Abstract
Transcranial magnetic stimulation (TMS) is a safe, non-invasive brain stimulation technique that uses a strong electromagnet in order to temporarily disrupt information processing in a brain region, generating a short-lived “virtual lesion.” Stimulation that interferes with task performance indicates that the affected brain region is necessary to perform the task normally. In other words, unlike neuroimaging methods such as functional magnetic resonance imaging (fMRI) that indicate correlations between brain and behavior, TMS can be used to demonstrate causal brain-behavior relations. Furthermore, by varying the duration and onset of the virtual lesion, TMS can also reveal the time course of normal processing. As a result, TMS has become an important tool in cognitive neuroscience. Advantages of the technique over lesion-deficit studies include better spatial-temporal precision of the disruption effect, the ability to use participants as their own control subjects, and the accessibility of participants. Limitations include concurrent auditory and somatosensory stimulation that may influence task performance, limited access to structures more than a few centimeters from the surface of the scalp, and the relatively large space of free parameters that need to be optimized in order for the experiment to work. Experimental designs that give careful consideration to appropriate control conditions help to address these concerns. This article illustrates these issues with TMS results that investigate the spatial and temporal contributions of the left supramarginal gyrus (SMG) to reading.
Keywords: Behavior, Issue 89, Transcranial magnetic stimulation, virtual lesion, chronometric, cognition, brain, behavior
Introduction
Transcranial magnetic stimulation (TMS) is a safe and non-invasive tool used for brain stimulation. It uses a rapidly changing electric current within a conducting coil to generate a strong, but relatively focal, magnetic field. When applied to the scalp, the magnetic field induces electrical activity in the underlying brain tissue, temporarily disrupting local cortical information processing. This transient interference effectively creates a short-lasting “virtual lesion”1,2. This technique offers a non-invasive method for drawing causal brain-behavior inferences and investigating the temporal dynamics of online neural information processing in both healthy adults and neurological patients.
By selectively interfering with regionally-specific cortical processing, TMS can be used to draw causal links between brain regions and specific behaviors3,4. That is, if stimulating a cortical area significantly affects task performance relative to appropriate control conditions, this indicates that the stimulated area is necessary to perform the task normally. Causal inferences of this sort are one of the major advantages of TMS over neuroimaging methods such as functional magnetic resonance imaging (fMRI) or positron emission tomography (PET). Unlike neuroimaging techniques that measure neural activity and correlate it with behavior, TMS offers the opportunity to perturb neural information processing and measure its effects on behavior. In this sense, it is more like traditional lesion-deficit analyses in patients with brain damage except that TMS is non-invasive and the effects are temporary and reversible. TMS also has several advantages over lesion studies. For instance, the effects of stimulation are generally more spatially precise than naturally occurring lesions, which are often large and vary greatly across patients. In addition, participants can be used as their own controls, thereby avoiding the issue of potential differences in pre-morbid abilities between patients and controls. Finally, there is insufficient time for functional reorganization to take place during TMS, meaning that recovery processes are unlikely to confound the results5. In other words, TMS offers a powerful tool for investigating causal brain-behavior relations that complements correlative techniques such as functional neuroimaging.
TMS can also be used to investigate the time course of neural information processing by using very short bursts of stimulation and varying the onset of stimulation6. Typically this involves either a single or double pulse TMS delivered to a region at different points of time within a trial. Because the effect of an individual TMS pulse occurs immediately and lasts somewhere between 5 and 40 msec7-10, this enables the researcher to map the temporal dynamics of regional neuronal activity including its onset, duration, and offset11,12. The duration of this disruption limits the temporal resolution of the technique to 10s of msec, roughly an order of magnitude coarser than electroencephalography (EEG) and magnetoencephalography (MEG). On the other hand, the timings observed in chronometric TMS studies tend to match those from invasive neurophysiological recordings better than EEG and MEG9,13. Presumably this is because EEG and MEG measure large scale neuronal synchrony that lags behind the earliest onset of activity14. In addition, like fMRI and PET, EEG and MEG are correlative measures of whole brain activity whereas chronometric TMS can not only provide important information about regional temporal dynamics but also about the necessity of the region for a given behavior.
Although TMS was originally developed for investigating the physiology of the motor system15, it was quickly adopted as a valuable tool for cognitive neuroscience. One of its earliest uses as a “virtual lesion” technique was to induce speech arrest by stimulating the left inferior frontal cortex16-18. The results confirmed the importance of Broca’s area for speech production and suggested a potential alternative to Wada testing to determine language dominance subsequent to neurosurgical interventions16,19. Now TMS is used in virtually all areas of cognitive neuroscience including attention20, memory21, visual processing22, action planning23, decision making24, and language processing25. Typically TMS induces either increased error rates or slower reaction times (RTs), both of which are taken as indicators of causal relations between brain and behavior3,4. Some studies use TMS in both its virtual lesion mode and as a chronometric tool. For example, Pitcher and colleagues11 first showed that repetitive TMS (rTMS) delivered to the occipital face area disrupted accurate facial discrimination and then used chronometric TMS to determine that this effect was only present when TMS was delivered at 60 and 100 msec, demonstrating that this particular brain region processes face-part information at an early stage of face recognition. In all of the examples mentioned here, TMS is administered “on-line”, that is during task performance, so that the effects of TMS are immediate and short lived (i.e., the effects last as long as the duration of stimulation). This contrasts with “off-line” TMS which involves either long runs of low frequency stimulation21 or short bursts of patterned stimulation26 before starting a task. In off-line TMS the effects last well beyond the duration of the TMS application itself. This article focuses exclusively on the “on-line” approach.
The initial steps in preparing any TMS experiment include identifying a stimulation protocol and choosing a localization method. Stimulation parameters include intensity, frequency and duration of TMS and are constrained by internationally defined safety requirements27,28. Each TMS experiment also requires a suitable localization procedure for positioning and orienting the coil accurately over the stimulation site. Localization can be based on standard space coordinates29 or 10 - 20 localization system30, but typically is customized to each individual participant31. For the latter, there are many options that include targeting stimulation based on each individual’s anatomy32, functionally localizing using fMRI33 or functionally localizing using TMS34. The protocol presented here advocates functional localization with TMS as part of a general protocol for on-line TMS experiments. Then an illustrative example is presented of how TMS can be used to investigate the functional contributions of the left supramarginal gyrus (SMG) to phonological processing in reading.
Protocol
This protocol was approved by the UCL Ethics Review Board (#249/001) for non-invasive brain stimulation of neurologically normal human volunteers.
1. Create the TMS protocol
Almost all TMS experiments in cognitive neuroscience use bi-phasic stimulation in conjunction with a figure-of-eight shaped coil. This provides the ability to deliver rapid trains of pulses (> 1 Hz) and target a cortical site as precisely as possible. It is possible to use mono-phasic stimulation35 or a different coil shape36, but here the standard configuration was applied.
Choose a frequency and duration of stimulation. NOTE: A common choice in cognitive neuroscience is to use 10 Hz stimulation for 500 msec from onset of the stimulus37-40.
Choose a level of intensity based on extensive pilot testing. Hold it constant across participants. NOTE: For the equipment used here, commonly used intensities range between 50 - 70% of the maximum stimulator output11,41-44.
Choose an inter-trial interval. For both practical and safety reasons, separate the stimulation trials by a minimum of 3 - 5 sec27,45.
2. Perform Head Registration
Acquire a high-resolution, T1-weighted anatomical magnetic resonance imaging (MRI) scan for each participant on a separate session prior to the TMS. Include the fiducial points in the image that will be used in step 2.3.
Load the scan into the frameless stereotaxy system before the TMS session to enable accurate targeting of stimulation sites in each participant. Mark the stimulation sites on the head at the beginning of the experiment or monitor continually throughout the experiment.
Mark four fiducial points on the participant’s image. Typically these include the tip of the nose, the bridge of the nose, and the notch above the tragus of each ear.
Provide the participant information about TMS in order for them to give informed consent to participate in the experiment.
Ask the participant to complete a TMS Safety Screen form that has been approved by the Institutional Review Board. NOTE: Permanent contradictions to TMS include a personal or family history of epilepsy, a clinical history of neurological or psychiatric problems, or implanted medical devices such as a cardiac pacemaker or cochlear implants. Not following TMS safety requirements can potentially induce syncope and seizure.
Place the subject tracker on the participant’s head; it will act as a reference when measuring fiducial points. Touch each fiducial point on the subject’s head with a pointer that comes with the stereotaxy system and save the corresponding co-ordinates on the computer. Calibrate subject’s head with the MRI image. Check the quality of registration and repeat the process if necessary.
Ask the participant to wear earplugs during stimulation to attenuate the sound of the coil discharge and avoid damage to participants’ hearing46.
Set up the TMS machine according to the choices made in Section 1.
Introduce the participant to stimulation before testing to ensure that the participant is familiarized with its sensation and tolerates well. First demonstrate stimulation on the researcher’s arm and then on the participant’s arm to acclimate the person with the sensation. NOTE: This is especially important for participants who are experiencing TMS for the first time.
Demonstrate the stimulation protocol on each of the testing sites as the sensation may be different at different locations. Place the coil on the first site as identified by the frameless stereotaxy system such that the coil is tangential to the scalp and the line of maximum magnetic flux intersects the stimulated site. NOTE: Stimulation sometimes affects facial nerves or muscles and may lead to discomfort so it is important to test whether the participant tolerates it well.
3. Perform Functional Localization
Optimize the stimulation site by customizing it to each participant. Mark several potential stimulation sites within the brain region of interest on the participant’s structural image. Locate targets at least 10mm from each other given the spatial resolution of TMS47 using a grid or anatomical marking (Figure 1).
Choose a localizer task that taps into the cognitive function of interest and has a measurable behavior (e.g., reaction times, accuracy, eye-movements). Repeat the task multiple times when testing the possible sites and create different versions of the task to avoid constant repetition of the stimuli.
Allow the participant to practice the task without stimulation until they are comfortable with it. Then introduce a second practice session with TMS randomly (or pseudo-randomly) presented on 50% of the trials so that the participant gets used to performing the task without being distracted by stimulation.
Choose a testing site and run one version of the localizer task. Immediately afterwards check the results to see whether stimulation affected performance. NOTE: In many cases, stimulating an “incorrect” site will actually facilitate responses relative to no stimulation due to inter-sensory facilitation2, in this case due to hearing the clicks and feeling the sensation of stimulation in the scalp. In addition, large effects of stimulation (i.e., over 100 msec) are often artifactual and require re-testing. If they replicate and are specific to a particularly testing site, then they may be genuine effects. Be sure to choose a robust measure of a TMS effect to be confident in localization.
If no effect is observed, choose a new testing site and repeat, otherwise test the same site again to determine whether it replicates. Test multiple sites back-to-back in the same session to ensure that they do not all produce an effect as this would indicate a non-specific TMS effect. Counterbalance the order that sites are stimulated across participants.
4. Main Task
After localization and in the same session, run the main experiment using the target site that was functionally localized. NOTE: This will involve a different task to the one used in localization but one that shares the key process of interest. For example, a rhyme judgment task can be used for localizing an area sensitive to processing the sounds of words while a homophone judgment task might be used for the main experiment. In this example, both tasks require phonological processing of written words although the specific task demands and stimuli differ.
Include sufficient control conditions to rule out non-specific effects of TMS.
Test the same site on a control task that does not include the process of interest to demonstrate functional specificity in processing.
Test a different site on the main task to demonstrate anatomical specificity of the effect.
Include additional control conditions such as sham TMS, control stimuli, or multiple time windows.
Conduct a traditional “virtual lesion” experiment using the same TMS parameters used during localization (e.g., intensity, frequency, and duration of stimulation). For chronometric TMS experiment, use the same intensity but replace the train of pulses used during localization by either a single48 or double pulse49 delivered at different onset latencies.
Representative Results
Figure 2 illustrates the results of two TMS experiments mentioned as examples. Namely, the first investigated whether the left SMG is causally involved in processing the sounds of words while the second investigated the temporal dynamics of this involvement. Figure 2A shows representative results of the first experiment where rTMS (10 Hz, 5 pulses, 55% of maximum intensity) was delivered to SMG during three tasks. The phonological task focused attention on the sounds of words (“Do these two words sound the same? knows-nose”) while the semantic task focused on their meaning (“Do these two words mean the same thing? idea-notion”). A third control task presented pairs of consonant letter strings and asked whether they were identical (“wsrft-wsrft”). Each task consisted of 100 trials. The results demonstrated that TMS significantly increased RTs relative to no stimulation in the phonological task by an average of 37 msec. In contrast, SMG stimulation had no significant effect on the RTs in the semantic or orthographic control tasks. In other words, a “virtual lesion” of the left SMG selectively interfered with processing the sounds of words, indicating the necessity of SMG in processing phonological aspects of written words44.
Figure 2B shows representative results of the chronometric experiment exploring the time course of phonological processing within SMG. Here, double pulse TMS was delivered at five different time windows after stimulus onset during the same phonological task with 100 trials divided into five equal blocks each testing different time window. When compared to the baseline condition (40/80 msec), a significant increase in RTs was observed when TMS was delivered 80/120, 120/160, and 160/200 msec after the onset of the stimulus. These results demonstrated SMG was engaged in phonological processing between 80 and 200 msec post-stimulus onset, indicating both early and sustained involvement in phonological processing44.
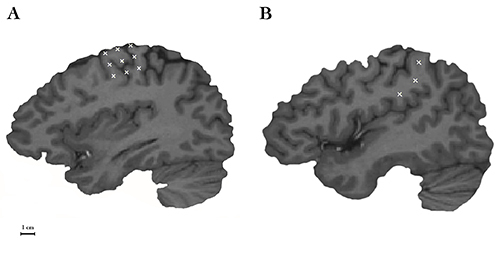 Figure 1. Two common methods of marking potential stimulation sites. (A) A first method involves placing a grid of markers over a hand motor area and testing each until TMS produces the expected effect. This approach is common for identifying a motor “hot spot”- that is, the place where stimulation produces the strongest, most reliable muscle contraction. (B) A second method applies additional anatomical constrains by placing a set of markers within a well-defined brain region. In this example, the location of the three markers is restricted to the anterior region of SMG. The first one is located superior to the termination of the posterior ascending ramus of the Sylvian fissure; the second one is at the ventral end of the anterior SMG; and the third one is approximately halfway between the other two sites. Stimulation markers are shown on a parasagittal plane of an individual MRI scan using frameless stereotaxy system. The black scale bar in the left bottom corner indicates a distance of 1 cm.
Figure 1. Two common methods of marking potential stimulation sites. (A) A first method involves placing a grid of markers over a hand motor area and testing each until TMS produces the expected effect. This approach is common for identifying a motor “hot spot”- that is, the place where stimulation produces the strongest, most reliable muscle contraction. (B) A second method applies additional anatomical constrains by placing a set of markers within a well-defined brain region. In this example, the location of the three markers is restricted to the anterior region of SMG. The first one is located superior to the termination of the posterior ascending ramus of the Sylvian fissure; the second one is at the ventral end of the anterior SMG; and the third one is approximately halfway between the other two sites. Stimulation markers are shown on a parasagittal plane of an individual MRI scan using frameless stereotaxy system. The black scale bar in the left bottom corner indicates a distance of 1 cm.
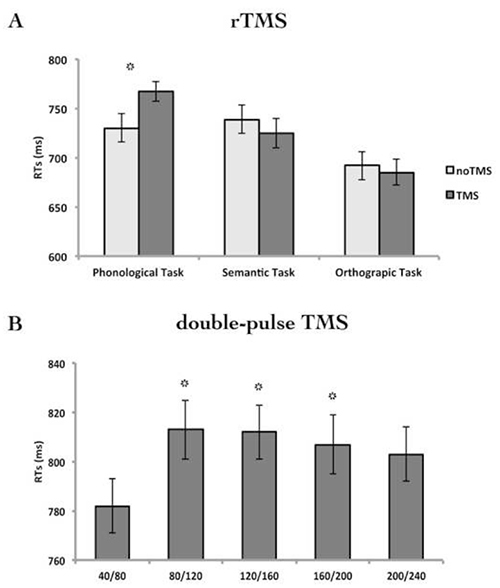 Figure 2. Reaction times (RTs) from the onset of the stimulus. (A) noTMS (light bars) and TMS (dark bars) conditions in three different language tasks. (B) Five stimulation timing conditions in the phonological task. In the example presented here, double pulses were delivered at either 40/80 msec, 80/120 msec, 120/160 msec, 160/200 msec, and 200/240 msec post stimulus onset. The first time window, 40/80 msec, was used as a baseline control condition because visual information was not expected to arrive at the SMG that rapidly. Error bars represent the standard error of the mean adjusted to correctly reflect within-subject variance50. The first experiment contains data from 12 participants and the second from 32 participants. *p < 0.05.
Figure 2. Reaction times (RTs) from the onset of the stimulus. (A) noTMS (light bars) and TMS (dark bars) conditions in three different language tasks. (B) Five stimulation timing conditions in the phonological task. In the example presented here, double pulses were delivered at either 40/80 msec, 80/120 msec, 120/160 msec, 160/200 msec, and 200/240 msec post stimulus onset. The first time window, 40/80 msec, was used as a baseline control condition because visual information was not expected to arrive at the SMG that rapidly. Error bars represent the standard error of the mean adjusted to correctly reflect within-subject variance50. The first experiment contains data from 12 participants and the second from 32 participants. *p < 0.05.
Discussion
This article presents a protocol for assessing the causal and temporal involvement of brain regions in cognitive processes using online TMS. This discussion highlights first the critical steps for creating a successful TMS protocol and then the limitations that need to be considered when designing a TMS experiment.
Because TMS protocols have a large number of free parameters, ensuring the optimal stimulation parameters is a critical step in preparing a TMS experiment. Normally, this is achieved through extensive pilot testing in order to determine the stimulation frequency, duration, intensity, inter-trial interval, and coil orientation necessary to produce robust effects. To create an effective “virtual lesion” the frequency must induce a robust effect that covers a sufficiently large time window to encompass the cognitive process of interest. As a result, both frequency and duration vary across studies. Similarly, the “right” stimulation intensity is one that ensures the magnetic field affects neural processing in the target brain region and here the main factor is the distance from the coil to the stimulation site51. Many studies identify the intensity of stimulation necessary to produce a motor response when stimulating the hand area of primary motor cortex and use this to normalize intensity across participants52,53-55. This measure, however, is not a reliable index of the optimal intensity for non-motor areas42,51,56. Another option is to use the same intensity for all participants. The chosen intensity should be effective across all pilot subjects after experimenting with a range of stimulation intensities. Additionally, the coil orientation is an important parameter that requires consideration. The specific coil orientation affects the distribution of the induced electric field within the stimulated neuronal population and therefore may influence behavior. In general, published protocols can provide a starting point that is iteratively modified during pilot testing to suit the specific experiment. Often, however, information about this pilot testing is omitted from the final manuscript, which has the unfortunate effect of hiding some key aspects of the protocol design process.
Choosing a localization procedure is also essential to ensure that stimulation is administered to the optimal site. Although many studies have successfully localized stimulation sites using anatomy-based methods that target a single location across individual participants 57,58, customizing the stimulation site for each subject individually reduces between-subject variance in behavioral results yielding a more efficient method31. Here we presented a TMS-based functional localization procedure that offers advantages over fMRI-based localization. Specifically, it avoids the problem of different spatial biases between fMRI (i.e., draining veins59) and TMS (i.e., the orientation of axons within the magnetic field6,60) that may result in the same neural response being localized to different locations. In addition, it is well known that the specific location of activation “peaks” in fMRI can vary considerably, making them sub-optimal as TMS targets55,61. Even so, a variety of different localization procedures are demonstrably effective, so the specific choice is less important that ensuring that whichever method is used provides reliable, reproducible effects.
Although the experiment data presented here used reaction times as the dependent measure, there are many other options available. For instance, some studies use accuracy instead9,12,62. In these cases, normal performance without TMS is already below ceiling levels so the disruption induced by stimulation is reflected in the accuracy scores. Other studies have measured the effects of stimulation on eye movements63,64. Most cognitive neuroscience experiments with TMS, however, use reaction times as their dependent measure13,48,65,66. Typically, the effects are on the order of tens of msec, or roughly a 10% change in reaction times67. Whatever dependent measure is used should be robust and consistent so that relatively small changes can be easily observed.
Like any experimental technique, TMS has important limitations that need to be considered when choosing this methodology. The most common ones are: i) the spatial resolution of TMS, ii) the non-specific effects associated with stimulation, and iii) safety aspects of the methodology. First, TMS has a limited depth of stimulation because the magnetic field reduces in intensity the further away it is from the coil. Consequently, it is most effective at stimulating brain regions near scalp (~2 - 3 cm)68,69 and is ineffective in stimulating deep brain structures. As a result, the only regions directly accessible to TMS are limited to the cortical mantle, although different shaped coils are being developed to reach deeper regions such as the basal ganglia69. TMS also has a spatial resolution of approximately 0.5 - 1 cm47,70-72. Thus, the method cannot be used to investigate the functional contributions from fine-grained spatial structures such as cortical columns.
A second limitation of TMS is that stimulation introduces concurrent sensory side effects as a result of the rapidly-changing magnetic field. Most notably, each magnetic pulse is accompanied by an auditory click and a tapping sensation. Therefore TMS may be inappropriate for certain auditory or somatosensory experiments where these side effects may interfere with task performance. Note, however, that online TMS has been used successfully in some auditory experiments73,74 and is therefore feasible in at least some tasks. Another consideration is that the intensity of the sensory effects differs across head locations. For example, stimulation that is administered to a location close to the ear will sound louder than locations further away. Similarly more ventral locations on the head produce greater muscle contraction than dorsal areas75,76. Because these site differences can induce experimental confounds, it is important to use either a control site with similar side-effects to the main site such as contralateral homologues77 or include control conditions/tasks that do not tap into the process of interest24,62,73,78,79.
Finally, safety considerations must always be taken into account when designing TMS experiments as it can potentially induce syncope and seizures27. To minimize this risk, internationally accepted guidelines for stimulation intensity, frequency, and duration exists, as well as for the total number of pulses and the inter-trial intervals27,28. Protocols that stay within these guidelines are believed to be safe for neurologically normal participants. It is worth noting, however, that these are as yet incomplete and that often novel TMS protocols are introduced that also prove safe. In general, the evidence suggests that when published guidelines are followed, TMS is a safe procedure with no dangerous side effects. One consequence of these limits, however, is that behavioral protocols will often need to be adjusted before they can be used with TMS. This has implications for several aspects of the design, including the length of the experiment, number of trials, number of conditions and stimulation sites that can be tested. Some of these limitations may be overcome by splitting the experiment into separate sessions such as testing different stimulation sites on different days. In those cases, it is important to ensure that localization and testing of a site are done within the same session. This minimizes experimental variance by maximizing the accuracy of the targeting. When deciding whether to use one or more testing session, the fundamental limitation is the safety of the participant – specifically, the amount of stimulation that is safe in a single session. The total stimulation involves familiarization, practice, localization (if using TMS), and testing, potentially over multiple sites, and critically depends on the number of trials per condition. Where this figure exceeds the guidelines for a single session, it is necessary to break the experiment into multiple sessions, conducted a minimum of 24 hr apart. There are no hard-and-fast rules regarding the minimum number of trials necessary for TMS experiments, but like any experiment, these can be computed using standard power calculations based on the effect size, variance, α-level (typically 0.05) and desired sensitivity. Often reasonable estimates of the effect size and variance are available as a result of the extensive pilot testing done to optimize the experimental protocol.
In summary, TMS has become an important tool with broad applications to cognitive neuroscience. This article provides a basic protocol for online TMS in conjunction with a behavioral task for investigating causal brain-behavioral relationships both in “virtual lesion” mode and also a chronometric tool for exploring the temporal dynamics of regionally-specific neural information processing.
Disclosures
The authors declare that they have no competing financial interests.
Acknowledgments
The authors have no acknowledgements.
References
- Pascual-Leone A, Bartres-Faz D, Keenan JP. Transcranial magnetic stimulation: studying the brain-behavior relationship by induction of 'virtual lesions. Philos Trans R Soc Lond B Biol Sci. 1999;354:1229–1238. doi: 10.1098/rstb.1999.0476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh V, Rushworth M. A primer of magnetic stimulation as a tool for neuropsychology. Neuropsychologia. 1999;37:125–135. [PubMed] [Google Scholar]
- Paus T. Inferring causality in brain images: a perturbation approach. Philos Trans R Soc Lond B Biol Sci. 2005;360:1109–1114. doi: 10.1098/rstb.2005.1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sack AT. Transcranial magnetic stimulation, causal structure-function mapping and networks of functional relevance. Curr Opin Neurobiol. 2006;16:593–599. doi: 10.1016/j.conb.2006.06.016. [DOI] [PubMed] [Google Scholar]
- Walsh V, Cowey A. Magnetic stimulation studies of visual cognition. Trends Cogn Sci. 1998;2:103–110. doi: 10.1016/s1364-6613(98)01134-6. [DOI] [PubMed] [Google Scholar]
- Walsh V, Pascual-Leone A. Transcranial Magnetic Stimulation. A Neurochronometrics of Mind. The MIT Press; 2003. [Google Scholar]
- Esser SK, Hill SL, Tononi G. Modeling the effects of transcranial magnetic stimulation on cortical circuits. J Neurophysiol. 2005;94:622–639. doi: 10.1152/jn.01230.2004. [DOI] [PubMed] [Google Scholar]
- Amassian VE, et al. Suppression of visual perception by magnetic coil stimulation of human occipital cortex. Electroencephalogr Clin Neurophysiol. 1989;74:458–462. doi: 10.1016/0168-5597(89)90036-1. [DOI] [PubMed] [Google Scholar]
- Corthout E, Uttl B, Walsh V, Hallett M, Cowey A. Timing of activity in early visual cortex as revealed by transcranial magnetic stimulation. Neuroreport. 1999;10:2631–2634. doi: 10.1097/00001756-199908200-00035. [DOI] [PubMed] [Google Scholar]
- Ilmoniemi RJ, et al. Neuronal responses to magnetic stimulation reveal cortical reactivity and connectivity. Neuroreport. 1997;8:3537–3540. doi: 10.1097/00001756-199711100-00024. [DOI] [PubMed] [Google Scholar]
- Pitcher D, Walsh V, Yovel G, Duchaine B. TMS evidence for the involvement of the right occipital face area in early face processing. Curr Biol. 2007;17:1568–1573. doi: 10.1016/j.cub.2007.07.063. [DOI] [PubMed] [Google Scholar]
- Amassian VE, et al. Unmasking human visual perception with the magnetic coil and its relationship to hemispheric asymmetry. Brain Res. 1993;605:312–316. doi: 10.1016/0006-8993(93)91757-j. [DOI] [PubMed] [Google Scholar]
- Duncan KJ, Pattamadilok C, Devlin JT. Investigating occipito-temporal contributions to reading with TMS. J Cogn Neurosci. 2010;22:739–750. doi: 10.1162/jocn.2009.21207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh V, Cowey A. Transcranial magnetic stimulation and cognitive neuroscience. Nat Rev Neurosci. 2000;1:73–79. doi: 10.1038/35036239. [DOI] [PubMed] [Google Scholar]
- Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet. 1985;1:1106–1107. doi: 10.1016/s0140-6736(85)92413-4. [DOI] [PubMed] [Google Scholar]
- Pascual-Leone A, Gates JR, Dhuna A. Induction of speech arrest and counting errors with rapid-rate transcranial magnetic stimulation. Neurology. 1991;41:697–702. doi: 10.1212/wnl.41.5.697. [DOI] [PubMed] [Google Scholar]
- Epstein CM, et al. Localization and characterization of speech arrest during transcranial magnetic stimulation. Clin Neurophysiol. 1999;110:1073–1079. doi: 10.1016/s1388-2457(99)00047-4. [DOI] [PubMed] [Google Scholar]
- Stewart L, Walsh V, Frith U, Rothwell JC. TMS produces two dissociable types of speech disruption. Neuroimage. 2001;13:472–478. doi: 10.1006/nimg.2000.0701. [DOI] [PubMed] [Google Scholar]
- Picht T, et al. A comparison of language mapping by preoperative navigated transcranial magnetic stimulation and direct cortical stimulation during awake surgery. Neurosurgery. 2013;72:808–819. doi: 10.1227/NEU.0b013e3182889e01. [DOI] [PubMed] [Google Scholar]
- Szczepanski SM, Kastner S. Shifting attentional priorities: control of spatial attention through hemispheric competition. J Neurosci. 2013;33:5411–5421. doi: 10.1523/JNEUROSCI.4089-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pobric G, Jefferies E, Lambon Ralph MA. Category-specific versus category-general semantic impairment induced by transcranial magnetic stimulation. Curr Biol. 2010;20:964–968. doi: 10.1016/j.cub.2010.03.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitcher D, Goldhaber T, Duchaine B, Walsh V, Kanwisher N. Two critical and functionally distinct stages of face and body perception. J Neurosci. 2012;32:15877–15885. doi: 10.1523/JNEUROSCI.2624-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neubert FX, Mars RB, Buch ER, Olivier E, Rushworth MF. Cortical and subcortical interactions during action reprogramming and their related white matter pathways. Proc Natl Acad Sci U S A. 2010;107:13240–13245. doi: 10.1073/pnas.1000674107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartwigsen G, et al. Phonological decisions require both the left and right supramarginal gyri. Proc Natl Acad Sci U S A. 2010;107:16494–16499. doi: 10.1073/pnas.1008121107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai KL, Noguchi Y, Takeuchi T, Watanabe E. Selective priming of syntactic processing by event-related transcranial magnetic stimulation of Broca's area. Neuron. 2002;35:1177–1182. doi: 10.1016/s0896-6273(02)00873-5. [DOI] [PubMed] [Google Scholar]
- Huang YZ, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron. 2005;45:201–206. doi: 10.1016/j.neuron.2004.12.033. [DOI] [PubMed] [Google Scholar]
- Rossi S, Hallett M, Rossini PM, Safety Pascual-Leone A. ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120:2008–2039. doi: 10.1016/j.clinph.2009.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassermann EM. Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, June 5-7, 1996. Electroencephalogr Clin Neurophysiol. 1998;108:1–16. doi: 10.1016/s0168-5597(97)00096-8. [DOI] [PubMed] [Google Scholar]
- Carreiras M, Pattamadilok C, Meseguer E, Barber H, Devlin JT. Broca's area plays a causal role in morphosyntactic processing. Neuropsychologia. 2012;50:816–820. doi: 10.1016/j.neuropsychologia.2012.01.016. [DOI] [PubMed] [Google Scholar]
- Knecht S, et al. Degree of language lateralization determines susceptibility to unilateral brain lesions. Nat Neurosci. 2002;5:695–699. doi: 10.1038/nn868. [DOI] [PubMed] [Google Scholar]
- Sack AT, et al. Optimizing functional accuracy of TMS in cognitive studies: a comparison of methods. J Cogn Neurosci. 2009;21:207–221. doi: 10.1162/jocn.2009.21126. [DOI] [PubMed] [Google Scholar]
- Camprodon JA, Zohary E, Brodbeck V, Pascual-Leone A. Two phases of V1 activity for visual recognition of natural images. J Cogn Neurosci. 2010;22:1262–1269. doi: 10.1162/jocn.2009.21253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanwisher N, McDermott J, Chun MM. The fusiform face area: a module in human extrastriate cortex specialized for face perception. J Neurosci. 1997;17:4302–4311. doi: 10.1523/JNEUROSCI.17-11-04302.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor PC, Nobre AC, Rushworth MF. FEF TMS affects visual cortical activity. Cereb Cortex. 2007;17:391–399. doi: 10.1093/cercor/bhj156. [DOI] [PubMed] [Google Scholar]
- Mottonen R, Watkins KE. Motor representations of articulators contribute to categorical perception of speech sounds. J Neurosci. 2009;29:9819–9825. doi: 10.1523/JNEUROSCI.6018-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levkovitz Y, et al. A randomized controlled feasibility and safety study of deep transcranial magnetic stimulation. Clin Neurophysiol. 2007;118:2730–2744. doi: 10.1016/j.clinph.2007.09.061. [DOI] [PubMed] [Google Scholar]
- Stewart L, Battelli L, Walsh V, Cowey A. Motion perception and perceptual learning studied by magnetic stimulation. Electroencephalogr Clin Neurophysiol Suppl. 1999;51:334–350. [PubMed] [Google Scholar]
- Wig GS, Grafton ST, Demos KE, Kelley WM. Reductions in neural activity underlie behavioral components of repetition priming. Nat Neurosci. 2005;8:1228–1233. doi: 10.1038/nn1515. [DOI] [PubMed] [Google Scholar]
- Bjoertomt O, Cowey A, Walsh V. Spatial neglect in near and far space investigated by repetitive transcranial magnetic stimulation. Brain. 2002;125:2012–2022. doi: 10.1093/brain/awf211. [DOI] [PubMed] [Google Scholar]
- Campana G, Pavan A, Casco C. Priming of first- and second-order motion: Mechanisms and neural substrates. Neuropsychologia. 2008;46:393–398. doi: 10.1016/j.neuropsychologia.2007.07.019. [DOI] [PubMed] [Google Scholar]
- Walsh V, Ellison A, Battelli L, Cowey A. Task-specific impairments and enhancements induced by magnetic stimulation of human visual area V5. Proc Biol Sci. 1998;265:537–543. doi: 10.1098/rspb.1998.0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart LM, Walsh V, Rothwell JC. Motor and phosphene thresholds: a transcranial magnetic stimulation correlation study. Neuropsychologia. 2001;39:415–419. doi: 10.1016/s0028-3932(00)00130-5. [DOI] [PubMed] [Google Scholar]
- Gough PM, Nobre AC, Devlin JT. Dissociating linguistic processes in the left inferior frontal cortex with transcranial magnetic stimulation. J Neurosci. 2005;25:8010–8016. doi: 10.1523/JNEUROSCI.2307-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sliwinska MW, Khadilkar M, Campbell-Ratcliffe J, Quevenco F, Devlin JT. Early and sustained supramarginal gyrus contributions to phonological processing. Front Psychol. 2012;161 doi: 10.3389/fpsyg.2012.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R, et al. Safety of different inter-train intervals for repetitive transcranial magnetic stimulation and recommendations for safe ranges of stimulation parameters. Electroencephalogr Clin Neurophysiol. 1997;105:415–421. doi: 10.1016/s0924-980x(97)00036-2. [DOI] [PubMed] [Google Scholar]
- Counter SA, Borg E, Lofqvist L. Acoustic trauma in extracranial magnetic brain stimulation. Electroencephalogr Clin Neurophysiol. 1991;78:173–184. doi: 10.1016/0013-4694(91)90031-x. [DOI] [PubMed] [Google Scholar]
- Brasil-Neto JP, et al. Optimal focal transcranial magnetic activation of the human motor cortex: effects of coil orientation, shape of the induced current pulse, and stimulus intensity. J Clin Neurophysiol. 1992;9:132–136. [PubMed] [Google Scholar]
- Schluter ND, Rushworth MF, Passingham RE, Mills KR. Temporary interference in human lateral premotor cortex suggests dominance for the selection of movements. A study using transcranial magnetic stimulation. Brain. 1998;121(5):785–799. doi: 10.1093/brain/121.5.785. [DOI] [PubMed] [Google Scholar]
- Juan CH, Walsh V. Feedback to V1: a reverse hierarchy in vision. Exp Brain Res. 2003;150:259–263. doi: 10.1007/s00221-003-1478-5. [DOI] [PubMed] [Google Scholar]
- Loftus GR, Masson MEJ. Using confidence-intervals in within-subject designs. Psychon Bull Rev. 1994;1:476–490. doi: 10.3758/BF03210951. [DOI] [PubMed] [Google Scholar]
- Stokes MG, et al. Biophysical determinants of transcranial magnetic stimulation: effects of excitability and depth of targeted area. J Neurophysiol. 2013;109:437–444. doi: 10.1152/jn.00510.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gobel S, Walsh V, Rushworth MF. The mental number line and the human angular gyrus. Neuroimage. 2001;14:1278–1289. doi: 10.1006/nimg.2001.0927. [DOI] [PubMed] [Google Scholar]
- Watkins K, Paus T. Modulation of motor excitability during speech perception: the role of Broca's area. J Cogn Neurosci. 2004;16:978–987. doi: 10.1162/0898929041502616. [DOI] [PubMed] [Google Scholar]
- Meister IG, Wilson SM, Deblieck C, Wu AD, Iacoboni M. The essential role of premotor cortex in speech perception. Curr Biol. 2007;17:1692–1696. doi: 10.1016/j.cub.2007.08.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawabata Duncan KJ, Devlin JT. Improving the reliability of functional localizers. Neuroimage. 2011;57:1022–1030. doi: 10.1016/j.neuroimage.2011.05.009. [DOI] [PubMed] [Google Scholar]
- Deblieck C, Thompson B, Iacoboni M, Wu AD. Correlation between motor and phosphene thresholds: a transcranial magnetic stimulation study. Hum Brain Mapp. 2008;29:662–670. doi: 10.1002/hbm.20427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knecht S, Sommer J, Deppe M, Steinstrater O. Scalp position and efficacy of transcranial magnetic stimulation. Clin Neurophysiol. 2005;116:1988–1993. doi: 10.1016/j.clinph.2005.04.016. [DOI] [PubMed] [Google Scholar]
- Carreiras M, et al. An anatomical signature for literacy. Nature. 2009;461:983–986. doi: 10.1038/nature08461. [DOI] [PubMed] [Google Scholar]
- Turner R. How much cortex can a vein drain? Downstream dilution of activation-related cerebral blood oxygenation changes. Neuroimage. 2002;16:1062–1067. doi: 10.1006/nimg.2002.1082. [DOI] [PubMed] [Google Scholar]
- Amassian VE, Eberle L, Maccabee PJ, Cracco RQ. Modelling magnetic coil excitation of human cerebral cortex with a peripheral nerve immersed in a brain-shaped volume conductor: the significance of fiber bending in excitation. Electroencephalogr Clin Neurophysiol. 1992;85:291–301. doi: 10.1016/0168-5597(92)90105-k. [DOI] [PubMed] [Google Scholar]
- Kung CC, Peissig JJ, Tarr MJ. Is region-of-interest overlap comparison a reliable measure of category specificity. J Cogn Neurosci. 2007;19:2019–2034. doi: 10.1162/jocn.2007.19.12.2019. [DOI] [PubMed] [Google Scholar]
- Pitcher D, Garrido L, Walsh V, Duchaine BC. Transcranial magnetic stimulation disrupts the perception and embodiment of facial expressions. J Neurosci. 2008;28:8929–8933. doi: 10.1523/JNEUROSCI.1450-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leff AP, Scott SK, Rothwell JC, Wise RJ. The planning and guiding of reading saccades: a repetitive transcranial magnetic stimulation study. Cereb Cortex. 2001;11:918–923. doi: 10.1093/cercor/11.10.918. [DOI] [PubMed] [Google Scholar]
- Acheson DJ, Hagoort P. Stimulating the brain's language network: syntactic ambiguity resolution after TMS to the inferior frontal gyrus and middle temporal gyrus. J Cogn Neurosci. 1162;25:1664–1677. doi: 10.1162/jocn_a_00430. [DOI] [PubMed] [Google Scholar]
- Stewart L, Meyer B, Frith U, Rothwell J. Left posterior BA37 is involved in object recognition: a TMS study. Neuropsychologia. 2001;39:1–6. doi: 10.1016/s0028-3932(00)00084-1. [DOI] [PubMed] [Google Scholar]
- Ashbridge E, Walsh V, Cowey A. Temporal aspects of visual search studied by transcranial magnetic stimulation. Neuropsychologia. 1997;35:1121–1131. doi: 10.1016/s0028-3932(97)00003-1. [DOI] [PubMed] [Google Scholar]
- Devlin JT, Watkins KE. Stimulating language: insights from TMS. Brain. 2007;130:610–622. doi: 10.1093/brain/awl331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth BJ, Saypol JM, Hallett M, Cohen LG. A theoretical calculation of the electric field induced in the cortex during magnetic stimulation. Electroencephalogr Clin Neurophysiol. 1991. pp. 47–56. [DOI] [PubMed]
- Zangen A, Roth Y, Voller B, Hallett M. Transcranial magnetic stimulation of deep brain regions: evidence for efficacy of the H-coil. Clin Neurophysiol. 2005;116:775–779. doi: 10.1016/j.clinph.2004.11.008. [DOI] [PubMed] [Google Scholar]
- Toschi N, Welt T, Guerrisi M, Keck ME. A reconstruction of the conductive phenomena elicited by transcranial magnetic stimulation in heterogeneous brain tissue. Phys Med. 2008;24:80–86. doi: 10.1016/j.ejmp.2008.01.005. [DOI] [PubMed] [Google Scholar]
- Ravazzani P, Ruohonen J, Grandori F, Tognola G. Magnetic stimulation of the nervous system: induced electric field in unbounded, semi-infinite, spherical, and cylindrical media. Ann Biomed Eng. 1996;24:606–616. doi: 10.1007/BF02684229. [DOI] [PubMed] [Google Scholar]
- Thielscher A, Kammer T. Linking physics with physiology in TMS: a sphere field model to determine the cortical stimulation site in TMS. Neuroimage. 2002;17:1117–1130. doi: 10.1006/nimg.2002.1282. [DOI] [PubMed] [Google Scholar]
- Pattamadilok C, Knierim IN, Kawabata Duncan KJ, Devlin JT. How does learning to read affect speech perception. J Neurosci. 2010;30:8435–8444. doi: 10.1523/JNEUROSCI.5791-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bestelmeyer PE, Belin P, Grosbras MH. Right temporal TMS impairs voice detection. Curr Biol. 2011;21:838–839. doi: 10.1016/j.cub.2011.08.046. [DOI] [PubMed] [Google Scholar]
- Mennemeier M, et al. Sham Transcranial Magnetic Stimulation Using Electrical Stimulation of the Scalp. Brain Stimul. 2009;2:168–173. doi: 10.1016/j.brs.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng ZD, Peterchev AV. Transcranial magnetic stimulation coil with electronically switchable active and sham modes. Conf Proc IEEE Eng Med Biol Soc. 2011. [DOI] [PubMed]
- Gobell SM, Rushworth MF, Walsh V. Inferior parietal rtms affects performance in an addition task. Cortex. 2006;42:774–781. doi: 10.1016/s0010-9452(08)70416-7. [DOI] [PubMed] [Google Scholar]
- Nixon P, Lazarova J, Hodinott-Hill I, Gough P, Passingham R. The inferior frontal gyrus and phonological processing: an investigation using rTMS. J Cogn Neurosci. 2004;16:289–300. doi: 10.1162/089892904322984571. [DOI] [PubMed] [Google Scholar]
- Mottonen R, Watkins KE. Using TMS to study the role of the articulatory motor system in speech perception. Aphasiology. 2012;26:1103–1118. doi: 10.1080/02687038.2011.619515. [DOI] [PMC free article] [PubMed] [Google Scholar]


