Abstract
Background
Mortality from external causes, of all kinds, is an important component of overall mortality on a global basis. However, these deaths, like others in Africa and Asia, are often not counted or documented on an individual basis. Overviews of the state of external cause mortality in Africa and Asia are therefore based on uncertain information. The INDEPTH Network maintains longitudinal surveillance, including cause of death, at population sites across Africa and Asia, which offers important opportunities to document external cause mortality at the population level across a range of settings.
Objective
To describe patterns of mortality from external causes at INDEPTH Network sites across Africa and Asia, according to the WHO 2012 verbal autopsy (VA) cause categories.
Design
All deaths at INDEPTH sites are routinely registered and followed up with VA interviews. For this study, VA archives were transformed into the WHO 2012 VA standard format and processed using the InterVA-4 model to assign cause of death. Routine surveillance data also provide person-time denominators for mortality rates.
Results
A total of 5,884 deaths due to external causes were documented over 11,828,253 person-years. Approximately one-quarter of those deaths were to children younger than 15 years. Causes of death were dominated by childhood drowning in Bangladesh, and by transport-related deaths and intentional injuries elsewhere. Detailed mortality rates are presented by cause of death, age group, and sex.
Conclusions
The patterns of external cause mortality found here generally corresponded with expectations and other sources of information, but they fill some important gaps in population-based mortality data. They provide an important source of information to inform potentially preventive intervention designs.
Keywords: external causes, accidents, suicide, assault, transport, drowning, Africa, Asia, mortality, INDEPTH Network, verbal autopsy, InterVA
Mortality from external causes – whether unintentional (such as transport-related, falls, drowning, fires and burns, venoms, and poisons) or intentional (suicides and assaults) – forms a worldwide phenomenon of considerable magnitude. Which cause categories dominate in particular places and which age-sex groups are most affected in particular populations vary widely. Fatalities due to external causes also present a non-trivial measurement issue, since instantaneous deaths in many settings are dealt with differently (e.g. by police and other authorities) as compared to deaths during or following medical treatment for injuries (typically in hospitals).
The Global Status Report on Road Safety 2013 (1) reports over 1 million people killed on the world's roads annually, with numbers rising in some countries. Despite technological improvements in vehicles and roads, increasing traffic density can bring increased risks, particularly to pedestrians. The World Health Organization (WHO) African Region is estimated to have the highest rate of road traffic deaths, at 0.24 per 1,000 population, with the South-East Asia Region at 0.18 per 1,000 population.
Child injuries have also been documented globally in the World Report on Child Injury Prevention (2). Globally, child injury deaths number close to one million per year, with the majority occurring in low- and middle-income countries. Leading cause categories are road traffic and drowning.
A review of data on suicide in Africa showed major gaps, making estimates of overall patterns uncertain (3). Published rates from various African countries ranged from 0.004 to 0.17 per 1,000 population. A global analysis of suicide estimated a rate of 0.06 per 1,000 in the WHO African Region and 0.16 in the WHO South-East Asia Region (4). The same source estimated rates for violence and war at 0.23 per 1,000 population in Africa and 0.08 per 1,000 in South-East Asia.
The INDEPTH Network works with Health and Demographic Surveillance Sites (HDSS) across Africa and Asia, which each follow circumscribed populations on a longitudinal basis. Core data collected include person-time at risk, together with deaths and, by means of verbal autopsy (VA), assessment of cause of death (5). This allows reporting of external cause mortality on the basis of individually documented deaths within defined populations, adding considerably to existing overall estimates, which are often based on health facility data.
Our aim in this article is to document deaths among entire populations in a dataset from 22 INDEPTH HDSSs covering Africa and Asia, looking particularly at those deaths attributable to external causes. We define external causes here to include all of the WHO 2012 VA standard chapter 12 causes, corresponding to ICD-10 codes S00 to Y98 (6). Although these 22 sites are not designed to be a representative sample, they enable comparisons to be made over widely differing situations, using standardised methods.
Methods
The overall INDEPTH data set from which these analyses of external cause mortality are drawn is described in detail elsewhere (7). Across the 22 participating sites (8–29) , there is documentation on 111,910 deaths in 12,204,043 person-years of observation. These data are available in a public-domain data set (30), and the methods used to compile that data set are summarised in Box 1.
Age–sex–time standardisation
To avoid effects of differences and changes in age-sex structures of populations, mortality fractions and rates have been adjusted using the INDEPTH 2013 population standard (31). A weighting factor was calculated for each site, age group, sex, and year category in relation to the standard for the corresponding age group and sex, and incorporated into the overall data set. This is referred to in this article as age-sex-time standardisation in the contexts where it is used.
Cause of death assignment
The InterVA-4 (version 4.02) probabilistic model was used for all of the cause-of-death assignments in the overall data set (32). InterVA-4 is fully compliant with the WHO 2012 Verbal Autopsy (VA) standard and generates causes of death categorised by ICD-10 groups (33). The data reported here were collected before the WHO 2012 VA standard was available, but were transformed into the WHO2012 and InterVA-4 format to optimise cross-site standardisation in cause-of-death attribution. For a small proportion of deaths, VA interviews were not successfully completed; a few others contained inadequate information to arrive at a cause of death. InterVA-4 assigns causes of death (a maximum of three) with associated likelihoods; thus, cases for which likely causes did not total 100% were also assigned a residual indeterminate component. This served as a means of encapsulating uncertainty in cause of death at the individual level within the overall data set, as well as accounting for 100% of every death.
Overall dataset
The overall public-domain data set (30) thus contains between one and four records for each death, with the sum of likelihoods for each individual being unity. Each record includes a specific cause of death, its likelihood, and its age-sex-time weighting.
Box 1. Summary of methodology based on the detailed description in the introductory paper (7)
Deaths assigned to any of the WHO 2012 VA cause-of-death categories relating to external causes (VA12.01 to VA12.99) were extracted from the overall database, together with details of site, age group at death, and sex. Person-year denominators corresponding to the same categories were included from the corresponding surveillance data.
Of the 22 sites reported in the data set, two (FilaBavi, Vietnam; Niakhar, Senegal) reported very few deaths due to external causes, accompanied by little specific information as to cause of death. These did not provide a credible picture of mortality from external causes, and consequently the following analyses are based on data from the remaining 20 sites, relating to 5,884 deaths over 11,828,253 person-years observed. The Karonga, Malawi, site did not contribute VAs for children. Sites reported for different time periods; overall, 5.0% of the person-time observed occurred before 2000, 28.2% from 2000 to 2005, and 66.7% from 2006 to 2012. As each HDSS covers a total population, rather than a sample, uncertainty intervals are not shown.
In this context, all of these data are secondary data sets derived from primary data collected separately by each participating site. In all cases, the primary data collection was covered by site-level ethical approvals relating to ongoing health and demographic surveillance in those specific locations. No individual identity or household location data were included in the secondary data, and no specific ethical approvals were required for these pooled analyses.
Results
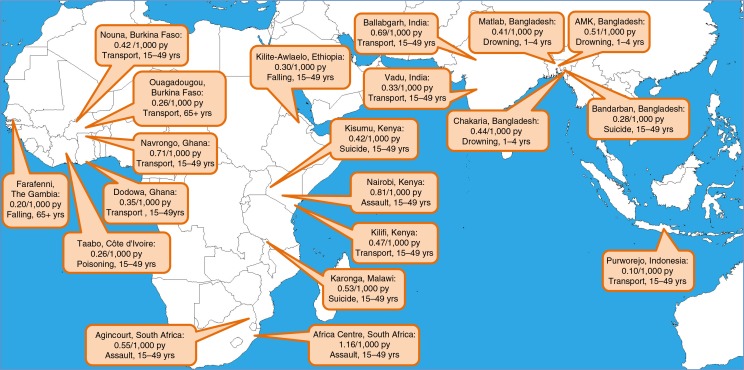
Table 1 shows the overall numbers of deaths from external causes and the exposure time for each site, by age group. Figure 1 shows a map of the 20 sites, each one marked with its age-sex-time standardised overall mortality rate for deaths due to external causes, plus a note of the specific WHO 2012 VA external cause category and age group which accounted for the largest proportion of overall deaths from external causes. Approximately one-quarter of deaths due to external causes occurred in the under-15-year age group. External cause mortality at three of the Bangladeshi sites was dominated by drownings among small children, while elsewhere leading cause categories mainly comprised transport-related deaths, suicides, and assaults.
Table 1.
Numbers of deaths from external causes and person-years (py) of exposure, by age group, for 20 INDEPTH sites
| Infants | 1–4 years | 5–14 years | 15–49 years | 50–64 years | 65+years | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Deaths | py | Deaths | py | Deaths | py | Deaths | py | Deaths | py | Deaths | py | |
| Bangladesh: Matlab | 12.4 | 41,792 | 242.5 | 167,334 | 88.7 | 401,272 | 202.3 | 886,951 | 56.4 | 189,069 | 78.7 | 108,061 |
| Bangladesh: Bandarban | 1,242 | 2.0 | 5,770 | 2.0 | 13,626 | 10.5 | 30,173 | 5,891 | 2.0 | 2,705 | ||
| Bangladesh: Chakaria | 4.8 | 5,636 | 29.5 | 21,992 | 20.7 | 60,951 | 15.8 | 104,097 | 5.8 | 16,234 | 9.9 | 8,257 |
| Bangladesh: AMK | 2.4 | 10,558 | 60.9 | 43,236 | 25.5 | 105,701 | 112.1 | 274,129 | 20.2 | 53,184 | 25.4 | 26,927 |
| Burkina Faso: Nouna | 13.7 | 30,362 | 37.8 | 105,185 | 50.0 | 181,699 | 91.8 | 275,936 | 30.0 | 47,682 | 44.6 | 27,722 |
| Burkina Faso: Ouagadougou | 0.9 | 6,943 | 3.0 | 27,941 | 6.5 | 51,217 | 17.1 | 119,468 | 6.6 | 11,459 | 8.3 | 4,149 |
| Côte d'Ivoire: Taabo | 3,962 | 3.0 | 12,951 | 6.9 | 30,967 | 14.1 | 48,484 | 6,967 | 3.4 | 3,173 | ||
| Ethiopia: Kilite Awlaelo | 3,185 | 1.5 | 13,009 | 11.3 | 39,917 | 16.4 | 59,397 | 4.6 | 11,173 | 6.9 | 7,125 | |
| The Gambia: Farafenni | 1.6 | 11,438 | 3.4 | 42,802 | 8.1 | 88,740 | 21.4 | 139,746 | 5.9 | 22,485 | 15.8 | 11,506 |
| Ghana: Navrongo | 19.2 | 30,124 | 52.3 | 116,283 | 119.3 | 296,767 | 314.7 | 534,464 | 140.7 | 128,494 | 226.6 | 70,664 |
| Ghana: Dodowa | 1.9 | 14,120 | 9.9 | 58,318 | 19.9 | 138,762 | 91.6 | 255,677 | 24.8 | 37,001 | 32.7 | 27,227 |
| India: Ballabgarh | 4.0 | 8,405 | 12.9 | 30,478 | 17.3 | 77,584 | 165.0 | 194,902 | 27.8 | 30,823 | 32.0 | 15,597 |
| India: Vadu | 4,285 | 0.0 | 16,484 | 2.0 | 33,973 | 49.7 | 128,387 | 11.4 | 15,518 | 15.8 | 7,469 | |
| Indonesia: Purworejo | 2,845 | 14,350 | 2.6 | 44,166 | 16.4 | 136,422 | 6.7 | 27,091 | 3.2 | 21,793 | ||
| Kenya: Kilifi | 3.0 | 38,526 | 13.5 | 147,331 | 41.8 | 310,584 | 169.2 | 422,507 | 61.6 | 65,606 | 86.1 | 33,092 |
| Kenya: Kisumu | 21.3 | 39,887 | 57.6 | 144,451 | 41.6 | 324,153 | 202.2 | 467,691 | 60.5 | 89,105 | 73.5 | 67,080 |
| Kenya: Nairobi | 11.9 | 14,350 | 22.0 | 62,552 | 22.2 | 108,651 | 354.7 | 383,810 | 23.6 | 24,804 | 10.6 | 5,640 |
| Malawi: Karonga | 41.0 | 117,499 | 11.5 | 14,783 | 15.5 | 11,356 | ||||||
| South Africa: Agincourt | 8.4 | 36,811 | 28.3 | 148,961 | 58.3 | 369,285 | 565.5 | 725,431 | 90.4 | 92,519 | 65.3 | 63,187 |
| South Africa: Africa Centre | 7.3 | 22,468 | 34.4 | 91,367 | 69.8 | 232,962 | 544.8 | 374,099 | 92.3 | 54,852 | 87.7 | 39,160 |
Fig. 1.
Map showing overall age-sex-time standardised mortality rates per 1,000 person-years due to external causes, also listing the specific cause category and age group accounting for the largest proportion of deaths due to external causes at each site, for 20 INDEPTH sites.
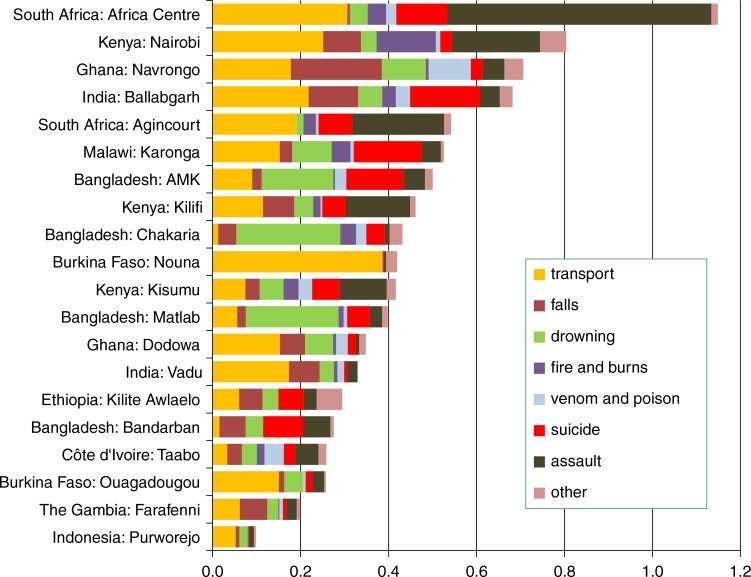
Figure 2 shows the breakdown of overall external cause mortality age-sex-time standardised rates by cause category and site. At the Nouna, Burkina Faso, site, almost all external cause deaths were attributed to transport-related causes (possibly through the use of an historic VA instrument that did not contain all of the WHO 2012 VA items). Elsewhere, there were similar mixes of cause categories between sites, with some local variations.
Fig. 2.
Age-sex-time standardised mortality rates per 1,000 person-years by category of external causes of death, from 20 INDEPTH sites.
Table 2 shows age-sex-time standardised cause-specific mortality rates by cause category, sex, and site for adults (aged 15 years and older). Men were at higher risk of transport-related death than women at every site. Suicides were most common in Bangladesh, particularly among women; in Eastern and Southern Africa, they were more common among men. Sites in Western Africa generally recorded low rates of suicide. South African men were subject to high rates of death following assault.
Table 2.
Age-sex-time standardised mortality rates per 1,000 person-years for adults (aged 15 years and older), by sex and category of external causes of death, for 20 INDEPTH sites
| Transport | Falls | Drowning | Fire and burns | Venom and poison | Suicide | Assault | Other | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||||
| Site | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female |
| Bangladesh: Matlab | 0.12 | 0.02 | 0.03 | 0.01 | 0.04 | 0.02 | 0.01 | 0.01 | 0.00 | 0.00 | 0.05 | 0.10 | 0.04 | 0.03 | 0.02 | 0.01 |
| Bangladesh: Bandarban | 0.05 | 0.05 | 0.10 | 0.18 | 0.19 | 0.02 | ||||||||||
| Bangladesh: Chakaria | 0.04 | 0.10 | 0.02 | 0.01 | 0.03 | 0.11 | 0.01 | 0.03 | 0.10 | 0.03 | 0.01 | 0.01 | 0.04 | |||
| Bangladesh: AMK | 0.19 | 0.02 | 0.03 | 0.02 | 0.01 | 0.01 | 0.00 | 0.15 | 0.21 | 0.09 | 0.01 | 0.04 | ||||
| Burkina Faso: Nouna | 0.62 | 0.38 | 0.01 | 0.01 | 0.01 | 0.04 | 0.03 | |||||||||
| Burkina Faso: Ouagadougou | 0.42 | 0.05 | 0.01 | 0.01 | 0.02 | 0.03 | 0.02 | 0.09 | 0.01 | |||||||
| Côte d'Ivoire: Taabo | 0.06 | 0.05 | 0.04 | 0.06 | 0.03 | 0.09 | 0.06 | 0.15 | 0.02 | 0.04 | ||||||
| Ethiopia: Kilite Awlaelo | 0.08 | 0.07 | 0.15 | 0.04 | 0.03 | 0.14 | 0.04 | 0.08 | 0.02 | 0.03 | 0.05 | |||||
| The Gambia: Farafenni | 0.17 | 0.05 | 0.07 | 0.10 | 0.06 | 0.01 | 0.01 | 0.01 | 0.01 | 0.10 | 0.01 | 0.01 | ||||
| Ghana: Navrongo | 0.41 | 0.12 | 0.32 | 0.25 | 0.09 | 0.01 | 0.00 | 0.00 | 0.13 | 0.06 | 0.06 | 0.03 | 0.12 | 0.04 | 0.09 | 0.03 |
| Ghana: Dodowa | 0.39 | 0.11 | 0.08 | 0.08 | 0.11 | 0.02 | 0.01 | 0.07 | 0.02 | 0.05 | 0.02 | 0.01 | 0.01 | 0.04 | 0.01 | |
| India: Ballabgarh | 0.33 | 0.26 | 0.14 | 0.08 | 0.02 | 0.06 | 0.01 | 0.05 | 0.03 | 0.02 | 0.24 | 0.21 | 0.07 | 0.06 | 0.04 | 0.02 |
| India: Vadu | 0.36 | 0.04 | 0.08 | 0.12 | 0.03 | 0.06 | 0.01 | 0.01 | 0.02 | 0.02 | 0.04 | 0.03 | ||||
| Indonesia: Purworejo | 0.11 | 0.01 | 0.02 | 0.01 | 0.02 | 0.02 | 0.01 | 0.00 | 0.02 | 0.01 | 0.01 | 0.00 | ||||
| Kenya: Kilifi | 0.33 | 0.07 | 0.22 | 0.06 | 0.12 | 0.01 | 0.05 | 0.02 | 0.02 | 0.20 | 0.03 | 0.53 | 0.08 | 0.03 | 0.00 | |
| Kenya: Kisumu | 0.21 | 0.04 | 0.05 | 0.05 | 0.10 | 0.02 | 0.01 | 0.02 | 0.04 | 0.02 | 0.19 | 0.05 | 0.34 | 0.05 | 0.04 | 0.01 |
| Kenya: Nairobi | 0.71 | 0.05 | 0.17 | 0.08 | 0.06 | 0.26 | 0.06 | 0.02 | 0.00 | 0.08 | 0.01 | 0.66 | 0.03 | 0.10 | 0.01 | |
| Malawi: Karonga | 0.26 | 0.06 | 0.01 | 0.04 | 0.18 | 0.01 | 0.05 | 0.04 | 0.02 | 0.23 | 0.09 | 0.14 | 0.04 | 0.01 | 0.01 | |
| South Africa: Africa Centre | 0.89 | 0.13 | 0.01 | 0.01 | 0.07 | 0.07 | 0.04 | 0.06 | 0.00 | 0.39 | 0.05 | 2.01 | 0.30 | 0.02 | 0.01 | |
| South Africa: Agincourt | 0.38 | 0.12 | 0.01 | 0.00 | 0.02 | 0.04 | 0.01 | 0.00 | 0.11 | 0.12 | 0.48 | 0.17 | 0.02 | 0.02 | ||
Table 3 shows, in the same format, age-sex-time standardised cause-specific mortality rates for children. Boys generally experienced higher rates of transport-related mortality than girls, although they were lower rates than for adults. At most sites, drowning occurred at higher rates among boys.
Table 3.
Age-sex-time standardised mortality rates per 1,000 person-years for children (aged under 15 years), by sex and category of external causes of death, for 19 INDEPTH sites
| Transport | Falls | Drowning | Fire and Burns | Venom and Poison | Suicide | Assault | Other | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||||
| Site | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female |
| Bangladesh: Matlab | 0.05 | 0.02 | 0.02 | 0.01 | 0.65 | 0.47 | 0.01 | 0.03 | 0.02 | 0.01 | 0.00 | 0.01 | 0.02 | 0.02 | 0.01 | 0.02 |
| Bangladesh: Bandarban | 0.25 | 0.12 | 0.11 | |||||||||||||
| Bangladesh: Chakaria | 0.01 | 0.03 | 0.61 | 0.48 | 0.02 | 0.09 | 0.02 | 0.01 | 0.06 | |||||||
| Bangladesh: AMK | 0.12 | 0.02 | 0.03 | 0.59 | 0.46 | 0.09 | 0.05 | 0.02 | 0.03 | 0.07 | 0.02 | 0.01 | 0.01 | |||
| Burkina Faso: Nouna | 0.36 | 0.17 | 0.02 | 0.02 | ||||||||||||
| Burkina Faso: Ouagadougou | 0.02 | 0.05 | 0.16 | 0.04 | ||||||||||||
| Côte d'Ivoire: Taabo | 0.07 | 0.04 | 0.04 | 0.04 | 0.05 | 0.07 | 0.04 | 0.04 | ||||||||
| Ethiopia: Kilite Awlaelo | 0.05 | 0.03 | 0.07 | 0.06 | 0.03 | 0.10 | 0.07 | |||||||||
| The Gambia: Farafenni | 0.01 | 0.01 | 0.03 | 0.02 | 0.03 | 0.01 | 0.01 | 0.02 | 0.02 | |||||||
| Ghana: Navrongo | 0.07 | 0.05 | 0.13 | 0.04 | 0.29 | 0.09 | 0.01 | 0.00 | 0.10 | 0.10 | 0.00 | 0.01 | 0.00 | 0.01 | 0.02 | |
| Ghana: Dodowa | 0.03 | 0.04 | 0.03 | 0.02 | 0.09 | 0.06 | 0.01 | 0.01 | 0.02 | 0.01 | ||||||
| India: Ballabgarh | 0.07 | 0.05 | 0.13 | 0.10 | 0.06 | 0.11 | 0.02 | 0.06 | 0.03 | 0.05 | 0.04 | 0.06 | ||||
| India: Vadu | 0.05 | 0.05 | 0.00 | |||||||||||||
| Indonesia: Purworejo | 0.05 | 0.03 | 0.05 | |||||||||||||
| Kenya: Kilifi | 0.04 | 0.04 | 0.02 | 0.03 | 0.02 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.01 | 0.00 | ||||
| Kenya: Kisumu | 0.04 | 0.01 | 0.01 | 0.00 | 0.05 | 0.05 | 0.06 | 0.05 | 0.03 | 0.03 | 0.01 | 0.00 | 0.03 | 0.01 | 0.03 | 0.01 |
| Kenya: Nairobi | 0.16 | 0.03 | 0.01 | 0.03 | 0.10 | 0.02 | 0.13 | 0.10 | 0.02 | 0.01 | 0.07 | 0.09 | ||||
| South Africa: Africa Centre | 0.12 | 0.12 | 0.01 | 0.00 | 0.06 | 0.06 | 0.02 | 0.04 | 0.02 | 0.02 | 0.02 | 0.01 | 0.06 | 0.05 | 0.00 | 0.02 |
| South Africa: Agincourt | 0.11 | 0.07 | 0.04 | 0.02 | 0.02 | 0.02 | 0.01 | 0.02 | 0.02 | 0.01 | 0.01 | 0.02 | ||||
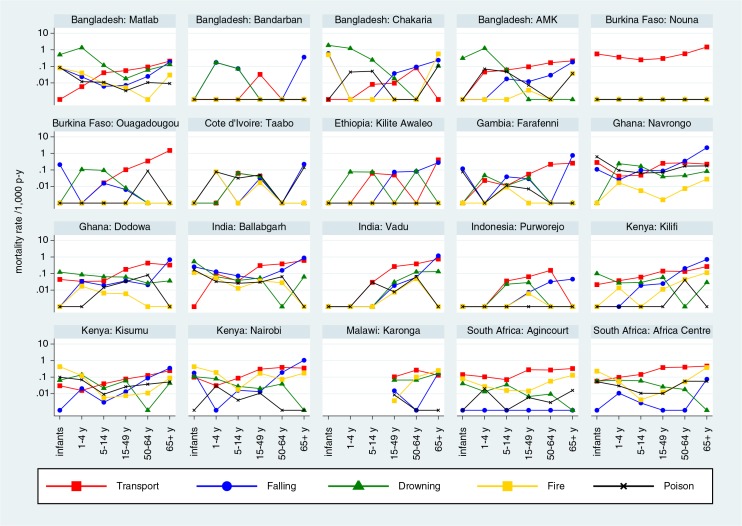
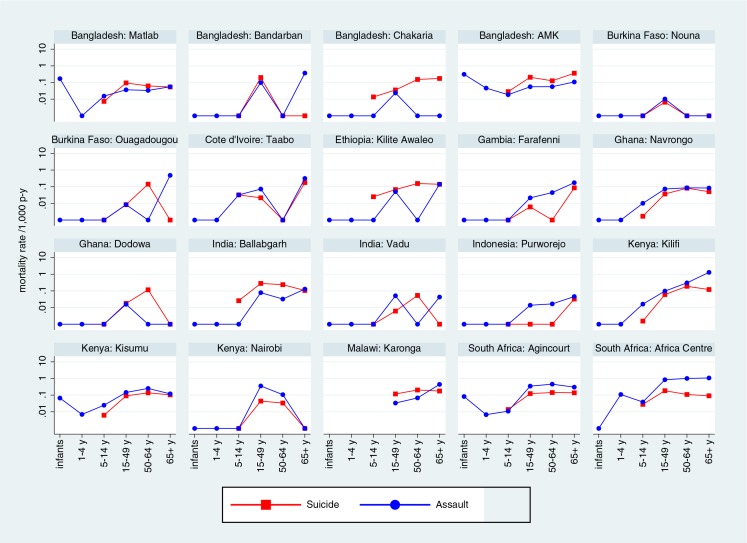
Figure 3 shows site-specific mortality rates by categories of unintentional external causes and age group, with rates for all sites shown on the same logarithmic scale for ease of comparison. Figure 4 shows intentional external causes on the same basis.
Fig. 3.
Site-specific mortality rates per 1,000 person-years by age group and category of unintentional external causes of death.
Fig. 4.
Site-specific mortality rates per 1,000 person-years by age group and category of intentional external causes of death.
Discussion
As was clear from the overview of this cause-specific mortality data set (7), deaths due to external causes form an important component of overall mortality, and in particular account for many premature deaths, in both childhood and early adulthood. The major advantage of addressing external cause mortality from this data set, which included all deaths within circumscribed surveillance populations, is that various biases from attempting to capture injury data alone were avoided. Most obviously, it avoids the difficulties of accounting for both instantaneous fatalities and health facility deaths, which otherwise involves trying to combine diverse reporting mechanisms.
Patterns of external cause mortality revealed from these analyses were more or less consistent with the relatively few other direct measurements from Sub-Saharan Africa and South-East Asia. It is clear that geographic location, age, and sex are major determinants not only of overall external cause mortality but also of specific cause categories. In some cases, geography appeared to play a direct role, for example in the problematically high rates of child drowning in Bangladesh. At the Bandarban site, some 200 m above sea level near the Myanmar border, drowning rates were appreciably lower than in the flat river delta environments of the other three sites in Bangladesh. Similarly, in the mountainous area covered by the Kilite Awlaelo, Ethiopia, site, falling was the major cause of death. It is important to be clear that the WHO 2012 VA standard and the InterVA-4 model are designed for assigning causes of death, and not mechanisms of injury, which are consequently not discussed here.
For suicide, rates were high among Bangladeshi women, whereas in Eastern and Southern Africa rates were high among men; suicide overall was much less common in Western Africa. South Africa and Kenya showed appreciably higher rates of assault-related deaths than other countries reporting here. Countries with poorly developed road transport infrastructures, for example in Western Africa, emerged clearly with high rates of transport-related mortality.
It is sometimes assumed that external causes of death represent a relatively easy option for assigning cause of death via VA. This may be true for a proportion of deaths from external causes, for example instantaneous fatalities with no complicating factors. This assumes, however, that all deaths from external causes have reliable witnesses who can be traced for VA interviews, and who, in the case of inflicted injuries, were not the perpetrators. In this study, based on VA material derived via a variety of antecedents to the WHO 2012 VA standards, there may also have been some difficulties in extracting all the necessary data items correctly, particularly for details of injuries contained in narratives. This probably led to artefacts with road transport deaths in the Nouna, Burkina Faso, site. A few deaths at the Karonga, Malawi, site were incorrectly attributed to burns only on the basis of skin symptoms.
However, there may also be cases where not all is as it seems at first sight, and the details of these may be difficult to ascertain from VA interviews. It has been suggested that suicide rates are actually correlated with autopsy rates; in other words, methods of assigning cause of death are important, particularly when complex and sensitive issues may be involved (34). Using VA, it is very likely, for example, that fatal injuries involving a motor vehicle will be attributed to road traffic deaths, even though motor vehicles can be used as weapons of assault or instruments of suicide.
Conclusions
The patterns of external cause mortality presented here generally conform to expectations, but at the same time they provide detail to fill in some of the gaps in knowledge about deaths arising from injuries of various kinds in Africa and Asia. Clearly, many of the specific mortality burdens identified must be considered as in principle being largely avoidable, given that they do not happen uniformly across locations and population groups. However, preventing external cause mortality poses major challenges involving social, behavioural, environmental, and regulatory considerations. Nevertheless, documenting the major targets for prevention is an important prerequisite.
Acknowledgements
We are grateful to all the residents of INDEPTH HDSS sites who have contributed personal information to this mortality data set, and to the field staff who undertook so many verbal autopsy interviews and data management staff who handled the data at every participating site. INDEPTH acknowledges all the site scientists who have participated in bringing this work together, and who variously participated in analysis workshops in Ghana, Belgium, Thailand, and the United Kingdom. The INDEPTH Network is grateful for core funding from Sida, the Wellcome Trust, and the William & Flora Hewlett Foundation. The Umeå Centre for Global Health Research is core funded by Forte, the Swedish Research Council for Health, Working Life and Welfare (grant no. 2006-1512). PB's residency at the University of the Witwatersrand Rural Knowledge Hub to analyse and draft these results was supported by the European Community Marie Curie Actions IPHTRE project (no. 295168). icddr,b is thankful to the Governments of Australia, Bangladesh, Canada, Sweden and the UK for providing core/unrestricted support. The Ouagadougou site acknowledges the Wellcome Trust for its financial support to the Ouagadougou HDSS (grant no. WT081993MA). The Kilite Awlaelo HDSS is supported by the US Centers for Disease Control and Prevention (CDC) and the Ethiopian Public Health Association (EPHA), in accordance with the EPHA-CDC Cooperative Agreement No.5U22/PS022179_10 and Mekelle University, though these findings do not necessarily represent the funders' official views. The Farafenni site is supported by the UK Medical Research Council. The Vadu site acknowledges core continued funding support from the KEM Hospital Research Centre since 2004. The Kilifi HDSS is supported through core support to the KEMRI-Wellcome Trust Major Overseas Programme from the Wellcome Trust. TNW is supported by a Senior Fellowship (no. 091758) and CN through a Strategic Award (no. 084538) from the Wellcome Trust. This article is published with permission from the Director of KEMRI. The Kisumu site wishes to acknowledge the contribution of the late Dr Kubaje Adazu to the development of the KEMRI/CDC HDSS, which was implemented and continues to be supported through a cooperative agreement between KEMRI and CDC. The Nairobi Urban Health and Demographic Surveillance System (NUHDSS), Kenya, since its inception has received support from the Rockefeller Foundation (USA), the Wellcome Trust (UK), the William and Flora Hewlett Foundation (USA), Comic Relief (UK), the Swedish International Development Cooperation Agency (SIDA) and the Bill and Melinda Gates Foundation (USA). The Agincourt site acknowledges that the School of Public Health and Faculty of Health Sciences, University of the Witwatersrand, and the Medical Research Council, South Africa, have provided vital support since the inception of the Agincourt HDSS. Core funding has been provided by the Wellcome Trust, UK (Grants 058893/Z/99/A, 069683/Z/02/Z, and 085477/Z/08/Z), with contributions from the National Institute on Aging (NIA) of the NIH, the William and Flora Hewlett Foundation, and the Andrew W. Mellon Foundation, USA.
This paper is part of the Special Issue: INDEPTH Network Cause-Specific Mortality. More papers from this issue can be found at http://www.globalhealthaction.net
Footnotes
Authors are listed arbitrarily in order of their site code, and alphabetically within each site.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.World Health Organization. Global status report on road safety 2013; Geneva: WHO; 2013. [Google Scholar]
- 2.World Health Organization, UNICEF. World report on child injury prevention; Geneva: WHO; 2008. [PubMed] [Google Scholar]
- 3.Mars B, Burrows S, Hjelmeland H, Gunnell D. Suicidal behaviour across the African continent: a review of the literature. BMC Public Health. 2014;14:606. doi: 10.1186/1471-2458-14-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Värnik P. Suicide in the World. Int J Environ Res Public Health. 2012;9:760–71. doi: 10.3390/ijerph9030760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sankoh O, Byass P. The INDEPTH Network: filling vital gaps in global epidemiology. Int J Epidemiol. 2012;41:579–88. doi: 10.1093/ije/dys081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leitao J, Chandramohan D, Byass P, Jakob L, Bundhamcharoen K, Choprapawon C, et al. Revising the WHO verbal autopsy instrument to facilitate routine cause-of-death monitoring. Glob Health Action. 2013;6 doi: 10.3402/gha.v6i0.21518. 21518, http://dx.doi.org/10.3402/gha.v6i0.21518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Streatfield PK, Khan WA, Bhuiya A, Alam N, Sie A, Soura AB, et al. Cause-specific mortality in Africa and Asia: evidence from INDEPTH Health and Demographic Surveillance System sites. Glob Health Action. 2014;7 doi: 10.3402/gha.v7.25362. 25362, http://dx.doi.org/10.3402/gha.v7.25362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Razzaque A, Nahar A, Akter Khanam M, Streatfield PK. Socio-demographic differentials of adult health indicators in Matlab, Bangladesh: self-rated health, health state, quality of life and disability level. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.4618. 4618, http://dx.doi.org/10.3402/gha.v3i0.4618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.INDEPTH Network. Bandarban HDSS. Available from: http://www.indepth-network.org/Profiles/Bandarban HDSS.pdf.
- 10.Hanifi MA, Mamun AA, Paul A, Hasan SA, Hoque S, Sharmin S, et al. Profile: the Chakaria Health and Demographic Surveillance System. Int J Epidemiol. 2012;41:667–75. doi: 10.1093/ije/dys089. [DOI] [PubMed] [Google Scholar]
- 11.Lindeboom W, Das SC, Ashraf A. Health and Demographic Surveillance Report 2009 – Abhoynagar and Mirsarai; Dhaka, Bangladesh: ICDDR,B; 2011. [Google Scholar]
- 12.Sié A, Louis VR, Gbangou A, Müller O, Niamba L, Stieglbauer G, et al. The Health and Demographic Surveillance System (HDSS) in Nouna, Burkina Faso, 1993–2007. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5284. 5284, http://dx.doi.org/10.3402/gha.v3i0.5284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rossier C, Soura A, Baya B, Compaoré G, Dabiré B, Dos Santos S, et al. Profile: the Ouagadougou Health and Demographic Surveillance System. Int J Epidemiol. 2012;41:658–66. doi: 10.1093/ije/dys090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kouadio MK, Righetti AA, Abé NN, Wegmüller R, Weiss MG, N'goran EK, et al. Local concepts of anemia-related illnesses and public health implications in the Taabo health demographic surveillance system, Côte d'Ivoire. BMC Hematol. 2013;13:5. doi: 10.1186/2052-1839-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weldearegawi B, Ashebir Y, Gebeye E, Gebregziabiher T, Yohannes M, Mussa S, et al. Emerging chronic non-communicable diseases in rural communities of Northern Ethiopia: evidence using population-based verbal autopsy method in Kilite Awlaelo surveillance site. Health Policy Plan. 2013;28:891–8. doi: 10.1093/heapol/czs135. [DOI] [PubMed] [Google Scholar]
- 16.Oduro AR, Wak G, Azongo D, Debpuur C, Wontuo P, Kondayire F, et al. Profile: the Navrongo Health and Demographic Surveillance System. Int J Epidemiol. 2012;41:968–76. doi: 10.1093/ije/dys111. [DOI] [PubMed] [Google Scholar]
- 17.Gyapong M, Sarpong D, Awini E, Manyeh AK, Tei D, Odonkor G, et al. Profile: the Dodowa Health and Demographic Surveillance System. Int J Epidemiol. 2013;42:1686–96. doi: 10.1093/ije/dyt197. [DOI] [PubMed] [Google Scholar]
- 18.Jasseh M, Webb EL, Jaffar S, Howie S, Townend J, Smith PG, et al. Reaching Millennium Development Goal 4 – the Gambia. Trop Med Int Health. 2011;16:1314–25. doi: 10.1111/j.1365-3156.2011.02809.x. [DOI] [PubMed] [Google Scholar]
- 19.Ng N, Hakimi M, Santosa A, Byass P, Wilopo SA, Wall S. Is self-rated health an independent index for mortality among older people in Indonesia? PLoS One. 2012;7:e35308. doi: 10.1371/journal.pone.0035308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kant S, Misra P, Gupta S, Goswami K, Krishnan A, Nongkynrih B, et al. Profile: the Ballabgarh Health and Demographic Surveillance System (CRHSP-AIIMS) Int J Epidemiol. 2013;42:37–644. doi: 10.1093/ije/dyt055. [DOI] [PubMed] [Google Scholar]
- 21.Hirve S, Juvekar S, Sambhudas S, Lele P, Blomstedt Y, Wall S, et al. Does self-rated health predict death in adults aged 50 years and above in India? Evidence from a rural population under health and demographic surveillance. Int J Epidemiol. 2012;41:1719–27. doi: 10.1093/ije/dys163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scott JA, Bauni E, Moisi JC, Ojal J, Gatakaa H, Nyundo C, et al. Profile: the Kilifi Health and Demographic Surveillance System (KHDSS) Int J Epidemiol. 2012;41:650–7. doi: 10.1093/ije/dys062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Odhiambo FO, Laserson KF, Sewe M, Hamel MJ, Feikin DR, Adazu K, et al. Profile: the KEMRI/CDC Health and Demographic Surveillance System – Western Kenya. Int J Epidemiol. 2012;41:977–87. doi: 10.1093/ije/dys108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oti SO, Mutua M, Mgomella GS, Egondi T, Ezeh A, Kyobutungi C. HIV mortality in urban slums of Nairobi, Kenya 2003–2010: a period effect analysis. BMC Public Health. 2013;13:588. doi: 10.1186/1471-2458-13-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crampin AC, Dube A, Mboma S, Price A, Chihana M, Jahn A, et al. Profile: the Karonga Health and Demographic Surveillance System. Int J Epidemiol. 2012;41:676–85. doi: 10.1093/ije/dys088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Delaunay V, Douillot L, Diallo A, Dione D, Trape JF, Medianikov O, et al. Profile: the Niakhar Health and Demographic Surveillance System. Int J Epidemiol. 2013;42:1002–11. doi: 10.1093/ije/dyt100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kahn K, Collinson MA, Gómez-Olivé FX, Mokoena O, Twine R, Mee P, et al. Profile: Agincourt health and socio-demographic surveillance system. Int J Epidemiol. 2012;41:988–1001. doi: 10.1093/ije/dys115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Herbst AJ, Mafojane T, Newell ML. Verbal autopsy-based cause-specific mortality trends in rural KwaZulu-Natal, South Africa, 2000–2009. Popul Health Metr. 2011;9:47. doi: 10.1186/1478-7954-9-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huong DL, Minh HV, Vos T, Janlert U, Van DD, Byass P. Burden of premature mortality in rural Vietnam from 1999–2003: analyses from a Demographic Surveillance Site. Popul Health Metr. 2006;4:9. doi: 10.1186/1478-7954-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.INDEPTH Network. INDEPTH Network Cause-Specific Mortality – Release 2014. 2014. Oct, Provided by the INDEPTH Network Data Repository. www.indepth-network.org. [DOI]
- 31.Sankoh O, Sharrow D, Herbst K, Whiteson Kabudula C, Alam N, Kant S. The INDEPTH standard population for low- and middle-income countries, 2013. Glob Health Action. 2014;7 doi: 10.3402/gha.v7.23286. 23286, http://dx.doi.org/10.3402/gha.v7.23286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Byass P, Chandramohan D, Clark SJ, D'Ambruoso L, Fottrell E, Graham WJ. Strengthening standardised interpretation of verbal autopsy data: the new InterVA-4 tool. Glob Health Action. 2012;5 doi: 10.3402/gha.v5i0.19281. 19281, http://dx.doi.org/10.3402/gha.v5i0.19281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. Geneva: WHO; 2012. Verbal autopsy standards: the 2012 WHO Verbal Autopsy Instrument. [Google Scholar]
- 34.Kapusta ND, Tran US, Rockett IRH, De Leo D, Naylor CPE, Niederkrotenthaler T, et al. Declining autopsy rates and suicide misclassification. Arch Gen Psychiatr. 2011;68:1050–7. doi: 10.1001/archgenpsychiatry.2011.66. [DOI] [PubMed] [Google Scholar]