Abstract
Background: Prescribing represents a new aspect of practice for nurses. To make qualitative results more accessible to clinicians, researchers, and policy makers, individuals are urged to synthesize findings from related studies. Therefore this study aimed to aggregate and interpret existing literature review and systematic studies to obtain new insights on nurse prescription.
Methods: This was a qualitative meta synthesis study using Walsh and Downe process. In order to obtain data all Digital National Library of Medicine's databases, search engines and several related sites were used. Full texts with "review and nurs* prescri* " words in the title or abstract in English language and published without any time limitation were considered. After eliminating duplicate and irrelevant studies, 11 texts were selected. Data analysis was conducted using qualitative content analysis. Multiple codes were compared based on the differences and similarities and divided to the categories and themes.
Results: The results from the meta synthesis of the 11 studies revealed 8 themes namely: leading countries in prescribing, views, features, infrastructures, benefits, disadvantages, facilitators and barriers of nursing prescription that are discussed in this article. The results led to a schematic model.
Conclusion: Despite the positive view on nurse prescribing, there are still issues such as legal, administrative, weak research and educational deficiencies in academic preparation of nurses that needs more effort in these areas and requires further research.
Keywords: Nurse prescribing, Meta-synthesis, Review
Introduction
Many countries have introduced non-medical prescription to improve efficiency and access to medication, particularly where access to doctors can be difficult (1). The number of countries where nurses are legally permitted to prescribe medication has grown considerably over the last two decades (2). Now in many countries (Australia, USA, UK, Canada, Ireland, etc) specific groups of nurses are allowed to prescribe various drugs (3).
In fact, in countries with a well-developed education system for nurses, opportunities exist for nurses to obtain advanced practice training and graduate education; in the US, Canada and the United Kingdom. For example, a nurse practitioner typically defined as a registered nurse who is educated to function in an advanced clinical role and prescribing is one aspect of this advanced clinical role (4).
The benefits of non-medical prescribing have been consistently reported in the literature (1). Improved speed and convenience of access to medicines have been consistently reported as key benefits of non-medical prescription by patients and health professionals (1).
According to this, the World Health Organization (WHO) in the fifth meeting of the regional advisory panel in the Eastern Mediterranean nursing convention (Islamabad, Pakistan, 2001) recommended that it required nurses as first-line health care providers to be empowered and prepared to prescribe properly (5). However, nurses in many countries still do not have the authority to prescribe medication. The introduction of major policy initiatives, such as nurse prescribing, requires high level of discussion and policy development to ensure successful implementation (6). Accordingly, each country can utilize international experiences to minimize their inevitable losses and damages. It can give new insight regarding the different aspects and necessity of implementation of nurse drug prescribing in leading countries. A significant number of review studies have been conducted related to nurse prescribing (2,7-16). Each of these studies has contributed to our understanding of nurse prescribing, but to both advance knowledge and policy making for its implementation, knowledge synthesis across multiple studies is required. To make qualitative results more accessible to clinicians, researchers, and policymakers, individuals are urged to synthesize findings from related studies (17). Thus the purpose of this study was to aggregate and interpret existing literature review and systematic review studies to obtain new insights on nurse prescribing drugs, and to present a schematic model of nurse prescribing that can be a useful framework for its implementation. According to the purpose of the study, the following questions were considered in literature reviews:
- What is the overall view on nurse prescribing?
- What are the positive and negative outcomes of nurse prescribing?
- What are the barriers and facilitators for its implementation?
Methods
Qualitative Meta synthesis method was applied to conduct this study. The purpose of the Meta synthesis is to dig below the surface of what is currently understood regarding a phenomenon, to emerge with the kernel of a new truth, a better kind of understanding of something (18). Metasynthesis, a systematic synthesis of findings across qualitative studies, seeks to generate new interpretations for which there is a consensus within a particular field of study (19). A qualitative meta synthesis integrates individual qualitative studies by bringing together and breaking down the findings (themes, metaphors, or categorizations) of individual studies, elucidating the key features, and combining these findings into a transformed whole –a single description of the findings that authentically represents all of the cases (20).
The meta synthesis process employed in this study followed that done by Walsh and Downe (2005) (21). Walsh and Downe developed and proposed a seven-step approach for the qualitative meta-synthesis: (1) framing a meta-synthesis exercise, (2) locating relevant papers, (3) deciding what to include, (4) appraising studies, (5) comparing and contrasting exercise, (6) reciprocating translation, and (7) synthesizing translation (21).
Search strategy included all of the following databases, search interfaces and journals of INLM (Integrated Digital National Library of Medicine) from August 14, 2012 to December week 4 2012: EBSCO host (CINAHL), EBSCO host (Medline), Ovid SP (MEDLINE(R)), Cochran Library, Scopus, Web of science, Elsevier, Emelard, JAMA Journals, Wiley, Oxford Journals, Springer and Thieme Journals and few related sites (World Health Organization (www.who.int), websites for health professionals (http://www.nurse-prescriber.co. uk), Google Scholar (scholar.google.com) and http://journals.cambridge.org/action/ search).
The inclusion, exclusion criteria and appropriate data sources were identified. The inclusion criteria included: all studies without time restriction that contain search terms (review and nurs* prescri*) in the title or abstract, with published full text in English. The review studies that had a search strategy were included but review studies of experts' opinion and without a search strategy were excluded from the meta synthesis.
One researcher screened all titles and abstracts and two other researchers during supervising the process of study, screened full texts as relevant to the purpose of study. Quality assessment and data extraction was carried out by three researchers.
The qualities of included papers were appraised using AMSTAR tool (Assessment of Multiple Systematic Reviews consists of 11 items) (22) and CASP tool (Critical Appraisal Skills Program for Review articles with 10 items) (23). Studies were awarded a score between 0 and 11 for AMSTAR and 0-10 for CASP tool. Studies rated as low, medium, and high quality.
Results
The electronic search yielded 5829 results in which. 49 were duplicated and 5739 had no relevant to the research objectives and therefore excluded. This reduced the number of texts to 41. The full texts of the remaining 41articles were reviewed and a further 30 put aside and not reviewed (i.e. book review). Finally, 11 studies were selected, reviewed and included in this study (2,7-16).Figure 1 shows summary of the selection process for articles used in the study. Table 1 illustrates search strategy of Ovid SP (MEDLINE(R))
Fig.1 .
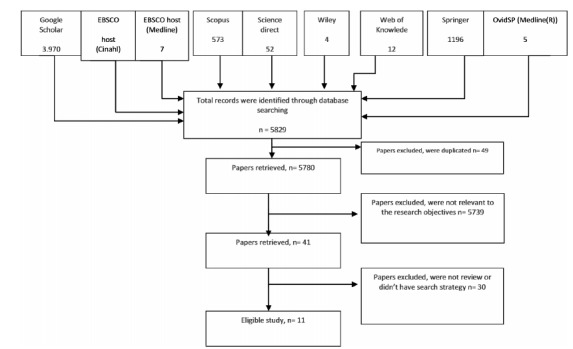
The flowchart for the search and selection process
Table 1 . Search Strategy of Ovid SP (MEDLINE(R)) .
| Search history | Search Terms | Studies Returned, n |
| 1 | nurs* prescri*.m_titl. | 338 |
| 2 | Limit 1 to (english language and yr=''1946-2012'') | 324 |
| 3 | Limit 1 to (english language and full text and yr=''1946-2012'') | 61 |
| 4 | nurs* prescri* and review.m_titl. | 9 |
| 5 | nurs* and prescri* and review.ti. | 20 |
| 6 | Limit 5 to (english language and full text) | 5 |
4 of these 11 review articles were considered as systematic review and 7 literature review. Systematic review articles were evaluated by means of AMSTAR in which three were strong (score of 0.8) and one moderate (score of 0.51 to 0.79). Review articles with CASP (Critical Appraisal Skills Program) tool were tested that three were evaluated as "strong" (score more than 0.8) and 4 "moderate" articles (score of 0.51 to 0.79).
All 11 studies that met the inclusion criteria were read line by line several times in order to get the intended message of the content as well as an accurate impression of the context. The results and conclusions of studies were considered as “meaning units” and coded, integrated, synthesized and categorized. Multiple codes based on the differences and similarities compared and divided into category and themes. The results of meta synthesis revealed 8 themes namely: Leading countries in prescribing, Views, Features, Infrastructures, Benefits, Disadvantages, Facilitators and Barriers. Examples illustrating these themes can be found in Tables 1, 2 and 3. These themes are described bellow.
Table 2 . Cods, Categories and Illustrations of Features of nurse prescribing identified by the meta- synthesis .
| Categories | Cods | Illustrations | Authors |
| Quality and safety of practice | -No differences in the health status of patients treated with Physicians and nurses | "No differences in health status were found" | Horrocks, et al., 2002 (7) |
| -Long consultation nurse practitioners than to physicians | "Nurse practitioners had longer consultations and made more investigations than did doctors" | Horrocks, et al., 2002 (7) | |
| - No differences in prescriptions, return consultations, or referrals | "No differences were found in prescriptions, return consultations, or referrals." | Horrocks, et al., 2002 (7) | |
| -Better quality of care Quality of care in some ways for nurse practitioner consultations | "Quality of care was in some ways better for nurse practitioner consultations" | Horrocks, et al., 2002 (7) | |
| some studies in primary and secondary care found that nurses had longer consultation times than GPs, although does not report the statistical significance of this finding. | Van Ruth, et al., 2008 (12) | ||
| -No security problem | "The synthesis revealed no major safety concerns as a result of the implementation of PGDs." | Price, et al., 2012 (16) | |
| similar or better therapeutic Clinical parameters of nursing | "Clinical parameters were the same or better for treatment by nurses" | Van Ruth, et al., 2008 (12) | |
| -Similar or higher patient satisfaction with nurse prescribing | "Eight studies all found that patients being treated by nurses were just as satisfied or more satisfied than patients being treated by physicians" | Van Ruth, et al., 2008 (12) | |
| -Same or better quality of perceived nurses care | "perceived quality of care by nurses is similar or better." | Van Ruth, et al., 2008 (12) | |
| Confidence in prescribing | - Felt confident | "All studies reported that the majority of respondents felt confident in their prescribing." | Creedon , et al., 2009 (13) |
| - moderately confident | "Most respondents that prescribed less than three times per week were moderately confident and felt somewhat limited by the nurse prescribers’ formulary" | O' Connell, et al., 2009 (14) | |
| -Feeling of Limited prescription | |||
| Areas of nurse prescribing | nurses prescribing practices | Nine studies investigated nurses prescribing practices consisted of antibiotics, anti hypertensives, cardiovascular drugs, dermatological and skin conditions, analgesics, diabetic medications and controlled drugs. | O' Connell, et al., 2009 (14) |
| Prescribing patterns | diversity of forces leding to nurse prescribing | "A diversity of external and internal forces has led to the introduction of nurse prescribing internationally." | Kroezen, et al., 2011 (2) |
| "The legal, educational and organizational conditions under which nurses prescribe medicines vary considerably between countries; from situations where nurses prescribe independently to situations in which prescribing by nurses is only allowed under strict conditions and supervision of physicians." | Kroezen, et al., 2011 (2) | ||
| variation in prescribing patterns | "There is some variation in the prescribing patterns of district nurses’, health visitors’ and practice nurses" | Latter and Courtenay, 2004 (10) |
Table 3 . Summary of barriers of nurse prescribing identified by the meta-synthesis .
| Categories | Cods | Illustrations | Authors |
| Legal limitations | limitations of Nurse Prescribers’ Formulary | There is some variation in the prescribing patterns of district nurses’, health visitors’ and practice nurses, and the limitations of the original Nurse Prescribers’ Formulary (NPF) have been highlighted | Latter and Courtenay, 2004 (10) |
| legal restrictions | All Western-European and Anglo-Saxon countries that have realised or initiated nurse prescribing have imposed legal restrictions on which categories of nurses can prescribe medicines, what, how much and to whom they can prescribe, and whether they are allowed to do so on an independent basis or under the supervision of a physician. | Kroezen, et al., 2011 (2) | |
| Executive Factors | implementation barriers | implementation barriers emerged from the empirical and anecdotal literature, including funding problems, delays in practicing and obtaining prescription pads, encumbering clinical management plans and access to records. | Cooper, et al., 2008 (11) |
| safety concerns | There were a number of safety concerns identified including: nurses using their professional judgment to deliberately work outside the parameters of PGDs (Miles et al, 2001), poor record keeping (Brooks et al, 2003; Deave et al, 2003; Baileff, 2007) and the development of PGDs that failed to comply with legal requirements (Deave et al, 2003). | Price, et al., 2012 (16) | |
| Humanistic Factors | Lack of confidence in applied pharmacology and therapeutics among nurses | although patients were consent with nurses prescribing medication, nurses lacked confidence in applied pharmacology and therapeutics and hence, required additional scientific education | Banning, 2004 (8) |
| nurses’ fears of becoming overconfident | Bradley et al (2007) reported nurses’ fears of becoming overconfident and prescribing outside their competency area. | Creedon , et al., 2009 (13) | |
| medical apathy | medical apathy and independent prescribing potentially undermine the success of SP | Cooper, et al., 2008 (11) | |
| Educational deficiencies | Lack of doctors knowledge on the training of nurse rescribers | The Swedish GPs interviewed in Wilhelmsson and Foldeive’s (2003) study lacked knowledge on the training of nurse prescribers, which could account for their negative views on nurse prescribing | Creedon , et al., 2009 (13) |
| substantial gaps in the knowledge base | Our review suggests that there are substantial gaps in the knowledge base to help evidence based policy making in this arena. | Bhanbhro, et al., 2011 (15) | |
| deficits in the scientific preparation of nurses | This review has drawn attention to the deficits in the scientific preparation of nurses in applied pharmacology and therapeutics. | Banning, 2004 (8) | |
| Research weaknesses | methodological weaknesses | there are both methodological weaknesses and under-researched issues that point to the need for further research into this important policy initiative. | Latter and Courtenay, 2004 (10) |
| Empirical studies were often methodological weaknesses and under-evaluation of safety, economic analysis and patients’ experiences were identified in empirical studies | Cooper, et al., 2008 (11) |
Further research is needed to provide a picture for investigated concept. The results were lead to a schematic model (Fig. 2). This model of nurse prescribing can help policymakers to identify areas for attention.
Fig. 2 .
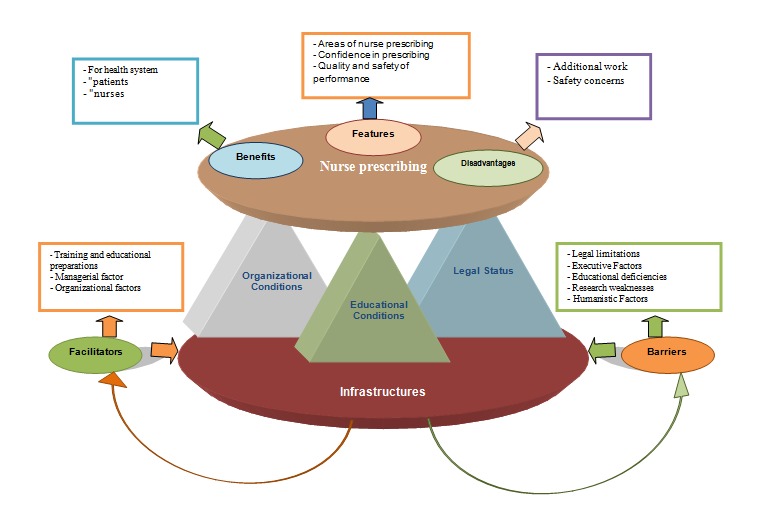
Schematic model of nurse prescribing medicine
Leading countries in prescription drug
The results showed that four studies in this meta synthesis focused on the leading countries in prescription drug (2, 13-15).
Bhanbhro et al (2011) found that the majority of studies about nurse prescribing were undertaken in the UK with only one from USA, Canada, Botswana and Zimbabwe each (15). In addition, Kroezen et al (2011) showed that seven Western European and Anglo-Saxon countries (Australia, Canada, Ireland, New Zealand, Sweden, the UK and the USA) had implemented nurse prescribing medicines. Netherlands and Spain were in the process of introducing nurse prescribing drug policies (2).
Views relating to nurse prescribing
Nine studies indicated the views (doctors, nurses, and patients) related to nurse prescriber (8-16). All of these studies have reported positive views on nurse. For example Latter and Courtenay (2004) stated: “The review highlights that nurse prescribing has generally been evaluated positively to date” (10).
Also Van Ruth et al (2008) mentioned "The effects of nurse prescribing seem positive, although the high risk of bias in the studies means they must be regarded with caution" (12).
In addition, Bhanbhro et al. (2011) reported that non-medical prescribing was widely accepted and viewed positively by patients and professionals (15).
Only two studies noted indirectly negative views of physicians on the nurse practitioners prescribing medicine as follows:
"Nurses and pharmacists were positive about supplementary prescribing (SP) but the medical profession were more critical and lacked awareness/ understanding, according to the identified literature" (11).
Also Creedon, et al (2009) quoted Wilhelmsson and Foldeivi (2003) that the Swedish GPs had lacked knowledge on the training of nurse prescribers, which could account for their negative views on nurse prescribing (13).
However, these negative views can be a barrier that should be given particular importance to the implementation of nurse prescriber.
Features
Results showed that seven authors came up with the issue of Features of nurse prescribing (2, 7, 10, 12-14,16).This issue consists of 4 category (Prescribing patterns, Areas of nurse prescribing, Confidence in prescribing and Quality and safety of practice) that emerged in this study. Table 2 shows summary of emerged cods and categories of this issue.
The findings showed the most important feature of nurse prescribing was long consultation results of Horrocks et al (2002) and Van Ruth et al (2008) studies. These studies noted that longer consultations lead to better quality of care and increase patient satisfaction and improve patient-centered care as the main goal of health care system (7, 12).
Benefits
Eight studies (7-10,12-14,16) investigated benefits of nurse prescribing. These benefits were categorized as: benefits for health system, patients, and nurses. Benefits for health system consists of better care delivery, acquiring patients satisfaction, reduction in number of required personnel, effectiveness and potentially reduction in costs.
There were some benefits for patients including convenience, easier access to drugs and care, receive better care, health promotion, earlier treatment, reduce in waiting time for medication, safety, satisfaction of care, improvement in compliance with medications, prevention of relapses, closeness and proximity of patients to health care providers, make sense of the nurses concerns expressed by patients and reduction in the number of journeys some carers had to make. And benefits for nurses included reduction in workload, time saving, professional autonomy, professional development, satisfaction of role, increasing clinical competence, better use of nurses' skills and experience, recognition abilities, capabilities and expertise of nurses, better accountability, enhance the effective monitoring and reporting of adverse drug reactions, improve communication between the professional health care team. In addition, the evidence showed that nurse prescribing was also useful for physicians and other health care professionals. Jabareen (2008) quoted Crossman (2006) that Nurse prescribing allows GPs to take on more complex cases (27). Also Bowskill (2009) quoted Jordan, Knight and Pointon (2004) and Jones et al (2007) that nurse prescribing was a useful means for reducing professional distance, enabling nurse prescribers to work more closely with medical colleagues (28).
Disadvantages
Two studies (9, 16) mentioned disadvantages of nurse prescribing. Harris (2004) stated this Disadvantage as follows: "Most of nurses felt that there was additional work associated with record keeping and administration" (9). Price et al (2012) has quoted the disadvantage as "safety concerns" including: working outside the parameters of Patient Group Directions (PGD), poor record keeping and the development of PGD that failed to comply with legal requirements (16).
Infrastructures
In total, the meta synthesis showed that three authors investigated the infrastructures of nurse prescribing (2, 10, 15). Most other studies were not relevant to the main study question. This issue covered three categories (legal status, educational and organizational conditions).
Only one study stated the legal restrictions as follows: "All Western-European and Anglo-Saxon countries that have realized or initiated nurse prescribing have imposed legal restrictions on which categories of nurses can prescribe medicines" (2).
Two studies (2, 15) addressed organizational conditions as illustrated in the following comment:
"The gradual growth over time of legislative authority and in the numbers of non-medical prescribers, particularly nurses, in some countries suggests that the acceptability of nonmedical prescribing is based on the perceived value to the health care system as a whole (15) and "It is nonetheless clear that most countries operate some sort of mandatory registration system in which nurse prescribers have to be registered before they are allowed to prescribe" (2).
One study (2) which focused on educational conditions stated: "nurses are required to successfully complete a prescribing course before they are allowed to start prescribing and one of the most important requirements for nurses internationally to enter prescribing programs is sufficient clinical experience" and also: "nurses must have three - five years of clinical experience in their own field of practice, before they are eligible for endorsements as a nurse practitioner and hence for prescribing medicines".
Barriers
The results indicated barriers to nurse prescribing categories included: legal limitations, executive factors, educational deficiencies, research weaknesses, humanistic factors such as concerns about the adequacy of pharmacologic knowledge and unaware of physicians about nurse prescribing education (Table 3).
Facilitators
The results of the meta synthesis indicated the facilitators of nurse prescribing such as training and educational preparations, managerial factor for support mechanisms and competency assessment, organizational factors to aware physicians and other staff about nurse prescribing. Table 4 shows summary of facilitators in nurse prescribing implementation identified by the meta-synthesis.
Table 4 . Summary of facilitators of nurse prescribing identified by the meta-synthesis .
| Categories | Cods | Illustrations | Authors |
| Educational factors | Appropriate education and training to safe and effective prescribing need for further training | appropriate education and training were essential not only for safe and effective prescribing but also for a wider role in medicines management | Harris, 2004 (9) |
| Both Luker et al. (1997) and Brooks et al. (2001) also comment on nurses’ need for further training as the expansions to the formulary are introduced. | Latter and Courtenay, 2004 (10) | ||
| Educational needs | Tyler & Hicks (2001) survey of family planning nurses’training needs for prescribing identified nurses’ views on the top 15 training needs, that included research, advanced clinical activities, applied pharmacology, administration and technical activities. | ||
| The need for scientific education in applied pharmacology | although patients were consent with nurses prescribing medication, nurses lacked confidence in applied pharmacology and therapeutics and hence, required additional scientific education | Banning, 2004 (8) | |
| One can suggest that pre-registration nurses should receive a comprehensive scientific foundation in applied pharmacology and therapeutics and professional knowledge in order to prepare them for post graduate education and training in medication management | |||
| Managerial factors | support mechanisms | Two studies looked specifically at the support mechanisms nurses require in practice to enable good prescribing. | Latter and Courtenay, 2004 (10) |
| nurses’ confidence with Supplementary prescribing to prescribe independently. | Supplementary prescribing was found to be useful in the initial stages as it builds nurses’ confidence to prescribe independently. | Creedon , et al.,2009 (13) | |
| competency assessment | In order to improve safety, increased competency assessment and training was recommended (Baxter et al, 2002; Jones, 2002b; Larsen, 2004; Baileff, 2007), in conjunction with the development of national PGDs by the DH (Baxter et al, 2002). Methods of competency assessment found to be effective included knowledge assessment via questionnaire (Brooks et al, 2003) and role play (Bacon et al, 2003). | Price, et al., 2012 (16) | |
| Organizational factors | awareness of physicians and other staff | There was a perception that nurse and pharmacist independent prescribing may supersede supplementary prescribing | Cooper, et al., 2008 (11) |
As the results show in Schematic model (Fig. 2), barriers and facilitators are directly in contact with infrastructures. In fact, with structural reforming, the barriers will be eliminated and the implementation of the nurse prescribing will be facilitated.
Discussion
Our analysis showed different aspects of nurse prescribing that can help other countries act on its implementation with greater recognition.
The first theme "the leading countries in prescribing" depicted that the implementation of nurse prescribing in UK was higher than other countries. Nurse drug prescribing in the UK has grown significantly over the last decade and it is well established as a mainstream qualification (29).
Despite this fact that nurse prescribing has had well growth in European and American countries, but unfortunately, there is no evidence to indicate its implementation in Asian countries. This may be attributed due to diverse policy of health care system, cultural, economical, political and social conditions dominated in these countries that the nurses. Hence, despite the useful information derived from leading countries, the health policy makers should consider their context for nurse prescribing implementation.
This issue can also be looked at the other side that may be nurses are prescribing in these countries now, but it has not been published in online articles. As the Miles et al (2006) mentioned detailed information about the specific nature of nurse prescribing in low-resource settings was generally lacking in the literature (30).
The theme "Views"(second theme) indicated the views of different stakeholders (doctors, nurses, and patients) on nurse prescribing. Although all reviews studies reported positive views regarding nurse prescribing but negative views of physicians was reported which may be due to lack of knowledge on the training of nurse prescribers. Health professions have often specific knowledge in their field and do not have sufficient awareness about other professions. This may cause resistance to implementation of such activities that have overlap with their areas of functions. However, the health policy makers should pay special attention to this issue in their strategic planning and provide proper context for professional's familiarity with other fields. For instance it is recommended some of nursing courses be taught by physicians. In this way, doctors may become more familiar with the content of nursing courses and also nurses learn better interaction with physicians.
Another theme in our findings was" features of nurse prescribing". One of the features of nurse prescribing noted in studies was longer consultations of nurse prescribers than physicians that can lead patient-centered care as a main goal of health care system. This feature is a unique characteristic of nursing that is affected by holistic perspective toward patient. Based on the Irajpour et al (2012) study, more problems raise when some professionals treat patients as medical cases only worth studying rather than a human who needs health services (31). Thus nurse prescribing with their holistic view may probably face fewer problems.
"Benefits" and "disadvantages" were the two other themes emerged in our study.
These results showed in contrast to the considerable benefits of nurse prescribing, there are a few disadvantages that can be corrected by managerial planning. Each of identified benefits is enough important to support the development of nurse prescribing in all countries. These benefits are likely to be extended if nurse practitioners are able to prescribe (32). Here's a point worth mentioning that these reviews despite the many benefits of nurse prescribing have not addressed cost-benefit and cost- effectiveness of nurse prescribing. In other words, there are very few published evaluations about the clinical outcomes and cost effectiveness of nurse prescribing, particularly in direct comparison with doctors, the traditional prescribers of medication (30).
For example it is mentioned in Venning et al (2000) study that clinical care and health service costs of nurse practitioners and general practitioners were similar. However, they concluded if nurse practitioners were able to maintain the benefits while reducing their return consultation rate or shortening consultation times, they could be more cost effective than general practitioners (33). Another possible explanation for cost- effectiveness of nurse prescribing may be the view of hospitals in the past which considered nurses as cheap labor and believed they “owned” nurses. Today, many hospitals hold the same view (34). Thus with a simple count it may be concluded that the nurse prescribing is both cost-benefit and cost-effectiveness. However more information is needed about the cost-benefit and cost-effectiveness of nurse prescribing that point to the need for further research.
Another theme in this meta-synthesis was infrastructures. Although the main issues for implementation of nurse prescribing (legal status, educational and organizational conditions) have been expressed in studies, but there is no available evidence regarding the cultural and political context that strongly affect on the entire topic of nurse prescribing. Importance of this issue is stated in Mills et al study (2oo6) who mentioned some of issues may be somewhat irrelevant when it comes to politically and economically unstable environments (30).
Thus it seems that one of the priorities of nurse prescribing implementation is providing cultural and political context. However these factors can affect as the barriers in nurse prescribing implementation because they can influence on views of policy makers and managers. Then their views can impact on strategic planning, implementation, and supportive structure or even on interaction of medical team colleagues.
The results identified a broad range of barriers and facilitators (Theme 7 and 8). These factors should be inferred as guides for policymakers to implementation of the nurse prescribing. Also the results revealed there are still issues such as legal, administrative, weak research and educational deficiencies in leading countries which needs for more effort to be made in these areas. Based on this review lack of confidence in applied pharmacology and therapeutics is an issue categorized in human factors as the barrier of nurse drug prescription. Conversely, self-confidence is a facilitator in nurse prescribing. On the other hand, delegating authority and enhancing self-confidence of nurses can help them to apply their knowledge in practice (35).
Miles et al (2oo6) expressed there are key elements of success in developing mechanisms for nurse prescribing such as strong political, support of nursing and academic programs to educate. (30). However, one of the problems highlighted with training programs is that many academic nursing education programs are not always feasible, affordable or attainable, particularly in rural areas (30). Support mechanisms are other important issues that are addressed in this meta synthesis. For providing this the nurse managers can play an important role. This support can undertake any facilitating activity, such as providing facilities, means and equipment, information, education, rewards and even some symbolic behaviors that nurses perceive to be facilitating (35). Also the support that physicians give in terms of ongoing training and supervision is important key in nurse prescribing (36).
Conclusion
Considering the findings of this study, it seems that nursing prescribing is positive experience and other countries can introduce its implementation without serious concern. In this metasynthesis, the most important factors identified including providing valuable information for nurse managers and policy makers. However, the results revealed there are still issues such as legal, administrative, weak research and educational deficiencies in leading countries that needs more effort in these areas. Appropriate training and support mechanisms are needed in order to facilitate implementation of nurse prescribing. In spite of the useful information that has been obtained from the study of the leading countries, cultural and social factors of each country are also of great importance. Hence health policy makers should identify barriers and facilitators within their own context and use this information to promote health system.
Ethical Considerations
Although the ethical issues were minimal in this study since no human subjects were involved, the researchers still had an ethical responsibility arising from this study. In order to fulfill this, the researchers considered the ethical responsibility as follows:
Commitment to respecting moral rights of authors and no forging parts or all of the results (data making)
Intentional manipulation of data or analyzes (falsification), or reporting methods not used by the researchers
Recommendations for future research
There are little evidences reporting the economic and financial outcomes of non-medical prescribing. It is therefore recommended that future studies explore cost-benefit and cost-effectiveness of nurse prescribing.
Considering the importance of the cultural context of health systems in implementation of programs, policymakers must recognize this within their own context. It is suggested that next research should be on understanding of infrastructures and existing context of nurse prescribing in each country.
There is also a need for more theory-based research on nurse prescribing. Future research should address this.
Limitations
Limitations of this synthesis include the exclusion of unpublished and in progress reviews and systematic reviews.
Acknowledgements
This study is part of a PhD thesis financially supported by Tehran University of Medical Sciences (Grant Number: 1929).
Conflict of Interest
No conflict of interest associated with this work.
Cite this article as: Darvishpour A, Joolaee S, Cheraghi M.A. A meta-synthesis study of literature review and systematic review published in nurse prescribing. Med J Islam Repub Iran 2014 (22 July). Vol. 28:77.
References
- 1. Carey N, Stenner K. Does non-medical prescribing make a difference to patients? Nursing Times 2011; 107 (26): 14-6. Available at: http://www.nursingtimes.net/nursing-practice/clinical-zones/prescribing/does-non-medical-prescribing-make-a-difference-to-patients/5032082.article [PubMed]
- 2.Kroezen M, van Dijk L, Groenewegen PP, Francke AL. Nurse prescribing of medicines in Western European and Anglo-Saxon countries: a systematic review of the literature. BMC health services research. 2011;11(127) doi: 10.1186/1472-6963-11-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Delamaire M, Lafortune G. Nurses in Advanced Roles: A Description and Evaluation of Experiences in 12 Developed Countries. OECD Health Working Papers. 2010;54(5) [Google Scholar]
- 4. Colleau S M. Expanding nurses' role in pain management: International news on nurse prescribing. WHO Pain &palliative care communication program.Volume 14, No. 4 -- 2001. Available at: http://www.whocancerpain.wisc.edu/?q=node/180.
- 5. WHO Regional Office for the Eastern Mediterranean. Report on the fifth meeting of the Regional Advisory Panel on Nursing and consultation on advanced practice nursing and nurse prescribing: implications for regulation, nursing education and practice in the Eastern Mediterranean. Islamabad: Pakistan 2002. Available at: (accessed 5 April 2012)http://whqlibdoc.who.int/emro/2002/WHO-EM_NUR_348_E_L.pdf.
- 6. Barrowman LM. Review of the Implementation of the Nurse Prescribing Role. Trust Nurses Association in Northern Ireland. 2007 Available at: (accessed 5 April 2012)www.nipec.hscni.net/pub/NursePrescribingFinalRpt.pdf.
- 7.Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. Bmj. 2002;324:819–23. doi: 10.1136/bmj.324.7341.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Banning M. Nurse prescribing, nurse education and related research in the United Kingdom: a review of the literature. Nurse education today. 2004;24(420) doi: 10.1016/j.nedt.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 9. Harris J, Taylor J, Mackie C. Research literature review on prescribing. Scottish Executive Social Research. 2004 Available at: http://www.scotland.gov.uk/Publications/2004/08/19843/42016 (accessed 5 April 2012)http://www.scotland.gov.uk/Publications/2004/08/19843/42016.
- 10.Latter S, Courtenay M. Effectiveness of nurse prescribing: a review of the literature. Journal of Clinical Nursing. 2004;13:26–32. doi: 10.1046/j.1365-2702.2003.00839.x. [DOI] [PubMed] [Google Scholar]
- 11.Cooper RJ, Anderson C, Avery T, Bissell P. et al. Nurse and pharmacist supplementary prescribing in the UK—A thematic review of the literature. Health Policy. 2008;85:277–92. doi: 10.1016/j.healthpol.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Van Ruth LM, Francke AL, Mistiaen P. Effects of nurse prescribing of medication: a systematic review. The Internet Journal of Healthcare Administration. 2008;5(2) [Google Scholar]
- 13.Creedon R, O' Connell E, McCarthy G, Lehane B. An evaluation of nurse prescribingPart 1: a literature review. British Journal of Nursing. 2009;18:1322–27. doi: 10.12968/bjon.2009.18.21.45366. [DOI] [PubMed] [Google Scholar]
- 14.O' Connell E, Creedon R, McCarthy G, Lehane B. An evaluation of nurse prescribing Part 2: a literature review. British Journal of Nursing. 2009;18(22):1398–1402. doi: 10.12968/bjon.2009.18.22.45570. [DOI] [PubMed] [Google Scholar]
- 15.Bhanbhro S, Drennan VM, Grant R, Harris R. Assessing the contribution of prescribing in primary care by nurses and professionals allied to medicine: a systematic review of literature. BMC health services research. 2011;11(330) doi: 10.1186/1472-6963-11-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Price O, Baker J, Paton C, Barnes T. Patient Group Directions: a safe and effective practice? British Journal of Nursing. 2012;21:26–31. doi: 10.12968/bjon.2012.21.1.26. [DOI] [PubMed] [Google Scholar]
- 17.Finfgeld DL. Metasynthesis: the state of the art – so far. Qual Health Res. 2003;13(7):893–904. doi: 10.1177/1049732303253462. [DOI] [PubMed] [Google Scholar]
- 18. Paterson BL, Thorne SE, Canam C, Jillings C. Meta study of Qualitative Health Research. : A Practical Guide to Meta-Analysis and Meta-Synthesis Thousand Oaks. California. Sage Publications 2001. Available at: (accessed 5 April 2012).http://books.google.com/books?id=CAW-g4DrVgwC&q=Meta-Synthesis
- 19.Jabareen YR. Building a conceptual framework: philosophy, definitions, and procedure. International Journal of Qualitative Methods. 2009;8(4):49–62. [Google Scholar]
- 20. Holly C, Salmond S. Comprehensive Systematic Review for Advanced Nursing Practice. Springer Publishing Company 2012. Available at: (accessed 5 April 2012).http://books.google.com/books
- 21.Walsh D, Downe S. Meta-synthesis method for qualitative research: A literature review. Journal of Advanced Nursing. 2005;50(2):204–211. doi: 10.1111/j.1365-2648.2005.03380.x. [DOI] [PubMed] [Google Scholar]
- 22.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Md Res Methodol. 2007;7(10) doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. NHS.Critical Appraisal Skills Programme (CASP) making sense of evidence. Available at: .http://www.casp-uk.net/wpcontent/uploads/2011/11/CASP_Systematic_Review_Appraisal_Checklist_14oct10.pdf
- 24.Humphreys A, Johnson S, Richardson J, Stenhouse E, Watkins M. A systematic review and meta-synthesis: evaluating the effectiveness of nurse, midwife/allied health professional consultants. Journal of Clinical Nursing. 2007;16:1792–1808. doi: 10.1111/j.1365-2702.2007.01757.x. [DOI] [PubMed] [Google Scholar]
- 25.Lefler LL, Bondy KN. Women’s delay in seeking treatment with myocardial infarction. Journal of Cardiovascular Nursing. 2004;19(4):251_268. doi: 10.1097/00005082-200407000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Bondas T, Hall E O C. A decade of metasynthesis research in health sciences: A meta-method study. International Journal of Qualitative Studies on Health and Well-being. 2007;2(2):101_113. [Google Scholar]
- 27. Jabareen H M. Skill Mix Development in General Practice: A Mixed Method Study of Practice Nurses and General Practitioners. PhD thesis. Faculty of Medicine University of Glasgow 2008. Available at: (accessed 5 April 2012).http://theses.gla.ac.uk/632/1/2008JabareenPhD.pdf
- 28. Bowskill D. The Integration of Nurse Prescribing: Case Studies in Primary and Secondary Care. DHSci thesis. University of Nottingham 2009. Available at: (accessed 7 April 2012).http://etheses.nottingham.ac.uk/1036/
- 29. RCN Fact Sheet .Nurse prescribing in the UK. http://www.rcn.org.uk/__data/assets/pdf_file/0004/462370/15.12_NursePrescribing_in_the_UK_RCN_Factsheet.pdf.
- 30.Miles K, Seitio O, McGilvray M. Nurse prescribing in low-resource settings: professional considerations. International Nursing Review. 2006;53(4):290–296. doi: 10.1111/j.1466-7657.2006.00491.x. [DOI] [PubMed] [Google Scholar]
- 31.Irajpour A, Alavi M, Abdoli S, Saberizafarghandi MB. Challenges of interprofessional collaboration in Iranian mental health services: A qualitative investigation. Iranian Journal of Nursing and Midwifery Research. 2012;17(2) [PMC free article] [PubMed] [Google Scholar]
- 32. McMillan M. Nurse prescribing: adding value to the consumer experience. Aust Prescr 2007; 30: 2–3. Online available at: http://www.australianprescriber.com/upload/pdf/articles/851.pdf.
- 33.Venning P, Durie A, Roland M, Roberts C, Leese B. Randomised controlled trial comparing cost effectiveness of general practitioners and nurse practitioners in primary care. BMJ. 2000 April 15;320(7241):1048–1053. doi: 10.1136/bmj.320.7241.1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jones & Bartlett Learning. The Profession of Nursing. available at: samples.jbpub.com/ 9781449649029/46066_CH01_6031.pdf.
- 35.Adib Hagbaghery M, Salsali M, Ahmadi F. A qualitative study of Iranian nurses' understanding and experiences of professional power. Human Resources for Health. 2004;2:9. doi: 10.1186/1478-4491-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stenner K, Carey N, Courtenay M. Implementing nurse prescribing:a case study in diabetes. Journal of Advanced Nursing. 2010;66(3):522–531. doi: 10.1111/j.1365-2648.2009.05212.x. [DOI] [PubMed] [Google Scholar]


