight undistorted (overweight or higher BMI and perceived overweight or very overweight).
Statistical analyses
The main analyses of the study were to examine body image distortion as a longitudinal predictor of depression. These analyses were conducted via mixed-level modeling in SPSS 19 (MIXED procedure). The time variable (age) provided the structure to the model with three waves of data (corresponding to average ages of 16, 22, and 29), and was entered as a fixed effect. Random intercepts and slopes were also entered, which allow different participants to have unique growth trajectories. Time invariant values of body image distortion (at age 16) were entered into the model, as fixed effects, to predict changes in the time varying depression variable. The autoregressive covariance structure was chosen based on the best goodness-of-fit (as evaluated by the Akaike Information Criterion—AIC), compared to competing covariance structures. The restricted maximum likelihood—REML—estimation method was chosen in lieu of maximum likelihood (ML) estimation, as the former approach tends to result in unbiased estimates of the variances and covariances (West, 2009).
Results
Preliminary analyses
The frequencies of the body image distortion groups at age 16 were: very underweight distortion (n = 23; 1%), underweight distortion (n = 404; 19%), overweight distortion (n = 108; 5%), average undistorted (n = 988; 46%), overweight undistorted (n = 249; 12%), average distorted (n = 312; 15%) and underweight undistorted (n = 55; 3%). The average depression scores were .55 (SE = .008, age 16), .45 (SE = .009, age 22), and .53 (SE = .01, age 29).
Primary analyses
An initial unconstrained model of depression over time revealed significant individual variance in the slope, (γ = .009, SE = .002, 95% CI [.005, .016], Wald z = 3.49, p < .0001), and intercept, (γ = .068, SE = .005, 95% CI [.058, .08], Wald z = 12.46, p < .0001). These findings indicate that participants varied in their initial depression score at age 16, as well as the rate of change over time, suggesting the utility of modeling participants' slopes and intercepts as random effects. Finally, the estimated covariance of the two random effects emerged as significant, γ = -.007, SE = .003, 95% CI [-.013, -.001], Wald z = -2.45, p = .014, indicating that the higher a participant's initial score on depression, the smaller the rate of change over time.
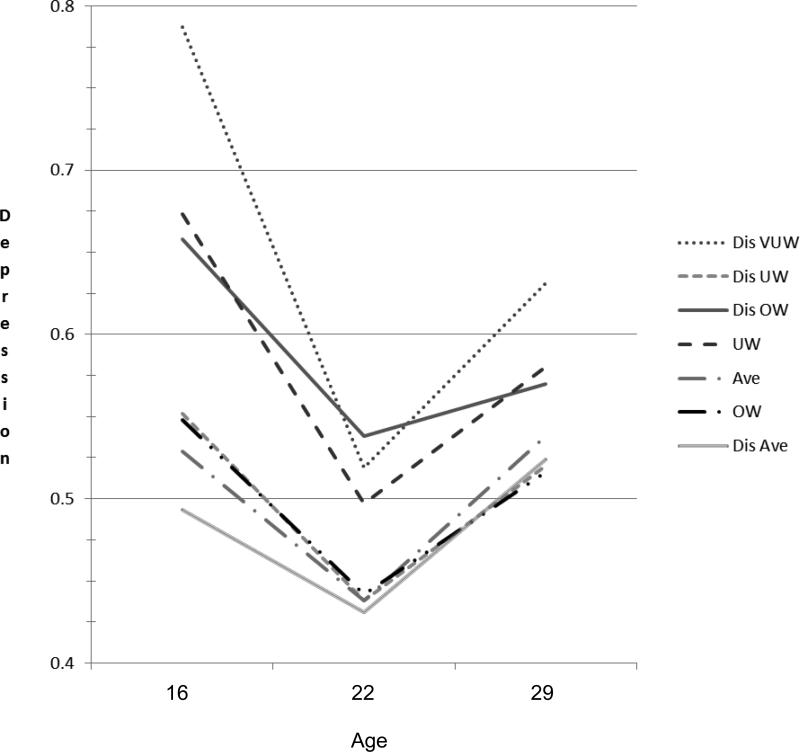
An additional model including the main effects of time, body image distortion, and their interaction term as the predictors of depression was also tested. Results revealed a significant effects of time F(2, 2944.29) = 22.87, p < .0001 and body image distortion, F(6, 2030.69) = 2.71, p = .012 (see Figure 1). Of note, the effect of body image distortion did not differ at various time points, as revealed in the non-significant interaction term, F(12, 2928.04) = 1.08, p = .36, indicating that the effect was constant over time. To follow-up the significant main effects, pairwise comparisons were conducted. Results revealed that depression scores at age 22 were lower than age 16 (-.13, SE = .02, 95% CI -.17, -.09, t2189 = -6.78, p < .0001) or age 29 (-.08, SE = .02, 95% CI -.12, -.04, t2057 = -3.80, p < .0001), and age 29 was lower than age 16 (-.05, SE = .02, 95% CI -.09, -.01, t2368 = -2.43, p = .015). Results also indicated that across time points, the very underweight distortion group reported the most elevated level of depression (.65, SE = .068, 95% CI .51, .77). Contrasted from the average undistorted group (referent), both the very underweight distortion (-.14, SE = .07, 95% CI -.28, -.01, p = .037, Cohen's d = .47) and overweight distortion (-.09, SE = .03, 95% CI -.16, -.02, p = .008, Cohen's d = .29) groups reported elevated depressive symptoms. See Table 1 for all pairwise contrasts between body image distortion groups as well as effect size parameters.
Figure 1.
Depression Scores by Body Image Distortion Group across Time. Dis VUW = very underweight distorted, Dis UW = underweight distorted, Dis OW = overweight distorted, UW = underweight undistorted, Ave = average weight undistorted, Dis Ave = average distorted, OW = overweight undistorted.
Table 1.
Depression Scores by Body Image Distortion Group across Time
| Average Across Time | ||||
|---|---|---|---|---|
| Group | M | SE | 95% CI | Cohen's d |
| 1Dist VUW | .652,5,6,7 | .07 | .51, .78 | .47 |
| 2Dist UW | .501,3 | .02 | .47, .54 | 0 |
| 3Dist OW | .592,5,6,7 | .03 | .53, .65 | .29 |
| 4UW | .587 | .04 | .50, .67 | .25 |
| 5Ave | .501,3 | .01 | .48, .52 | Referent |
| 6OW | .501,3 | .02 | .46, .54 | 0 |
| 7Dis Ave | .481,3,4 | .02 | .45, .52 | −.10 |
Note. Different subscripts denote significant (p < .05) pairwise comparisons. M = mean, SE = standard error, 95% CI = upper and lower 95% confidence intervals. Cohen's d was calculated using the average undistorted group as the comparison. Cohen's d is interpreted as .20 = small, .50 = medium, and ≥ .80 = large. Dist VUW = very underweight distorted, Dist UW = underweight distorted, Dist OW = overweight distorted, UW = underweight undistorted, Ave = average weight undistorted, OW = overweight undistorted, Dis Ave = average distorted.
Discussion
The current study sought to examine the longitudinal relationship between body image distortion and depression among U.S. males, from adolescence into early adulthood. To date, the literature has been mixed, possibly accounted for by varied methodological designs. To our knowledge, this is the first longitudinal, U.S. nationally-representative study that has explored the relationship between body image distortions and depression. Results were partially supportive of the stated hypotheses, in that boys who possessed a distorted body image at age 16, both very underweight distorted and overweight distorted, reported the highest levels of depression, across time. Further, although not significantly different from the average undistorted group, boys who accurately perceived their weight as underweight also reported elevated levels of depression. These findings remained constant across the entire 13-year span on the study.
It is possible that the very underweight distortion and overweight distortion groups also exhibited symptoms of additional forms of psychological distress. For instance, the very underweight distortion group may have been experiencing symptoms of muscle dysmorphia, as males with muscle dysmorphia typically view their bodies to be smaller than they actually are (Grieve, 2007; Olivardia, 2001, 2007). Further, mood disorders are highly comorbid with muscle dysmorphia (Pope, Pope, Menard, Fay, Olivardia, & Phillips, 2005). Regarding the overweight distorted group, it is possible that these individuals were experiencing elevated symptoms of eating pathology, given the overestimation of their own weight. Here too, mood disorders are highly comorbid (Hudson, Hirpi, Pope, & Kessler, 2007). It is also important to contrast the underweight distortion vs. the very underweight distortion groups. The former group reported relatively low levels of depression in comparison to the very underweight distortion group. This is an important finding, as it suggests that rather than making distortions about one's weight, it is the degree to which males make these underweight distortions which appear to confer a risk for elevated depressive symptoms. Indeed, perhaps these most extreme forms of distortions would be more prevalent among individuals suffering from forms of body image psychopathology. Thus, perhaps one factor that may have been driving the elevated depression among these groups was symptoms of comorbid muscle dysmorphia and/or eating disorders.
Relative low levels of depression were revealed among males who possessed distorted body image favoring an average weight self-perception, in addition to males who accurately rated their weight as average, overweight or obese. Consequently, for adolescent to young adult males, overweight and obesity appears to have modest influence on depressive symptoms. Conversely, males who accurately perceived themselves as underweight experienced elevated symptoms of depression. Indeed, either actually being underweight or perceiving oneself to be an extreme weight, while possessing a normal weight is a risk factor for elevated depressive symptoms. These findings also have implications for future research in the area of weight and mood. Specifically, it would appear prudent to include measures of self-perceived weight in addition to objective measures, given the salience of distortions in predicting depression.
Depressive symptoms also significantly changed over time. Specifically, participants at age 22 reported lower level of depressive symptoms compared at age 16 or 29, with depressive symptoms at age 29 being significantly lower than at age 16. Additionally, across the body distortion groups, age 16 was associated with the highest levels of depressive symptoms. These findings correspond to previous longitudinal data on adolescent boys depressive symptom trajectories into adulthood (e.g., Kim, Capaldi, & Stoolmiller, 2003) and highlight adolescence as a particularly vulnerable developmental window for experiencing elevated depression.
Despite the additions to the literature the current study yields, it is not without limitations. Of note was the lack of inclusion of items assessing body image dissatisfaction. Although body image distortion and body image dissatisfaction are related constructs, they are not redundant (Thompson & Gardner, 2004). Longitudinal research on body image dissatisfaction among adolescent boys has revealed that it is also predictive of elevated depression (e.g., Paxton, Neumark-Sztainer, Hannan, & Eisenberg, 2006). Therefore, future studies in the area should incorporate multidimensional aspects of body image, in lieu of focusing on one element of this broad construct. Further, the body image distortion variable was also unable to parcel perceptions of adiposity vs. muscularity. Given that both adiposity and muscle dissatisfaction are salient aspects of male body image (Ridgeway & Tylka, 2005), future research would benefit from assessing each of these components. Due to the relative exploratory nature of the current study, as well as small n's for some of the groups, moderator and mediator variables were not examined. However, this is a rich avenue future research should explore. For instance, there is some evidence that body dissatisfaction among males varies as a function of race and ethnicity (Ricciardelli, McCabe, Williams, & Thompson, 2007), and sexual orientation (Morrison, Morrison, & Sager, 2004). As a result, including these variables in prospective designs may illuminate nuanced buffers and risk factors that protect or place adolescent boys at risk for developing elevated depressive symptoms as a function of body image distortions. It is also worth noting that the very underweight distortion group included only 23 participants. This relatively small cell size leaves questions regarding its stability and generalizability. Replication of this finding via other research labs would aid in confidently suggesting this group represents a risk factor for elevated depressive symptoms. The assessment of depressive symptoms is also worth noting, as only nine of the 20 items from the CESD were consistently included in the parent study. Although the items assessed do cover a range of depressive symptoms, they also fail to capture the most comprehensive conceptualization of depression (e.g., no items on suicidality). Finally, the magnitude of the differences noted between body image distortion groups warrants comment. The difference between the very underweight distortion vs. the undistorted average weight group was medium, yielding an effect size of Cohen's d = .47. Despite this medium sized effect, it is important to view these differences within the scope of clinical significance. For instance, the mean score of .65 for the very underweight distortion group would translate to a total score of 13 if the full 20-item CESD was used. Clinical cutoff scores of major depressive disorder are typically set at 16 for the CESD (Radloff, 1977), and although the mean did not reach this threshold, a sizable proportion of participants' scores did fall at or above this level. Further, given that the distortion groups were operationalized with rather simplistic data (i.e., objective and subjective weight), which did not include any evaluative or affective components, the fact that medium-sized effects were revealed is noteworthy.
Clinical implications
The findings from the current study also have the potential to inform clinical practice. Given that body distortion appears to be a risk factor for elevated depressive symptoms among males, interventions should focus on altering these misperceptions regarding body shape. It is important to note that body distortions may be more likely to be a function of attitudinal rather than truly sensory-perceptual distortions (Thompson & Gardner, 2004); however, there is currently debate on this topic (cf. Feusner et al., 2010). Thus, targeting maladaptive beliefs regarding shape, via cognitive restructuring, would likely reap benefits in reducing distortions and depression (Cash, 2008; Wilhelm, 2006). Given the previously mentioned relationship between muscularity and masculinity (e.g., Blashill, 2011; McCreary et al., 2005), incorporating the role of male norms into treatment may also be warranted (see Parent, 2013). Mindfulness-based perceptual mirror retraining may also be an effective technique (Wilhelm, Buhlmann, Hayward, Greenberg, & Dimaite, 2010). In this strategy, patients learn to observe themselves at a reasonable (i.e., arms length) distance from a mirror using nonjudgmental descriptions regarding their appearance. This approach combined with formal cognitive restructuring has the potential to reduce distorted body perceptions and subsequent negative affect (Wilhelm, Phillips, Fama, Greenberg, & Steketee, 2011).
Conclusions
In conclusion, adolescent and young adult males, who possess distorted body image, particularly those who view their body weight as extreme, along with males who accurately assess their weight as underweight, are at risk for developing, and maintaining elevated levels of depressive symptoms. It appears that overweight and obesity has a modest effect on depressive symptoms in adolescent and adult males, and future research should include objective and subjective measures of body image variables. The utility of cognitive behavioral interventions addressing body distortion are promising, and should be treatments of choice for clinicians working with adolescent and young adult males with weight-based distortions.
Acknowledgements
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under award number K23MH096647, awarded to Dr. Blashill. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Addis ME. Gender and depression in men. Clinical Psychology: Science & Practice. 2008;15:153–168. [Google Scholar]
- Al Mamun A, Cramb S, McDermott BM, O'Callaghan M, Najman JM, Williams GM. Adolescents’ perceived weight associated with depression in young adulthood: A longitudinal study. Obesity. 2007;15:3097–3105. doi: 10.1038/oby.2007.369. [DOI] [PubMed] [Google Scholar]
- Blashill AJ. Gender roles, eating pathology, and body dissatisfaction in men: A meta-analysis. Body Image. 2011;8:1–11. doi: 10.1016/j.bodyim.2010.09.002. [DOI] [PubMed] [Google Scholar]
- Calzo JP, Corliss HL, Blood EA, Field AE, Austin SB. Development of muscularity and weight concerns in heterosexual and sexual minority males. Health Psychology. 2013;32:42–51. doi: 10.1037/a0028964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cash TF. Body image: Past, present, and future. Body Image. 2004;1:1–5. doi: 10.1016/S1740-1445(03)00011-1. [DOI] [PubMed] [Google Scholar]
- Cash TF. The body image workbook: An eight-step program for learning to like your looks. 2nd ed. New Harbinger Publications; Oakland, CA: 2008. [Google Scholar]
- Centers for Disease Control and Prevention Data table for BMI-for-age charts. 2000 Retrieved from http://www.cdc.gov/growthcharts/html_charts/bmiagerev.htm.
- Cohen LD, Adler NE. Female and male perceptions of ideal body shapes: Distorted views among Caucasian college students. Psychology of Women Quarterly. 1992;16:69–79. [Google Scholar]
- Craighead WE, Sheets ES, Brosse AL, Ilardi SS. Psychosocial treatments for major depressive disorder. In: Nathan PE, Gorman JM, editors. A guide to treatments that work. 3 ed. Oxford University Press; New York: 2007. [Google Scholar]
- Donohue JM, Pincus HA. Reducing the societal burden of depression: A review of economic costs, quality of care and effects of treatment. Pharmacoeconomics. 2007;25:7–24. doi: 10.2165/00019053-200725010-00003. [DOI] [PubMed] [Google Scholar]
- Fallon AE, Rozin P. Sex differences in perceptions of desirable body shape. Journal of Abnormal Psychology. 1985;94:102–105. doi: 10.1037//0021-843x.94.1.102. [DOI] [PubMed] [Google Scholar]
- Feusner JD, Moody T, Hembacher E, Townsend J, McKinley M, Moller H, Bookheimer S. Abnormalities of visual processing and frontostriatal systems in body dysmorphic disorder. Archives of General Psychiatry. 2010;67:197–205. doi: 10.1001/archgenpsychiatry.2009.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grieve FG. A conceptual model of factors contributing to the development of muscle dysmorphia. Eating Disorders. 2007;15:63–80. doi: 10.1080/10640260601044535. [DOI] [PubMed] [Google Scholar]
- Harris KM, Halpern CT, Whitsel E, Hussey J, Tabor J, Entzel P, Udry JR. The National Longitudinal Study of Adolescent Health: Research Design. 2009 Retrieved from http://www.cpc.unc.edu/projects/addhealth/design.
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan SL, Busner J, Pollack S. Perceived weight, actual weight, and depressive symptoms in a general adolescent sample. International Journal of Eating Disorders. 1988;7:107–113. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kim HK, Capaldi DM, Stoolmiller M. Depressive symptoms across adolescence and young adulthood in men: Predictions from parental and contextual risk factors. Development and Psychopathology. 2003;15:469–495. doi: 10.1017/s0954579403000257. [DOI] [PubMed] [Google Scholar]
- Lo WS, Ho SY, Mak KK, Lai HK, Lai YK, Lam TH. Weight misperception and psychosocial health in normal weight Chinese adolescents. International Journal of Pediatric Obesity. 2011;6:e381–e389. doi: 10.3109/17477166.2010.514342. [DOI] [PubMed] [Google Scholar]
- Maida DM, Armstrong SL. The classification of muscle dysmorphia. International Journal of Men's Health. 2005;4:73–91. [Google Scholar]
- McCreary DR. The Drive for Muscularity Scale: Description, psychometrics, and research findings. In: Thompson JK, Cafri G, editors. The muscular ideal: Psychological, social, and medical perspectives. American Psychological Association; Washington DC: 2007. pp. 87–106. [Google Scholar]
- McCreary DR, Sadava SW. TV-viewing and self-perceived health, weight, and physical fitness: Evidence for the cultivation hypothesis. Journal of Applied Social Psychology. 1999;29:2342–2361. [Google Scholar]
- McCreary DR, Sadava SW. Gender differences in relationships among perceived attractiveness, life satisfaction, and health in adults as a function of body mass index and perceived weight. Psychology of Men & Masculinity. 2001;2:108–116. [Google Scholar]
- McCreary DR, Sasse DK. An exploration of the drive for muscularity in adolescent boys and girls. Journal of American College Health. 2000;48:297–304. doi: 10.1080/07448480009596271. [DOI] [PubMed] [Google Scholar]
- McCreary DR, Saucier DM, Courtenay WH. The drive for muscularity and masculinity: Testing the associations among gender-role traits, behaviors, attitudes, and conflict. Psychology of Men & Masculinity. 2005;6:83–94. doi:10.1037/1524-9220.6.2.83. [Google Scholar]
- Morrison MA, Morrison TG, Sager CL. Does body satisfaction differ between gay men and lesbian women and heterosexual men and women?: A meta-analytic review. Body Image. 2004;1:127–138. doi: 10.1016/j.bodyim.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Olivardia R. Mirror, mirror on the wall, who's the largest of them all? The features and phenomenology of muscle dysmorphia. Harvard Review of Psychiatry. 2001;9:254–259. [PubMed] [Google Scholar]
- Olivardia R. Muscle dysmorphia: Characteristics, assessment, and treatment. In: Thompson JK, Cafri G, editors. The muscular ideal: Psychological, social, and medical perspectives. American Psychological Association; Washington DC: 2007. pp. 123–139. [Google Scholar]
- Olivardia R, Pope HG, Borowiecki JJ, Cohane GH. Biceps and body image: The relationship between muscularity and self-esteem, depression, and eating disorder symptoms. Psychology of Men & Masculinity. 2004;5:112–120. [Google Scholar]
- Parent MC. Clinical considerations in etiology, assessment, and treatment of men's muscularity-focused body image disturbance. Psychology of Men & Masculinity. 2013;14:88–100. [Google Scholar]
- Park E. Overestimation and underestimation: Adolescents’ weight perception in comparison to BMI-based weight status and how it varies across socio-demographic factors. Journal of School Health. 2011;81:57–64. doi: 10.1111/j.1746-1561.2010.00561.x. [DOI] [PubMed] [Google Scholar]
- Paxton SJ, Neumark-Sztainer D, Hannan PJ, Eisenberg ME. Body dissatisfaction prospectively predicts depressed mood and low self-esteem in adolescent girls and boys. Journal of Clinical Child & Adolescent Psychology. 2006;35:539–549. doi: 10.1207/s15374424jccp3504_5. [DOI] [PubMed] [Google Scholar]
- Phillips KA, Diaz SF. Gender differences in body dysmorphic disorder. Journal of Nervous & Mental Disease. 1997;185:570–577. doi: 10.1097/00005053-199709000-00006. [DOI] [PubMed] [Google Scholar]
- Pope CG, Pope HG, Menard W, Fay C, Olivardia R, Phillips KA. Clinical features of muscle dysmorphia among males with body dysmorphic disorder. Body Image. 2005;4:395–400. doi: 10.1016/j.bodyim.2005.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powlishta K, Watterson E, Blashill A, Kinnucan C. Physical or appearance-related gender stereotypes.. Poster presented at the Gender Development Research Conference; San Francisco, CA. Apr, 2008. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ricciardelli LA, McCabe MP, Williams RJ, Thompson JK. The role of ethnicity and culture in body image and disordered eating among males. Clinical Psychology Review. 2007;27:582–606. doi: 10.1016/j.cpr.2007.01.016. [DOI] [PubMed] [Google Scholar]
- Richards D. Prevalence and clinical course of depression: A review. Clinical Psychology Review. 2011;31:1117–1125. doi: 10.1016/j.cpr.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Ridgeway RT, Tylka TL. College men's perceptions of ideal body composition and shape. Psychology of Men & Masculinity. 2005;6:209–220. [Google Scholar]
- Schiefelbein EL, Mirchandani GG, George GC, Becker EA, Castrucci BC, Hoelscher DM. Association between depressed mood and perceived weight in middle and high school age students: Texas 2004-2005. Maternal & Child Health Journal. 2012;16:169–176. doi: 10.1007/s10995-010-0733-1. [DOI] [PubMed] [Google Scholar]
- Shim RS, Baltrus P, Ye J, Rust G. Prevalence, treatment, and control of depressive symptoms in the United States: Results from the National Health and Nutrition Examination Survey (NHANES), 2005-2008. Journal of the American Board of Family Medicine. 2011;24:33–38. doi: 10.3122/jabfm.2011.01.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press; New York, NY: 2003. [Google Scholar]
- Striegel-Moore RH, Franko DL. Body image issues among girls and women. In: Cash TF, Pruzinsky T, editors. Body image: A handbook of theory, research, and clinical practice. Guilford Press; New York, NY: 2004. pp. 183–191. [Google Scholar]
- ter Bogt TFM, van Dorsselaer SAFM, Monshouwer K, Verdurmen JEE, Engels RCME, Vollebergh WAM. Body mass index and body weight perception as risk factors for internalizing and externalizing problem behavior among adolescents. Journal of Adolescent Health. 2006;39:27–34. doi: 10.1016/j.jadohealth.2005.09.007. [DOI] [PubMed] [Google Scholar]
- Thompson JK, Gardner RM. Measuring perceptual body image among adolescents and adults. In: Cash TF, Pruzinsky T, editors. Body image: A handbook of theory, research, and clinical practice. Guilford Press; New York, NY: 2004. pp. 135–141. [Google Scholar]
- Thompson JK, Stice E. Thin-ideal internalization: Mounting evidence for a new risk factor for body-image disturbance and eating pathology. Current Directions in Psychological Science. 2001;10:181–183. [Google Scholar]
- West BT. Analyzing longitudinal data with the linear mixed models procedure in SPSS. Evaluation & the Health Professions. 2009;32:207–228. doi: 10.1177/0163278709338554. [DOI] [PubMed] [Google Scholar]
- Wienke C. Negotiating the male body: Men, masculinity, and cultural ideals. Journal of Men's Studies. 1998;6:255–282. Retrieved from http://mensstudies.metapress.com/content/c5qp785w06h01380/ [Google Scholar]
- Wilhelm S. Feeling good about the way you look: A program for overcoming body image problems. Guilford Press; New York, NY: 2006. [Google Scholar]
- Wilhelm S, Buhlmann U, Hayward LC, Greenberg JL, Dimaite R. A cognitive-behavioral treatment approach for body dysmorphic disorder. Cognitive & Behavioral Practice. 2010;17:241–247. [Google Scholar]
- Wilhelm S, Phillips KA, Fama JM, Greenberg JL, Steketee G. Modular cognitive-behavioral therapy for body dysmorphic disorder. Behavior Therapy. 2011;42:624–633. doi: 10.1016/j.beth.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie B, Chou CP, Spruijt-Metz D, Reynolds K, Clark F, Palmer PH, Johnson CA. Weight perception, academic performance, and psychological factors in Chinese adolescents. American Journal of Health Behavior. 2006;30:115–124. doi: 10.5555/ajhb.2006.30.2.115. [DOI] [PubMed] [Google Scholar]