Abstract
Learning Objectives
After participating in this activity, learners should be better able to:
1. Assess anomalous self-experience as a core feature of schizophrenia spectrum disorders.
2. Evaluate current and historical research regarding disorders of self-experience in schizophrenia.
Abstract
This article explores the phenomenological and empirical rediscovery of anomalous self-experience as a core feature of the schizophrenia spectrum disorders and presents the current status of research in this field. Historically, a disordered self was considered to be a constitutive phenotype of schizophrenia. Although the notion of a disordered self has continued to appear occasionally over the years—mainly in the phenomenologically or psychodynamically oriented literature—this notion was usually considered as a theoretical construct rather than as referring to concretely lived anomalous experiences. Empirical research on the disorders of self-experience in schizophrenia can be traced back to the US-Denmark psychopathological collaboration in the well-known adoption and high-risk studies, which aimed at identifying trait or phenotypic vulnerability features. This research was later followed by clinical work with first-admission schizophrenia patients. We offer clinical descriptions of anomalous self-experience and outline the phenomenological structures of subjectivity that are needed for grasping the nature of these anomalous experiential phenomena. What appears to underlie these experiences is an instability of the first-person perspective that threatens the basic experience of being a self-coinciding, embodied, demarcated, and persisting subject of awareness. We summarize a series of empirical studies targeting self-experience in schizophrenia performed prior to and after the construction of a phenomenologically oriented psychometric instrument for assessing anomalies of self-experience, the Examination of Anomalous Self-Experience (EASE). These empirical studies support the classic clinical intuition that anomalous self-experiences form a central phenotype of schizophrenia. Implications for diagnosis and research are briefly discussed.
Keywords: empirical studies, Examination of Anomalous Self-Experience (EASE), phenomenology, schizophrenia, self-disorders
The purpose of this article is to review recent phenomenologically oriented research that focuses on certain characteristic anomalies of self-experience (i.e., self-disorders) in schizophrenia spectrum disorders. This research has implications for the nosology of schizophrenia and for efforts to identify etiologically relevant phenotypes, and it has potentially important clinical consequences regarding early diagnosis, differential diagnosis, and therapeutic approaches to the disease.
In addition to reviewing the empirical literature, we emphasize the clinical and scientific roots of these particular research efforts and also their evolution and conceptual continuity with both classic and more recent, phenomenologically oriented empirical studies of schizophrenia. This research is also a product of interdisciplinary collaboration between psychopathology, philosophy of mind, and phenomenology. The interdisciplinary and mixed clinical and scientific background means that the research also is relevant to the current debate on the status of psychiatry as a science and a profession.1 This heated debate, triggered most recently by the release of the Diagnostic and Statistical Manual of Mental Disorders [DSM]-5 and the preparations for the International Classification of Diseases [ICD]-11, has been fueled by a widespread disappointment with psychiatry’s lack of etiological and therapeutic progress2—a lack partly attributed to the DSM’s rigid “diagnostic silos.”3,4
HISTORICAL BACKGROUND
The earliest—and quite sophisticated—psychopathological descriptions of anomalous self-experience appeared in French psychiatry at the turn of the twentieth century,5,6 but they were never associated with dementia praecox or schizophrenia because these latter concepts emerged only later in the French classification of mental disorders. By contrast, explicit references to a disordered self, considered as the fundamental phenotype of schizophrenia, are present in nearly all foundational texts on the disease, though using various terms and with varying clarity. For example, Kraepelin considered “disunity of consciousness” to be the core feature of schizophrenia.7 To grasp the link between selfhood and “unity of consciousness,” consider the following example. My current field of consciousness, as I am typing this essay, comprises heterogeneous dimensions, including thinking, perception, movement, and visual, tactile, and proprioceptive stimuli. Their coherence, or “unity,” is established by the fact that they are all my experiences; that is, they all appear in a single field of awareness, that of a single subject—namely, me.8
Eugen Bleuler listed the experiential “ego disorders” among the “complex fundamental” (diagnostic, or almost pathognomonic) schizophrenic symptoms.9 Karl Jaspers observed that for the patient with schizophrenia, the sense of self-presence was fundamentally weakened: “Descartes’ ‘cogito ergo sum’ (I think therefore I am) may still be superficially cogitated but it is no longer a valid experience” (emphasis added).10(p122) Kurt Schneider considered a “radical qualitative change” of the field of consciousness to be a generative matrix of the first-rank symptoms: “[Certain] disturbances of self-experience show the greatest degree of schizophrenic specificity. Here we refer to those disturbances of first personal givenness (Ich-heit) or ‘mineness’ (Meinhaftigkeit).”11(p58)
The interest in disorders of the self in schizophrenia persisted in phenomenological psychiatry (e.g., Minkowski,12 Ey,13 Laing,14 Kimura,15,16 Sass17) and in psychodynamically oriented theoretical contributions and case studies. The ICD-8 and -9 diagnostic prototypes, valid until 1992, described schizophrenia as a “fundamental disturbance of the personality, which involves its most basic functions, those that give the normal person his feeling of individuality, uniqueness, and self-direction” (emphasis added).18,19(p27) Note that the ICD-8/9 term “personality,” borrowed from the writings of Karl Jaspers and Kurt Schneider, actually originated in nineteenth-century psychiatry and psychology, where it signified what we today tend to call the “self” or “subjectivity,” and not the contemporary concept of personality, which refers to temperamental and habitual characterological dispositions.
Despite continuing interest in the self and its experiential distortions in schizophrenia, research that was systematic and empirical remained largely absent through the end of the twentieth century. The only notable exception is the recent work (1995) by the Swiss psychiatrist Christian Scharfetter,20 who developed self-rating scales for measuring the psychotic alteration of the sense of self—using dimensions of selfhood originally proposed by Jaspers—over the symptomatic course of the schizophrenic psychosis.
The publication of DSM-III in 1980,21 which completed the so-called operational revolution in psychiatry, involved a behavioristic, subjectivity-aversive stance that emphasized “observable features, demanding only a minimum of inference,” and that radically privileged reliability over validity.22 The issue of subjectivity or self vanished from the canonical discourse on the nature of schizophrenia and from the research agendas. That is not to say, of course, that the notion of self completely disappeared from the literature on schizophrenia. It continued to appear occasionally, though not as an anomalous experience accessible to description or study, but as a theoretical construct, a metaphor, or a meta-cognitive locus in cognitive science. Consequently, we stress that the research discussed in this article relates not to an abstract or inferred construct of the self but to an experientially disordered self—that is, a concretely lived, experiential phenomenon (phenotype) that is accessible to empirical and phenomenological observation and analysis.
CLINICAL AND RESEARCH BACKGROUND
The contemporary Copenhagen research on self-disorders in schizophrenia has its roots in the collaborative US-Denmark studies on adoption,23,24 high-risk populations,25 and linkage.26 These research projects focused on detecting characteristic, phenotypic traits that represent the psychopathological features of schizophrenia spectrum disorders. The diagnostic portion of these studies employed various standard semi-structured interviews, and the psychiatrists performing these interviews were all senior, consultant-level clinicians who were trained in the tenets of psychiatric phenomenology and in phenomenological interview methods.10,27 The adoption studies demonstrated the role of genes in the etiology of schizophrenia and led to the emergence of the “spectrum” concept, reviving the old concept of “schizoidia”28 and thereby providing the empirical foundation for the diagnostic category of schizotypal disorders, which was introduced in DSM-III. The US-Denmark high-risk prospective longitudinal study25 (involving 207 offspring of schizophrenic mothers) identified the following adolescent (age 15) premorbid predictors adult diagnostic outcome on the schizophrenia spectrum (i.e., schizophrenia; other nonorganic, nonaffective psychosis; and schizotypal disorders): deficient interpersonal emotional rapport, eccentric appearance or behavior, subtle formal thought disorder, social isolation, and interpersonal difficulties.29–32 These results seemed to fit into Bleuler’s and Meehl’s intuition that the (autistic) “fundamental traits” in schizophrenia are manifest in the expressive, interpersonal, and communicative-symbolic space.9,33 These traits were considered as the phenotypic core of vulnerability to schizophrenia in the diathesis-stress models of the illness—a model articulated in 1927 by Éugene Minkowski, a French psychiatrist and a pupil of Eugen Bleuler:
The notion of schizophrenia as a mental disease can be decomposed into two factors of different order. First, the schizoidia [the clinical core], which is a constitutional, highly specific, and temporally enduring factor, and, second, a nonspecific noxious factor of [environmental] evolutive nature. This noxious factor, acting upon the [vulnerability of] schizoidia, transforms the latter into schizophrenia.*,12(pp50–51)
Independently, writing in 1962, Paul Meehl33 presented a new version of this diathesis-stress model, in which schizophrenia was considered a severely decompensated schizotypal disorder influenced by environmental stressors and polygenetic factors. In his account the core schizotypal features (i.e., ambivalence, social aversiveness, cognitive slippage [formal thought disorder], and anhedonia) were considered to be proximally tied to the neural substrate of the illness. Likewise, the Copenhagen High-Risk Project indicated affinities between these core features and the notion of “schizophrenic autism,” a concept from Bleuler9 but subsequently rearticulated by phenomenological psychiatry in a clinically more useful and adequate way.34 On that view the core of schizophrenic autism is not a defensive withdrawal to inner fantasy life (as Bleuler seemed to suggest)9(p63) but a lack of a basic, automatic, and nonreflective attunement in the individual’s self-, other-, and world-relation.34–36 In addition to manifesting itself as a series of “external” or behavioral signs, this lack of attunement invariably entails a profound change of subjective experience.12,34,35,37–39 Blankenburg’s famous patient, Anne, presents the following frequently quoted complaint that dramatically illustrates this personal milieu (which Blankenburg interprets as a “crisis of common sense” or “lack of natural self-evidence”):
What is it that I am missing? It is something so small, but strange, it is something so important. It is impossible to live without it. I find that I no longer have footing in the world. I have lost a hold in regard to the simplest, everyday things. It seems that I lack a natural understanding for what is matter of course and obvious to others ... Every person knows how to behave, to take a direction, or to think something specific ... [A]ll these involve rules that the person follows. I am not able to recognize what these rules are. I am missing the basics ... I don’t know what to call this ... It is not knowledge ... Every child knows these things!38(pp307–08)
PRELIMINARIES: CLINICAL MANIFESTATIONS
When reading Blankenburg’s vignette, a natural question comes to mind: how is it like to be the subject lacking this basic foothold in the world? This question inspired two explorative, phenomenologically oriented studies of first-admission schizophrenia spectrum patients in Denmark40 and Norway.41 These (and later) studies demonstrated that the majority of young, first-admitted schizophrenia spectrum patients complained of not feeling truly alive, not fully existing, lacking their innermost identity, and being fundamentally, though ineffably, different from others (a feeling often expressed through childhood fantasies of being time travelers or extraterrestrials, or of having biological parents other than the ones they were being raised by. What distinguishes this basic feeling of being different or “wrong” in the schizophrenia spectrum disorders from the apparently similar feelings in other conditions is that this sense of being different cannot be articulated in terms of concrete, mundane characteristics such as feeling stupid, being too fat or not well dressed, having unusual interests, or coming from another socioeconomic background than one’s peers. Instead, what the patient struggles to describe is a basic sense of being ontologically different (different in kind) or of living in another ontological dimension; as an illustration, one of our patients said, “I do not feel like a spiritual being. It is as if I am a physical object; for example, like this radiator.” Put in another way, this sense of being different puts one’s own humanity in question; another patient of ours reported that while growing up, she often wondered if she was actually a robot.
Another aspect of this disordered self is a typically deficient sense of “mineness” of the field of awareness, as in “my thoughts are strange and have no respect for me.” This phenomenon is often closely related to various distortions of the first-person perspective; for example, “my point of view seems to tremble slightly, moves backwards ...”). Patients also frequently describe a hyper-reflective attitude to their own experiences: thoughts, feelings, or sense impressions are regarded or inspected from afar as objects of awareness rather than simply “lived through.” One patient distinguished between “being thoughts,” when these thoughts were permeated by her sense of self, and “having thoughts,” when thoughts were experienced as introspectible, thing-like objects. There may also be different forms of disembodiment (e.g., “there is a split between my mind and my body” or “it feels as if my body does not really fit”) and quasi-solipsistic experiences, usually with a fleeting sense of being at the center of the world or that one’s experiential field is the only extant reality.
The disorders at the subject- or self-pole of experience are typically also associated with deformations at the “world pole,” as vividly described by Blankenburg’s patient Anne: the lack of immersion in the surrounding world; the questioning of what others consider obvious or self-evident (often reflected in questions such as “why is the grass green?” or “why do people say ‘hello’ to each other?”); varieties of derealization; and alienation from the social world. In phenomenological terms, the basic or foundational pre-reflective articulation of the subject-object intentional relation has gone astray.42 Self-disorders, as described above, are sometimes enacted through altered or strange existential patterns, including solipsistic grandiosity, bizarre attitudes and actions, “double bookkeeping” (i.e., the capacity to inhabit both the psychotic and real worlds at once), mannerist behaviors, or a search for a new existential or metaphysical meaning (e.g., adherence to sectarian political or religious groups).43–45
A few additional clinical observations merit attention here.
First, anomalous self-experiences (self-disorders) have mainly a persisting, trait-like character. The notion of trait phenotype is usually applied to persistent expressive or behavioral features (e.g., persistent subtle formal thought disorder or inadequate affective modulation). In the case of experiential (subjective) phenomena such as self-disorders, the trait-like character of the anomalous self-experiences lies in their tendency to articulate themselves as a constant or recurring infrastructure of the patient’s conscious life—an infrastructure that determines more the form of experience (the how of experience) than the particular contents of experience (the what of experience). For example, what is distinctive about thought pressure is not that the patient has particular thoughts at a given moment but that the patient frequently experiences, say, several thematically unrelated trains of thought occurring chaotically at the same time and without his or her control. In sum, self-disorders are to a large extent structural aspects of subjective life that are, based on what the patients describe, never far away (as a potentiality) from their ongoing stream of experience. Very often, patients report that self-disorders date back to childhood or early adolescence. By the same token, at the time of patients’ first admission, many self-disorders have become almost indistinctly interwoven into patients’ mode of experiencing. At least partly for this reason, patients seldom seem to experience their initial self-disorders as “symptoms” of an illness (parallel to severe abdominal pain as a potential symptom of pancreatitis) but rather as intrinsic features of their existence and how they experience themselves, others, and the world—which might present a new framework for understanding poor insight into illness in schizophrenia.45 Moreover, self-disorders not only precede the onset of psychosis but also seem to persist after remission of a frank psychotic episode.
Second, we are not dealing here with psychotic phenomena. Self-disorders, no matter how strangely they are experienced, do not simply become elaborated at a psychotic level, although the articulation of psychosis in schizophrenia is related to the initial self-disorders.45 Self-disorders are typically verbally reported with the “as if” qualification (e.g., “it feels as if I am without a soul” or “I feel as if the thoughts aren’t really coming from me”). That is, the reflective reality judgment is still intact.
Third, many patients whom we have interviewed over the years seem to consider self-disorders as the very core of their illness and as contributing more to their suffering than the symptoms of psychosis.41 Frequently, patients are surprised to learn that the psychiatrist is familiar with their experiences, and they may become profoundly relieved after realizing that others also have similar experiences. Patients with an antecedent psychiatric history often express surprise that nobody ever asked them the necessary questions about their subjective life and way of experiencing. In this context it is worth noting that the alleviation of the feeling of existential solitude—albeit only partial or temporary—that comes to patients when they address their self-disorders may itself be of therapeutic value.
Finally, we emphasize that this kind of information about patients’ experience of their self-disorders cannot be obtained by a series of structured questions on a checklist. Rather, it requires a phenomenologically adequate interviewing approach that seeks to establish rapport and trust, and in which the active inquiry into the concrete phenomena, including examples and self-descriptions, is adequately and smoothly integrated into the patient’s own narrative.46 It is clinically important to recognize that the patient’s initial complaints are often in the nature of vague or nonspecific clichés that may be a shorthand for more specific complaints. Blankenburg termed this phenomenon the “non-specific specificity.”37,47 Often, only when the patient is asked for a concretely lived example of his (nonspecific) complaint does a more characteristic (and specific) configuration of anomalous experience emerge. For example, a patient complaining of “fatigue” may, upon prompting, report the constant, oppressive burden of a reflective, energy-consuming effort to decode and understand the meanings of ordinary, everyday conversations (in this case “fatigue” covers anomalous self-experiences, including loss of common sense, perplexity, and hyper-reflection). Another patient, complaining about “concentration difficulties,” may, upon request, describe these difficulties as rooted in several thematically unrelated and chaotic trains of thought that occur at the same time and that he can neither stop nor control, thus making it almost impossible to concentrate on something else. The psychiatrist’s acquaintance with the phenomenon of “non-specific specificity”37,47 is, in our view, extremely important in the context of early diagnostic assessment, especially of patients presenting with a vague, unelaborated picture of maladjustment, underperformance, chronic malaise and dysphoria, negative symptoms, or hypochondriac preoccupations.
PHENOMENOLOGY OF DISORDERED SELF
The empirical studies on self-disorders, which we review in detail below, jointly point toward an instability of the very basic sense of self in schizophrenia spectrum disorders (i.e., schizophrenia and schizotypal disorders). This instability does not, however, equal a lack or dissolution of the self (which perhaps may only occur in severe cases of catatonia). Thus, a patient suffering from a disordered sense of self continues to be a subject of awareness and to affirm himself or herself with the first personal pronoun “I.” In other words, patients experience self-disorders within an overarching experiential-existential perspective that constitutes their being-in-the-world; no matter how vulnerable the patients may be or how many self-disorders they are exposed to, their lives remain full and complete forms of human existence. The terms “instability” or “dis-order” indicate, however, that the normally tacit, taken-for-granted, pre-reflective, and pre-conceptual sense of being a subject of awareness no longer saturates one’s experiences in the usual, unproblematic way. Rather, in schizophrenia spectrum disorders the basic sense of self appears to be fragile, threatened, and oscillating. But what does this basic sense of self more specifically amount to? To answer this question, psychiatry must go beyond its own confines and draw on resources particularly from philosophy of mind and phenomenology. Grasping consciousness is not like grasping a spatial object or thing.
The basic sense of self signifies that we each live our conscious life as a self-present, single, temporally persistent, bodily, and demarcated (bounded) subject of experience and action.10,48 To articulate the most basic or irreducible dimension of selfhood, phenomenology49 and the cognitive sciences50 operate with the notions of a “minimal” or “core” self; that is, a necessary structure that must be in place in order for any experience to be experienced as someone’s experience (in contrast to, say, the experience existing in a sort of free-floating state and only post hoc appropriated by the subject in an act of reflection). The basic (or minimal) sense of self is experientially, but pre-reflectively, manifest. It refers to the first-personal articulation of experiencing, typically called “mineness,” “myness,” “for-me-ness,” or “ipseity.”42,49,51 The term “ipseity” (in Latin, ipse = self) conveys that all experiences are tacitly or pre-reflectively lived as my experiences—that is, from my first-person perspective. Yet the notion of a mere or pure perspective does not exhaust the sense of ipseity. This notion also has a more substantial aspect in which the sense of “I-me-myself” persists over time and across different and changing modalities of conscious life. It is immediately, pre-reflectively, and non-inferentially given or present as a founding stratum of our experiential life. This sense of “I-me-myself” is property-less; that is, it cannot be further described with a series of adjectives or attributes. We may even say that “if intelligibility is grasping properties, then the ‘myself’ ... eludes our grasp.”52(p310) From a phenomenological perspective, ipseity or the self does not “show up” in our experiences as a sort of object or quasi-object toward which we may direct our attention. Thus, ipseity is not a product of reflection, introspection, or meta-representational mental activity but a passively emerging first-person configuration of experience. Ipseity has been compared to a flame that enlightens its surroundings and thereby itself.53(p173) In other words, ipseity cannot be defined or grasped independently from the stream of consciousness in which it manifests itself as a specific structural configuration of that stream.
Ipseity is a precondition of more rich and complex feelings of identity. It signifies that I am always already aware of myself and that I therefore have no need for introspection, self-observation, or self-reflection to assure myself of being myself or being the one who entertains these thoughts or undergoes these experiences. Ipseity conveys a foundational, immutable core that is necessary for our sense of existing as a self-present, bodily, demarcated, and persisting subject of awareness. Thus, ipseity exhibits a paradoxical nature; it may be considered as a general, universal form of consciousness, while also, notwithstanding its lack of properties, serving as the most intimate, individuated core of our personal identity.52 Ipseity thus needs to be distinguished from fuller, more complex notions of the self (e.g., the so-called narrative, extended, or personal self). And our central claim is that schizophrenia spectrum disorders involve a selective disturbance of ipseity,42,51 though it may also, in turn, influence those more complex levels of the self. By contrast, personality disorders outside the schizophrenia spectrum seem, in our view, to reflect disturbances at the more complex, self-representational or narrative levels of selfhood,54 leaving ipseity largely unaffected.
Today, various approaches—including the phenomenological, existential, psychoanalytical, and metacognitive—as well as autobiographical reports55–57 suggest that schizophrenia involves a diminished sense of self. The meaning of the term “self,” however, and how it may be “diminished” in schizophrenia seems to differ markedly from one author to the next. To elucidate the distinctness of our own hypothesis, we will briefly compare it to another theoretical proposal: the so-called dialogical model of the self (as developed by Paul and John Lysaker).58 On that model, a “sense of self involves a disclosure of the self-as-X,”58(p63) where the “X” refers to what is termed (1) a “character-position” (e.g., self-as-citizen), (2) an “organism-position” (e.g., self-as-hungry), or (3) a “meta-position” (e.g., self-as-fortunate).58(pp54,63) According to Lysaker and Lysaker, a sense of self emerges from a dynamic interplay (or “dialogue”) between these three self-positions. On this model, the diminished sense of self in schizophrenia results from a relative loss of an ordered, interanimating play among these three self-positions,58(p74) each of which has its own attributes. This approach contrasts sharply with the view we have presented here, according to which schizophrenia spectrum disorders involve a disturbance of ipseity—an instability of the normally tacit, pre-reflective, and pre-predicative founding stratum of our experiential life that is property-less and that resists further qualification. Our proposal and the proposal by Lysaker and Lysaker target different dimensions or levels of self-experience.
Finally, we note that our proposal is not necessarily at odds with brain- or metacognitive-based models of the self in schizophrenia. The difference is that the latter tend to posit disruptions of the self as resulting from failures of higher-order capacities, whereas we suggest that the sense of self in schizophrenia is often diminished at the level of immediate, first-order experience.
EARLY EMPIRICAL STUDIES
Data-collection instruments in the early (pre-2005) self-disorders research included the forerunners of the Bonn Scale for the Assessment of Basic Symptoms (BSABS)59 and the final, published version of the BSABS (translated into Danish),60 which had been expanded to include a few items that were explicitly designed to target anomalous self-experience. The BSABS is a comprehensive, semi-structured interview scheme that assesses various anomalies of experience (affective, volitional, cognitive, perceptual, and bodily), each illustrated by patient-derived prototypical statements. The empirical studies during this early period are presented in Table 1. The BSABS, used in many of those studies, has been found to have satisfactory reliability.63
Table 1.
Pre-EASE Studiesa
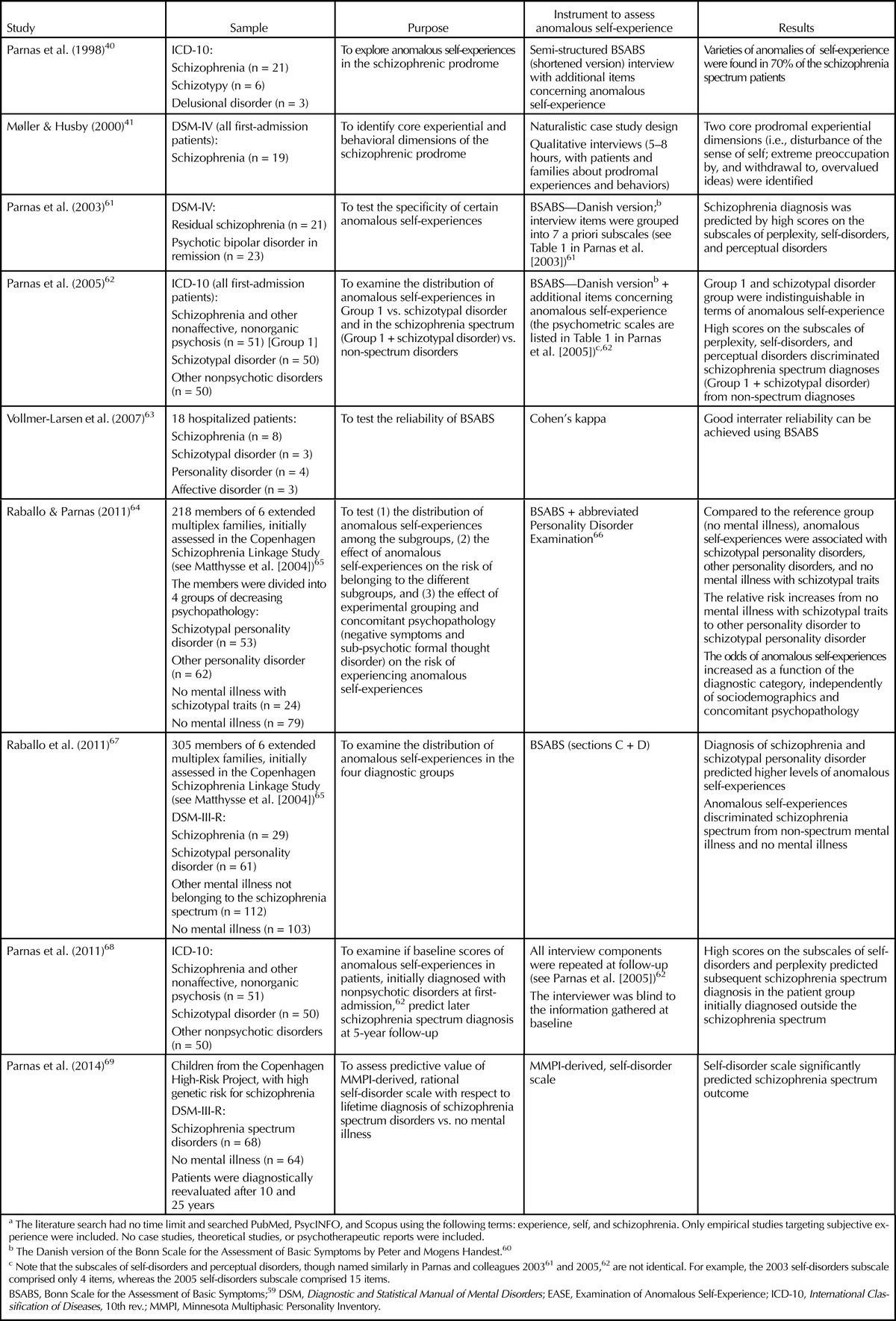
A central, joint finding of the empirical studies was that self-disorders aggregated selectively among the first-admission patients diagnosed with ICD-10 schizophrenia and schizotypal disorder as compared to patients with other psychiatric diagnoses.62 In a five-year follow-up of this particular clinical sample, high levels of self-disorders at baseline in patients with a first-admission diagnosis outside the schizophrenia spectrum predicted subsequent diagnostic transition into the schizophrenia spectrum; by contrast, the Positive and Negative Syndrome Scale scores on the canonical dimensions of schizophrenia symptomatology were unpredictive.68 In another study, which compared a group of patients with residual/remitted schizophrenia to a group of remitted psychotic bipolar patients, a significant aggregation of self-disorders was found in the former group.61 The selective aggregation of self-disorders within the schizophrenia spectrum was replicated in a large population sample comprising six extended families at high genetic risk for schizophrenia.65 The individuals with DSM-III-R schizophrenia or schizotypal disorder proved to have higher levels of self-disorders than the individuals with other psychiatric diagnoses or those with no clinical diagnosis.64 Most interestingly, when the healthy control group (note that all subjects were related to a schizophrenia proband) was later divided into those individuals exhibiting one or few schizotypal features (but without qualifying for any psychiatric diagnosis) and those completely free of schizotypal traits, it was found that the former group scored significantly higher on the self-disorders scale—a finding consistent with the view of self-disorders as an aspect of vulnerability.67
Finally, Parnas and colleagues69 applied the concept of self-disorders to the data from the Copenhagen High-Risk Project—in particular, by selecting the items from the premorbid Minnesota Multiphasic Personality Inventory assessment that, if voiced as a complaint in a clinical context, would trigger an in-depth assessment of a corresponding EASE-item (see next section). This MMPI-derived self-disorder scale (Cronbachs alpha > 0.9) successfully discriminated a lifetime diagnostic outcome of schizophrenia spectrum disorders (i.e., schizophrenia and schizotypal personality disorder) versus no mental illness among the genetically predisposed individuals.
EASE-BASED EMPIRICAL RESEARCH
In 2005, a semi-structured psychometric instrument for a qualitative and quantitative assessment of the anomalies of self-experience—the Examination of Anomalous Self-Experience (EASE)—was published.70 Senior psychiatrists from three European countries collaborated in constructing the EASE, which also included conceptual input from philosophy of mind and phenomenology. The selection of the scale items was based on the combined experience of clinical units for first-admitted patients, reflected detailed reviews of English, French, German, and Scandinavian psychopathological literature, and took into account the data collected in the available pre-EASE empirical studies (see Table 1). The construction process also included the authors’ joint discussions of videotaped psychopathological assessments, conducted individually by the EASE’s Danish authors, of 40 selected patients with potential self-disorders.
The EASE contains 57 main items, sometimes divided into subtypes. Each item is briefly defined and illustrated by prototypical examples of complaints. The items are aggregated into five rationally cohesive sections: (1) Cognition and Stream of Consciousness, (2) Self-Awareness and Presence, (3) Bodily Experiences, (4) Demarcation/Transitivism, (5) Existential Reorientation. The EASE exhibits high internal consistency,71,72 a monofactorial structure,72,73 and good to excellent interrater reliability among trained and experienced psychiatrists or clinical psychologists.70,71,74
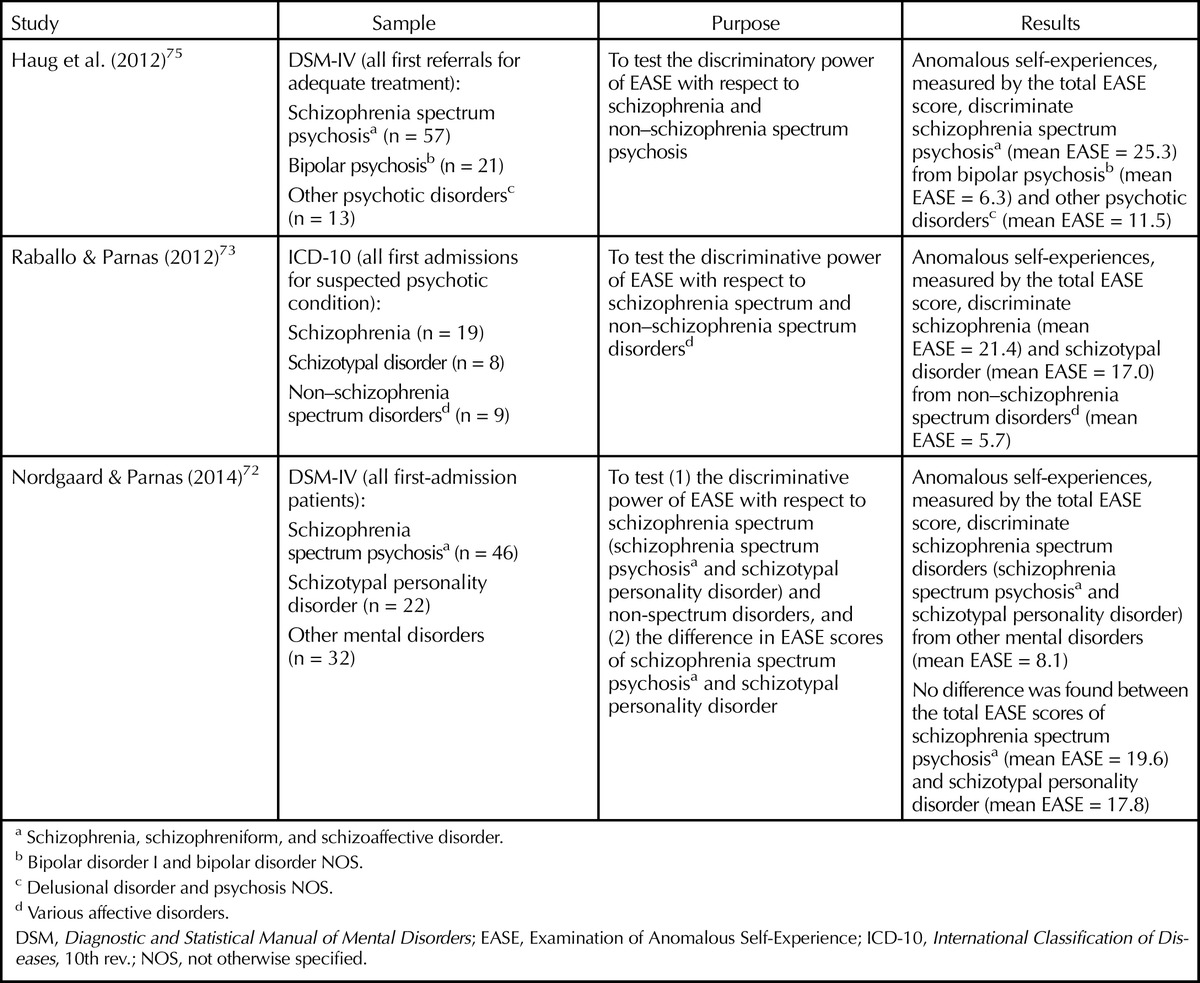
Several studies have now explored the association of EASE scores with psychiatric diagnoses (see Table 2). In samples comprising patients with ICD-10 or DSM-IV schizophrenia, schizotypal disorder, and other non-spectrum mental disorders, Raballo and Parnas73 and Nordgaard and Parnas72 successfully replicated the results from the pre-EASE empirical studies,62,64 thus finding a significant, selective aggregation of self-disorders among the schizophrenia spectrum patients. Additionally, the patients with schizophrenia and schizotypal disorders had similar levels of self-disorders. Haug and colleagues75 examined a sample of first-episode psychosis patients diagnosed with DSM-IV schizophrenia, bipolar psychosis, or other psychotic disorders. They found that high EASE scores markedly and significantly differentiated schizophrenia from the two other groups. This effect remained significant after controlling for severity differences in positive and negative symptoms.
Table 2.
EASE-Related Studies and Diagnosis of Schizophrenia Spectrum Disorders
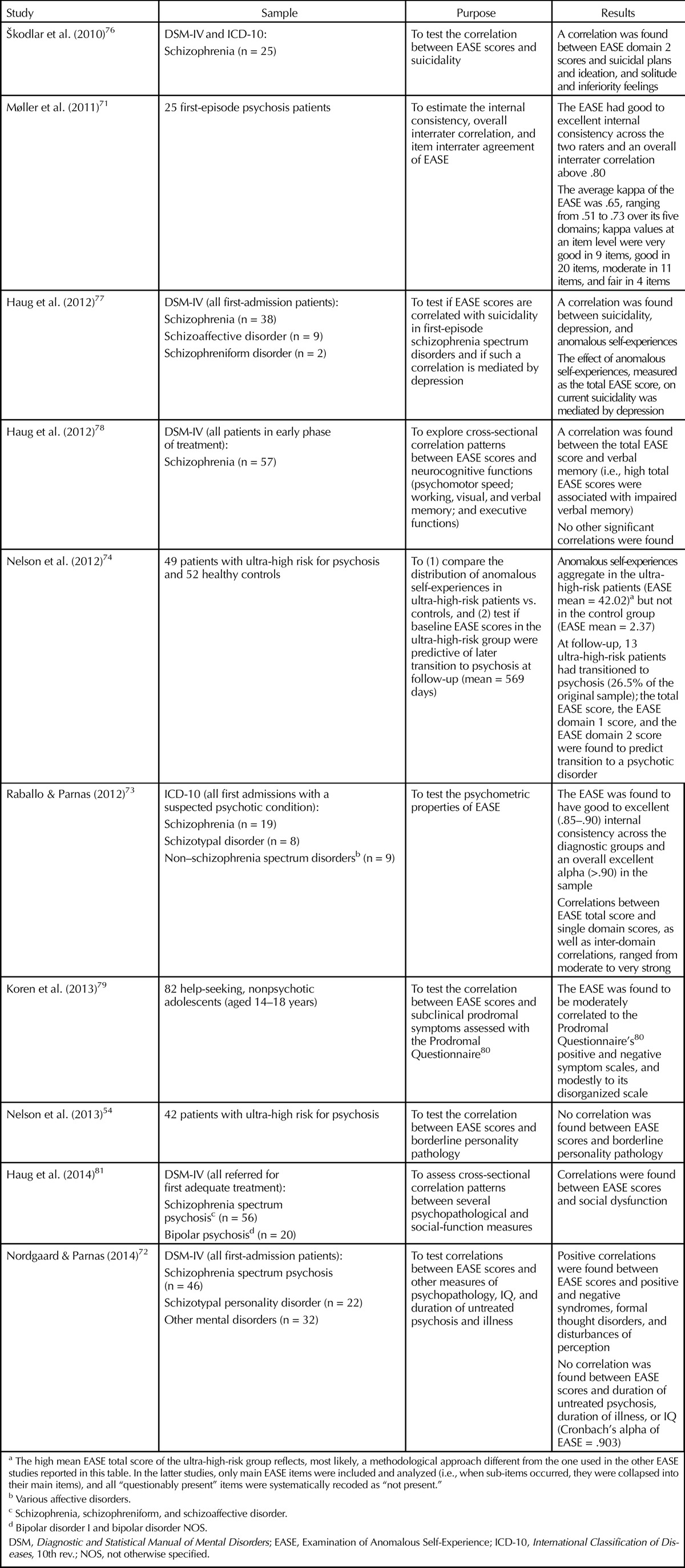
A range of empirical studies has explored correlations between EASE scores and other measures such as those for psychopathology (see Table 3). In samples of patients with schizophrenia, Škodlar and colleagues76 and Haug and colleagues77 found a correlation between self-disorders and measures of suicidality. In another study, Haug and colleagues78 found no correlation between self-disorders and neurocognitive measures except for impaired verbal memory, and Nordgaard and Parnas73 found no correlation between self-disorders and IQ. Haug and colleagues81 found that elevated levels of self-disorders were independently associated with poorer social functioning in schizophrenia and bipolar disorder; the study controlled for relevant factors such as premorbid adjustment, duration of untreated psychosis, negative symptoms, neurocognitive function, and diagnosis. Koren and colleagues79 identified self-disorders among nonpsychotic, help-seeking adolescents (aged 14–18 years) and found that self-disorders correlated with subclinical prodromal symptoms. The symptomatic distribution identified three separate groups of adolescents: one with prodromal symptoms only, one with prodromal symptoms and self-disorders, and one with self-disorders only. Nelson and colleagues74 demonstrated that elevated EASE scores at baseline predicted psychosis outcome in a sample of subjects at ultra-high risk for psychosis subjects. In a related study,54 they found no correlation between the borderline dimension of psychopathology and self-disorders, suggesting that the EASE-measured self-disorders are of a different kind than the self-related problems characteristic of borderline personality disorder and perhaps also other personality disorders outside the schizophrenia spectrum. Sass and colleagues82 conducted an interesting theoretical-comparative study of the similarities and differences between selected literature reports on depersonalization and the anomalous self-experiences identified through the EASE. They concluded that erosion of the first-person perspective appeared specific to schizophrenia.
Table 3.
Miscellaneous EASE Studies
CONCLUSIONS AND IMPLICATIONS
The presented research supports the notion of disturbances of specific structures of consciousness as important phenotypes of the schizophrenia spectrum disorders, thus corroborating the clinical intuitions of those who first identified them. A self-evident conclusion is that much empirical and conceptual work lies ahead of us. Most importantly, the temporal stability of self-disorders and their trait-like status need systematic longitudinal investigations. In our view, the central issues concern the nosological status and the diagnostic boundaries of schizophrenia and schizotypal conditions, along with the consequences of understanding how important self-disorders are in understanding these phenomena. For many years, we have witnessed a rebirth of a unitary view of psychosis, collapsing schizophrenia and psychotic affective illness into one disorder. This assumption is typically legitimized by findings of certain genetic and neurocognitive commonalities, and it is supported by the graded distributions of positive and negative symptoms (assessed by standard checklists), with absent “points of rarity.” As we have recently argued at some length elsewhere,39,83,84 however, the original prototypical (founding) definition of schizophrenia was not based on a number of specific psychotic symptoms but rather relied on the identification of a characteristic trait or gestalt, predominantly marked by peculiarities or strangeness in the expressive, communicative, and symbolic spaces. Many metaphors were employed or even invented to describe this particular gestalt—for example, discordance, intra-psychic ataxia, autism, loss of vital contact with reality, and cognitive dysmetria. This gestalt is intrinsically elusive and resists any simple, straightforward attempt to define it.39
In characterizing a phenotypic gestalt for schizophrenia, we need not only to take into account its expressive, external features or signs, but to grasp a certain whole that is jointly constituted by its “outer” and the “inner” aspects. We must recognize that the patient’s structures of subjectivity are profoundly different, even though we may not be able to verbalize this difference in precise terms. In other words, we not only register the external signs but also sense an inner change (what might be called the symptoms). What we sometimes perceive as incomprehensible or strange in the interaction with such a patient is therefore not solely due to a disorder of expressivity, operating as a somewhat autonomous series of signs (e.g., inappropriate affect). Rather, the perceived strangeness is also reflective of, and codetermined by, the altered structures of subjectivity. It is in this particular context that a phenomenologically coherent notion of a disorder of the self, itemized into its multiple empirical aspects in the EASE scale, permits a more focused, targeted, and explicitly articulated (and therefore reliable) investigation and description of the psychopathological aspects of the schizophrenic gestalt. Until now, these dimensions of the gestalt have been dismissed as too “atmospheric,” “intuitive,” or “subjective” to be useful either scientifically or clinically. The notion of self-disorder, however, presents a more specific, articulated, and robust demarcation of the schizophrenia spectrum disorders. Not only is this demarcation based on central psychopathological considerations, but it can play a crucial role in etiological and pathogenetic research.85–87 The diagnostic notion of self-disorder also has important implications clinically—for example, in early detection and differential diagnosis.88,89 Finally, it seems to us that psychotherapeutic approaches that are intimately informed about the specific nature of the patient’s suffering are likely to have better therapeutic success.90
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Translation and bracketed insertions by authors.
Supported, in part, by the Carlsberg Foundation, grant no. 2012010195 (Dr. Henriksen).
CME Harvard Review of Psychiatry offers CME for readers who complete questions about featured articles. Questions can be accessed from the Harvard Review of Psychiatry website (www.harvardreviewofpsychiatry.org) by clicking the CME tab. Please read the featured article and then log into the website for this educational offering. If you are already online, click here to go directly to the CME page for further information.
REFERENCES
- 1.Katschnig H. Are psychiatrists an endangered species? Observations on internal and external challenges to the profession. World Psychiatry 2010; 9: 21– 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frances AJ, Widiger T. Psychiatric diagnosis: lessons from the DSM-IV past and cautions for the DSM-5 future. Annu Rev Clin Psychol 2012; 8: 109– 30. [DOI] [PubMed] [Google Scholar]
- 3.Hyman SE. The diagnosis of mental disorders: the problem of reification. Annu Rev Clin Psychol 2010; 6: 155– 79. [DOI] [PubMed] [Google Scholar]
- 4.Hyman SE. Diagnosing the DSM: diagnostic classification needs fundamental reform. Cerebrum 2011; 2011: 6. [PMC free article] [PubMed] [Google Scholar]
- 5.Janet P. Les obsessions et la psychasthénie. Paris: Alcan, 1903. [Google Scholar]
- 6.Hesnard A-LM. Les troubles de la personalité dans les états d’asthénie psychique. Étude de psychologie clinique. Thèse de médecine. Bordeaux: Université de Bordeaux, 1909. [Google Scholar]
- 7.Kraepelin E. Psychiatrie. Ein Lehrbuch für Studierende und Ärzte. Auflage 8, vollständig umgearbeitet. Leipzig: Johann Ambrosius Barth, 1913. [Google Scholar]
- 8.Bayne T. The unity of consciousness. Oxford: Oxford University Press, 2010. [Google Scholar]
- 9.Bleuler E, Zinkin J, trans. Dementia praecox or the group of schizophrenias. New York: International Universities, 1950. [1911]. [Google Scholar]
- 10.Jaspers K, Hoenig J, Hamilton MW, trans. General psychopathology. London: John Hopkins University Press, 1997. [1913]. [Google Scholar]
- 11.Schneider K, Hamilton MW, trans. Clinical psychopathology. New York: Grune & Stratton, 1959. [1950]. [Google Scholar]
- 12.Minkowski E. La schizophrénie. Psychopathologie des schizoïdes et des schizophrènes. Paris: Payot, 1927. [Google Scholar]
- 13.Ey H, Flodstrom JH, trans. Consciousness: a phenomenological study of being conscious and becoming conscious. Bloomington; London: Indiana University Press, 1978. [Google Scholar]
- 14.Laing RD. The divided self. London: Penguin, 2010. [1960]. [Google Scholar]
- 15.Kimura B. Réflexion et soi chez le schizophréne. Paris: Presses Universitaires de France, 1992. [Google Scholar]
- 16.Kimura B. Cogito and I: a bio-logical approach. Philos Psychiatr Psychol 2001; 8: 331– 6. [Google Scholar]
- 17.Sass LA. Madness and modernism: insanity in the light of modern art, literature, and thought. Cambridge, MA: Harvard University Press, 1992. [Google Scholar]
- 18.World Health Organization. International classification of diseases. 8th ed Geneva: WHO, 1965. [Google Scholar]
- 19.World Health Organization. International classification of diseases. 9th ed Geneva: WHO, 1975. [Google Scholar]
- 20.Scharfetter C. The ego/self experience of schizophrenic patients. Schweiz Arch Neurol Psychiatr 1995; 146: 200– 6. [PubMed] [Google Scholar]
- 21.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed Washington, DC: American Psychiatric Press, 1980. [Google Scholar]
- 22.Parnas J, Bovet P. Psychiatry made easy: operation(al)ism and some of its consequences. In: Kendler K Parnas J, eds. Philosophical issues in psychiatry III: the nature and sources of historical science. Oxford: Oxford University Press (forthcoming; 2014). [Google Scholar]
- 23.Kety SS, Rosenthal D, Wender PH, Schulsinger F. The types and prevalence of mental illness in the biological and adoptive families of adopted schizophrenics. In: Rosenthal D Kety SS, eds. The transmission of schizophrenia. Oxford: Pergamon, 1968: 345– 62. [Google Scholar]
- 24.Kety SS, Rosenthal D, Wender PH, Schulsinger F, Jacobsen B. Mental illness in the biological and adoptive families of adopted individuals who have become schizophrenic: a preliminary report based upon psychiatric interviews. In: Fieve R Rosenthal D Brill H, eds. Genetic research in psychiatry. Baltimore, London: Johns Hopkins University Press, 1975: 147– 65. [PubMed] [Google Scholar]
- 25.Mednick SA, Parnas J, Schulsinger F. The Copenhagen High-Risk Project, 1962–1986. Schizophr Bull 1987; 13: 485– 95. [DOI] [PubMed] [Google Scholar]
- 26.Matthysse S, Parnas J. Extending the phenotype of schizophrenia: implications for linkage analysis. J Psychiatr Res 1992; 26: 329– 44. [DOI] [PubMed] [Google Scholar]
- 27.Parnas J, Zahavi D. The role of phenomenology in psychiatric diagnosis and classification. In: Maj M Gaebel W López-Ibor JJ Sartorius N, eds. Psychiatric diagnosis and classification. New York: Wiley, 2002: 137– 62. [Google Scholar]
- 28.Parnas J, Bovet P, Licht D. Cluster A personality disorders: a review. In: Maj M Aksiskal H Mezzich JE Okasha A, eds. Personality disorders. WPA series: evidence and experience in psychiatry. Chichester, UK: Wiley, 2005: 1– 74. [Google Scholar]
- 29.Parnas J, Schulsinger F, Schulsinger H, Mednick SA, Teasdale TW. Behavioral precursors of schizophrenia spectrum: a prospective study. Arch Gen Psychiatry 1982; 396: 658– 64. [DOI] [PubMed] [Google Scholar]
- 30.Parnas J, Jørgensen Å. Premorbid psychopathology in schizophrenia spectrum. Br J Psychiatry 1989; 155: 623– 7. [DOI] [PubMed] [Google Scholar]
- 31.Parnas J, Cannon TD, Jacobsen B, Schulsinger H, Schulsinger F, Mednick SA. Lifetime DSM-III-R diagnostic outcomes in the offspring of schizophrenic mothers. Results from the Copenhagen High-Risk Study. Arch Gen Psychiatry 1993; 50: 707– 14. [DOI] [PubMed] [Google Scholar]
- 32.Tyrka AR, Cannon TD, Haslam N, et al. The latent structure of schizotypy: I. Premorbid indicators of a taxon of individuals at risk for schizophrenia-spectrum disorders. J Abnorm Psychol 1995; 104: 173– 83. [DOI] [PubMed] [Google Scholar]
- 33.Meehl P. Schizotaxia, schizotypy, schizophrenia. Am Psychol 1962; 17: 827– 38. [Google Scholar]
- 34.Parnas J, Bovet P, Zahavi D. Schizophrenic autism: clinical phenomenology and pathogenetic implications. World Psychiatry 2002; 1: 131– 6. [PMC free article] [PubMed] [Google Scholar]
- 35.Parnas J, Bovet P. Autism in schizophrenia revisited. Compr Psychiatry 1991; 3: 7– 21. [DOI] [PubMed] [Google Scholar]
- 36.Henriksen MG, Škodlar B, Sass LA, Parnas J. Autism and perplexity: a qualitative and theoretical study of basic subjective experiences in schizophrenia. Psychopathology 2010; 43: 357– 68. [DOI] [PubMed] [Google Scholar]
- 37.Blankenburg W. Der Verlust der natürlichen Selbstverständlichkeit. Ein Beitrag zur Psychopathologie symptomarmer Schizophrenien. Stuttgart: Enke, 1971. [Google Scholar]
- 38.Blankenburg W, Mishara A, trans. First steps toward a psychopathology of “common sense.” Philos Psychiatr Psychol 2001; 8: 303– 15. [Google Scholar]
- 39.Parnas J. A disappearing heritage: the clinical core of schizophrenia. Schizophr Bull 2011; 37: 1121– 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parnas J, Jansson L, Sass LA, Handest P. Self-experience in the prodromal phases of schizophrenia. Neurol Psychiatry Brain Res 1998; 6: 97– 106. [Google Scholar]
- 41.Møller P, Husby R. The initial prodrome in schizophrenia: searching for naturalistic core dimensions of experience and behavior. Schizophr Bull 2000; 26: 217– 32. [DOI] [PubMed] [Google Scholar]
- 42.Parnas J, Sass LA. The structure of self-consciousness in schizophrenia. In: Gallagher S, ed. The Oxford handbook of the self. Oxford: Oxford University Press, 2011: 521– 46. [Google Scholar]
- 43.Møller P. First-episode schizophrenia: do grandiosity, disorganization, and acute initial development reduce duration of untreated psychosis? An exploratory naturalistic case study. Compr Psychiatry 2000; 41: 184– 90. [DOI] [PubMed] [Google Scholar]
- 44.Henriksen MG, Parnas J. Clinical manifestations of self-disorders and the gestalt of schizophrenia. Schizophr Bull 2012; 38: 657– 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Henriksen MG, Parnas J. Self-disorders and schizophrenia: a phenomenological reappraisal of poor insight and noncompliance. Schizophr Bull 2014; 40: 542– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nordgaard J, Sass LA, Parnas J. The psychiatric interview: validity, structure, and subjectivity. Eur Arch Psychiatry Clin Neurosci 2013; 263: 353– 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blankenburg W. Der Versagenszustand bei latenten Schizophrenien. Deutsche Medizinische Wochenschrift 1968; 93: 67– 71. [DOI] [PubMed] [Google Scholar]
- 48.Albahari M. Analytical Buddhism: the two-tiered illusion of self. Basingstoke, UK: Palgrave Macmillan, 2006. [Google Scholar]
- 49.Zahavi D. Subjectivity and selfhood: investigating the first-person perspective. Cambridge, MA: MIT, 2005. [Google Scholar]
- 50.Damasio AR. Self comes to mind: constructing the conscious brain. New York: Pantheon, 2010. [Google Scholar]
- 51.Sass LA, Parnas J. Schizophrenia, consciousness, and the self. Schizophr Bull 2003; 29: 427– 44. [DOI] [PubMed] [Google Scholar]
- 52.Hart JG. Who one is. Book 1: Meontology of the ‘I’: a transcendental phenomenology. Berlin: Springer, 2009. [Google Scholar]
- 53.Henry M. L’essence de la manifestation. Paris: PUF, 1963. [Google Scholar]
- 54.Nelson B, Thompson A, Chanen AM, Amminger GP, Yung AR. Is basic self-disturbance in ultra-high risk for psychosis (‘prodromal’) patients associated with borderline personality pathology? Early Interv Psychiatry 2013; 7: 306– 10. [DOI] [PubMed] [Google Scholar]
- 55.Moe AM, Docherty NM. Schizophrenia and the sense of self. Schizophr Bull 2014; 40: 161– 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lysaker PH, Lysaker PT. Schizophrenia and alterations in self-experience: a comparison of 6 perspectives. Schizophr Bull 2010; 36: 331– 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lysaker PH, Carcione A, Dimaggio G, et al. Metacognition amidst narratives of self and illness in schizophrenia: associations with neurocognition, symptoms, insight and quality of life. Acta Psychiatr Scand 2005; 12: 64– 71. [DOI] [PubMed] [Google Scholar]
- 58.Lysaker PH, Lysaker PT. Schizophrenia and the fate of the self. Oxford: Oxford University Press, 2008. [Google Scholar]
- 59.Gross G, Huber G, Klosterkotter J, et al. Bonner Skala für die Beurteilung von Basissymptomen. Berlin: Springer, 1987. [Google Scholar]
- 60.Parnas J Handest P, eds; Handest P Handest M, trans. Bonn Scale for the Assessment of Basic Symptoms. Copenhagen: Synthélabo Scandinavia A/S, 1995. [trans. of: Gross G, Huber G, Klosterkötter J, Linz M. Bonner Skala für die Beurteilung von Basisymptomen (in Danish)]. [Google Scholar]
- 61.Parnas J, Handest P, Saebye D, Jansson L. Anomalies of subjective experience in schizophrenia and psychotic bipolar illness. Acta Psychiatr Scand 2003; 108: 126– 33. [DOI] [PubMed] [Google Scholar]
- 62.Parnas J, Handest P, Jansson L, Saebye D. Anomalous subjective experience among first-admitted schizophrenia spectrum patients: empirical investigation. Psychopathology 2005; 38: 259– 67. [DOI] [PubMed] [Google Scholar]
- 63.Vollmer-Larsen A, Handest P, Parnas J. Reliability of measuring anomalous experience: the Bonn scale for the assessment of basic symptoms. Psychopathology 2007; 40: 345– 8. [DOI] [PubMed] [Google Scholar]
- 64.Raballo A, Parnas J. The silent side of the spectrum: schizotypy and the schizotaxic self. Schizophr Bull 2011; 37: 1017– 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Matthysse S, Holzman PS, Gusella JF, et al. Linkage of eye movement dysfunction to chromosome 6p in schizophrenia: additional evidence. Am J Med Genet B Neuropsychiatr Genet 2004; 128B: 30– 6. [DOI] [PubMed] [Google Scholar]
- 66.Loranger AW. Personality Disorder Examination (PDE) Manual. Yonkers, NY: DV Communications, 1988. [Google Scholar]
- 67.Raballo A, Sæbye D, Parnas J. Looking at the schizophrenia spectrum through the prism of self-disorders: an empirical study. Schizophr Bull 2011; 37: 344– 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Parnas J, Raballo A, Handest P, Jansson L, Vollmer-Larsen A, Saebye D. Self-experience in the early phases of schizophrenia: 5-year follow-up of the Copenhagen Prodromal Study. World Psychiatry 2011; 10: 200– 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Parnas J, Carter J, Nordgaard J. Premorbid self-disorders and lifetime diagnosis in the schizophrenia spectrum: a prospective high-risk study. Early Interv Psychiatry 2014. Apr 11 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 70.Parnas J, Møller P, Kircher T, et al. EASE: Examination of Anomalous Self-Experience. Psychopathology 2005; 38: 236– 58. [DOI] [PubMed] [Google Scholar]
- 71.Møller P, Haug E, Raballo A, Parnas J, Melle I. Examination of anomalous self-experience in first-episode psychosis: interrater reliability. Psychopathology 2011; 44: 386– 90. [DOI] [PubMed] [Google Scholar]
- 72.Nordgaard J, Parnas J. Self-disorders and schizophrenia-spectrum: a study of 100 first hospital admissions. Schizophr Bull 2014. Feb 7 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Raballo A, Parnas J. Examination of anomalous self-experience: initial study of the structure of self-disorders in schizophrenia spectrum. J Nerv Ment Dis 2012; 200: 577– 83. [DOI] [PubMed] [Google Scholar]
- 74.Nelson B, Thompson A, Yung AR. Basic self-disturbance predicts psychosis onset in the ultra high risk for psychosis ‘prodromal’ population. Schizophr Bull 2012; 38: 1277– 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Haug E, Lien L, Raballo A, et al. Selective aggregation of self-disorders in first-treatment DSM-IV schizophrenia spectrum disorders. J Nerv Ment Dis 2012; 200: 632– 6. [DOI] [PubMed] [Google Scholar]
- 76.Škodlar B, Parnas J. Self-disorder and subjective dimensions of suicidality in schizophrenia. Compr Psychiatry 2010; 51: 363– 6. [DOI] [PubMed] [Google Scholar]
- 77.Haug E, Melle I, Andreassen OA, et al. The association between anomalous self-experience and suicidality in first-episode schizophrenia seems mediated by depression. Compr Psychiatry 2012; 53: 456– 60. [DOI] [PubMed] [Google Scholar]
- 78.Haug E, Øie M, Melle I, et al. The association between self-disorders and neurocognitive dysfunction in schizophrenia. Schizophr Res 2012; 135: 79– 83. [DOI] [PubMed] [Google Scholar]
- 79.Koren D, Reznik N, Adres M, et al. Disturbances of basic self and prodromal symptoms among nonpsychotic helpseeking adolescents. Psychol Med 2013; 43: 1365– 76. [DOI] [PubMed] [Google Scholar]
- 80.Loewy RL, Bearden CE, Johnson JK, Raine A, Cannon TD. The prodromal questionnaire (PQ): preliminary validation of a self-report screening measure for prodromal and psychotic syndromes. Schizophr Res 2005; 79: 117– 25. [PubMed] [Google Scholar]
- 81.Haug E, Øie M, Andreassen OA, et al. Anomalous self-experiences contribute independently to social dysfunction in the early phases of schizophrenia and psychotic bipolar disorder. Compr Psychiatry 2014; 55: 475– 82. [DOI] [PubMed] [Google Scholar]
- 82.Sass L, Pienkos E, Nelson B, Medford N. Anomalous self-experience in depersonalization and schizophrenia: a comparative investigation. Conscious Cogn 2013; 22: 430– 41. [DOI] [PubMed] [Google Scholar]
- 83.Parnas J. The core gestalt of schizophrenia. World Psychiatry 2012; 11: 67– 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Parnas J. The DSM-IV and the founding prototype of schizophrenia: are we regressing to a pre-Kraepelinian nosology? In: Kendler K Parnas J, eds. Philosophical issues in psychiatry II: nosology. Oxford: Oxford University Press, 2012: 237– 59. [Google Scholar]
- 85.Ebisch SJ, Mantini D, Northoff G, et al. Altered brain long-range functional interactions underlying the link between aberrant self-experience and self-other relationship in first-episode schizophrenia. Schizophr Bull 2013. Nov 4 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ferri F, Ardizzi1 M, Ambrosecchia M, Gallese V. Closing the gap between the inside and the outside: interoceptive sensitivity and social distances. Plos One 2013; 8: e75758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gamma F, Goldstein JM, Seidman LJ, Fitzmaurice GM, Tsuang MT, Buka SL. Early intermodal integration in offspring of parents with psychosis. In: Schizophr Bull, 2013. Aug 28 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nelson B, Yung AR, Bechdolf A, McGorry PD. The phenomenological critique and self-disturbance: implications for ultra-high risk (“prodrome”) research. Schizophr Bull 2008; 34: 381– 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nelson B, Parnas J, Sass LA. Disturbance of minimal self (ipseity) in schizophrenia: clarification and current status [Editorial]. Schizophr Bull 2014; 40: 479– 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Škodlar B, Henriksen MG, Sass LA, Nelson B, Parnas J. Cognitive-behavioral therapy for schizophrenia: a critical evaluation of its theoretical framework from a clinical-phenomenological perspective. Psychopathology 2013; 46: 249– 65. [DOI] [PubMed] [Google Scholar]


