Abstract
Background
There have been conflicting results across the trials that evaluated prophylactic efficacy of short-term high-dose statin pre-treatment for prevention of contrast-induced acute kidney injury (CIAKI) in patients undergoing coronary angiography (CAG). The aim of the study was to perform an up-to-date meta-analysis regarding the efficacy of high-dose statin pre-treatment in preventing CIAKI.
Methods and Results
Randomized-controlled trials comparing high-dose statin versus low-dose statin or placebo pre-treatment for prevention of CIAKI in patients undergoing CAG were included. The primary endpoint was the incidence of CIAKI within 2–5days after CAG. The relative risk (RR) with 95% CI was the effect measure. This analysis included 13 RCTs with 5,825 total patients; about half of them (n = 2,889) were pre-treated with high-dose statin (at least 40 mg of atorvastatin) before CAG, and the remainders (n = 2,936) pretreated with low-dose statin or placebo. In random-effects model, high-dose statin pre-treatment significantly reduced the incidence of CIAKI (RR 0.45, 95% CI 0.35–0.57, p<0.001, I2 = 8.2%, NNT 16), compared with low-dose statin or placebo. The benefit of high-dose statin was consistent in both comparisons with low-dose statin (RR 0.47, 95% CI 0.34–0.65, p<0.001, I2 = 28.4%, NNT 19) or placebo (RR 0.34, 95% CI 0.21–0.58, p<0.001, I2 = 0.0%, NNT 16). In addition, high-dose statin showed significant reduction of CIAKI across various subgroups of chronic kidney disease, acute coronary syndrome, and old age (≥60years), regardless of osmolality of contrast or administration of N-acetylcystein.
Conclusions
High-dose statin pre-treatment significantly reduced overall incidence of CIAKI in patients undergoing CAG, and emerges as an effective prophylactic measure to prevent CIAKI.
Introduction
Contrast-induced acute kidney injury (CIAKI) is a well-recognized complication of coronary angiography (CAG) with iodinated contrast medium and is the third leading cause of hospital-acquired acute renal failure. CIAKI has been known to be associated with prolonged hospitalization, increased costs, and increased short and long-term morbidity and mortality. [1] The incidence of CIAKI varies widely depending on the patient's underlying co-morbidities, definition criteria, and preventive strategies. But, certain subgroup of coronary heart disease patients, especially with acute coronary syndrome or chronic kidney disease, showed higher risk for the CIAKI. [2], [3] Investigators have examined several strategies to prevent CIAKI, such as fenolopam, mannitol, theophylline, iloprost, furosemide, dopamine, hemofiltration, ascorbic acid, and N-acetylcystein (NAC). [4] However, none of the agents were proved to be effective in preventing CIAKI. [4], [5] Currently, recommendations of the European Society of Cardiology/European Association for Cardio-Thoracic Surgery (ESC/EACTS) or the ACCF/AHA/SCAI guideline are limited to the prophylactic intravenous hydration, use of iso- or low-osmolar contrast agents, and reduced dosages of contrast agents to prevent occurrence of CIAKI. [6], [7] Since a few observational studies suggested that 3-hydroxyl-3-methylglutaryl coenzyme A reductase inhibitors (statins) may reduce CIAKI incidence, several RCTs have evaluated the potential benefit of statin in prevention of CIAKI. [8], [9]Statin's postulated mechanism of kidney protection was through its pleotropic effects, i.e. antioxidant, anti-inflammatory, and antithrombotic actions. However, these previous RCTs and meta-analysis of high-dose statin pre-treatment showed disappointing results. [10]–[12] Recently, three RCTs with relatively large sample size (NAPLES II, PRATO-ACS, TRACK-D trial) have reported promising results favoring prophylactic efficacy of high-dose statin in prevention of CIAKI. [13]–[15] Considering insufficient evidences regarding efficacy of high-dose statin pre-treatment and prognostic importance of CIAKI, we therefore performed a systematic review and comprehensive meta-analysis of all published randomized control trials, in order to evaluate the efficacy of high-dose statin pre-treatment to reduce the incidence of CIAKI in various clinical situations including overall population, chronic kidney disease, or acute coronary syndrome.
Methods
Data Sources and Searches
Relevant published or unpublished studies were independently searched in PubMed, Cochrane Central Register of Controlled Trials, EMBASE, the United States National Institutes of Health registry of clinical trials (www.clinicaltrials.gov), and relevant websites (www.crtonline.org, www.clinicaltrialresults.com, www.tctmd.com, www.cardiosource.com, and www.pcronline.com) were also searched. Detailed search strategy was presented in the Method S1. The electronic search strategy was complemented by manual review of reference lists of included articles. References of recent reviews, editorials, and meta-analyses were also examined. No restrictions were imposed on language, study period, or sample size.
Study Selection
We included RCTs assessing preventive strategies for CIAKI that met following criteria. First, we selected studies which enrolled adult patients undergoing CAG with or without percutaneous coronary intervention (PCI). Second, the intervention was high-dose statin (defined as a daily dose of at least 40 mg of Atorvastatin or equivalent dose of available statins including Simvastatin, Pitavastatin, Fluvastatin, Lovastatin, Pravastatin, or Rosuvastatin), compared with low-dose statin (defined as a daily dose of less than 40 mg of Atorvastatin or equivalent dose of available statins), placebo or none of medication pre-treatment. In cases where a concomitant prophylactic measures were used (for example, NAC, sodium bicarbonate, or other preventive medications), both arms must have shared the same concomitant prophylactic measures, with only a difference in statin protocol. Finally, the incidences of post-procedural CIAKI were reported in both arms, regardless of its definition or the timing of data collection. We excluded RCTs conducted on pediatric patients (including neonates and preterm infants) and randomized crossover trials that assigned patients to both high-dose and low-dose or placebo arms.
Data Extraction and Quality Assessment
Data extraction and quality assessment was performed as previously described. [16] Summarized data as reported in the published manuscripts were used in the analysis. A standardized form was used to extract characteristics of trials, study design (including randomization sequence generation, allocation concealment, crossover between assigned groups, number of post-randomization withdrawals or follow-up loss), number of study patients, age, eligibility criteria of each trials, definition of CIAKI in each trials, baseline serum creatinine and estimated glomerular filtration rates (eGFR), mean change of serum creatinine after procedure, total cumulative dose of statin before procedure, protocols for statin treatment, hydration protocols, type or mean dosage of radio-contrast agents, the proportion of diabetes mellitus, hypertension, chronic kidney disease, timing of data collection, length of follow-up, adverse events data associated with statin treatment reported on an intention-to-treat basis. We primarily focused our analysis on the effect of prophylactic treatment with high-dose statin on the incidence of CIAKI, not on the surrogate markers of inflammation or oxidative stress. The quality of eligible RCTs was assessed using the Cochrane Collaboration's tool for assessing the risk of bias for RCTs (Table S1 in File S1). Because most previous meta-analyses have reported the methodological quality of each trial using the Jadad score, we also provided this score, as well as the Cochran Collaboration's tool, for each RCT. [17] Two investigators (JML and JP) independently performed screening of titles and abstracts, identified duplicates, reviewed full articles, and determined their eligibility. Disagreements were resolved by discussions. The last search was performed in February 2014.
Outcomes and Definitions
The primary outcome was the incidence of post-procedural CIAKI within 2–5 days after index procedure. Secondary outcomes included the incidence of post-procedural CIAKI, stratified according to the various subgroups for example, type of contrast agents (iso-osmolar or low-osmolar) used, mean age of the study patients, presence of underlying chronic kidney disease, patients with acute coronary syndrome, NAC usage, or placebo control. All of the patients and outcomes were analyzed according to the originally assigned group.
Data Synthesis and Analysis
Data synthesis and analsysis was performed as described in detail previously [16], The primary outcome was analyzed by both a random effects model and a fixed effects model. Relative risks (RR) with 95% confidence interval (CI) were presented as summary statistics. The pooled RR was calculated with the DerSimonian and Laird method for random effects model, as well as the Mantel–Haenszel method for fixed effects model. [18] To evaluate the effect of progressive chronological change in study design, such as study population, protocol of statin pre-treatment, hydration protocols or concomitant prophylactic medications including NAC or sodium bicarbonate, we evaluated the impact of publication date on the overall effect of pooled RRs for incidence of CIAKI by a cumulative meta-analysis. Stratified subgroup analyses were performed to assess treatment effects according to the control group (low-dose statin, placebo, or no medication), type of contrast agent, mean age of the patients, underlying chronic kidney disease, acute coronary syndrome, and usage of NAC along with tests for interaction derived from random effects meta-regression. Statistical heterogeneity was assessed by Cochran's Q via a χ2 test and was quantified with the I2 test. [19] Publication bias was assessed by funnel plot asymmetry, along with Egger's and Begg's test. The κ statistic was used to assess agreement between investigators for study selection. Results were considered statistically significant at 2-sided p<0.05. Statistical analysis was performed with the use of STATA/SE 12.0 (Stata Corp LP, College Station, Texas, USA). The present study was performed in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and the review protocol has not been registered (Checklist S1). [20]
Results
Search Results
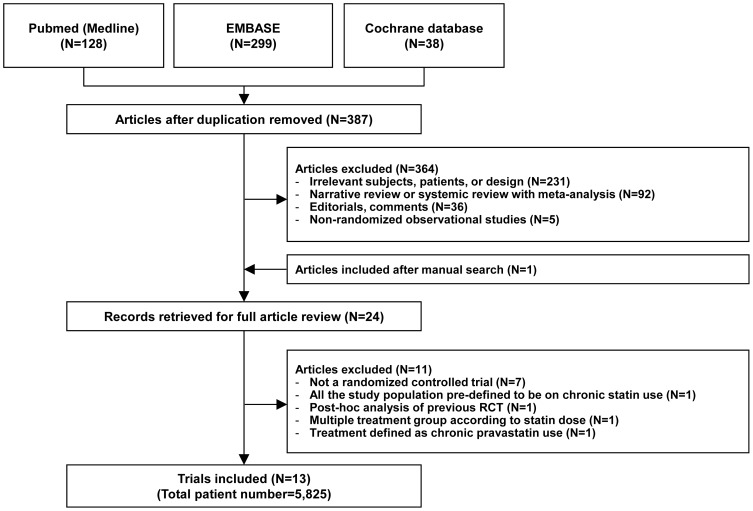
We identified 465 citations from searches as previously described. Among these, 24 studies were retrieved for detailed evaluation, of which 13 RCTs met inclusion criteria (Figure 1). [11]–[15], [21]–[28] These 13 RCTs included a total of 5,825 adult patients, 2,889 (49.6%) of which were allocated to the high-dose statin group and 2,936 (50.4%) of which were allocated to the control group (low-dose statin or placebo group). The characteristics of 11 excluded studies after full article review are summarized in the Method S2. The inter-observer agreement for study selection was high (κ = 0.92).
Figure 1. Flow diagram of trial selection.
Abbreviations: RCT, randomized controlled trial.
Trial Characteristics
The main characteristics of the individual studies are summarized in Table 1 and 2. All trials reported the incidence of CIAKI within 2-5days from index procedure using contrast agents. Four trials exclusively enrolled the patients with chronic kidney disease, which was defined as eGFR of less than 60 ml/min/1.73 m2 in PROMISS, Toso et al, and NAPLES II trial, and eGFR of between 30–90 ml/min/1.73 m2 in TRACK-D trial. [11]–[14] Only one trial (TRACK-D) exclusively enrolled type 2 diabetes mellitus patients, whereas the others enrolled the patients regardless of diabetes mellitus. [14] Among the 13 trials, 4 trials compared high-dose statin versus low-dose statin pre-treatment. [21], [22], [25], [27] Majority of trials used Atorvastin, whereas 2 trials [11], [21] used Simvastatin, and 2 trials [14], [15] used Rosuvastatin. Total cumulative dose of statin in high-dose statin group ranged from 40 mg to 560 mg of Atorvastatin equivalent dose from 1 to 7 days before CAG. The detailed medication protocols in each included trials are summarized in Table 1. The definition of CIAKI slightly differed across trials. Ten trials [11], [14], [15], [21], [22], [24]–[28] used an increase in serum creatinine of ≥0.5mg/dL or ≥25% from baseline within 48–72 hours after radiocontrast exposure, whereas 2 trials [12], [23] regarded an absolute increase in serum creatinine of ≥0.5 mg/dL within 5 days as their primary definition of CIAKI. One trial (NAPLES II) used an increase in serum cystatin C ≥10% from baseline, which was used in this analysis, although they reported the incidence of CIAKI on the base of the change in serum creatinine as secondary outcomes. [13] All trials evaluated patients with coronary artery disease undergoing CAG with or without percutaneous coronary intervention. Among the trials, 5 studies [15], [21], [26]–[28] exclusively enrolled the patients with acute coronary syndrome including unstable angina and non ST-segment elevation myocardial infarction, and 2 of these 5 studies [21], [28] further included the patients with ST-segment elevation myocardial infarction. Four trials [12], [13], [15], [24] used NAC (600 mg or 1200 mg twice daily) as additional preventive measure of CIAKI in both arms, and 1 trial [13] used sodium bicarbonate solution as primary hydration protocol.
Table 1. Characteristics of the study, trial characteristics and protocols.
| Trial (Year) | Patients number | Inclusion criteria | Definition of CIN | Medication Protocols | Contrast agent | Contrast volumes (mean), ml | Hydration protocols | |||
| Statin (N = 2889) | Control (N = 2936) | Statin | Control | Statin | Control | |||||
| PROMISS (2008) | 118 | 118 | CKD patients undergoing CAG or PCI, CrCl≤60 mL/min or SCr≥1.1 mg/dL | Increase of SCr≥0.5 mg/dL or ≥25% at 48 hours | Simvastatin 40 mg bid, 1 day pre-procedure and 1 day post-procedure | Placebo | Visipaque (iodixanol) | 173.3 | 190.9 | NS 1 mg/kg/h for 12 h before and 12 h after procedure |
| Toso et al. (2009) | 152 | 152 | CKD patients undergoing CAG or PCI, CrCl<60 mL/min | Increase of SCr≥0.5 mg/dl within 5 days. | Atorvastatin 80 mg/day 2 days pre-procedure and 2 days post-procedure, NAC 1200 mg bid from 1 day before to 1 day post-procedure | Placebo + NAC 1200 mg bid from 1day before to 1 day post-procedure | Visipaque (iodixanol) | 151.0 | 164.0 | NS 1 ml/kg/h for 12 h before and after the procedure |
| Xinwei et al. (2009) | 113 | 115 | ACS (UA/NSTEMI) including STEMI patients undergoing PCI | Increase of SCr≥0.5 mg/dL or ≥25% at 48 hours | Simvastatin 80 mg/day from admission to the day before, 20 mg/day after procedure | Simvastatin, 20 mg/day from admission to the end | Visipaque (iodixanol) for CKD, Omnipaque (iohexol) for non-CKD | 227.0 | 240.0 | NS 1 ml/kg/h for 6 to 12 h before and 12 h after procedure |
| Zhou Xia et al. (2009) | 50 | 50 | Patients undergoing CAG or PCI | Increase of SCr≥0.5 mg/dL or ≥25% at 72 hours | Atorvastatin 80 mg/day before for 1day,10 mg/day for 6days after procedure | Atorvastatin 10 mg/day for 7 days | Iopamidol 370 mg/ml | 118.7 | 112.9 | NS 1000 mL infusion, for 12 h before and 12 h after intervention |
| Acikel et al. (2010) | 80 | 80 | Patients undergoing elective CAG or PCI (excluding ACS), LDL≥70 mg/dl, eGFR≥60 ml/min/1.73 m2 | Increase of SCr≥0.5 mg/dL at 48 hours | Atorvastatin 40 mg/day 3 days pre-procedure and 2 days post-procedure | None | Omnipaque(iohexol) | 105.0 | 103.0 | NS 1 ml/kg/h starting 4 h before and continuing until 24 h after procedure |
| Ozhan et al. (2010) | 60 | 70 | Patients undergoing CAG or PCI, eGFR≥70 ml/min/1.73 m2 or SCr≤1.5 mg/dL | Increase of SCr≥0.5 mg/dL or ≥25% at 48 hours | Atorvastatin 80 mg 1 day pre-procedure and 2 days post-procedure, NAC 600 mg bid pre-procedure | No statin pre-procedure, NAC 600 mg bid pre-procedure | Iopamidol | 97.0 | 93.0 | NS 1000 ml infusion during 6 h after procedure |
| Hua et al. (2010) | 76 | 97 | Patients undergoing CAG or PCI | Increase of SCr≥0.5 mg/dL or ≥25% at 72 hours | Atorvastatin 80 mg/day pre-procedure | Atorvastatin 20 mg/day pre-procedure | Iopromide | 173.0 | 177.0 | NR |
| ARMYDA-CIN (2011) | 120 | 121 | ACS (UA/NSTEMI) Patients undergoing CAG or PCI (excluding high-risk NSTEMI requiring emergency PCI), SCr≤3 mg/dl | Increase of SCr≥0.5 mg/dL or ≥25% at 48 hours | Atorvastatin 80 mg (12 h before) → 40 mg (2 h before), 40 mg for 2days after procedure | Placebo before procedure → Atorvastatin 40 mg for 2days after procedure | Xenetix (iobitridol) | 209.0 | 213.0 | For patients CrCl <60 ml/min, NS 1 ml/kg/h for 12 h before and 24 h after intervention |
| Wei Li et al. (2012) | 78 | 83 | STEMI patients undergoing emergency PCI within 12 hours of symptom onset | Increase of SCr≥0.5 mg/dL or ≥25% at 72 hours | Atorvastatin 80 mg loading pre-procedure, long-term 40 mg/day after procedure | Placebo 801mg loading pre-procedure, long-term 40 mg/day after procedure | Ultravist 370 (iopromide) | 100.0 | 103.6 | NS 1 ml/kg/h before the procedure and for 12 h after the procedure |
| NAPLES II (2012) | 202 | 208 | CKD patients undergoing CAG or PCI, eGFR<60 ml/min/1.73 m2 | Increase of Serum Cystatin C concentration ≥10% at 24 hours | Atorvastatin 80 mg before procedure, NAC 1200 mg bid the day before and the day of procedure | No statin pre-procedure, NAC 1200 mg bid the day before and the day of procedure | Visipaque (iodixanol) | 177.0 | 184.0 | Sodium bicarbonate solution (154 mEq/L), initial bolus of 3 mL/kg/h for 1 h before procedure, 1 mL/kg/h during and for 6 h after the procedure |
| CAO et al. (2012) | 90 | 90 | Patients undergoing CAG or PCI | Increase of SCr≥0.5 mg/dL or ≥25% at 72 hours | Atorvastatin 40 mg/day from 3days before procedure, 20 mg/day after procedure | Atorvastatin 20 mg/day from 3days before procedure, 20 mg/day after procedure | NR | 162.3 | 158.9 | NR |
| PRATO-ACS (2014) | 252 | 252 | ACS (UA/NSTEMI) patients undergoing CAG or PCI (excluding STEMI and high-risk NSTEMI requiring emergency PCI), SCr≤3 mg/dl | Increase of SCr≥0.5 mg/dL or ≥25% at 72 hours | Rosuvastatin 40 mg loading → 20 mg/day before procedure, Rosuvastatin 20 mg/day continued after procedure, NAC 1200 mg bid the day before and the day of procedure | No statin pre-procedure, Atorvastatin 40 mg/day after procedure, NAC 1200 mg bid the day before and the day of procedure | Visipaque (iodixanol) | 149.7 | 138.2 | NS 1 ml/kg/h for 12 h both before and after the procedure. Hydration rate was reduced to 0.5 ml/kg/h inboth arms for patients with LVEF <40% |
| TRACK-D (2014) | 1498 | 1500 | Stage 2 or 3 CKD and type II DM patients undergoing CAG or PCI, eGFR ≥30 ml/min/1.73 m2 and <90 ml/min/1.73 m2 (excluded stage 0,1,4,5 CKD patients) | Increase of SCr≥0.5 mg/dL or ≥25% at 72 hours | Rosuvastatin 10 mg/day from 2 days before to 3 days after procedure → continued after procedure | No statin pre-procedure, Rosuvastatin 10 mg. day 3 days after procedure | Visipaque (iodixanol) | 120.0 | 110.0 | NS 1 ml/kg/h started 12 h before and continued for 24 h after procedure |
Abbreviations: ACS, acute coronary syndrome; CAG, coronary angiography; CIN, contrast induced nephropathy; CKD, chronic kidney disease; CrCl, creatinine clearance; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; LDL, low-density lipoprotein; LVEF, left ventricular ejection fraction; NAC, N-acetylcystein; NR, not reported; NS, normal saline (isotonic saline, 0.9%); NSTEMI, non ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; SCr, serum creatinine; STEMI, ST-segment elevation myocardial infarction; UA, unstable angina.
Table 2. Characteristics of the study, baseline characteristics.
| Mean age, year | Mean baseline SCr (mg/dL) | Mean baseline eGFR (ml/min) | ||||||||
| Trial (Year) | Statin | Control | Statin | Control | Statin | Control | Male proportion | Diabetes Mellitus proportion | Hypertension proportion | Additional measures |
| PROMISS (2008) | 65 | 66 | 1.29 | 1.25 | 53.46 | 55.40 | 72.5% | 25.9% | 63.2% | None |
| Toso et al. (2009) | 75 | 76 | 1.20 | 1.18 | 46.00 | 46.00 | 64.5% | 21.1% | 60.5% | NAC |
| Xinwei et al. (2009) | 65 | 66 | 0.82 | 0.83 | 86.50 | 93.60 | 36.0% | 20.6% | 63.6% | None |
| Zhou Xia et al. (2009) | 60 | 61 | 1.04 | 1.08 | 76.88 | 70.54 | 59.0% | 20.0% | 75.0% | None |
| Acikel et al. (2010) | 59 | 61 | 0.84 | 0.85 | 97.70 | 97.00 | 63.8% | 24.4% | 58.1% | None |
| Ozhan et al. (2010) | 54 | 55 | 0.88 | 0.88 | 92.00 | 89.00 | 59.2% | 16.2% | 22.3% | NAC |
| Hua et al. (2010) | 65 | 65 | 1.34 | 1.40 | 68.20 | 66.70 | 67.1% | 26.6% | 74.6% | None |
| ARMYDA-CIN (2011) | 65 | 66 | 1.04 | 1.04 | 79.80 | 77.00 | 77.6% | 28.2% | 75.1% | None |
| Wei Li et al. (2012) | 66 | 65 | 0.93 | 0.93 | NR | NR | 75.8% | 28.0% | 80.7% | None |
| NAPLES II (2012) | 70 | 70 | 1.32 | 1.29 | 42.00 | 43.00 | 54.4% | 41.2% | 86.3% | NAC, bicarbonate |
| CAO et al. (2012) | 63 | 63 | 0.85 | 0.83 | 109.60 | 106.80 | 57.2% | 21.7% | 37.2% | None |
| PRATO-ACS (2014) | 66 | 66 | 0.95 | 0.96 | 69.90 | 69.30 | 65.7% | 21.2% | 55.8% | NAC |
| TRACK-D (2014) | 62 | 61 | 1.08 | 1.07 | 74.16 | 74.43 | 65.2% | 100.0% | 71.9% | None |
Abbreviations: ACS, acute coronary syndrome; CAG, coronary angiography; CIN, contrast induced nephropathy; CKD, chronic kidney disease; CrCl, creatinine clearance; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; LDL, low-density lipoprotein; LVEF, left ventricular ejection fraction; NAC, N-acetylcystein; NR, not reported; NS, normal saline (isotonic saline, 0.9%); NSTEMI, non ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; SCr, serum creatinine; STEMI, ST-segment elevation myocardial infarction; UA, unstable angina.
Risk of Bias within Trials
Figure S1 in File S1 shows the risk of bias graph illustrating the proportion of studies with each of the judgments (‘Yes’, ‘No’, ‘Unclear’) for each entry in the Cochrane Collaboration's tool. A full description of the summary of risk of bias judgments of each study is available in Figure S2 and Table S1 in File S1. All of the included trials were RCTs and no substantial risk of bias was observed in random sequence generation. The included trials showed relatively high methodological quality. Among the 13 RCTs, 5 trials [11], [12], [15], [26], [28] had double-blinded design, whereas others were open-label or non-blinded trials. However, all trials used objective findings (serum creatinine or cystatin C) to define the primary endpoint (the incidence of CIAKI), the authors, therefore, judged that the outcomes were not likely to be influenced by lack of blinding.
Effect of Statin on the Incidence of Contrast-Induced Acute Kidney Injury
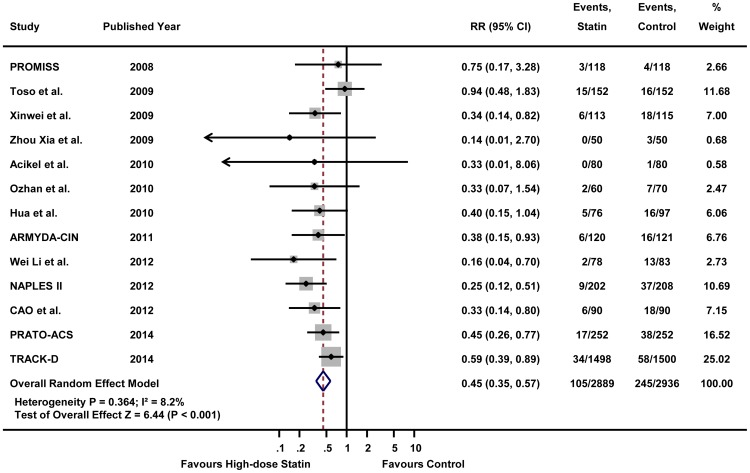
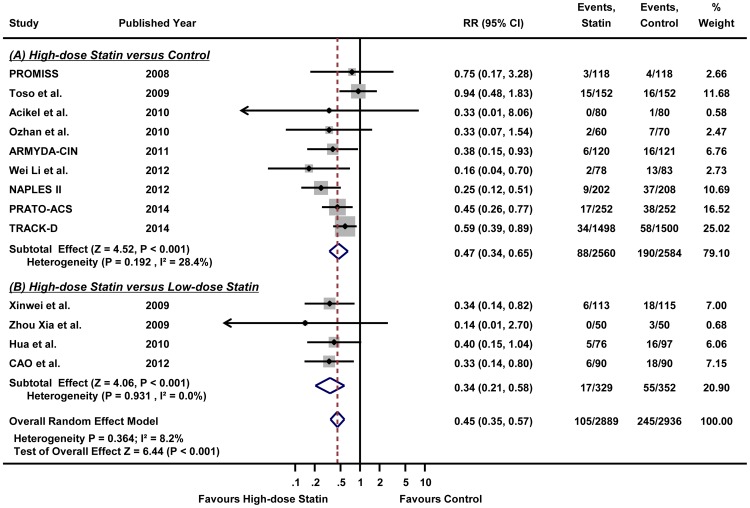
As shown in Figure 1, this meta-analysis included 13 RCTs [11]–[15], [21]–[28], all of which provided the incidence of CIAKI. Figure 2 illustrates the RRs of individual study and pooled RR in regards to the incidence of CIAKI, the primary outcome. The overall incidence of CIAKI in the intention-to-treat population was 3.6% (105/2889) in high-dose statin group and 8.3% (245/2936) in control group, respectively. In pooled analysis using random effects model, patients receiving high-dose statin pre-treatment had 55% less risk of CIAKI compared with the control group (RR 0.45, 95% CI 0.35–0.57, p<0.001) (Figure 2). A fixed effects model yielded a similar result (RR 0.44, 95% CI 0.35–0.55, p<0.001) (Figure S3 in File S1). The number needed to treat (NNT) of high-dose statin was 16 in random effects model which means that treatment of 16 patients with high-dose statin will reduce 1 event of CIAKI. There was no significant heterogeneity in either the random effects or the fixed effects model (I2 = 8.2%, heterogeneity p = 0.364 for both random and fixed effects model). Since 4 trials compared high-dose versus low-dose statin group and 9 trials compared high-dose versus placebo or no treatment, we performed stratified analysis according to the type of treatment (Figure 3). High-dose statin significantly reduced the risk of CIAKI by 53% (RR 0.47, 95% CI 0.34–0.65, p<0.001, I2 = 28.4%, heterogeneity p = 0.192) or 66% (RR 0.34, 95% CI 0.21–0.58, p<0.001, I2 = 0.0%, heterogeneity p = 0.931), when compared with placebo or low-dose statin group, respectively.
Figure 2. The effect of high-dose statin on the incidence of contrast-induced acute kidney injury by random effects model.
Forest plot with relative risks for the incidence of contrast-induced acute kidney injury associated with high-dose statin pre-treatment, compared with control group (low-dose statin or placebo) for individual trials and the pooled population. Abbreviations: CI, confidence intervals; RR, relative risks.
Figure 3. The effect of high-dose statin on the incidence of contrast-induced acute kidney injury, stratified according to the high-dose versus low-dose statin or high-dose versus placebo.
Forest plot with relative risks for the incidence of contrast-induced acute kidney injury associated with (A) high-dose statin versus low-dose statin or (B) high-dose statin versus placebo for individual trials and the pooled population. Abbreviations: CI, confidence intervals; RR, relative risks.
Visual estimation of the funnel plot indicated no apparent publication or small study effect bias with the support of the Egger's test (p = 0.128) and Begg's test (p = 0.625) (Figure S4 in File S1). No individual study unduly influenced the pooled estimate of high-dose statin for the incidence of CIAKI (Figure S5 in File S1). Cumulative meta-analysis, which sorts trials chronologically, showed no apparent progressive shift of pooled estimate of high-dose statin from a negative to a positive effect, despite of differences in practice patterns or patient populations from 2008 to 2014 (Figure S6 in File S1). Along with the significantly reduced incidence of CIAKI in high-dose statin group, mean change of post-procedural serum creatinine was also significantly lower in the high-dose statin group, compared with control group (SMD −0.37, 95% CI −0.59 to −0.15, p = 0.001) (Figure S7 in File S1).
Subgroup Analysis
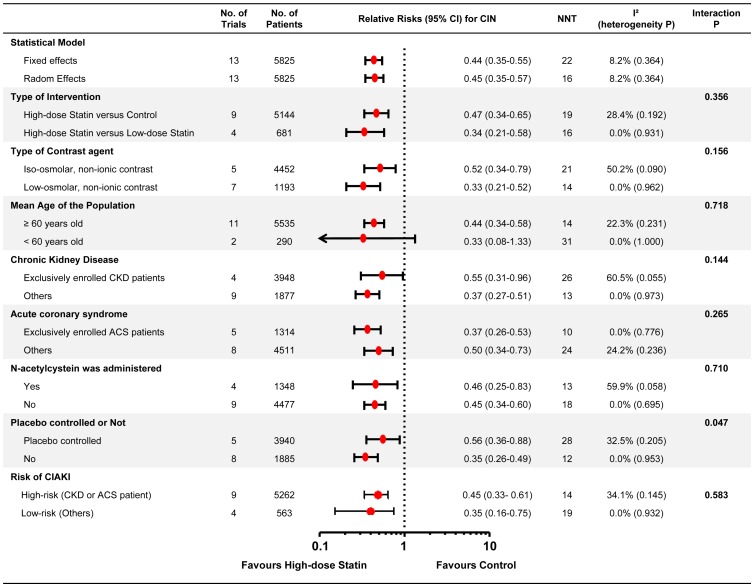
The results of subgroup analysis are presented in Figure 4. The beneficial effect of high-dose statin pre-treatment was consistent across all the subgroups, except the subgroup of age less than 60 years old. The high-dose statin showed significantly less development of CIAKI in the patients with old age (≥60 years old), underlying chronic kidney disease, or acute coronary syndrome. When the high-risk subgroup was defined with the patients with chronic kidney disease or acute coronary syndrome, the high-dose statin showed also significant beneficial effect in reducing CIAKI in both high-risk and low-risk subgroup. In addition, the protective effect of high-dose statin was also significant regardless of the osmolality of the contrast agents (iso- or low-osmolar) or concomitant treatment of NAC. Lastly, high-dose statin significantly reduced the incidence of CIAKI compared with placebo or low-dose statin. The NNT of high-dose statin ranged from 12 to 26 (Figure 4). Detailed results of pooled analysis in each subgroup are summarized in the Figure S8-S12 in File S1.
Figure 4. Subgroup analyses according to the study protocols.
The forest plot shows relative risks (by random effects model) for the incidence of contrast-induced acute kidney injury associated with high-dose statin pre-treatment, compared with control group (low-dose statin or placebo), stratified according to (1) type of intervention, (2) type of contrast agent, (3) mean age of the patients, (4) underlying chronic kidney disease, (5) acute coronary syndrome, (6) N-acetylcystein as concomitant prophylactic measure, and (7) placebo controlled trial or not. Abbreviations: ACS, acute coronary syndrome; CI, confidence intervals; CKD, chronic kidney disease; RR, relative risks.
Discussion
The results of this meta-analysis indicate that high-dose statin pre-treatment in patients undergoing CAG with or without PCI significantly reduced the incidence of CIAKI, compared with control (placebo or low-dose statin). The beneficial effect of high-dose statin was obvious in various subgroups of patients including underlying chronic kidney disease, acute coronary syndrome, or old age (≥60 years). The effect of high-dose statin was also clear regardless of type of contrast agent or concomitant treatment of NAC.
This study is the most up-to-date comprehensive meta-analysis with improved statistical power to address the effect of statin for CIAKI prevention in CAG. [10], [29]–[33] The inconclusive results of previous meta-analyses regarding the efficacy of statin pre-treatment, might mainly originate from the limited sample size of included trials. [29]–[31] Some of these studies included both randomized and non-randomized clinical trials, which might have led to potential bias. [10], [32] In the most recent meta-analysis by Li et al. [33], the authors showed significant benefit of statin pre-treatment in reducing the incidence of CIAKI. However, they argued that statin pre-treatment had no protective effect in the patients with underlying chronic kidney disease (RR 0.79, 95% CI 0.47–1.32, p = 0.37), however, the included studies in this subgroup analysis were only 3 studies with total sample size of 390 in high-dose statin versus 391 in control group. [33] In the present meta-analysis we evaluated over 5,800 patients from 13 RCTs, the benefit of high-dose statin was consistently observed in both overall population and various subgroups including patients with chronic kidney disease (RR 0.55, 95% CI 0.31–0.96, p = 0.036). The limited sample size of the pooled analysis and larger chance of type II error would explain the negative result of Li et al.
Previous studies have suggested that statin protects CIAKI through its pleotropic effect rather than its lipid lowering effect. The pleotropic effect includes enhancement of nitric oxide production, anti-inflammatory, and antioxidative effect. [34], [35] These pleotropic effects could decrease renal cell injury after iodinated contrast exposure. In the NAPLES II trial, high-dose atorvastatin reduced contrast-induced JNK activation and p53 phosphorylation which is the key steps of oxidative stress induced intrinsic apoptosis. [13] Also, statin may modulate the kidney hypoperfusion after radio-contrast exposure by down-regulation of angiotensin receptors and by decrease of endothelin-1 synthesis. [36] Lastly, anti-inflammatory effect of statin may prevent renal cell damage through decrease of pro-inflammatory cytokines which induce tissue factor expression by macrophage and activate nuclear factor-kappa B [37].
Although high-dose statin showed clear beneficial effect in preventing CIAKI, the risk of high-dose statin should be considered. Among the 13 RCTs, only 2 trials reported adverse events related with high-dose statin treatment. [14], [28] Wei Li et al. reported that the rates of hepatotoxicity (defined as>3 times of upper normal limits of alanine aminotransferase within 1 month of the procedure) were 3.85% in high-dose statin group and 1.20% in control group (p = 0.57). In TRACK-D trial, they described that the rates of muscle pain, liver function abnormality, gastrointestinal disorders, edema or rash were not statistically different between high-dose statin and control group without presentation of actual numbers of the complications. Since limited data of adverse events in the included trials, the hazard of high-dose statin pre-treatment could not be evaluated in this meta-analysis. Previous meta-analysis of 35 RCTs comparing statin versus placebo, which was not a meta-analysis for CIAKI, reported that the absolute risk differences (RD) of most frequent adverse drug reactions were as follows; transaminase elevation (RD 4.2%, 95% CI 1.5 to 6.9%), myalgia (RD 2.7%, 95% CI −3.2 to 8.7%), rhabdomyolysis (RD 0.4%, 95% CI −0.1 to 0.9%), and discontinuation due to any adverse drug reaction (RD −0.5%, 95% CI −4.3 to 3.3%). [38] According to this report, the number needed to harm of statin treatment regarding adverse drug reaction are from 24 (hepatotoxicity) to 250 (rhabdomyolysis, defined as creatinine kinase elevations ≥10 times upper normal limit). Considering substantially lower NNT of 16 in this meta-analysis for reducing CIAKI and the clinical importance of CIAKI, high-dose statin pre-treatment before CAG with or without PCI could be considered as an effective prophylactic measure to prevent CIAKI.
Limitations
Several important limitations of the study should not be ignored. First, this meta-analysis included clinically- and methodologically-diverse studies. Although we included only RCTs to the final analysis and assured statistically insignificant heterogeneity, there were some differences in the enrollment criteria (some studies exclusively enrolled patients with chronic kidney disease or diabetes mellitus), definition of the CIAKI, medication or hydration protocols. Also, basically this meta-analysis comprising 13 RCTs inherently shares the limitations of each trial. Second, variations in the type, dose, and duration of statin pretreatment among the included trials might have potential effects to our results, since all statins may not be equivalent to each other in their pleotropic and nephroprotective effects. Finally, as this study was a study-level meta-analysis, individual patient data were not included in the analysis, and therefore, we could not adjust for patient-level confounders.
Conclusion
High-dose statin pre-treatment significantly reduced the incidence of CIAKI in patients undergoing CAG. Considering prognostic importance of CIAKI and clear beneficial effect of statin in this meta-analysis, high-dose statin pre-treatment may be more actively employed as an effective prophylactic measure to prevent CIAKI.
Supporting Information
PRISMA checklist.
(DOCX)
Supporting information files. Method S1, Search Strategy on Medline, EMBASE and Cochran Central. Method S2, Characteristics of the Excluded Study. Table S1, The Cochrane Collaboration's tool for assessing risk of bias. Figure S1, Risk of bias assessment graph. Risk of bias of each included trial was assessed with the Cochrane Collaboration's tool. This ‘risk of bias graph’ illustrates the proportion of studies with each of the judgments for each entry in the tool. Green represents ‘Yes (low risk of bias)’; yellow, ‘Unclear’; red, ‘No (high risk of bias)’. Figure S2, Risk of bias assessment summary. Risk of bias of each included trial was assessed with the Cochrane Collaboration's tool. This ‘risk of bias summary’ figure presents all of the judgments in a cross-tabulation of study by entry. Green represents ‘Yes (low risk of bias)’; yellow, ‘Unclear’; red, ‘No (high risk of bias)’. Figure S3, The effect of High-dose statin on the incidence of contrast-induced nephropathy by fixed effects model. Forest plot with relative risks for the incidence of contrast-induced nephropathy associated with high-dose statin versus low-dose statin or placebo for individual trials and the pooled population. The squares and the horizontal lines indicate the relative risks (by fixed effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the frequentist meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; RR, relative risks. Figure S4, The effect of High-dose statin on mean change of post-procedural serum creatinine. Forest plot with standardized mean difference (SMD) for the mean change of post-procedural serum creatinine from the baseline value associated with high-dose statin versus low-dose statin or placebo for individual trials and the pooled population. The squares and the horizontal lines indicate the SMD (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the frequentist meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; SD, standard deviation; SMD, standardized mean difference. Figure S5, Funnel plot for evaluation of publication and small study bias. Figure S6, Influence of individual studies Abbreviations: CI, confidence intervals; RR, relative risks. Figure S7, Cumulative Meta-analysis of high-dose statin on the incidence of contrast-induced nephropathy. The first row shows the effect of one study, the second row shows the cumulative pooled estimates based on the two studies, and so on. The squares and the horizontal lines indicate the cumulative relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included. Abbreviations: CI, confidence intervals; RR, relative risks. Figure S8, The effect of High-dose statin on the incidence of contrast-induced nephropathy, stratified according to the type of contrast. The squares and the horizontal lines indicate the relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; RR, relative risks. Figure S9, The effect of High-dose statin on the incidence of contrast-induced nephropathy, stratified according to the mean age of the patients. The squares and the horizontal lines indicate the relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; RR, relative risks. Figure S10, The effect of High-dose statin on the incidence of contrast-induced nephropathy, stratified according to the underlying chronic kidney disease. The squares and the horizontal lines indicate the relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rates; RR, relative risks. Figure S11, The effect of High-dose statin on the incidence of contrast-induced nephropathy, stratified according to the acute coronary syndrome. The squares and the horizontal lines indicate the relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; RR, relative risks. Figure S12, The effect of High-dose statin on the incidence of contrast-induced nephropathy, stratified according to the concomitant treatment of N-acetylcystein. The squares and the horizontal lines indicate the relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; RR, relative risks.
(PDF)
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by grants from the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (2010-0020258) and from the IRICT, Seoul National University Hospital (A062260), sponsored by the Ministry of Health and Welfare, Republic of Korea. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. McCullough PA (2008) Contrast-induced acute kidney injury. J Am Coll Cardiol 51: 1419–1428. [DOI] [PubMed] [Google Scholar]
- 2. McCullough PA, Adam A, Becker CR, Davidson C, Lameire N, et al. (2006) Epidemiology and prognostic implications of contrast-induced nephropathy. Am J Cardiol 98: 5K–13K. [DOI] [PubMed] [Google Scholar]
- 3. Klein LW, Sheldon MW, Brinker J, Mixon TA, Skelding K, et al. (2009) The use of radiographic contrast media during PCI: a focused review: a position statement of the Society of Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 74: 728–746. [DOI] [PubMed] [Google Scholar]
- 4. Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC (2008) Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med 148: 284–294. [DOI] [PubMed] [Google Scholar]
- 5. Kitzler TM, Jaberi A, Sendlhofer G, Rehak P, Binder C, et al. (2012) Efficacy of vitamin E and N-acetylcysteine in the prevention of contrast induced kidney injury in patients with chronic kidney disease: a double blind, randomized controlled trial. Wien Klin Wochenschr 124: 312–319. [DOI] [PubMed] [Google Scholar]
- 6. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, et al. (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 82: E1–27. [DOI] [PubMed] [Google Scholar]
- 7. Task Force on Myocardial Revascularization of the European Society of C, the European Association for Cardio-Thoracic S, European Association for Percutaneous Cardiovascular I, Wijns W, Kolh P, et al (2010) Guidelines on myocardial revascularization. Eur Heart J 31: 2501–2555.20802248 [Google Scholar]
- 8. Attallah N, Yassine L, Musial J, Yee J, Fisher K (2004) The potential role of statins in contrast nephropathy. Clin Nephrol 62: 273–278. [DOI] [PubMed] [Google Scholar]
- 9. Khanal S, Attallah N, Smith DE, Kline-Rogers E, Share D, et al. (2005) Statin therapy reduces contrast-induced nephropathy: an analysis of contemporary percutaneous interventions. Am J Med 118: 843–849. [DOI] [PubMed] [Google Scholar]
- 10. Pappy R, Stavrakis S, Hennebry TA, Abu-Fadel MS (2011) Effect of statin therapy on contrast-induced nephropathy after coronary angiography: a meta-analysis. Int J Cardiol 151: 348–353. [DOI] [PubMed] [Google Scholar]
- 11.Jo SH, Koo BK, Park JS, Kang HJ, Cho YS, et al. (2008) Prevention of radiocontrast medium-induced nephropathy using short-term high-dose simvastatin in patients with renal insufficiency undergoing coronary angiography (PROMISS) trial—a randomized controlled study. Am Heart J 155: 499 e491–498. [DOI] [PubMed]
- 12. Toso A, Maioli M, Leoncini M, Gallopin M, Tedeschi D, et al. (2010) Usefulness of atorvastatin (80 mg) in prevention of contrast-induced nephropathy in patients with chronic renal disease. Am J Cardiol 105: 288–292. [DOI] [PubMed] [Google Scholar]
- 13. Quintavalle C, Fiore D, De Micco F, Visconti G, Focaccio A, et al. (2012) Impact of a high loading dose of atorvastatin on contrast-induced acute kidney injury. Circulation 126: 3008–3016. [DOI] [PubMed] [Google Scholar]
- 14. Han Y, Zhu G, Han L, Hou F, Huang W, et al. (2014) Short-term rosuvastatin therapy for prevention of contrast-induced acute kidney injury in patients with diabetes and chronic kidney disease. J Am Coll Cardiol 63: 62–70. [DOI] [PubMed] [Google Scholar]
- 15. Leoncini M, Toso A, Maioli M, Tropeano F, Villani S, et al. (2014) Early high-dose rosuvastatin for contrast-induced nephropathy prevention in acute coronary syndrome: Results from the PRATO-ACS Study (Protective Effect of Rosuvastatin and Antiplatelet Therapy On contrast-induced acute kidney injury and myocardial damage in patients with Acute Coronary Syndrome). J Am Coll Cardiol 63: 71–79. [DOI] [PubMed] [Google Scholar]
- 16. Lee JM, Bae W, Lee YJ, Cho YJ (2014) The efficacy and safety of prone positional ventilation in acute respiratory distress syndrome: updated study-level meta-analysis of 11 randomized controlled trials. Crit Care Med 42: 1252–1262. [DOI] [PubMed] [Google Scholar]
- 17. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, et al. (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17: 1–12. [DOI] [PubMed] [Google Scholar]
- 18. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 19. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151: 264–269 [DOI] [PubMed] [Google Scholar]
- 21. Xinwei J, Xianghua F, Jing Z, Xinshun G, Ling X, et al. (2009) Comparison of usefulness of simvastatin 20 mg versus 80 mg in preventing contrast-induced nephropathy in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Am J Cardiol 104: 519–524. [DOI] [PubMed] [Google Scholar]
- 22. Zhou X, Jin YZ, Wang Q, Min R, Zhang XY (2009) [Efficacy of high dose atorvastatin on preventing contrast induced nephropathy in patients underwent coronary angiography]. Zhonghua Xin Xue Guan Bing Za Zhi 37: 394–396. [PubMed] [Google Scholar]
- 23. Acikel S, Muderrisoglu H, Yildirir A, Aydinalp A, Sade E, et al. (2010) Prevention of contrast-induced impairment of renal function by short-term or long-term statin therapy in patients undergoing elective coronary angiography. Blood Coagul Fibrinolysis 21: 750–757. [DOI] [PubMed] [Google Scholar]
- 24. Ozhan H, Erden I, Ordu S, Aydin M, Caglar O, et al. (2010) Efficacy of short-term high-dose atorvastatin for prevention of contrast-induced nephropathy in patients undergoing coronary angiography. Angiology 61: 711–714. [DOI] [PubMed] [Google Scholar]
- 25. X-p H, R-x W, Y Y, Zheng C, Bin C (2010) Prevention of contrast-induced nephropathy using high-dose atorvastatin in patients with coronary heart disease undergoing elective percutaneous coronary intervention] [in Chinese. Milit Med J South China 24: 448–451. [Google Scholar]
- 26. Patti G, Ricottini E, Nusca A, Colonna G, Pasceri V, et al. (2011) Short-term, high-dose Atorvastatin pretreatment to prevent contrast-induced nephropathy in patients with acute coronary syndromes undergoing percutaneous coronary intervention (from the ARMYDA-CIN [atorvastatin for reduction of myocardial damage during angioplasty—contrast-induced nephropathy] trial. Am J Cardiol 108: 1–7. [DOI] [PubMed] [Google Scholar]
- 27. Cao S, Wang P, Cui K, Zhang L, Hou Y (2012) [Atorvastatin prevents contrast agent-induced renal injury in patients undergoing coronary angiography by inhibiting oxidative stress]. Nan Fang Yi Ke Da Xue Xue Bao 32: 1600–1602. [PubMed] [Google Scholar]
- 28. Li W, Fu X, Wang Y, Li X, Yang Z, et al. (2012) Beneficial effects of high-dose atorvastatin pretreatment on renal function in patients with acute ST-segment elevation myocardial infarction undergoing emergency percutaneous coronary intervention. Cardiology 122: 195–202. [DOI] [PubMed] [Google Scholar]
- 29. Takagi H, Umemoto T (2011) A meta-analysis of randomized trials for effects of periprocedural atorvastatin on contrast-induced nephropathy. Int J Cardiol 153: 323–325. [DOI] [PubMed] [Google Scholar]
- 30. Zhang BC, Li WM, Xu YW (2011) High-dose statin pretreatment for the prevention of contrast-induced nephropathy: a meta-analysis. Can J Cardiol 27: 851–858. [DOI] [PubMed] [Google Scholar]
- 31. Zhang L, Zhang L, Lu Y, Wu B, Zhang S, et al. (2011) Efficacy of statin pretreatment for the prevention of contrast-induced nephropathy: a meta-analysis of randomised controlled trials. Int J Clin Pract 65: 624–630. [DOI] [PubMed] [Google Scholar]
- 32. Zhang T, Shen LH, Hu LH, He B (2011) Statins for the prevention of contrast-induced nephropathy: a systematic review and meta-analysis. Am J Nephrol 33: 344–351. [DOI] [PubMed] [Google Scholar]
- 33. Li Y, Liu Y, Fu L, Mei C, Dai B (2012) Efficacy of short-term high-dose statin in preventing contrast-induced nephropathy: a meta-analysis of seven randomized controlled trials. PLoS One 7: e34450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. John S, Schneider MP, Delles C, Jacobi J, Schmieder RE (2005) Lipid-independent effects of statins on endothelial function and bioavailability of nitric oxide in hypercholesterolemic patients. Am Heart J 149: 473. [DOI] [PubMed] [Google Scholar]
- 35. Ridker PM, Rifai N, Clearfield M, Downs JR, Weis SE, et al. (2001) Measurement of C-reactive protein for the targeting of statin therapy in the primary prevention of acute coronary events. N Engl J Med 344: 1959–1965. [DOI] [PubMed] [Google Scholar]
- 36. Ichiki T, Takeda K, Tokunou T, Iino N, Egashira K, et al. (2001) Downregulation of angiotensin II type 1 receptor by hydrophobic 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors in vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 21: 1896–1901. [DOI] [PubMed] [Google Scholar]
- 37. Bonetti PO, Lerman LO, Napoli C, Lerman A (2003) Statin effects beyond lipid lowering—are they clinically relevant? Eur Heart J 24: 225–248. [DOI] [PubMed] [Google Scholar]
- 38. Kashani A, Phillips CO, Foody JM, Wang Y, Mangalmurti S, et al. (2006) Risks associated with statin therapy: a systematic overview of randomized clinical trials. Circulation 114: 2788–2797. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(DOCX)
Supporting information files. Method S1, Search Strategy on Medline, EMBASE and Cochran Central. Method S2, Characteristics of the Excluded Study. Table S1, The Cochrane Collaboration's tool for assessing risk of bias. Figure S1, Risk of bias assessment graph. Risk of bias of each included trial was assessed with the Cochrane Collaboration's tool. This ‘risk of bias graph’ illustrates the proportion of studies with each of the judgments for each entry in the tool. Green represents ‘Yes (low risk of bias)’; yellow, ‘Unclear’; red, ‘No (high risk of bias)’. Figure S2, Risk of bias assessment summary. Risk of bias of each included trial was assessed with the Cochrane Collaboration's tool. This ‘risk of bias summary’ figure presents all of the judgments in a cross-tabulation of study by entry. Green represents ‘Yes (low risk of bias)’; yellow, ‘Unclear’; red, ‘No (high risk of bias)’. Figure S3, The effect of High-dose statin on the incidence of contrast-induced nephropathy by fixed effects model. Forest plot with relative risks for the incidence of contrast-induced nephropathy associated with high-dose statin versus low-dose statin or placebo for individual trials and the pooled population. The squares and the horizontal lines indicate the relative risks (by fixed effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the frequentist meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; RR, relative risks. Figure S4, The effect of High-dose statin on mean change of post-procedural serum creatinine. Forest plot with standardized mean difference (SMD) for the mean change of post-procedural serum creatinine from the baseline value associated with high-dose statin versus low-dose statin or placebo for individual trials and the pooled population. The squares and the horizontal lines indicate the SMD (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the frequentist meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; SD, standard deviation; SMD, standardized mean difference. Figure S5, Funnel plot for evaluation of publication and small study bias. Figure S6, Influence of individual studies Abbreviations: CI, confidence intervals; RR, relative risks. Figure S7, Cumulative Meta-analysis of high-dose statin on the incidence of contrast-induced nephropathy. The first row shows the effect of one study, the second row shows the cumulative pooled estimates based on the two studies, and so on. The squares and the horizontal lines indicate the cumulative relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included. Abbreviations: CI, confidence intervals; RR, relative risks. Figure S8, The effect of High-dose statin on the incidence of contrast-induced nephropathy, stratified according to the type of contrast. The squares and the horizontal lines indicate the relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; RR, relative risks. Figure S9, The effect of High-dose statin on the incidence of contrast-induced nephropathy, stratified according to the mean age of the patients. The squares and the horizontal lines indicate the relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; RR, relative risks. Figure S10, The effect of High-dose statin on the incidence of contrast-induced nephropathy, stratified according to the underlying chronic kidney disease. The squares and the horizontal lines indicate the relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rates; RR, relative risks. Figure S11, The effect of High-dose statin on the incidence of contrast-induced nephropathy, stratified according to the acute coronary syndrome. The squares and the horizontal lines indicate the relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; RR, relative risks. Figure S12, The effect of High-dose statin on the incidence of contrast-induced nephropathy, stratified according to the concomitant treatment of N-acetylcystein. The squares and the horizontal lines indicate the relative risks (by random effects model) and the 95% confidence intervals (CI) for each trial included; the size of each square is proportional to the statistical weight of a trial in the meta-analysis; diamond indicates the effect estimate derived from meta-analysis, with the center indicating the point estimate and the left and the right ends the 95% CI. Abbreviations: CI, confidence intervals; RR, relative risks.
(PDF)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.