Abstract
Background
Data needed to estimate causes of death and the pattern of these deaths are scarce in sub-Saharan Africa. Such data are very important for targeting, monitoring, and evaluating health interventions.
Objective
To estimate the mortality rate and determine causes of death among adults (aged 15 years and older) in a rural district of southern Ghana, using the InterVA-4 model.
Design
Data used were generated from verbal autopsies conducted for registered adult members of the Dodowa Health and Demographic Surveillance System who died between 2006 and 2010. The InterVA-4 model was used to assign the cause of death.
Results
Overall, the mortality rate for the period under review was 7.5/1,000 person-years (py) for the general population and 10.4/1,000 py for those aged 15 and older. The leading cause of death was communicable diseases (CDs), with a malaria-specific mortality rate of 1.06/1,000 py. Pulmonary tuberculosis (TB)-specific mortality rate was the next highest (1.01/1,000 py). HIV/AIDS attributed deaths were lower among males than females. Non-communicable diseases (NCDs) contributed to 28.3% of the deaths with cause-specific mortality rate of 2.93/1,000 py. Stroke topped the list with cause-specific mortality rate of 0.69/1,000 py. As expected, young males (15–49 years) contributed to more road traffic accident (RTA) deaths; they had a lower RTA cause-specific mortality rate than older males (50–64 years).
Conclusions
Data indicate that CDs (e.g. malaria and TB) remain the major cause of death with NCDs (e.g. stroke) following closely behind. Verbal autopsy data can provide the causes of mortality in poorly resourced settings where access to timely and accurate data is scarce.
Keywords: adults, cause of death, verbal autopsy, InterVA-4, Health and Demographic Surveillance System, Dodowa, Ghana
The ability to have a healthy long life is an essential part of development. Survival can, thus, be said to be a measure of a country's development (1). For interventions to be effectively implemented and tailored to the right people, it is important for policy makers and planners to be aware of what causes diseases and death among the population they serve, hence the need for accurate and timely data (2). This will help in prioritizing interventions, using the most appropriate strategies for their delivery, and monitoring of their effectiveness (3). Data for the estimation of causes of death and the pattern of these deaths are scarce in sub-Sahara Africa (SSA) (4) unlike the developed countries where vital registration systems are well-developed and medical certifications of death are available (5).
Studies have shown that conducting verbal autopsy (VA) is the best available approach in obtaining empirical information on the cause of many deaths in settings with poor or no routine death certification (5, 6). The conducting of VA for community-reported death is a common practice among sites belonging to the International Network for Demographic Evaluation of Population and Their Health (INDEPTH) Network (7, 8). VA is the process used to obtain information on the cause of death by interviewing close relatives or primary caregivers on the signs and symptoms experienced by the deceased and the sequence of events that led to the death of their relative (6, 9).
The idea of VAs started in 1956 when WHO encouraged lay reporting of health information and a lay reporting form was developed. Diversity in the use of VA instruments demanded standardization; hence, in 2007 WHO standardized the VA form for use (10). A detailed review of the process involved in the development of VA tools exists (11). Traditionally, VAs are coded independently by at least two physicians to determine the cause of death. This has been demanding for sites in low- and middle-income countries where there is a lack of physicians to do clinical work, let alone code VAs. This creates huge backlogs of VAs that require coding. In fact, physician coding has been found to be an expensive and slow process (9). Besides, physician's reliability and repeatability of interpreting the VAs has been questioned (12). It is in this light that a probabilistic model has been developed to interpret VAs (InterVA) for the determination of causes of death (9).
This model has been tested on data from both demographic surveillance sites and hospital records as well as in a number of studies and has been refined based on previous InterVA models (5, 9, 12, 13). The revised InterVA-4 brings on a new standard of interpreting VA that fits into the WHO VA instrument in terms of cause of death categories and input indicators (14). This new tool was used on the Dodowa Health and Demographic Surveillance System (DHDSS) data to estimate causes of deaths of those aged 15 and older for 2006–2010.
This paper therefore focuses on estimating the mortality rate and determining the causes of death among the adult population (15 years and older) in a rural district of southern Ghana using the revised InterVA-4 model.
Methods
Study area
The study area is the DHDSS site. The DHDSS operates within the boundaries of the former Dangme West District (now the Shai-Osudoku and Ningo-Prampram districts); one of the ten districts within the Greater Accra Region of Ghana located in the southeastern part of Ghana, lying between latitude 5°45′ S and 6°05′ N and longitude 0°05′ E and 0°20′ W. The district covers about 41.5% (1528.9/km2) of the total land size within the region. It is about 40.8 km from the national capital of Ghana, Accra.
The site conducted its baseline survey in 2005. By the end of 2010, there were 22,767 households with 111,976 residents under surveillance. Persons younger than age 15 formed 40.5% of the population, which is similar to other developing countries (15) with children younger than 5 years accounting for 15.2%. There were 87 males to every 100 females. Households headed by females constituted 39.1%. The district is fairly rural and the inhabitants are mainly fishermen, petty traders, and artisans, with a handful of civil servants. Detailed description of the study area is available elsewhere (16). In total, 21 static health facilities delivered services in the district. Many inhabitants live more than 5 km away from government health facilities (17). Malaria, diarrhea, Acute Respiratory Infection (ARI), hypertension, and skin diseases are the top five most common diseases seen at the outpatient departments in the district, with malaria ranking first (18). Malaria prevalence in the district was estimated at about 7% in 2011 (19). The national HIV/AIDS level was 2.0% in 2010, but that of the Greater Accra region was 2.6% (20).
Death registration and VA procedures
The DHDSS collects vital statistics from all households in its Demographic Surveillance Area (DSA). Between 2006 and 2010, households were visited every 6 months and events such as pregnancies, births, deaths, and migration was registered. Community key informants (CKIs) were trained to pick the events in their communities to supplement those collected by the fieldworkers. Deaths of registered household members picked by fieldworkers and CKIs were followed up by trained field supervisors who conducted VAs using standard VA questionnaires, which are in three categories: neonatal (0–27 days), children (28 days to below 12 years), and adult (12 years and above). Once an interview was completed, VA forms were returned to the field office of the HDSS for cross checking of inconsistencies and blanks.
The InterVA model
The InterVA-4 model version 4.02 which was used to estimate the cause of death for this paper is computer-based, and uses the Bayes’ theorem, in an attempt to overcome the longstanding limitations of alternative methods (1, 4, 6), such as physicians coding. To use this model, there is the need to categorize the local conditions of malaria and HIV into ‘high’ or ‘low’ (9). Because malaria is persistently number one on the list of top 10 diseases in the study area (19), malaria was categorized as ‘high’ and HIV as ‘low’ in this analysis. More information on the development of this probabilistic model and its robustness are available elsewhere (9, 22). InterVA-4 generates up to three probable causes of death for each case with their assigned likelihoods or indeterminate result. If the sum of the three likelihoods is less than 1, then the residual component is assigned as indeterminate. For cases in which the information is limited or inconsistent, that case is assigned indeterminate with a likelihood of 1. Registered deaths without VAs were assigned as ‘VA not completed’. This group was, however, added to the indeterminate during analysis. The InterVA-4 model was applied to the dataset using the methods previously described (14) and as described in detail in the introductory paper of this issue (23).
Results
General trends in mortality between 2006 and 2010
Between 2006 and 2010, 3,988 deaths were registered with the DSA. Of these, 3,005 had a VA completed. In total, 3,324 of the registered deaths were aged 15 and older, and of those, 2,547 had a VA completed (76.7%). Among the 15 years and older, 1,158 deaths did not have their causes determined. Of these, 777 did not have VA completed, whereas for 381 of them, InterVA-4 could not assign any cause.
The overall mortality rate for the period was 7.5/1,000 person-years (py) whereas that of 15 years and older was 10.4/1,000 py. The crude mortality rate declined from 9.8/1,000 in 2006 to 6.6/1,000 py in 2010 (data not shown).
Table 1 presents the number of deaths, person-time observed, and the trends in mortality between 2006 and 2010. Mortality rates consistently declined for the age groups 15–49 and 65 years and older for the 5-year period. Males generally had higher mortality rates than females.
Table 1.
Number of deaths, person-time observed, and mortality rates by sex, age, and year 2010
| 15–49 years | 50–64 years | 65+ years | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Person year | Deaths | Rate/1,000 py | Person year | Deaths | Rate/1,000 py | Person year | Deaths | Rate/1,000 py | |
| 2006 | |||||||||
| Male | 20,462 | 124 | 6.06 | 2,771 | 75 | 27.07 | 1,848 | 153 | 82.80 |
| Female | 24,327 | 153 | 6.29 | 3,737 | 66 | 17.66 | 3,389 | 207 | 61.08 |
| Total | 44,789 | 277 | 6.18 | 6,508 | 141 | 21.67 | 5,237 | 360 | 68.74 |
| 2007 | |||||||||
| Male | 22,096 | 124 | 5.61 | 3,004 | 50 | 16.64 | 1,879 | 128 | 68.13 |
| Female | 26,635 | 130 | 4.88 | 4,015 | 57 | 14.20 | 3,471 | 162 | 46.68 |
| Total | 48,731 | 254 | 5.21 | 7,019 | 107 | 15.24 | 5,349 | 290 | 54.21 |
| 2008 | |||||||||
| Male | 23,876 | 117 | 4.90 | 3,232 | 63 | 19.49 | 1,933 | 106 | 54.83 |
| Female | 28,956 | 124 | 4.28 | 4,311 | 63 | 14.61 | 3,576 | 184 | 51.45 |
| Total | 52,832 | 241 | 4.56 | 7,543 | 126 | 16.70 | 5,509 | 290 | 52.64 |
| 2009 | |||||||||
| Male | 24,310 | 102 | 4.20 | 3,299 | 62 | 18.80 | 1,921 | 107 | 55.69 |
| Female | 29,668 | 129 | 4.35 | 4,397 | 57 | 12.96 | 3,580 | 170 | 47.48 |
| Total | 53,978 | 231 | 4.28 | 7,696 | 119 | 15.46 | 5,502 | 277 | 50.35 |
| 2010 | |||||||||
| Male | 24,859 | 87 | 3.50 | 3,516 | 76 | 21.61 | 1,986 | 105 | 52.86 |
| Female | 30,488 | 111 | 3.64 | 4,719 | 65 | 13.78 | 3,644 | 167 | 45.83 |
| Total | 55,346 | 198 | 3.58 | 8,235 | 141 | 17.12 | 5,631 | 272 | 48.31 |
Cause-specific mortality as determined by InterVA-4
Malaria was found to be the leading cause of death with a cause-specific mortality rate of 1.06/1,000 py, followed by pulmonary tuberculosis (TB), with 1.01/1,000 py. Cause-specific mortality rate for stroke was 0.69/1,000 py, whereas that of ARIs and digestive neoplasms were 0.54/1,000 py and 0.47/1,000 py, respectively. The cause-specific mortality rates for acute cardiac diseases and acute abdomen were 0.46/1,000 py and 0.44/1,000 py, respectively (Table 2).
Table 2.
Deaths calculated as sum of fractional likelihoods, then rounded to nearest whole number
| Cause of death | Deaths* | CSMFs (%) | Rate/1,000 py |
|---|---|---|---|
| Malaria | 339 | 10.21 | 1.06 |
| Pulmonary tuberculosis | 322 | 9.7 | 1.01 |
| Stroke | 220 | 6.62 | 0.69 |
| ARIs | 174 | 5.22 | 0.54 |
| Digestive neoplasms | 150 | 4.52 | 0.47 |
| Acute cardiac disease | 146 | 4.4 | 0.46 |
| Acute abdomen | 141 | 4.25 | 0.44 |
| Other and unspecified infect diseases | 120 | 3.61 | 0.38 |
| Road traffic accident | 70 | 2.11 | 0.22 |
| Other and unspecified cardiac diseases | 61 | 1.82 | 0.19 |
| HIV/AIDS-related death | 59 | 1.76 | 0.18 |
| Other and unspecified neoplasms | 38 | 1.14 | 0.12 |
| Accidental fall | 29 | 0.86 | 0.09 |
| Respiratory neoplasms | 26 | 0.78 | 0.08 |
| Indeterminate | 381 | 11.45 | 1.19 |
| VA not completed | 777 | 23.38 | 2.43 |
Deaths calculated as sum of fractional likelihoods, then rounded to nearest whole number.
Causes of deaths and mortality rates for males and females aged 15 and above
Table 3 shows the leading causes of deaths for males and females by mortality rates and age groups. TB was the first leading cause of death for males in all the age groups, whereas malaria was the leading cause of death in females within the 15–49 and 65 years and above age groups. However, mortality rate attributable to stroke was the leading cause of death for the females in the 50–64 years age group. Mortality rate due to deaths from road traffic accident (RTA) was higher in males than females. HIV/AIDs mortality rate was higher in females than in males. Unexpectedly, digestive neoplasms were among the leading causes of death. Males in the age group 50 years and above had higher mortality rates than females, whereas in the 15–49 years age group females had a higher mortality rate.
Table 3.
Deaths calculated as sum of fractional likelihoods, then rounded to nearest whole number
| Male | Female | ||||
|---|---|---|---|---|---|
|
|
|
||||
| Cause of deaths | Deaths* | Rate/1,000 py | Cause of deaths | Deaths* | Rate/1,000 py |
| 15–49 years | |||||
| Pulmonary tuberculosis | 72 | 0.62 | Malaria | 103 | 0.74 |
| Malaria | 51 | 0.45 | Pulmonary tuberculosis | 64 | 0.45 |
| Road traffic accident | 36 | 0.31 | HIV/AIDS-related death | 32 | 0.23 |
| Other unspecified infections | 28 | 0.24 | Digestive neoplasms | 26 | 0.18 |
| Acute abdomen | 23 | 0.2 | Acute abdomen | 26 | 0.18 |
| ARIs | 22 | 0.19 | ARIs | 25 | 0.18 |
| Digestive neoplasms | 17 | 0.14 | Stroke | 17 | 0.12 |
| Stroke | 13 | 0.11 | Other unspecified infections | 15 | 0.10 |
| Accidental drowning | 12 | 0.10 | Acute cardiac disease | 13 | 0.10 |
| HIV/AIDS-related death | 10 | 0.08 | Obstetric hemorrhage | 13 | 0.09 |
| Acute cardiac disease | 10 | 0.08 | Road traffic accident | 10 | 0.07 |
| Indeterminate | 62 | 0.54 | Indeterminate | 71 | 0.5 |
| VA not completed | 141 | 1.22 | VA not completed | 152 | 1.09 |
| 50–64 years | |||||
| Pulmonary tuberculosis | 35 | 2.20 | Stroke | 30 | 1.42 |
| Digestive neoplasms | 26 | 1.62 | Pulmonary tuberculosis | 29 | 1.36 |
| ARIs | 23 | 1.44 | Malaria | 25 | 1.18 |
| Stroke | 22 | 1.42 | Acute cardiac disease | 15 | 0.70 |
| Acute cardiac disease | 22 | 1.36 | Digestive neoplasms | 15 | 0.70 |
| Malaria | 21 | 1.32 | Other unspecified infections | 13 | 0.63 |
| Other unspecified infections | 15 | 0.93 | ARIs | 13 | 0.61 |
| Acute abdomen | 14 | 0.86 | HIV/AIDS-related death | 9 | 0.41 |
| Road traffic accident | 9 | 0.56 | Acute abdomen | 8 | 0.39 |
| Other unspecified cardiac disease | 7 | 0.43 | Other unspecified cardiac disease | 8 | 0.39 |
| HIV/AIDS-related death | 5 | 0.3 | Road traffic accident | 7 | 0.32 |
| Diabetes mellitus | 4 | 0.26 | Severe anemia | 4 | 0.2 |
| Indeterminate | 38 | 2.41 | Indeterminate | 28 | 1.32 |
| VA not completed | 70 | 4.42 | VA not completed | 79 | 3.73 |
| 65+ years | |||||
| Pulmonary tuberculosis | 59 | 6.17 | Malaria | 92 | 5.24 |
| Stroke | 47 | 4.93 | Stroke | 90 | 5.09 |
| Malaria | 46 | 4.83 | Pulmonary tuberculosis | 64 | 3.62 |
| Acute cardiac disease | 41 | 4.3 | ARIs | 53 | 3.00 |
| ARIs | 39 | 4.03 | Acute cardiac disease | 46 | 2.60 |
| Acute abdomen | 33 | 3.44 | Acute abdomen | 38 | 2.14 |
| Digestive neoplasms | 32 | 3.37 | Digestive neoplasms | 35 | 1.99 |
| Other unspecified infections | 21 | 2.24 | Other unspecified infections | 28 | 1.60 |
| Other unspecified cardiac disease | 14 | 1.48 | Other unspecified cardiac disease | 24 | 1.34 |
| Other unspecified neoplasms | 11 | 1.18 | Accidental fall | 16 | 0.90 |
| Diabetes mellitus | 7 | 0.78 | Other unspecified neoplasms | 15 | 0.84 |
| Asthma | 6 | 0.62 | Severe malnutrition | 11 | 0.61 |
| Respiratory neoplasms | 5 | 0.56 | Severe anemia | 10 | 0.55 |
| Indeterminate | 65 | 6.82 | Indeterminate | 116 | 6.59 |
| VA not completed | 141 | 14.74 | VA not completed | 194 | 10.99 |
Deaths calculated as sum of fractional likelihoods, then rounded to nearest whole number.
Distribution of causes of deaths by cause category
Considering cause categories, communicable diseases (CDs) were the leading causes of death, with a cause-specific mortality rate of 3.29/1,000 py. Non-communicable diseases (NCDs) (hypertension, stroke, acute cardiac disease, diabetes mellitus, severe anemia, sickle cell disease, chronic obstructive pulmonary disease, asthma, acute abdomen, liver cirrhosis, renal failure, epilepsy, neoplasm, severe malnutrition, other unspecified cardiac disease, and other unspecified NCD) had a mortality rate of 2.93/1,000 py. Trauma or injury-specific mortality rate was 0.47/1,000 py, whereas that of maternal-related causes was 0.08/1,000 py (data not shown).
Cause of death by cause group by sex
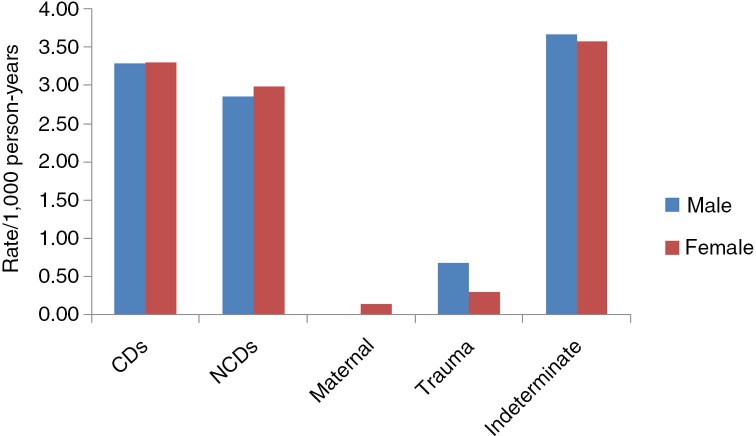
The mortality rates and the pattern of distribution of causes of death were virtually the same in both males and females except with trauma (Fig. 1). Mortality rate was highest in CDs, followed by NCDs, and then trauma. The rates of CDs (3.30/1,000 py) and NCDs (2.99/1,000 py) in females (3.28/1,000 py) were slightly higher than in males (2.86/1,000 py). Males had higher mortality rate from trauma (0.68/1,000 py) than females (0.30/1,000 py).
Fig. 1.
Mortality rates per 1,000 person-years by cause group by sex (2006–2010).
Cause of death by age
The pattern of cause of death differed for the various age groups (Table 4). Generally, mortality rates for all cause groups, except maternal mortality, increased with age. Mortality rates from NCDs were higher in males than in females for the 50 and above age groups, whereas for the 15–49 years age group, the rate was higher in females. Among the same age group, mortality rate for maternal causes was 0.19/1,000 py.
Table 4.
Deaths calculated as sum of fractional likelihoods, then rounded to nearest whole number
| Male | Female | |||
|---|---|---|---|---|
|
|
|
|||
| Cause of deaths | Deaths* | Rate/1,000 py | CSMFs | Rate/1,000 py |
| 15–49 years | ||||
| Communicable | 219 | 1.89 | 253 | 1.80 |
| Non-communicable | 92 | 0.79 | 122 | 0.87 |
| Maternal | 0.00 | 0.00 | 26 | 0.19 |
| Trauma | 68 | 0.59 | 24 | 0.17 |
| Indeterminate | 203 | 1.76 | 223 | 1.59 |
| 50–64 years | ||||
| Communicable | 98 | 6.22 | 121 | 5.72 |
| Non-communicable | 103 | 6.53 | 102 | 4.82 |
| Maternal | 0.00 | 0.00 | 0.00 | 0.00 |
| Trauma | 16 | 1.02 | 9 | 0.41 |
| Indeterminate | 108 | 6.84 | 107 | 5.06 |
| 65+ years | ||||
| Communicable | 174 | 18.14 | 247 | 13.98 |
| Non-communicable | 208 | 21.74 | 311 | 17.62 |
| Maternal | 0.00 | 0.00 | 0.00 | 0.00 |
| Trauma | 11 | 1.16 | 22 | 1.22 |
| Indeterminate | 206 | 21.56 | 310 | 17.57 |
Deaths calculated as sum of fractional likelihoods, then rounded to nearest whole number.
Mortality rates and causes of death by cause group by year
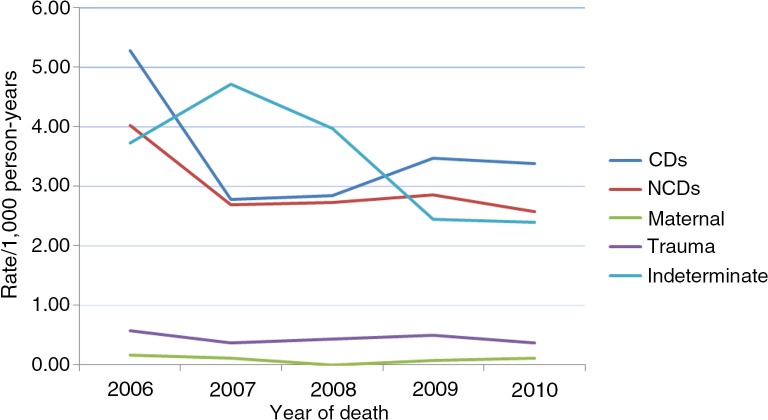
The information in Fig. 2 shows that with the exception of maternal-related causes, mortality rates attributable to all causes of death by cause group recorded the same pattern in the 5-year period. There was no recorded maternal-related death in 2008, whereas the highest mortality rate was recorded in 2006 (0.17/1,000 py). Indeterminate rate was highest in 2007 (4.71/1,000 py) and lowest in 2010 (2.39/1,000 py).
Fig. 2.
Mortality rates per 1,000 person-years by cause group by year (2006–2010).
Discussion
Our results show that the major causes of death among adults in the study area from 2006 to 2010 remain CDs followed by NCDs. The main causes of CDs are malaria and TB, and for NCDs, stroke and digestive neoplasms. These are largely preventable and treatable diseases.
Mortality rates
The findings indicate a decline of mortality from 9.8/1,000 py in 2006 to 6.6/1,000 py in 2010. According to the 2012 World Bank Report, the crude death rate for Ghana was 8/1,000 people in 2010. The death rate for the year 2010 is lower than that of the national rate, an indication of low mortality rates in the study area (24). It must, however, be noted that the methods used for estimating the death rates are slightly different. Whereas, the World Bank used the midyear population as the denominator, this study used person-years contributed. Mortality rates are lower in the 15–49 years age group and highest among the 65 years and older. This finding is similar to what was reported by Becher et al. that mortality rates were lowest in the 15–49 years age group and highest in the 60 years and above in a malaria endemic area of West Africa.
Generally, mortality rates in males are higher than in females. The sex differential in mortality rates confirms what has been documented in other studies (25). Obermeyer et al. also showed higher mortality in males than females for Ghana in their study, which covered 44 countries (26). There are a number of explanations given for the sex difference in mortality that are based on biological, psychological, and social interpretations (27).
Causes of deaths
The predominant cause of death is CDs with cause-specific rate of 3.29/1,000 py in the 5-year period. This reflects what pertains in the rural and less industrial settings in many developing countries, including Ghana (16). The trends over the 5-year period in this study suggest that there has been a decrease in all causes of death by cause group even though the trend has not been progressive. Nevertheless, studies indicate that although the threats of communicable and poverty-related diseases (malaria, infant mortality, cholera, malnutrition) are still in existence (28, 29) chronic disease prevalence was increasing in SSA countries such as Ghana, Nigeria, and South Africa.
Although, Group II causes which are NCDs are the leading causes of death worldwide, Group I causes which are CDs, maternal, neonatal, and nutritional causes are the leading causes of death in SSA (28). Lozano et al. estimated that CDs, maternal, neonatal, and nutritional causes accounted for 76% of deaths in SSA in 2010 and 24.9% of deaths worldwide (5). In estimating cause-specific mortality rates in SSA, Adjuik et al. found that in most of the countries, including Ghana, deaths were caused mainly by CDs (7). The double burden of NCDs and CDs in developing countries like Ghana has been reported by other studies (30, 31) and has a long-term impact on its public health which can lead to the collapse of the health system due to the further stretching of limited resources in terms of infrastructure and finance (28).
This study found that mortality rates attributable to NCDs were higher in females than in males. However, BeLue et al. reported that men were more likely to develop NCDs as a result of lifestyle behaviors such as smoking and alcoholism for which those living in low socioeconomic settings are not excluded (28). This can be attributed to nutritional transitions resulting in obesity or overweight, which has been found to be increasing in some rural areas (32, 33).
Malaria in this study is the leading cause of death in the 15–49 and the 65 years and above age groups among females. These findings were least expected since malaria is known to be more prevalent in children. However, the same concerns were raised in the findings of a systematic analysis of global malaria mortality from 1989 to 2010. It was found that 20% of malaria deaths in 2010 was contributed by adults aged 15–49 years (34).
Pulmonary TB was the leading cause of death among males and also among the top three causes of mortality among females. According to the WHO 2013 Global TB report, Africa is one of the regions, which currently is not on track in achieving the mortality and prevalence targets of 50% reduction by 2015 (35). From the report, TB was the leading cause of deaths among men globally and remains among the top three killers of women; these were confirmed in the study being discussed.
The proportion of HIV/AIDS deaths in this study is very low and is not different from Ghana's HIV prevalence in 2009 (1.9%), which dropped further to 1.5%, respectively, in 2010 and 2011 (20). It is possible that some of the HIV cases may be comorbid and diagnosed as TB by the model. This can be attributed to the fact that measuring TB mortality is very difficult among HIV-positive people even in cases where vital registration systems are complete (35). According to the WHO 2013 Global TB report, causes of death by TB are usually not reliably recorded (35).
With RTA as one of the emerging causes of death, the global status report on road safety showed that more than 90% of fatalities on the road occur in low- and middle-income countries where only 48% of the world's registered vehicles can be found (36). According to the report, RTAs were among the 10 leading causes of death, ranking first and third, respectively, among the age groups 15–29 and 30–44. In this study, RTA is among the top three causes of death among males aged 15–49. This finding is comparable to what was found by Ohene et al., and in the 2012 UNODC report that males contribute more to injury deaths than female (37, 38).
Strengths of the study
This study covered the whole population in the two districts under study, and data collected at the household level closely following the death event. It is therefore representative of the two districts and can be extrapolated to the districts with similar ecological and demographic characteristics.
Study limitation
About 23% of deaths did not have VA completed because of inability to find a relative or individual who was with or knew the deceased to be interviewed. Additionally, 11.5% of the forms had very limited information or the description of the type of ailment or symptoms made it difficult for a cause to be assigned. The narrative part of VA and open-ended questions are excluded from the InterVA model, but these questions may be more appropriate in settings where there is poor knowledge of symptoms of certain diseases, and especially in cases where more local terms maybe relevant (22).
Conclusion
This work has demonstrated that VA can provide data for estimating causes of death in settings where the civil vital registration system is poor or nonexistent. The leading cause of death among the study population was CDs with malaria topping the list. The findings also indicate variations in the patterns of mortality and causes of death and have provided useful empirical information, which is instrumental in understanding disease burden, health planning, and prioritization of health interventions in resource-poor settings where access to timely and accurate data is scarce. To unravel and understand the sources of differential vulnerability in the distribution and patterns of mortality and causes of death among adult rural dwellers, additional research is needed.
Acknowledgements
The INDEPTH Network supported this research. We thank Peter Byass for taking us through the use of InterVA-4 model. The authors express their profound gratitude to the community members, opinion leaders, and all other stakeholders of the Shai-Osudoku and Ningo-Prampram districts of the Greater Accra Region of Ghana who continue to support the research work of the Dodowa Health Research Center. This work could not have been possible without the Dodowa Health and Demographic Surveillance System; the authors extend their appreciation to all field staff of the DHDSS, the ISDPU, and the entire staff of the DHRC. We are grateful to the INDEPTH Secretariat for organising and funding a series of data analysis and scientific writing workshops in Ghana, Thailand, Belgium and UK through core support grants from Sida (Research Cooperation), the Wellcome Trust and the William & Flora Hewlett Foundation.
This paper is part of the Special Issue: INDEPTH Network Cause-Specific Mortality. More papers from this issue can be found at http://www.globalhealthaction.net
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.World Bank. World development indicators. In: Development Data Group, editor. World Bank free PDF; 2012. http://siteresources.worldbank.org/EXTANNREP2012/Resources/8784408-1346247445238/AnnualReport2012_En.pdf [cited June 2013] [Google Scholar]
- 2.Mathers CD, Ma Fat D, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83:171–177c. [PMC free article] [PubMed] [Google Scholar]
- 3.Bryce J, Boschi-Pinto C, Shibuya K, Black RE. WHO estimates of the causes of death in children. Lancet. 2005;365:1147–52. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 4.Morris SS, Black RE, Tomaskovic L. Predicting the distribution of under-five deaths by cause in countries without adequate vital registration systems. Int J Epidemiol. 2003;32:1041–51. doi: 10.1093/ije/dyg241. [DOI] [PubMed] [Google Scholar]
- 5.Lozano R, Freeman MK, James SL, Campbell B, Lopez AD, Flaxman AD, et al. Performance of InterVA for assigning causes of death to verbal autopsies: multisite validation study using clinical diagnostic gold standards. Popul Health Metr. 2011;9:50. doi: 10.1186/1478-7954-9-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fottrell E, Byass P. Verbal autopsy: methods in transition. Epidemiol Rev. 2010;32:38–55. doi: 10.1093/epirev/mxq003. [DOI] [PubMed] [Google Scholar]
- 7.Adjuik M, Smith T, Clark S, Todd J, Garrib A, Kinfu Y, et al. Cause-specific mortality rates in sub-Saharan Africa and Bangladesh. Bull World Health Organ. 2006;84:181–8. doi: 10.2471/blt.05.026492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Becher H, Kynast-Wolf G, Sié A, Ndugwa R, Ramroth H, Kouyaté B, et al. Patterns of malaria: cause-specific and all-cause mortality in a malaria-endemic area of West Africa. Am J Trop Med Hyg. 2008;78:106–13. [PubMed] [Google Scholar]
- 9.Byass P, Huong DL, Van Minh H. A probabilistic approach to interpreting verbal autopsies: methodology and preliminary validation in Vietnam. Scandinavian J Public Health. 2003;31(Suppl 62):32–7. doi: 10.1080/14034950310015086. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Geneva: World Health Organization; 2007. Verbal autopsy standards: ascertaining and attributing causes of death. [Google Scholar]
- 11.Fottrell E, Byass P, Ouedraogo TW, Tamini C, Gbangou A, Sombié I, et al. Revealing the burden of maternal mortality: a probabilistic model for determining pregnancy-related causes of death from verbal autopsies. Popul Health Metr. 2007;5:1. doi: 10.1186/1478-7954-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leitao J, Chandramohan D, Byass P, Jakob R, Bundhamcharoen K, Choprapawon C, et al. Revising the WHO verbal autopsy instrument to facilitate routine cause-of-death monitoring. Glob Health Action. 2013;6 doi: 10.3402/gha.v6i0.21518. 21518, http://dx.doi.org/10.3402/gha.v6i0.21518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fantahun M, Fottrell E, Berhane Y, Wall S, Högberg U, Byass P. Assessing a new approach to verbal autopsy interpretation in a rural Ethiopian community: the InterVA model. Bull World Health Organ. 2006;84:204–10. doi: 10.2471/blt.05.028712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Byass P, Chandramohan D, Clark SJ, D'Ambruoso L, Fottrell E, Graham WJ, et al. Strengthening standardised interpretation of verbal autopsy data: the new InterVA-4 tool. Glob Health Action. 2012;5 doi: 10.3402/gha.v5i0.19281. 19281, http://dx.doi.org/10.3402/gha.v5i0.19281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haub C, Gribble JN. World at 7 Billion [Internet] Population Reference Bureau. 2011 Available from: http://www.questia.com/magazine/1P3-2426603771/the-world-at-7-billion [cited 11 September 2014]. [Google Scholar]
- 16.Gyapong M, Sarpong D, Awini E, Manyeh AK, Tei D, Odonkor G, et al. Profile: the Dodowa HDSS. Int J Epidemiol. 2013;42:1686–96. doi: 10.1093/ije/dyt197. [DOI] [PubMed] [Google Scholar]
- 17.Dodowa Health Research Centre (DHRC) Dangme West District, Accra: Dodowa Health Research Centre, Ghana Health Service; Annual report on health and demographic surveillance system (HDSS) 2009/2010 (unpublished) [Google Scholar]
- 18.Dangme West District Health Management Team (DWDHMT) Accra: Ghana Health Service; (2010). Annual report. [Google Scholar]
- 19.Amu A, Schellenderg D, Agbenyega T. Malaria Prevalence in the Dangme West District [Google Scholar]
- 20.Ghana AIDS Commission, others. Accra: Ghana AIDS Commission; 2012. Ghana country AIDS progress report. [Google Scholar]
- 21.World Health Organization, others. Geneva: WHO; 2005. Technical Consultation on Verbal Autopsy Tools. [Google Scholar]
- 22.Tadesse S. Validating the InterVA model to estimate the burden of mortality from verbal autopsy data: a population-based cross-sectional study. PloS one. 2013;8:e73463. doi: 10.1371/journal.pone.0073463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Streatfield PK, Khan WA, Bhuiya A, Alam N, Sié A, Soura AB, et al. Cause-specific mortality in Africa and Asia: evidence from INDEPTH Health and Demographic Surveillance System Sites. Glob Health Action. 2014;7 doi: 10.3402/gha.v7.25362. 25362, http://dx.doi.org/10.3402/gha.v7.25362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chinbuah MA, Kager PA, Abbey M, Gyapong M, Awini E, Nonvignon J, et al. Impact of community management of fever (using antimalarials with or without antibiotics) on childhood mortality: a cluster-randomized controlled trial in Ghana. Am J Trop Med and Hyg. 2012;87(Suppl 5):11–20. doi: 10.4269/ajtmh.2012.12-0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goudge J, Gilson L, Russell S, Gumede T, Mills A. Affordability, availability and acceptability barriers to health care for the chronically ill: longitudinal case studies from South Africa. BMC Health Serv Res. 2009;9:75. doi: 10.1186/1472-6963-9-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Obermeyer Z, Rajaratnam JK, Park CH, Gakidou E, Hogan MC, Lopez AD, et al. Measuring adult mortality using sibling survival: a new analytical method and new results for 44 countries. 1974–2006. PLoS Med. 2010;7:e1000260. doi: 10.1371/journal.pmed.1000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jacobsen R, Oksuzyan A, Engberg H, Jeune B, Vaupel JW, Christensen K. Sex differential in mortality trends of old-aged Danes: a nation wide study of age, period and cohort effects. European J Epidemiol. 2008;23:723–30. doi: 10.1007/s10654-008-9288-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.BeLue R, Okoror TA, Iwelunmor J, Taylor KD, Degboe AN, Agyemang C, et al. An overview of cardiovascular risk factor burden in sub-Saharan African countries: a socio-cultural perspective. Global Health. 2009;5:10. doi: 10.1186/1744-8603-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van der Sande MA, Milligan PJ, Walraven GE, Dolmans WM, Newport M, Nyan OA, et al. Geographical variation in prevalence of hypertension within the Gambia. J Hum Hypertens. 2001;15:733–9. doi: 10.1038/sj.jhh.1001259. [DOI] [PubMed] [Google Scholar]
- 30.Miszkurka M, Haddad S, Langlois ÉV, Freeman EE, Kouanda S, Zunzunegui MV. Heavy burden of non-communicable diseases at early age and gender disparities in an adult population of Burkina Faso: World Health Survey. BMC Public Health. 2012;12:24. doi: 10.1186/1471-2458-12-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Agyei-Mensah S, Aikins A de-G. Epidemiological transition and the double burden of disease in Accra, Ghana. J Urban Health. 2010;87:879–97. doi: 10.1007/s11524-010-9492-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ntandou G, Delisle H, Agueh V, Fayomi B. Abdominal obesity explains the positive rural-urban gradient in the prevalence of the metabolic syndrome in Benin, West Africa. Nutr Res. 2009;29:180–9. doi: 10.1016/j.nutres.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 33.Fezeu LK, Assah FK, Balkau B, Mbanya DS, Kengne A-P, Awah PK, et al. Ten-year Changes in central obesity and BMI in rural and urban Cameroon. Obesity. 2008;16:1144–7. doi: 10.1038/oby.2008.44. [DOI] [PubMed] [Google Scholar]
- 34.Murray CJ, Rosenfeld LC, Lim SS, Andrews KG, Foreman KJ, Haring D, et al. Global malaria mortality between 1980 and 2010: a systematic analysis. Lancet. 2012;379:413–31. doi: 10.1016/S0140-6736(12)60034-8. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization, others. Global tuberculosis report [Internet] World Health Organization. 2013 Available from: http://apps.who.int/iris/handle/10665/91355 [cited 1 September 2014]. [Google Scholar]
- 36.World Health Organization, others. Geneva: World Health Organization; 2013. Global status report on road safety: time for action 2009. [Google Scholar]
- 37.Ohene S-A, Tettey Y, Kumoji R. Injury-related mortality among adolescents: findings from a teaching hospital's post mortem data. BMC Res Notes. 2010;3:124. doi: 10.1186/1756-0500-3-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.United Nations Office on Drugs and Crime (UNODC) 2012 http://en.Wikipedia.Org/wiki/List_of_countries_by_international_homicide_rate [cited 11 June 2013]. [Google Scholar]