Abstract
Background/Aims
Amiodarone is one of the most widely used antiarrhythmic agents; however, amiodarone-induced pulmonary toxicity (APT) can be irreversible and sometimes fatal. The aim of this study was to evaluate the feasibility of chest computed tomography (CT) as a diagnostic tool for APT and to assess the utility of the CT APT score as an index for predicting the severity of APT.
Methods
Patients underwent amiodarone treatment for various reasons, most often atrial fibrillation, for more than 2 years, and those that received a cumulative dose > 100 g were enrolled. A total of 34 patients who underwent chest CT between December 2011 and June 2012 were enrolled, whether or not they had clinical symptoms. The APT CT score was defined as the number of involved regions in the lung, which was divided into 18 regions (right and left, upper, middle, and lower, and central, middle, and peripheral). The CT findings were evaluated according to the total dose and duration of amiodarone treatment and the results of a pulmonary function test. Clinical symptoms and outcomes were also evaluated according to APT CT scores.
Results
Seven patients had positive APT CT scores (interstitial fibrosis in five, organizing pneumonia in one, and mixed interstitial fibrosis and organizing pneumonia in one), and these patients exhibited significantly lower diffusion capacity for carbon monoxide in the lungs compared with patients without an increased APT CT score (70.2% ± 6.9% vs. 89.7% ± 19.4%; p = 0.011). Three of the seven patients experienced overt APT that required hospital admission.
Conclusions
Chest CT is a useful diagnostic tool for APT, and the APT CT score might be a useful index for assessing the severity of APT.
Keywords: Amiodarone, Pulmonary toxicity, Computed tomography, Cumulative dose
INTRODUCTION
Amiodarone is one of the most widely used antiarrhythmic agents; however, amiodarone-induced pulmonary toxicity (APT) can be irreversible and sometimes fatal [1]. Furthermore, the long half-life and lipophilic nature of amiodarone, as well as its tendency to accumulate in various tissues, make it challenging to predict toxicity [1,2].
The intracellular accumulation of phospholipids and T cell-mediated hypersensitivity are potential mechanisms of APT [2,3,4]. Chest computed tomography (CT) findings related to amiodarone exposure are well defined and include lung parenchymal changes, septal thickening, interstitial fibrosis, high attenuation pleuroparenchymal opacities, and interstitial or alveolar opacities [2,5,6,7]. These findings, unlike other drug-induced pulmonary changes, often present with asymmetric patterns, whether diffuse or patchy infiltration [6]. Although APT-related CT findings have been described, the relationship between the extent of these abnormal findings and the diagnosis or severity of APT remain unclear.
Several studies have assessed the effects of amiodarone cumulative total doses [8,9]. The long-term use of low maintenance doses of amiodarone can reach a high total cumulative dose as high as 101 to 151 g, which was associated with a significantly increased risk of APT (odds ratio [OR], 10.29); however, this risk reached a plateau at cumulative doses > 150 mg (OR, 9.5) [9].
The aim of the current study was to evaluate the utility of chest CT as a diagnostic tool for APT in chronic amiodarone users, particularly in individuals prescribed lower maintenance doses that result in a high total cumulative dose. In addition, we also assessed the usefulness of the CT APT score, a surrogate for the extent of APT, as an index for predicting the severity of APT.
METHODS
Study population
This was a cross-sectional cohort study with a 1-year prospective follow-up. Patient medical records were reviewed retrospectively, and 1-year outcomes were observed prospectively after discontinuing amiodarone therapy. Patients who had been treated with amiodarone for > 2 years with a total cumulative dose > 100 g were enrolled based on information in the medical database between January 2000 to October 2011. A total of 65 patients were eligible for inclusion in the study. Patients who had no available medical records within the last 2 years (due to transfer to another hospital or lack of follow-up, n = 11), who could not discontinue amiodarone treatment (due to aggravation of underlying heart disease, n = 1), and who did not agree to inclusion in the study (n = 9) were excluded.
A total of 44 patients provided oral informed consent and were recruited into the study. They underwent chest CT between December 2011 and June 2012, whether they were symptomatic or asymptomatic. Patients with a medical history of chronic obstructive lung disease (COPD), interstitial lung disease, preexisting lung disease, or those with no known medical history of bronchiectasis but in whom lesions were evident on chest X-ray were excluded. The total cumulative amiodarone doses were calculated from the medical records. Seven of the 44 patients were excluded because their actual cumulative dose or the period of amiodarone treatment did not satisfy the enrollment criteria, and three patients were excluded due to preexisting lung disease (bronchiectasis, emphysema, and chronic bronchitis, respectively). Therefore, a total 34 patients were entered into the final analysis. All individuals discontinued amiodarone within 1 week of the chest CT and had been followed up for 1 year without taking amiodarone. This study was approved by the Institutional Review Board of Ewha Medical Center (IRB No. ECT 12-17A-22). Patients were enrolled after providing oral informed consent.
Computed tomography
All CT scans were assessed for the presence of APT, and an experienced radiologist (YK, 17 years of experience in chest CT) analyzed the CT patterns of APT. The CT findings were pulmonary lesions defined as follows: (1) pulmonary interstitial fibrosis besides bronchiectasis, pleural thickening, stable pulmonary tuberculosis, and linear atelectasis related to other lung problems; (2) pulmonary consolidation or ground-glass opacity that was not related to any etiology other than a medical history of amiodarone use; (3) pulmonary lesions with a high CT-attenuation not related to the calcification of another pulmonary disease.
The APT CT score was calculated for each patient by counting the number of involved regions in the lung, which was divided into 18 regions (right and left, upper, middle, and lower, and central, middle, and peripheral). Both lungs were divided into three regions in the craniocaudal direction: upper, above the carina; middle, between the carina and the inferior pulmonary vein; lower, below the inferior pulmonary vein. Each region was then divided into central, middle, and peripheral thirds. Therefore, the maximum APT CT score was 18, and the minimum APT CT score was 0. When different types of pulmonary lesions existed in the same region, that region was counted as "1," regardless of the number of types of pulmonary lesions (more detailed examples are presented in Figs. 1 and 2). For example, the presence of both pulmonary interstitial fibrosis and pulmonary consolidation in the right middle central region would be counted as 1.
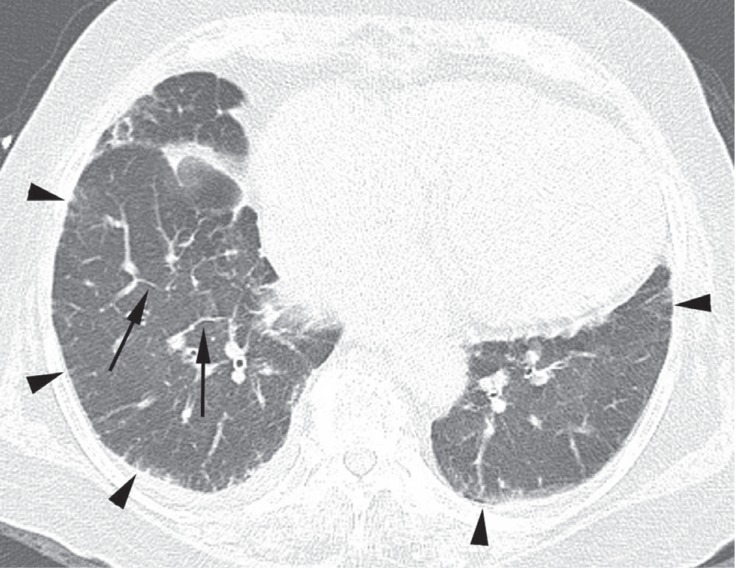
Figure 1.
A 74-year-old female with amiodarone pulmonary toxicity (APT) exhibiting a pulmonary interstitial fibrosis pattern. Computed tomography (CT) scans obtained at the level of both lower lobes revealed intralobular and interlobular septal thickenings in the peripheral regions of both lower lobes (arrowheads), and interlobular septal thickenings in the central and middle regions of the right lower lobe (arrows). The APT CT score was 4 on this CT section; the involved regions included the central, middle, and peripheral regions.
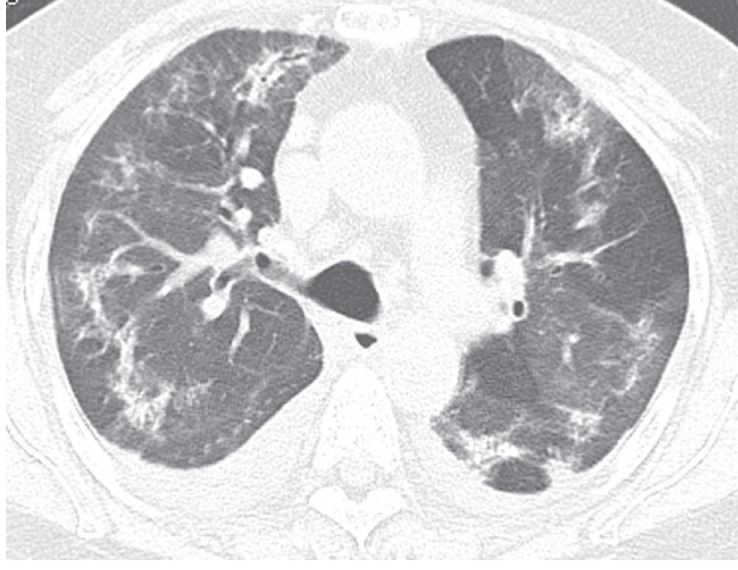
Figure 2.
A 62-year-old female with amiodarone pulmonary toxicity (APT) exhibiting an organizing pneumonia pattern. A computed tomography (CT) scan obtained at the level of both upper lobes revealed bilateral patchy consolidations and ground-glass opacities. Also noted were small bilateral pleural effusions. The APT CT score was 6, and the involved regions included the right and left upper lungs in the central, middle, and peripheral regions.
Overt APT was defined when the individuals had a positive APT CT score and required hospital treatment due to clinical symptoms and/or respiratory failure related to amiodarone use. Clinical symptoms included cough, dyspnea, and/or fever.
Statistical analysis
The baseline characteristics of the subjects were compared using chi-square tests for categorical variables and Student t tests for continuous variables. Continuous variables were expressed as means ± SD. Spearman's correlation analyses were performed to assess the correlation between variables. In addition, a forward stepwise logistic regression model was applied to identify variables related to the APT CT score. A value of p < 0.05 was used to define statistical significance, and all statistical analyses were performed using SPSS version 19.0 (IBM Co., Armonk, NY, USA).
RESULTS
The most common reason for amiodarone treatment in the study population was atrial fibrillation (AF): (1) AF alone (n = 21); (2) AF with valvular heart disease (n = 10); (3) AF and a medical history of aborted sudden cardiac death related to acute myocardial infarction (n = 2); (4) AF with ischemic heart disease (n = 1); and (5) supraventricular tachycardia with ischemic heart disease (n = 1). The mean age of the 34 subjects was 67.3 ± 10.5 years, and 64.2% were female. The mean starting dose of amiodarone was 314.7 ± 135.1 mg, and the mean total cumulative dose was 408.4 ± 221.1 g over ~5.87 years (Table 1). Eleven patients (32.4%) had clinical symptoms such as cough (14.7%), fever (5.9%), and dyspnea (26.5%), and 11.8% of patients had more than two symptoms.
Table 1.
Baseline characteristics of the study population (n = 34)
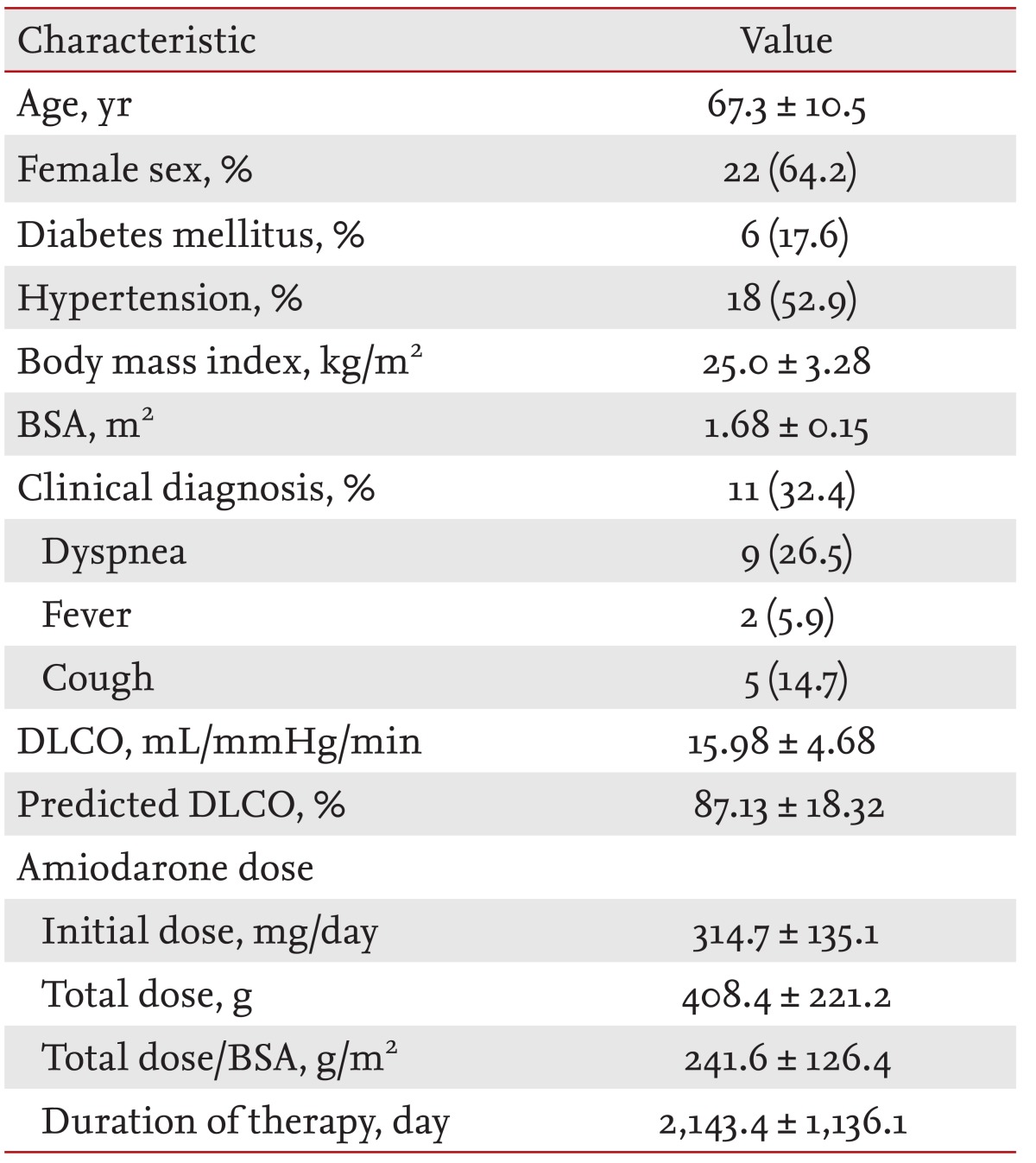
Values are presented as mean ± SD or number (%).
BSA, body surface area; DLCO, diffusion capacity for carbon monoxide of the lungs.
Seven patients had positive APT findings on CT scans. The CT pattern was a pulmonary interstitial fibrosis pattern of interlobular and intralobular septal thickenings predominantly involving the lower lungs in five patients (Fig. 1), an organizing pneumonia pattern of consolidation and ground-glass opacity in one patient (Fig. 2), and a mixed pattern of pulmonary interstitial fibrosis and organizing pneumonia in one patient (Fig. 3).
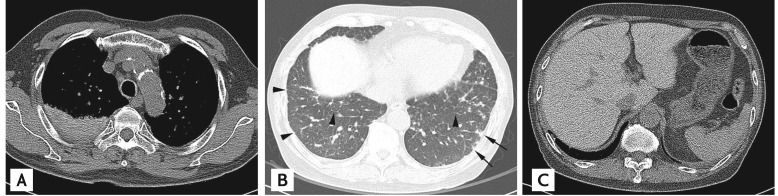
Figure 3.
A 65-year-old male with amiodarone pulmonary toxicity (APT) exhibiting a mixed organizing pneumonia and interstitial fibrosis pattern. (A) A computed tomography (CT) scan obtained without intravenous contrast injection revealed consolidation in the posterior segment of the right upper lobe, which exhibited high CT-attenuation compared with the muscles of the thorax. (B) A CT scan at the level of both lower lobes showed interlobular septal thickenings in both lower lobes (arrowheads) and small subpleural consolidations in the left lower lobe (arrows). (C) In the upper abdomen, the liver showed a diffuse high attenuation, which is a characteristic CT finding of APT caused by iodine accumulation in the liver.
The APT CT scores, clinical manifestations, chest radiographical, and CT findings of all patients are summarized in Table 2. Cases 1 to 3 had APT CT scores < 5, no symptoms, and no overt APT during the 1-year follow-up period. Case 3 had suspected APT, both on a chest X-ray and chest CT, but had no symptoms and did not experience APT. These patients were treated for septic shock that was unrelated to amiodarone. An APT CT score of 9 to 16 was observed in four patients, three of whom were admitted to the hospital for treatment of overt APT. Cases six (Fig. 3) and seven (Fig. 2), who showed an organizing pneumonia pattern, experienced acute respiratory failure that required ventilator care. Two of the three patients recovered completely after the discontinuation of amiodarone and medical treatment, but one patient died.
Table 2.
Summary of the seven positive amiodarone-induced pulmonary toxicity computed tomography score patients
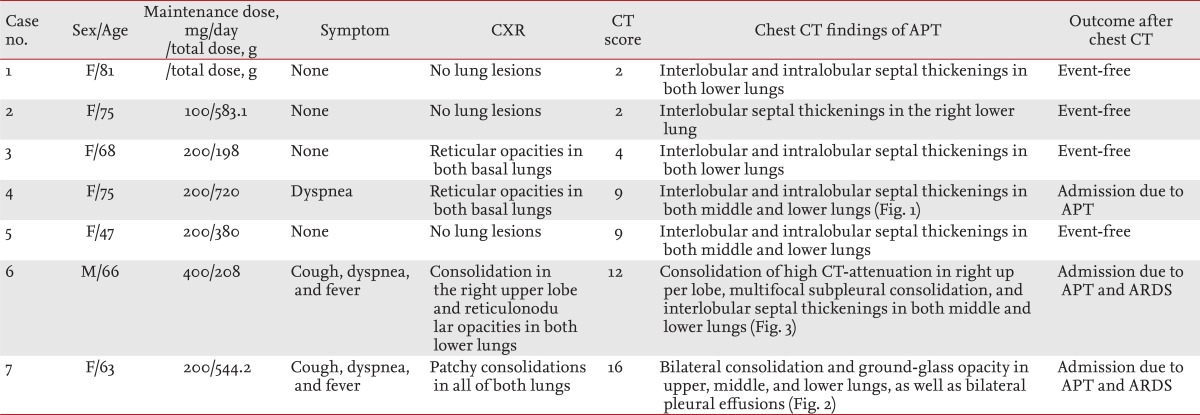
CXR, chest X-ray; CT, computed tomography; APT, amiodarone-induced pulmonary toxicity; ARDS, acute respiratory distress syndrome.
Overt APT was not evident in patients with negative APT CT scores. During follow-up, three minor events of supraventricular tachycardia, one morbidity of nonwitnessed outside hospital sudden cardiovascular collapse, and one unrelated minor event of community-acquired pneumonia occurred in the patients with negative APT CT scores. After the discontinuation of amiodarone, there were no newly developed instances of APT or APT relapse in any of the 34 patients during the 1-year follow-up.
The subjects were further divided into two groups according to positive and negative APT CT scores (PCT and NCT, respectively). There were no differences in age, gender, and medical history between the groups. Amiodarone-related variables, such as initial dose, total cumulative dose, and the duration of administration, were also comparable between groups (Table 3). The PCT group had a lower diffusion capacity for carbon monoxide in the lungs (DLCO) and less body surface area (BSA) than did the NCT group. In addition, the APT CT score was correlated negatively with BSA according to a forward stepwise logistic regression model (95% confidence interval, -2.075 to -0.263; p = 0.013).
Table 3.
Comparisons according to the computed tomography score
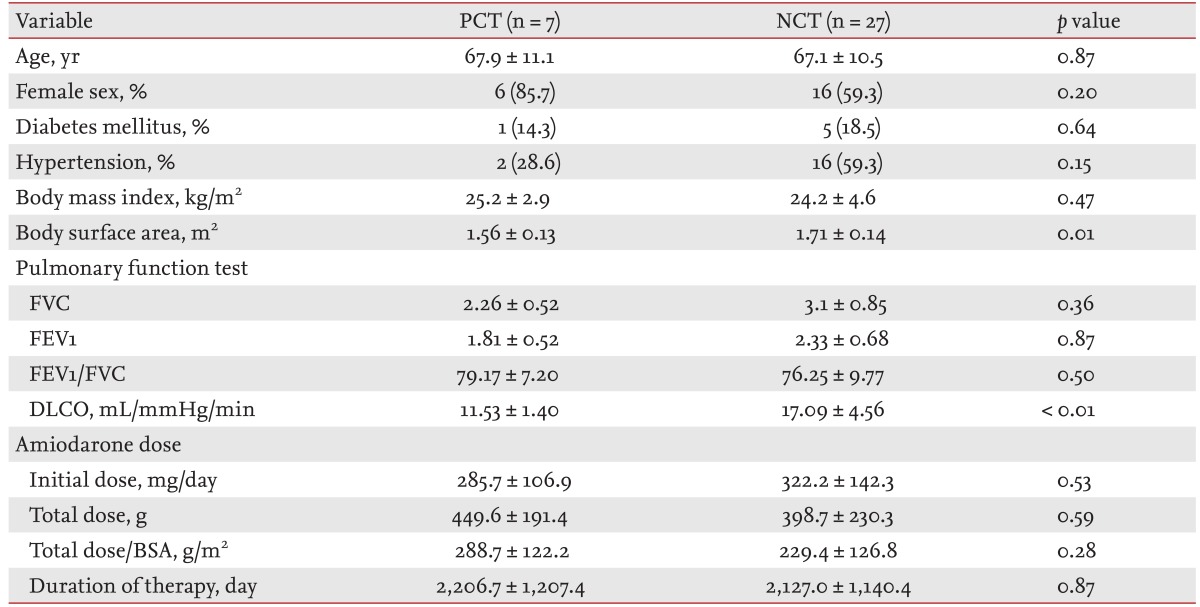
Values are presented as mean ± SD or number (%).
PCT, positive amiodarone-induced pulmonary toxicity (APT) computed tomography (CT) score; NCT, negative APT CT score; BSA, body surface area; FVC, forced vital capacity; FEV1, forced expiratory volume in 1 second; DLCO, diffusion capacity for carbon monoxide in the lungs.
DISCUSSION
The prevalence of APT is ~5% [6,10], with an annual incidence of ~2% [11]. The current study showed that the incidence of overt APT was 8.8%; however, this might be exaggerated due to the excluded patients. A Japanese study reported that the 1-, 3-, and 5-year cumulative incidences of APT in amiodarone users on a 141-mg maintenance dose were 4.2%, 7.8%, and 10.6%, respectively [12]. This is consistent with the current observations.
APT is diagnosed by exclusion, and diagnoses may be based on existing findings or clinical symptoms (cough or dyspnea), particularly by the presence of local or diffuse opacities on chest CT and a decrease in DLCO from baseline [1]. However, there is no consensus on whether APT can be diagnosed only using symptoms, pulmonary function tests (PFT), chest CT, or pathology. Therefore, there are no pathognomonic findings regarding chest CT and APT.
The general guidelines for APT recommend performing baseline and surveillance of PFT, as well as chest X-rays [6,11]. However, these recommendations are not always followed in real-world practice. The results of a cross-sectional retrospective study in a large tertiary-care hospital revealed that only 52% of patients underwent baseline PFT, and 60% underwent both chest X-ray and PFT surveillance [11]. The current results showed that PCT subjects also had a decreased DLCO compared with NCT subjects, although baseline DLCO data were not available.
Chest CT could be useful for differential diagnosis when no baseline data for PFT and/or chest X-ray are available, or in the presence of underlying pulmonary diseases such as COPD. The clinical symptoms for APT are nonspecific [7,10]. Our data also revealed no difference in clinical symptoms between the two groups (p = 0.66, data not shown), and clinical symptoms presented regardless of APT. However, all three patients who were diagnosed with overt APT had clinical symptoms. Therefore, a positive APT CT score and the presence of clinical symptoms might be helpful for the diagnosis of APT in long-term amiodarone users. In particular, a high APT CT score such as ≥ 9 could be related to severe APT that requires hospital admission. Other patients with positive ATP CT scores but no symptoms or clinical events were not diagnosed with APT; therefore, no treatment was considered.
There are two major hypotheses regarding APT: immune-mediated hypersensitivity and the direct cytotoxicity of drug-induced phospholipidosis [6,13]. Moreover, amiodarone has several pharmacological properties that contribute to its toxicities [2,14], including the presence of two iodine atoms that result in the release of 7 mg iodine per 200 mg amiodarone (normal iodine intake, 150 to 200 µg/day), its lipophilic nature and high affinity for tissue accumulation, long half-life, and a large distribution volume. Consequently, amiodarone accumulates in fatty tissue, the liver, and lungs in chronic users, which leads to drug-induced direct organ toxicities. Iodine is highly attenuated on CT; therefore, the high attenuation of these organs on nonenhanced CT might represent iodine accumulation in the lungs and/or liver of chronic amiodarone users [6]. Increased lung attenuation seems to present in more advanced APT cases [7]. Case six in the current study showed characteristic high attenuation on nonenhanced CT in both the liver and lungs, which suggested iodine accumulation related to chronic amiodarone use (Fig. 3A and 3C).
When a long-term amiodarone user with a cumulative dose > 100 g presents with newly developed symptoms, it is necessary to evaluate not only chest X-ray and PFT, but also chest CT. Cases six and seven experienced acute respiratory failure that required ventilator support. Both patients exhibited organized pneumonia patterns on chest CT, and their APT CT scores were 12 and 16, respectively. If the APT CT score is ≥ 9, the patient should be assessed and managed according to the possibility of severe APT and respiratory failure.
There are several known risk factors for APT, including old age, duration of amiodarone therapy and a high cumulative dose, pre-existing lung disease, and high oxygen therapy [6,15,16]. In the current study, the two groups were similar in age, which might be due to the small number of patients, or age might not be a significant risk factor in long-term amiodarone users who have reached a high cumulative dose. However, there are no published data available regarding this specific situation.
In addition, the current study showed no significant differences according to the duration of treatment and cumulative dose between the two groups. This might be because our study population included only patients with a cumulative dose > 100 g and total treatment periods > 2 years. The total cumulative doses in the PCT and NCT groups were 449.6 and 398.7 g, respectively; the mean dose was higher in the PCT group, but not significantly (p = 0.59). BSA showed an inverse relationship with a positive APT CT score (p = 0.013), and patients in the PCT group had a higher total dose/BSA compared with the NCT group (288.7 g/m2 vs. 229.4 g/m2), but not significantly. Therefore, this should be investigated further. In addition, a previous report [9] suggested that the risk of APT might plateau at very high cumulative doses > 150 g. However, another study revealed a significantly increased risk of ATP when the cumulative dose reached 140 to 230 g [8].
All patients had discontinued amiodarone ~1 week before the chest CT, and some were prescribed other antiarrhythmic agents as a substitute. All subjects were followed for at least 1 year after discontinuation of amiodarone. Some studies reported that the recurrence of APT after discontinuing amiodarone was related to the rapid tapering of steroids [6]. Nevertheless, our data did not reveal newly developed or recurrent APT. Two patients who received hospital treatment due to overt APT also did not show recurrent APT or additional lung problems during the follow-up period.
There are some limitations to our study. It had a small subject number and was a single-center study. Therefore, the results cannot be generalized. In addition, baseline PFT data were not available. We performed 1-year follow-up by prospective observation, and chest CTs were not repeated routinely. Therefore, we could not evaluate the reversibility of chest CT lesions in patients with positive APT CT scores without overt APT after discontinuing amiodarone. Consequently, the meaning of APT CT scores < 5 not associated with overt APT could not be assessed.
In conclusion, the APT CT score might be helpful for the assessment and management of APT in symptomatic long-term amiodarone users. Chest CT has value for differential diagnosis, and a high APT CT score might be related to pulmonary insufficiency and rapid progression of respiratory failure. There was little evidence to suggest new development or recurrence of APT after discontinuing amiodarone.
KEY MESSAGE
Computed tomography (CT) score is helpful in assessment and management of amiodarone-induced pulmonary toxicity (APT) for symptomatic long term amiodarone user.
Especially, high APT CT score may be related with pulmonary insufficiency and rapid progress of respiratory failure.
There was little evidence of new development or recurrence of APT after discontinuing amiodarone.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Goldschlager N, Epstein AE, Naccarelli GV, et al. A practical guide for clinicians who treat patients with amiodarone: 2007. Heart Rhythm. 2007;4:1250–1259. doi: 10.1016/j.hrthm.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 2.van Erven L, Schalij MJ. Amiodarone: an effective antiarrhythmic drug with unusual side effects. Heart. 2010;96:1593–1600. doi: 10.1136/hrt.2008.152652. [DOI] [PubMed] [Google Scholar]
- 3.Camus P, Fanton A, Bonniaud P, Camus C, Foucher P. Interstitial lung disease induced by drugs and radiation. Respiration. 2004;71:301–326. doi: 10.1159/000079633. [DOI] [PubMed] [Google Scholar]
- 4.Pitcher WD. Amiodarone pulmonary toxicity. Am J Med Sci. 1992;303:206–212. doi: 10.1097/00000441-199203000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Chai JL, Patz EF., Jr CT of the lung: patterns of calcification and other high-attenuation abnormalities. AJR Am J Roentgenol. 1994;162:1063–1066. doi: 10.2214/ajr.162.5.8165982. [DOI] [PubMed] [Google Scholar]
- 6.Schwaiblmair M, Berghaus T, Haeckel T, Wagner T, von Scheidt W. Amiodarone-induced pulmonary toxicity: an under-recognized and severe adverse effect? Clin Res Cardiol. 2010;99:693–700. doi: 10.1007/s00392-010-0181-3. [DOI] [PubMed] [Google Scholar]
- 7.Siniakowicz RM, Narula D, Suster B, Steinberg JS. Diagnosis of amiodarone pulmonary toxicity with high-resolution computerized tomographic scan. J Cardiovasc Electrophysiol. 2001;12:431–436. doi: 10.1046/j.1540-8167.2001.00431.x. [DOI] [PubMed] [Google Scholar]
- 8.Ashrafian H, Davey P. Is amiodarone an underrecognized cause of acute respiratory failure in the ICU? Chest. 2001;120:275–282. doi: 10.1378/chest.120.1.275. [DOI] [PubMed] [Google Scholar]
- 9.Ernawati DK, Stafford L, Hughes JD. Amiodarone-induced pulmonary toxicity. Br J Clin Pharmacol. 2008;66:82–87. doi: 10.1111/j.1365-2125.2008.03177.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dusman RE, Stanton MS, Miles WM, et al. Clinical features of amiodarone-induced pulmonary toxicity. Circulation. 1990;82:51–59. doi: 10.1161/01.cir.82.1.51. [DOI] [PubMed] [Google Scholar]
- 11.Stelfox HT, Ahmed SB, Fiskio J, Bates DW. Monitoring amiodarone's toxicities: recommendations, evidence, and clinical practice. Clin Pharmacol Ther. 2004;75:110–122. doi: 10.1016/j.clpt.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Yamada Y, Shiga T, Matsuda N, Hagiwara N, Kasanuki H. Incidence and predictors of pulmonary toxicity in Japanese patients receiving low-dose amiodarone. Circ J. 2007;71:1610–1616. doi: 10.1253/circj.71.1610. [DOI] [PubMed] [Google Scholar]
- 13.Tanawuttiwat T, Harindhanavudhi T, Hanif S, Sahloul MZ. Amiodarone-induced alveolar haemorrhage: a rare complication of a common medication. Heart Lung Circ. 2010;19:435–437. doi: 10.1016/j.hlc.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Mackenzie C, Syed J, Pollak PT, Koren G. Falling between the cracks: a case of amiodarone toxicity. CMAJ. 2011;183:1393–1397. doi: 10.1503/cmaj.100351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Papiris SA, Triantafillidou C, Kolilekas L, Markoulaki D, Manali ED. Amiodarone: review of pulmonary effects and toxicity. Drug Saf. 2010;33:539–558. doi: 10.2165/11532320-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 16.Nacca N, Bhamidipati CM, Yuhico LS, Pinnamaneni S, Szombathy T. Severe amiodarone induced pulmonary toxicity. J Thorac Dis. 2012;4:667–670. doi: 10.3978/j.issn.2072-1439.2012.06.08. [DOI] [PMC free article] [PubMed] [Google Scholar]