Abstract
Le Fort II and III distraction osteogenesis (DO) is a powerful tool in the craniofacial armamentarium that is most often employed to treat patients with craniofacial syndromes such as Crouzon, Apert, or Pfeiffer syndrome who present with midfacial retrusion, shallow orbits, exorbitism, malocclusion, obstructive sleep apnea and facial imbalance. In this article, the authors will provide the reader with an update on techniques for the treatment of various forms of midfacial retrusion.
Keywords: distraction osteogenesis, midface advancement, Le Fort II and III
Background
In 1901, Rene Le Fort published a report on fractures of the craniofacial skeleton.1 He defined and differentiated fractures patterns of the adult craniofacial skeleton, developing the now commonly used terminology Le Fort I, II, and III.2 Gilles, Tessier, and others applied Le Fort's principles to facial osteotomies, and today they are employed to treat patients with craniofacial syndromes such as Crouzon, Apert, or Pfeiffer syndromes who present with midfacial retrusion, shallow orbits, exorbitism, malocclusion, obstructive sleep apnea, and facial imbalance.2 3 4 5 6 7 8
Classically, the Le Fort II osteotomy involves pyramidal-shaped osteotomies. The bony cuts traverse the nasofrontal suture, the nasal process of the maxilla, the medial orbital wall at the lacrimal bone, the orbital floor, inferior orbital rim and the zygomaticomaxillary suture (Fig. 1). Both pterygoid plates also need to be osteotomized posteriorly. Le Fort III osteotomy, also known as craniofacial dysjunction, can be performed via an intracranial or extracranial approach. The osteotomy traverses the nasofrontal suture, through the fontal process of the maxilla down the medial orbital, through the orbital floor, across the zygomatic frontal suture and zygomatic arch (Fig. 2). Similarly, both pterygoid plates need to be osteotomized posteriorly.4 6
Fig. 1.
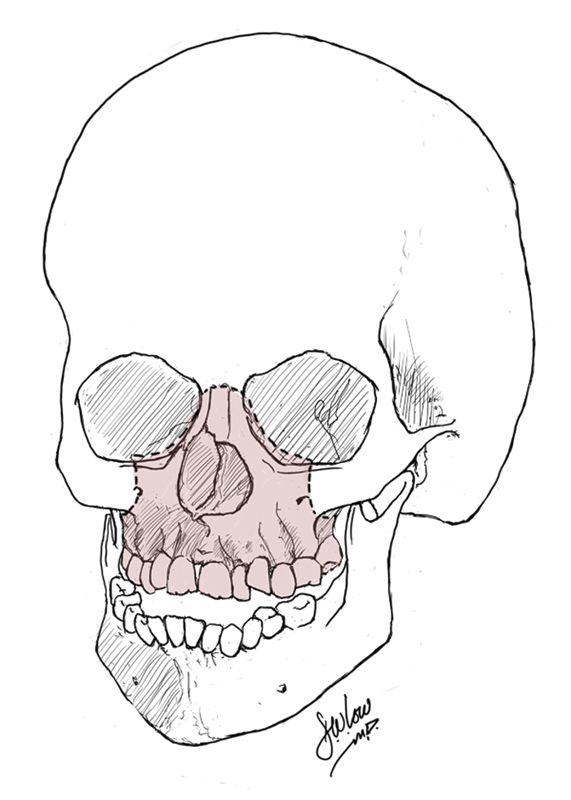
Diagram illustrating standard Le Fort II osteotomies.
Fig. 2.
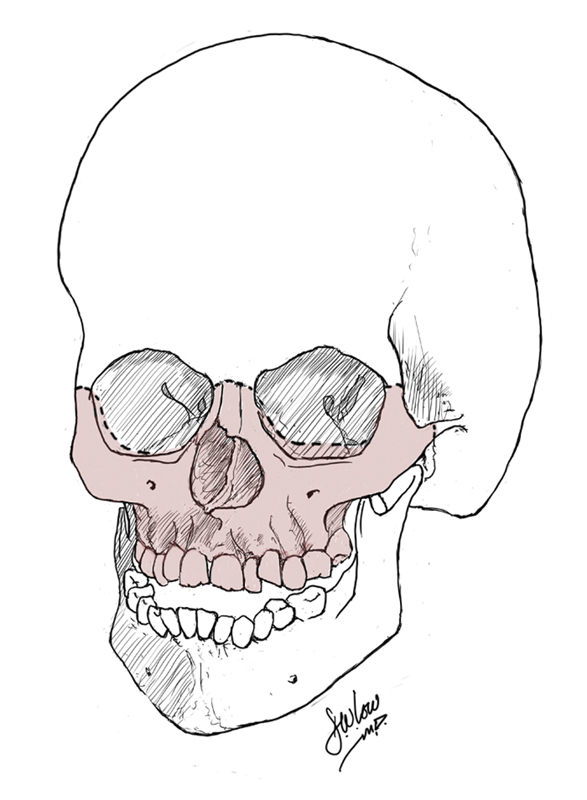
Diagram illustrating standard Le Fort III osteotomies.
Concepts of Midfacial Distraction
Introduced in 1993 by Cohen et al,9 midfacial distraction osteogenesis (DO) has since become a powerful tool in the armamentarium of the craniomaxillofacial surgeon. Over the past two decades, DO has become an adjunct technique to conventional advancement procedures associated with grafting and rigid fixation.10 The main advantages of midfacial DO over traditional osteotomies include the possibility of producing larger movements, as well as a decreased infectious risk and relapse rate due to the progressive distraction and formation of bone. Distraction osteogenesis also provides for gradual expansion of soft tissues, often resulting in pleasing repositioning of the lips, cheek mounds, and eyelids. Moreover, less subperiosteal dissection is performed, operative procedures are shorter in duration, intraoperative blood loss is reduced, the potential use of bone grafts for stabilization purposes is eliminated, while at the same time eliminating potential donor site morbidity. Hospital stays have also been reported to be shorter.11 12 13 14 15 16 17 18 19
The general rule of thumb is that conventional advancement of the midface is indicated in patients requiring less than 8 to 10 mm of advancement. Midface DO is often indicated in patients with craniofacial syndromes or any patients with severe midfacial retrusion requiring advancement of more than 10 mm.15 19 Several reports in the literature demonstrate that DO can achieve advancements exceeding the advancement of the traditional procedure by two- to threefold.11 12 13 20 21 22 23 That stated, some feel that DO is indicated because of its positive soft tissue effects, even in smaller advancements.
Indications
Le Fort II
Midface advancement using Le Fort II DO is commonly indicated in patients with midface hypoplasia involving the maxilla and nasal complex, with an acceptable position of the zygomatic complex and orbits. Those patients often will have an anterior cross bite, class III malocclusion, and obstructive sleep apnea. The aims of the Le Fort II DO are to re-establish ideal overjet and overbite and achieve an acceptable occlusion with good functional class I occlusion.17 24 25 26 At the same time, the Le Fort II allows for lengthening of the nose, a pleasing effect especially in syndromic patients with a classic “dish face” and short nose such as Apert syndrome.25
Le Fort III
Le Fort III DO is indicated in syndromic craniofacial patients with midface hypoplasia involving the nasal, maxillary and zygomatic complex, shallow orbits, exophthalmos, upper airway obstruction and obstructive sleep apnea, class III malocclusion and an overall severe facial aesthetic imbalance. Advancement of the midface with Le Fort III expands the nasopharynx and oropharynx, often allowing for tracheostomy decannulation. In addition, by advancing the midface using Le Fort III DO, the abnormal proptotic position of the globe relative to the orbital rim will be corrected preventing amblyopia, corneal exposure with subsequent exposure keratitis, keratoconjunctivitis sicca and infection leading to corneal ulceration, cataracts, and possibly vision loss.27
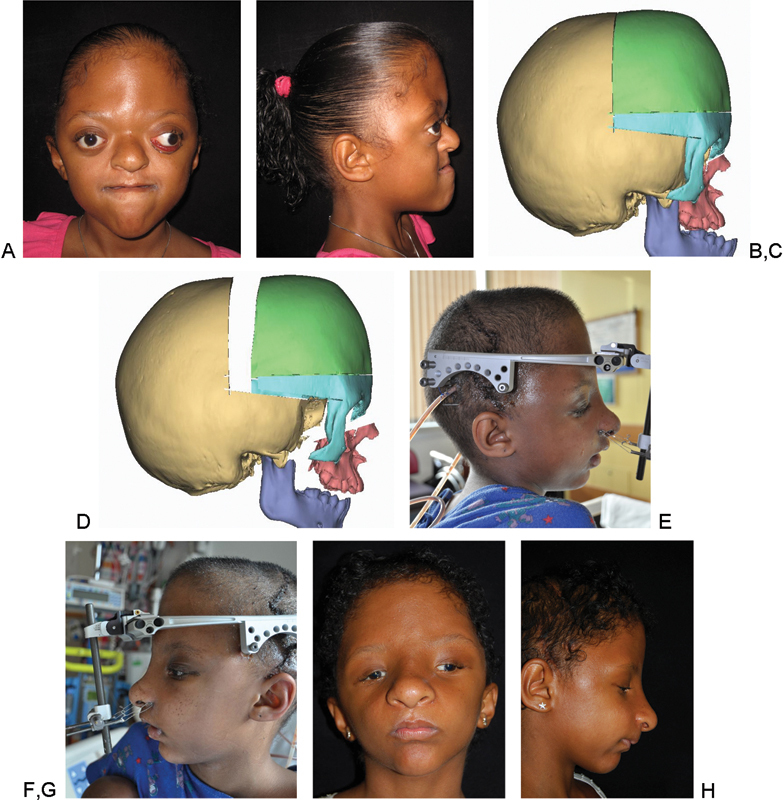
Often a Le Fort III is converted to a monobloc procedure when the retrusive midface is also associated with a retrusive forehead.28 In Fig. 3, we present a 12-year-old girl with Crouzon syndrome and associated midface hypoplasia involving the nasal, maxillary, and zygomatic complex, who underwent successfully a subcranial Le Fort III with DO.
Fig. 3.

A 12-year-old girl with Crouzon syndrome who underwent a subcranial Le Fort III with distraction osteogenesis. (A) Preoperative photograph, anteroposterior (AP) view. (B) Preoperative photograph, left three-quarter view. (C) Preoperative photograph, left lateral view. (D) Early postoperative photograph, with the internal distractor in place, left lateral view. (E) Postoperative photograph, AP view. (F) Postoperative photograph, right three-quarter view. (G) Postoperative photograph, left three-quarter view. (H) Postoperative photograph, right lateral view.
Designer Osteotomies
In rare instances, the traditional Le Fort osteotomies do not ideally treat all patients with craniofacial syndromes. The concept of designer osteotomies can be applied more broadly to include nonclassic midfacial osteotomies in syndromic patients. The following are two examples.
Le Fort II with Zygomatic Repositioning
Hopper29 has extensively studied the unique morphology of the Apert craniofacial skeleton, reporting a “dual axial and sagittal plane concavity that creates an abnormal face in an abnormal position.”29 In this subset of patients, a simple Le Fort III does not address the axial concavity of the maxilla. His approach consists of a Le Fort III osteotomy and acute repositioning of the zygomas (osteotomies illustrated in Fig. 4), which are fixated laterally with titanium plates to the lateral orbital wall and frontal bone, as well as a Le Fort II osteotomy segment that is externally distracted using a custom maxillary splint. Using this combined Le Fort II distraction and zygoma repositioning, the orbital–malar relationship is preserved, no iatrogenic periorbital deformity is created, the Le Fort II segment is distracted significantly more than the zygoma, the midface is lengthened, and the anterior open bite is closed.
Fig. 4.
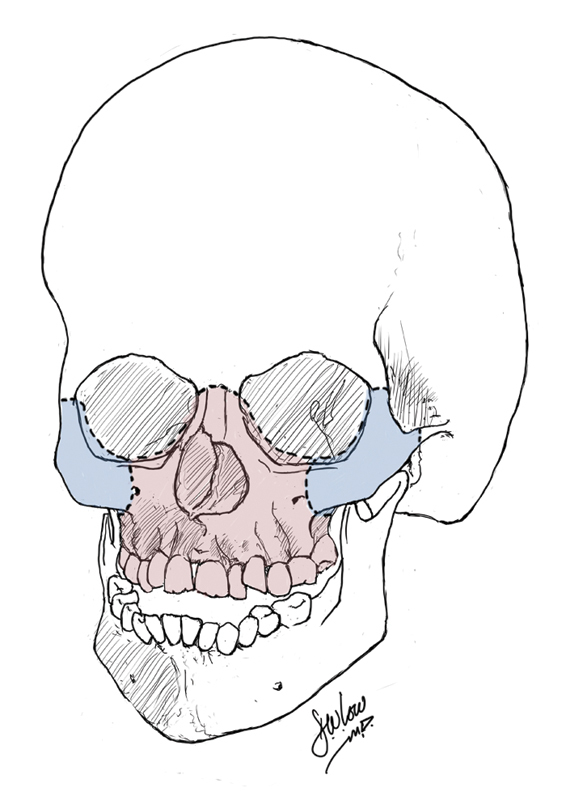
Diagram illustrating osteotomies of the Le Fort II distraction with zygomatic repositioning described by Hopper et al.29
Combined Monobloc and Le Fort II
Along the same lines, Taylor and colleagues25 described a different technique to address the facial dysmorphology of Apert patients, who require, as we mentioned above, differential advancement of the forehead, orbits, and midface to correct fronto-orbital retrusion as well as to lengthen the midface and close the anterior open bite. This technique involves a monobloc minus Le Fort II to address these differential movements in a single operation. Advancement of the forehead and midface is accomplished with the monobloc, while the nose is lengthened and maxilla rotated using the Le Fort II distraction. Similar to Hopper's approach, the monobloc Le Fort II adapts classic craniofacial osteotomies to fit the unique morphology of a given situation. In Fig. 5, we present an 11-year-old girl with Apert syndrome who presented to our clinic with the typical the Apert phenotype, including bicoronal synostosis, papilledema, exorbitism, a severely retruded midface, a shortened nose, and a severe class III malocclusion. To correct her turribrachycephaly and exorbitism, a monobloc distraction with a horizontally oriented vector was planned with internal distractors. To simultaneously correct the hypoplastic midface, lengthen the nose, correct the class III malocclusion, and close the anterior open bite, a Le Fort II distraction with an oblique vector and clockwise rotation was planned. To minimize interference between these two independent moving segments, computer aided design/computer aided modeling (CAD/CAM) planning with cutting and positioning guides was utilized. Distraction of the Le Fort II segment was achieved using an external halo, with fixation pins located at the bilateral pyriform apertures.
Fig. 5.
An 11-year-old girl with Apert Syndrome who underwent monobloc minus Le Fort II. (A) Preoperative photograph, anteroposterior (AP) view. (B) Preoperative photograph, right lateral view. (C,D) Computer aided design/computer aided modeling virtual planning. (E) Early postoperative photograph, right lateral view, with external distractor in place. (F) Early postoperative photograph, left lateral view, with external distractor in place. (G) Late postoperative photograph, AP view. (H) Late postoperative photograph, right lateral view.
Timing
Facial growth occurs in two important phases.30 The first phase consists of the first 6 to 7 years of life and is mostly dependent on growth of the brain, eyes, and nasal cartilage. In the second phase, after 6 to 7 years of life, facial growth occurs mostly because of bony apposition, enlargement of the nasal cavity, and growth of the maxillary alveolar process.30 Ideally, Le Fort II and III osteotomies and DO are performed at age 6 to 10 years when the craniofacial skeleton is easier to mobilize and an attempt can be made to position the orbital rim and margins at the ideal relationship to the globes.31
Various studies have evaluated facial growth in patients with craniofacial syndromes,13 32 33 34 35 reporting minimal or absent horizontal and sagittal growth with preservation of vertical growth. Along the same lines, Fearon13 concludes that the absence of growth in this specific patient population is intrinsic to the disease process and not to the procedure performed. Thus, surgery may have no detrimental effect on skeletal growth. One has to keep in mind that scarring may however impair soft tissue growth.
Thus, timing of the midface procedure should be bound to clear indications. For instance, patients with severe OSA, midface retrusion and ocular proptosis/exophthalmos may benefit from a relatively early procedure. On the other hand, patients with less severe morphology and symptoms may benefit from these procedures at skeletal maturity. Each patient should be approached in an individual manner.
External versus Internal Distractors for Le Fort II and III
Distractors come in various shapes and forms, but they can generally be classified as either internal distractors or external distractors (halo-like devices). The advantages and disadvantages of each are discussed in the following paragraphs.27
The main advantage of an internal distractor is that it is less conspicuous and impacts less the patient's daily activities. These devices are relatively small and less intrusive for patients and families. Major disadvantages include uniplanar distraction vector, inability to manipulate the distraction vector postoperatively, and a slightly increased infection rate.27 Internal devices require a second procedure under anesthesia for removal, which can also be challenging.27 Various groups36 37 have examined the role of resorbable internal devices, however, no comparative studies have been performed and no long-term follow-up studies have been published.
In 1997, Polley38 was the first to describe the use of an external “halo-type” distractor for Le Fort III distraction. Although rigid, external devices allow for easy adjustment in the postoperative period, often in more than one vector. This allows for “orthodontic” adjustment of the distracted segment in multiple vectors to maximize its final position. Additionally, halo-type distractors provide a central “pull” rather than a peripheral “push,” which serves to further unfurl facial concavity often present in syndromic patients. The ability to minimize buried hardware, especially in the region of the bony regenerate, helps to minimize infectious complications as well as maximize bone formation. Generally, they are easy to apply and easy to remove. Disadvantages include the psychosocial discomfort of wearing a large external device, risk of accidental dislodgement, possible infections around the pin sites, scars in the scalp, and the risk of penetration transcranially of the fixation pins.27
Two studies, by Gosain et al39 and Fearon,18 compared outcomes between the use of an external and internal devices. Gosain suggests the use of an external device in older patients and found similar outcomes between the two devices.39 Fearon reported superior results with external distractors compared with internal ones when performing Le Fort III distraction.18 At the Children's Hospital of Philadelphia, we have noticed a trend toward using external devices, likely for all of the reasons noted above.
Author's Preferred Technique
Le Fort II Distraction Osteogenesis
Le Fort II osteotomies and DO is performed under general anesthesia via a standard zig-zag coronal incision for exposing the nasion and medial orbital region. The maxillary antrum and inferior portion of the zygomatic body are exposed via an upper gingivobuccal incision. The upper gingivobuccal sulcus incision is made along the maxillary vestibule from first molar to first molar. Once the nasion, maxillary antrum, and zygomaticomaxillary buttresses are well exposed, reciprocating standard osteotomies following Le Fort II design are performed. The osteotomy through the nasion is made through the coronal incision, slightly below the nasofrontal suture. The nasal septum is cut from above with a guarded osteotome. Osteotomies of the frontal process of the maxilla, the medial orbital wall at the lacrimal bone, the orbital floor, inferior orbital rim, and the zygomaticomaxillary suture are then performed through the gingivobuccal incision. Both pterygoid plates are osteotomized posteriorly using a curved osteotome. Rowe-Kiley disimpaction forceps are then used to gently verify complete mobilization of the Le Fort II segment. Once complete mobilization is verified, an external distractor is applied, with two fixations pins that are applied bilaterally paranasally at the pyriform aperture. For additional control of the distraction segment, a fixation pin can be added at the region of the nasion. Following abundant irrigation, layered closure of the coronal incision and gingivobuccal sulcus incision is performed. Distraction is begun after a 5-day latency period and proceeds at a rate of 1 mm per day. Our consolidation period lasts approximately 2 to 3 months and the external distraction device is then removed in the operating room. Close consultation with a craniofacial orthodontist can help guide the occlusion either with Tads or guiding elastics.
Le Fort III Distraction Osteogenesis
Subcranial Le Fort III DO is performed under general anesthesia via a standard zig-zag coronal incision for exposure of the lateral frontotemporal skull, nasion, temporal fossa, lateral orbital region, zygomatic arch, and zygomatic body. Using a reciprocating saw as well as an ultrasonic saw, standard osteotomies are performed through the zygomatic arch, frontozygomatic suture, floor of the orbit, and nasion. Care is taken to avoid transcranial migration of the saw during this portion of the osteotomy. In the midline, the vomer and ethmoid are separated from the cranial base using a guarded swallow-tail osteotome. Both pterygoid plates are osteotomized posteriorly via transmucosal approach or the coronal approach. Rowe-Kiley disimpaction forceps are then used to gently verify complete mobilization of the Le Fort III segment. Once complete mobilization is verified and prior to the application of the external distractor, a titanium mesh may be applied to both temporal fossas, to prevent transcranial migration of the distractor fixation pins (in patients with thin bone or cranial defects in the temporal region). Two fixation pins are applied bilaterally paranasally at the pyriform aperture; for added control, additional fixation pins can be applied in the region of the nasion. Those pins will act as bony anchors for the distraction device. Following abundant irrigation, layered closure of the coronal incision is performed and the external distractor is applied.
Complications
Complications Related to Le Fort II and III Osteotomies
Complications with Le Fort II and III osteotomies with subsequent DO are similar to the ones associated with traditional Le Fort II and III,28 40 41 42 43 and include infraorbital nerve injury, orbital/globe injury, excessive bleeding, and infection. Dural injury with subsequent cerebrospinal fluid leak is rare but can occur. Other complications include injury to the infraorbital nerve, orbital/globe injury, strabismus, partial anosmia, and localized infections.
Complications Related to Distraction Osteogenesis
Despite technique and device refinements, midfacial DO remains associated with high complication rates, up to 30 to 40%.16 44 45 These complications range from superficial surgical site infections, mostly around the pin sites, to deep soft tissue infection and abscess formation. Specific to the devices, mechanical failure, pin loosening, frame migrations, and finally intracranial fixation pin migration with dural violation, in the setting of halotype distractor can occur (Fig. 6A).44 46 47 Management of this latter complication by the application of temporary titanium meshes bilaterally in both temporal areas hosting the fixation pins is demonstrated in Figs. 6B and 6C.
Fig. 6.
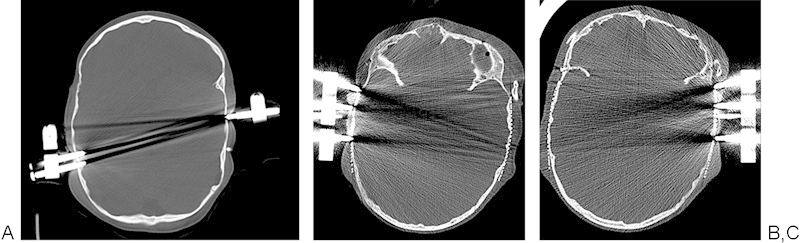
Example of a complication associated with an external halo-type distractor. (A) Axial view of computed tomography scan demonstrating intracranial fixation pin migration with dural violation. (B,C) Management of this latter complication by the application of temporary titanium meshes bilaterally in both temporal areas hosting the fixation pins.
Other complications associated with distraction include asymmetric advancement and severe infections requiring surgical drainage and hospitalization. Despite these complications, while comparing midfacial distraction to traditional advancement, Fearon13 18 reported lower complications rates as well as shorter hospital stay in the distraction group.
Authors' Experience and Complication Rate
From 1999 to 2012, 54 patients underwent midface DO at the Children's Hospital of Philadelphia, including 23 patients with Apert syndrome, 19 with Crouzon syndrome, and 10 with Pfeiffer syndrome, as well as 2 patients with other craniofacial syndromes. Thirty-three patients underwent a total of 34 subcranial Le Fort III distraction procedures and 21 underwent 21 monobloc distraction procedures. The average age at surgery was 8.0 years (range: 4.0–17.7), while average time between distractor placement and removal was 102.9 days. Thirty procedures were performed with external halo-type distractors (18 Le Fort III and 12 monoblocs), while 25 were performed with buried midface distractors (16 Le Fort III and 9 monoblocs). We identified 19 distractor-related complications: There were a total of 10 (18.2%) in the halo group including 5 (9.1%) requiring separate operative intervention, and 9 (16.4%) in the buried distractor group including 6 (10.1%) requiring separate operative intervention. Major infections were more common in the buried distractor group (n = 8) compared with the halo distractor group (n = 3; p = 0.048). There were four (7.3%) patients in the halo group who had malposition or transcranial pin migration related to postoperative positioning or falls that required operative repositioning. Our experience demonstrates that higher rates of halo displacement requiring surgery are offset with lower rates of infections compared with internal devices.
Relapse and Postsurgical Growth
The main advantages of midfacial distraction over traditional osteotomies and advancement include the possibility of producing larger movements, but also a decreased relapse rate due to the progressive distraction and formation of bone and progressive soft tissue expansion.11 12 13 20 21 22 23 48 Since the introduction in 1993 of midfacial DO,9 all reports12 18 35 49 50 51 52 53 54 55 are unanimous with regards to the absence or minimal relapse after DO compared with a higher relapse rate in the traditional acute advancement group. The stability of Le Fort II or III DO advancement is well documented in the literature, particularly in the long-term outcomes studies published by the group from New York University49 50 51 and the Dallas group.18 35 55 However, they demonstrated that although the midface is stable in its new position, it has absent or minimal horizontal and sagittal postsurgical growth and minimal vertical growth. Relapse seen following midfacial distraction is often a misdiagnosis, with “pseudo-relapse” being actually observed. What is possibly seen is absence of growth of the midfacial distracted segment while the mandible is growing normally. This can be easily corrected with a Le Fort I procedure.
Moreover, when considering postsurgical growth of patients after Le Fort II or III, it is important to recognize which patients are evaluated for growth. For instance, one cannot expect a patient with a craniofacial syndrome and severe midface retrusion to develop midface growth following midface DO. Various studies evaluating facial growth in patients with craniofacial syndromes have reported minimal or absent horizontal and sagittal growth, while vertical growth seems to be preserved.32 33 34 49 56 57 58 Along the same lines, Fearon13 concludes that the absence of growth in this specific patient population is intrinsic to the disease process and not to the procedure performed. Thus, with regards to these findings, overcorrection and overdistraction in this subset of patients should be strongly considered. As mentioned previously, timing of the midface procedure should be bound to clear indications. For example, patients with severe obstructive sleep apnea (OSA), midface retrusion, and ocular proptosis benefit from a relatively early procedure, while patients with less severe symptoms and moderate class III malocclusion may benefit from these procedures at skeletal maturity.
Future Directions
As with any procedure that involves patient compliance, distraction may benefit from removal of the responsibility of “turning a screw” through the creation of a motor-driven, computer-controlled device. Inclusion of a wireless micromotor would eliminate concerns about compliance as well as potentially increase the accuracy of distraction. This would likely lead to an improved experience for families.
Improved engineering of devices will help minimize complications and improve outcomes. Smaller, less intrusive, internal devices would be better tolerated by patients. Smaller devices can be worn out of plain sight and impacts minimally the patient's daily activities. Ideally, these smaller internal devices would also allow for multidirectional adjustment of the distraction vector. Along those lines, resorbable devices have been introduced.36 37 CAD/CAM software can also be used for virtual surgical simulation of the procedure. Cutting and positioning guides improve the accuracy of the osteotomies and distractor placement, potentially improving the final aesthetic outcome of the reconstruction.59 60
Enhancement of bone biology–through growth factor manipulation, stem cell enrichment, or genetic manipulation—may shorten treatment regimens. Shortening the consolidation period would allow for an earlier removal of the distractors, allowing patients to return to their regular activities sooner. Significant research is currently underway evaluating various growth factors that will allow for a faster bony formation and consolidation.61 62 63 64 65 66
References
- 1.Tessier P. The classic reprint. Experimental study of fractures of the upper jaw. I and II. René Le Fort, M.D. Plast Reconstr Surg. 1972;50(5):497–506. doi: 10.1097/00006534-197211000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Tessier P. Syndrome de Crouzon, syndrome d'Apert: oxycéphalie, scaphocéphalies, turricéphalies. Ann Chir Plast. 1967;12(4):273–286. [PubMed] [Google Scholar]
- 3.Tessier P. Relationship of craniostenoses to craniofacial dysostoses, and to faciostenoses: a study with therapeutic implications. Plast Reconstr Surg. 1971;48(3):224–237. doi: 10.1097/00006534-197109000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Tessier P. Total osteotomy of the middle third of the face for faciostenosis or for sequelae of Le Fort 3 fractures. Plast Reconstr Surg. 1971;48(6):533–541. doi: 10.1097/00006534-197112000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Tessier P. The definitive plastic surgical treatment of the severe facial deformities of craniofacial dysostosis. Crouzon's and Apert's diseases. Plast Reconstr Surg. 1971;48(5):419–442. doi: 10.1097/00006534-197111000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Tessier P, Guiot G, Rougerie J, Delbet J P, Pastoriza J. Ostéotomies cranio-naso-orbito-faciales. Hypertelorism. Ann Chir Plast. 1967;12(2):103–118. [PubMed] [Google Scholar]
- 7.Gillies H, Harrison S H. Operative correction by osteotomy of recessed malar maxillary compound in a case of oxycephaly. Br J Plast Surg. 1950;3(2):123–127. doi: 10.1016/s0007-1226(50)80019-x. [DOI] [PubMed] [Google Scholar]
- 8.Gillies H, Millard R. Boston, MA: Little, Brown and Company; 1957. The Principles and Art of Plastic Surgery. [Google Scholar]
- 9.Cohen S R, Rutrick R E, Burstein F D. Distraction osteogenesis of the human craniofacial skeleton: initial experience with new distraction system. J Craniofac Surg. 1995;6(5):368–374. doi: 10.1097/00001665-199509000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Sándor G KB, Ylikontiola L P, Serlo W, Pirttiniemi P M, Carmichael R P. Midfacial distraction osteogenesis. Atlas Oral Maxillofac Surg Clin North Am. 2008;16(2):249–272. doi: 10.1016/j.cxom.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Cedars M G, Linck D L II, Chin M, Toth B A. Advancement of the midface using distraction techniques. Plast Reconstr Surg. 1999;103(2):429–441. doi: 10.1097/00006534-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Chin M Toth B A Le Fort III advancement with gradual distraction using internal devices Plast Reconstr Surg 19971004819–830., discussion 831–832 [DOI] [PubMed] [Google Scholar]
- 13.Fearon J A The Le Fort III osteotomy: to distract or not to distract? Plast Reconstr Surg 200110751091–1103., discussion 1104–1106 [DOI] [PubMed] [Google Scholar]
- 14.McCarthy J G, Stelnicki E J, Mehrara B J, Longaker M T. Distraction osteogenesis of the craniofacial skeleton. Plast Reconstr Surg. 2001;107(7):1812–1827. doi: 10.1097/00006534-200106000-00029. [DOI] [PubMed] [Google Scholar]
- 15.Phillips J H, George A K, Tompson B. Le Fort III osteotomy or distraction osteogenesis imperfecta: your choice. Plast Reconstr Surg. 2006;117(4):1255–1260. doi: 10.1097/01.prs.0000204865.97302.5c. [DOI] [PubMed] [Google Scholar]
- 16.Swennen G, Schliephake H, Dempf R, Schierle H, Malevez C. Craniofacial distraction osteogenesis: a review of the literature: Part 1: clinical studies. Int J Oral Maxillofac Surg. 2001;30(2):89–103. doi: 10.1054/ijom.2000.0033. [DOI] [PubMed] [Google Scholar]
- 17.Cheung L K, Lo J. Distraction of Le Fort II osteotomy by intraoral distractor: a case report. J Oral Maxillofac Surg. 2006;64(5):856–860. doi: 10.1016/j.joms.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 18.Fearon J A. Halo distraction of the Le Fort III in syndromic craniosynostosis: a long-term assessment. Plast Reconstr Surg. 2005;115(6):1524–1536. doi: 10.1097/01.prs.0000160271.08827.15. [DOI] [PubMed] [Google Scholar]
- 19.Iannetti G, Fadda T, Agrillo A, Poladas G, Iannetti G, Filiaci F. LeFort III advancement with and without osteogenesis distraction. J Craniofac Surg. 2006;17(3):536–543. doi: 10.1097/00001665-200605000-00025. [DOI] [PubMed] [Google Scholar]
- 20.McCarthy J G Schreiber J Karp N Thorne C H Grayson B H Lengthening the human mandible by gradual distraction Plast Reconstr Surg 19928911–8., discussion 9–10 [PubMed] [Google Scholar]
- 21.Gosain A K. Plastic Surgery Educational Foundation DATA Committee. Distraction osteogenesis of the craniofacial skeleton. Plast Reconstr Surg. 2001;107(1):278–280. doi: 10.1097/00006534-200101000-00050. [DOI] [PubMed] [Google Scholar]
- 22.Bradley J P, Gabbay J S, Taub P J. et al. Monobloc advancement by distraction osteogenesis decreases morbidity and relapse. Plast Reconstr Surg. 2006;118(7):1585–1597. doi: 10.1097/01.prs.0000233010.15984.4d. [DOI] [PubMed] [Google Scholar]
- 23.Mofid M M Manson P N Robertson B C Tufaro A P Elias J J Vander Kolk C A Craniofacial distraction osteogenesis: a review of 3278 cases Plast Reconstr Surg 200110851103–1114., discussion 1115–1117 [DOI] [PubMed] [Google Scholar]
- 24.Steinhäuser E W. Variations of Le Fort II osteotomies for correction of midfacial deformities. J Maxillofac Surg. 1980;8(4):258–265. doi: 10.1016/s0301-0503(80)80112-3. [DOI] [PubMed] [Google Scholar]
- 25.Paliga J T, Goldstein J A, Storm P B, Taylor J A. Monobloc minus Le Fort II for single-stage treatment of the Apert phenotype. J Craniofac Surg. 2013;24(4):1380–1382. [PubMed] [Google Scholar]
- 26.Watanabe K, Kuroda S, Takahashi T. et al. Segmental distraction osteogenesis with modified LeFort II osteotomy for a patient with craniosynostosis. Am J Orthod Dentofacial Orthop. 2012;142(5):698–709. doi: 10.1016/j.ajodo.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Nout E, Cesteleyn L LM, van der Wal K GH, van Adrichem L NA, Mathijssen I MJ, Wolvius E B. Advancement of the midface, from conventional Le Fort III osteotomy to Le Fort III distraction: review of the literature. Int J Oral Maxillofac Surg. 2008;37(9):781–789. doi: 10.1016/j.ijom.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 28.Fearon J A, Whitaker L A. Complications with facial advancement: a comparison between the Le Fort III and monobloc advancements. Plast Reconstr Surg. 1993;91(6):990–995. [PubMed] [Google Scholar]
- 29.Hopper R A, Kapadia H, Morton T. Normalizing facial ratios in apert syndrome patients with Le Fort II midface distraction and simultaneous zygomatic repositioning. Plast Reconstr Surg. 2013;132(1):129–140. doi: 10.1097/PRS.0b013e318290fa8a. [DOI] [PubMed] [Google Scholar]
- 30.Ranly D M Craniofacial growth Dent Clin North Am 2000443457–470., v [PubMed] [Google Scholar]
- 31.Posnick J C. The craniofacial dysostosis syndromes. Staging of reconstruction and management of secondary deformities. Clin Plast Surg. 1997;24(3):429–446. [PubMed] [Google Scholar]
- 32.Bachmayer D I, Ross R B, Munro I R. Maxillary growth following LeFort III advancement surgery in Crouzon, Apert, and Pfeiffer syndromes. Am J Orthod Dentofacial Orthop. 1986;90(5):420–430. doi: 10.1016/0889-5406(86)90007-7. [DOI] [PubMed] [Google Scholar]
- 33.Kreiborg S, Aduss H. Pre- and postsurgical facial growth in patients with Crouzon's and Apert's syndromes. Cleft Palate J. 1986;23 01:78–90. [PubMed] [Google Scholar]
- 34.Meazzini M C, Mazzoleni F, Caronni E, Bozzetti A. Le Fort III advancement osteotomy in the growing child affected by Crouzon's and Apert's syndromes: presurgical and postsurgical growth. J Craniofac Surg. 2005;16(3):369–377. doi: 10.1097/01.scs.0000157201.81438.31. [DOI] [PubMed] [Google Scholar]
- 35.Fearon J A Patel N Abstract 1: Treatment of the syndromic mid face with rigid external distraction Le Fort III: a long-term assessment at skeletal maturity Plast Reconstr Surg 2014133(4, Suppl)973 [Google Scholar]
- 36.Cohen S R, Holmes R E. Internal Le Fort III distraction with biodegradable devices. J Craniofac Surg. 2001;12(3):264–272. doi: 10.1097/00001665-200105000-00013. [DOI] [PubMed] [Google Scholar]
- 37.Burstein F D, Williams J K, Hudgins R. et al. Single-stage craniofacial distraction using resorbable devices. J Craniofac Surg. 2002;13(6):776–782. doi: 10.1097/00001665-200211000-00013. [DOI] [PubMed] [Google Scholar]
- 38.Polley J W Figueroa A A Management of severe maxillary deficiency in childhood and adolescence through distraction osteogenesis with an external, adjustable, rigid distraction device J Craniofac Surg 199783181–185., discussion 186 [DOI] [PubMed] [Google Scholar]
- 39.Gosain A K, Santoro T D, Havlik R J, Cohen S R, Holmes R E. Midface distraction following Le Fort III and monobloc osteotomies: problems and solutions. Plast Reconstr Surg. 2002;109(6):1797–1808. doi: 10.1097/00006534-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Freihofer H P Jr. Results after midface-osteotomies. J Maxillofac Surg. 1973;1(1):30–36. doi: 10.1016/s0301-0503(73)80009-8. [DOI] [PubMed] [Google Scholar]
- 41.Girotto J A Davidson J Wheatly M et al. Blindness as a complication of Le Fort osteotomies: role of atypical fracture patterns and distortion of the optic canal Plast Reconstr Surg 199810251409–1421., discussion 1422–1423 [DOI] [PubMed] [Google Scholar]
- 42.McCarthy J G La Trenta G S Breitbart A S Grayson B H Bookstein F L The Le Fort III advancement osteotomy in the child under 7 years of age Plast Reconstr Surg 1990864633–646., discussion 647–649 [PubMed] [Google Scholar]
- 43.Matsumoto K, Nakanishi H, Seike T, Koizumi Y, Hirabayashi S. Intracranial hemorrhage resulting from skull base fracture as a complication of Le Fort III osteotomy. J Craniofac Surg. 2003;14(4):545–548. doi: 10.1097/00001665-200307000-00029. [DOI] [PubMed] [Google Scholar]
- 44.Nout E, Wolvius E B, van Adrichem L N, Ongkosuwito E M, van der Wal K G. Complications in maxillary distraction using the RED II device: a retrospective analysis of 21 patients. Int J Oral Maxillofac Surg. 2006;35(10):897–902. doi: 10.1016/j.ijom.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 45.Holmes A D, Wright G W, Meara J G, Heggie A A, Probert T C. LeFort III internal distraction in syndromic craniosynostosis. J Craniofac Surg. 2002;13(2):262–272. doi: 10.1097/00001665-200203000-00014. [DOI] [PubMed] [Google Scholar]
- 46.Brown R, Higuera S, Boyd V, Taylor T, Hollier L H Jr. Intracranial migration of a halo pin during distraction osteogenesis for maxillary hypoplasia: case report and literature review. J Oral Maxillofac Surg. 2006;64(1):130–135. doi: 10.1016/j.joms.2005.09.021. [DOI] [PubMed] [Google Scholar]
- 47.Le B T, Eyre J M, Wehby M C, Wheatley M J. Intracranial migration of halo fixation pins: a complication of using an extraoral distraction device. Cleft Palate Craniofac J. 2001;38(4):401–404. doi: 10.1597/1545-1569_2001_038_0401_imohfp_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 48.Saltaji H, Altalibi M, Major M P. et al. Le Fort III distraction osteogenesis versus conventional Le Fort III osteotomy in correction of syndromic midfacial hypoplasia: a systematic review. J Oral Maxillofac Surg. 2014;72(5):959–972. doi: 10.1016/j.joms.2013.09.039. [DOI] [PubMed] [Google Scholar]
- 49.Shetye P R, Kapadia H, Grayson B H, McCarthy J G. A 10-year study of skeletal stability and growth of the midface following Le Fort III advancement in syndromic craniosynostosis. Plast Reconstr Surg. 2010;126(3):973–981. doi: 10.1097/PRS.0b013e3181e60502. [DOI] [PubMed] [Google Scholar]
- 50.Warren S M, Shetye P R, Obaid S I, Grayson B H, McCarthy J G. Long-term evaluation of midface position after Le Fort III advancement: a 20-plus-year follow-up. Plast Reconstr Surg. 2012;129(1):234–242. doi: 10.1097/PRS.0b013e3182362a2f. [DOI] [PubMed] [Google Scholar]
- 51.Shetye P R, Davidson E H, Sorkin M, Grayson B H, McCarthy J G. Evaluation of three surgical techniques for advancement of the midface in growing children with syndromic craniosynostosis. Plast Reconstr Surg. 2010;126(3):982–994. doi: 10.1097/PRS.0b013e3181e6051e. [DOI] [PubMed] [Google Scholar]
- 52.Iannetti G, Ramieri V, Pagnoni M, Fadda M T, Cascone P. Le Fort III external midface distraction: surgical outcomes and skeletal stability. J Craniofac Surg. 2012;23(3):896–900. doi: 10.1097/SCS.0b013e31824e2549. [DOI] [PubMed] [Google Scholar]
- 53.Figueroa A A Polley J W Friede H Ko E W Long-term skeletal stability after maxillary advancement with distraction osteogenesis using a rigid external distraction device in cleft maxillary deformities Plast Reconstr Surg 200411461382–1392., discussion 1393–1394 [DOI] [PubMed] [Google Scholar]
- 54.Chin M Toth B A Distraction osteogenesis in maxillofacial surgery using internal devices: review of five cases J Oral Maxillofac Surg 199654145–53., discussion 54 [DOI] [PubMed] [Google Scholar]
- 55.Fearon J A. Le Fort III osteotomy or distraction osteogenesis imperfecta. Plast Reconstr Surg. 2007;119(3):1122–1123. doi: 10.1097/01.prs.0000253444.32346.6d. [DOI] [PubMed] [Google Scholar]
- 56.David D J, Sheen R. Surgical correction of Crouzon syndrome. Plast Reconstr Surg. 1990;85(3):344–354. doi: 10.1097/00006534-199003000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Epker B N, Wolford L M. Middle-third facial osteotomies: their use in the correction of congenital dentofacial and craniofacial deformities. J Oral Surg. 1976;34(4):324–342. [PubMed] [Google Scholar]
- 58.Kaban L B, Conover M, Mulliken J B. Midface position after Le Fort III advancement: a long-term follow-up study. Cleft Palate J. 1986;23 01:75–77. [PubMed] [Google Scholar]
- 59.Seruya M, Borsuk D E, Khalifian S, Carson B S, Dalesio N M, Dorafshar A H. Computer-aided design and manufacturing in craniosynostosis surgery. J Craniofac Surg. 2013;24(4):1100–1105. doi: 10.1097/SCS.0b013e31828b7021. [DOI] [PubMed] [Google Scholar]
- 60.Mommaerts M Y, Jans G, Vander Sloten J, Staels P F, Van der Perre G, Gobin R. On the assets of CAD planning for craniosynostosis surgery. J Craniofac Surg. 2001;12(6):547–554. doi: 10.1097/00001665-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 61.Makhdom A M, Hamdy R C. The role of growth factors on acceleration of bone regeneration during distraction osteogenesis. Tissue Eng Part B Rev. 2013;19(5):442–453. doi: 10.1089/ten.TEB.2012.0717. [DOI] [PubMed] [Google Scholar]
- 62.Farberg A S, Sarhaddi D, Donneys A, Deshpande S S, Buchman S R. Deferoxamine enhances bone regeneration in mandibular distraction osteogenesis. Plast Reconstr Surg. 2014;133(3):666–671. doi: 10.1097/01.prs.0000438050.36881.a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Donneys A, Deshpande S S, Tchanque-Fossuo C N. et al. Deferoxamine expedites consolidation during mandibular distraction osteogenesis. Bone. 2013;55(2):384–390. doi: 10.1016/j.bone.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wu G P, He X C, Hu C B, Li D P, Yang Z H, Guo L. Effect of electroporation-mediated transfecting recombinant plasmid pIRES-hBMP2-hVEGF165 on mandibular distraction osteogenesis. Ann Plast Surg. 2012;69(3):316–325. doi: 10.1097/SAP.0b013e3182119275. [DOI] [PubMed] [Google Scholar]
- 65.Eguchi Y, Wakitani S, Naka Y, Nakamura H, Takaoka K. An injectable composite material containing bone morphogenetic protein-2 shortens the period of distraction osteogenesis in vivo. J Orthop Res. 2011;29(3):452–456. doi: 10.1002/jor.21225. [DOI] [PubMed] [Google Scholar]
- 66.Sailhan F, Gleyzolle B, Parot R, Guerini H, Viguier E. Rh-BMP-2 in distraction osteogenesis: dose effect and premature consolidation. Injury. 2010;41(7):680–686. doi: 10.1016/j.injury.2009.10.010. [DOI] [PubMed] [Google Scholar]


