Dear Editor,
Neural-immune interaction in health and disease is a hot topic in current biomedical research1,2. While the central nervous system (CNS) regulates systemic immune responses through hormonal and neuronal route, the peripheral nervous system (PNS) appears to modulate local innate immune responses1. Our organs are heavily innervated by the peripheral nerves, yet, it is not fully understood how the PNS controls immunity2. Toll-like receptors (TLRs) are traditionally expressed in immune cells to regulate innate immunity, but recent studies indicated that TLRs (such as TLR3, 4 and 7) are also expressed in primary sensory neurons, especially nociceptive neurons in dorsal root ganglia (DRGs) and trigeminal ganglia of the PNS to regulate sensory functions such as pain and itch3,4,5,6. TLR signaling is largely mediated by the myeloid differentiation factor 88 (MyD88) protein (but see7), and activation of MyD88 in turn activates the NF-κB and MAP kinase pathways, leading to the production of inflammatory cytokines and chemokines for the initiation of innate immunity3. Increasing evidence suggests that nociceptor neurons play a critical role in host defense and inflammation8,9. However, the key signaling molecules in nociceptors for the regulation of immunity remain to be identified. To this end, we generated MyD88-conditional knockout (CKO) mice by deleting MyD88 in nociceptive neurons expressing the sodium channel subunit Nav1.88,9.
We first examined the expression of MyD88 in DRG neurons in wild-type (WT) and CKO mice. MyD88 is expressed in majority of DRG neurons, including both small-sized C-fiber and large-sized A-fiber neurons in WT mice. Notably, MyD88 expression was dramatically reduced in small-sized neurons of MyD88-CKO mice (Supplementary information, Figure S1, A-C). Loss of MyD88 expression in DRG neurons of CKO mice was also confirmed by single-cell PCR analysis in small-sized neurons (Supplementary information, Figure S1, D and E). Together, we have validated the successful generation of the CKO mice with selective deletion of MyD88 in small-sized nociceptive neurons.
Given the well-known role of MyD88 adapter in innate immunity9, we next investigated if MyD88 in nociceptive neurons would regulate immunity in DRGs by employing fluorescence-activated cell sorting (FACS) analysis. We used CD45 antibody to identify the overall population of infiltrating leukocytes in normal DRGs of C57BL/6 mice. Although at low abundance (0.03% to 0.5% of total cells in DRGs), fourteen different types of immune cells including macrophages, monocytes, neutrophils, helper T cells, cytotoxic T cells and antigen presenting cells (APCs) could be detected in naïve DRGs (Supplementary information, Table S1), suggesting that infiltrating innate and adaptive immune cells are present in low numbers in the normal DRGs where they may play a surveillance role.
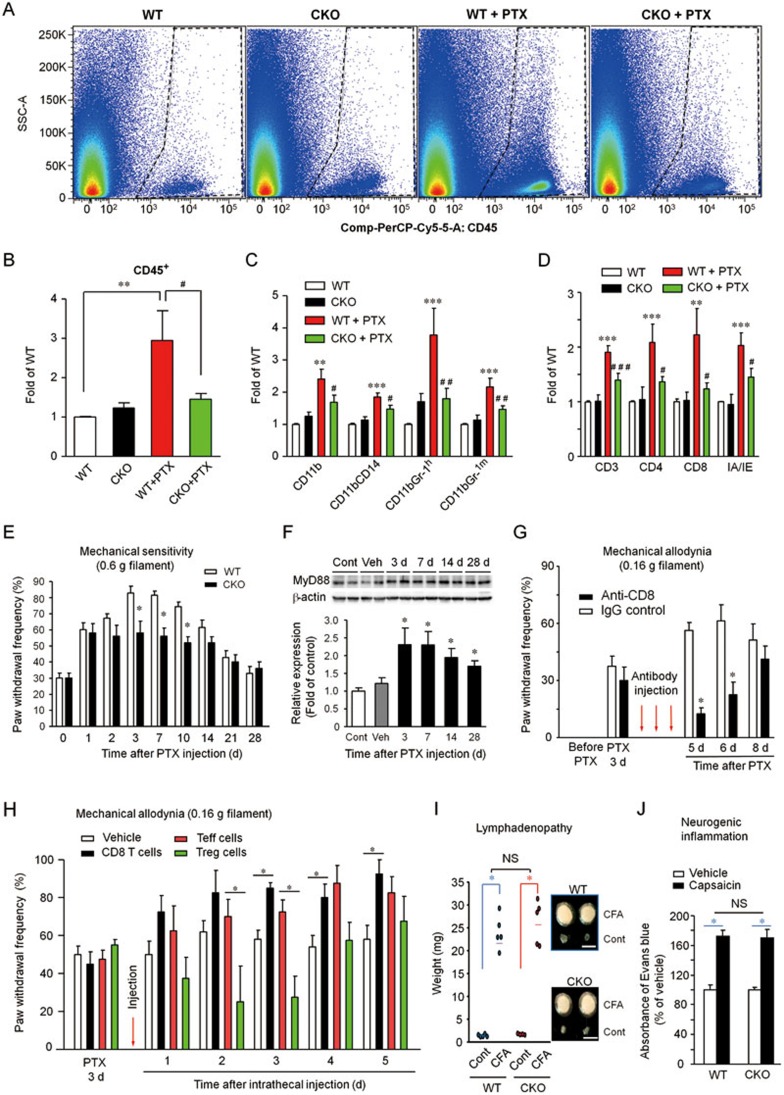
Chemotherapy is known to cause peripheral nerve neuropathy and neuropathic pain5. Unlike other neuropathic pain models which only affect limited numbers of DRGs of an animal, chemotherapy drugs, such as paclitaxel (PTX) could affect all DRGs following systemic injection. Thus, we collected all DRGs in this neuropathic pain model for FACS analysis. One week after the PTX injection, we found significant increases in infiltrating CD45+ leukocytes, which include innate immune cells such as macrophages (CD11b+), monocytes (CD11b+CD14+, also marked by CD11b+Gr-1medium), and neutrophils (CD11b+Gr-1high) in DRGs. These proinflammatory immune cells such as macrophages are known to promote neuropathic pain10. Strikingly, all these increases in innate immune cells were abrogated in the CKO mice (Figure 1A-1C and Supplementary information, Table S1, Figure S1, F-H).
Figure 1.
MyD88 in nociceptive neurons is essential for driving innate and adaptive immunity in DRGs and maintaining neuropathic pain following chemotherapy. (A) FACS analysis showing the overall populations of leukocytes (CD45+) in DRGs of WT and CKO mice with and without PTX treatment (7 d). (B) Quantification of CD45+ leukocytes in DRGs with fold changes (vs. WT-control). (C) Fold changes of monocytes (CD11b+CD14+ and CD11b+Gr-1medium), macrophages (CD11b+), and neutrophils (CD11b+Gr-1high) in DRGs of WT and CKO mice with and without PTX treatment (7 d). **P< 0.01, ***P< 0.001, compared with WT; #P< 0.05, ##P< 0.01, compared with WT + PTX; n = 7-10 mice/group in B-C. (D) Fold changes of T lymphocytes (CD3+), helper T cells (CD4+), cytotoxic T cells (CD8+), and antigen presenting cells (IA/IE+) in DRGs of WT and CKO mice with and without PTX treatment (7 d). **P< 0.01, ***P< 0.001, compared with WT; #P< 0.05, ###P< 0.001, compared with WT + PTX; n = 6-9 mice/group. (E) Time course of PTX-induced neuropathic pain (mechanical hypersensitivity, 0.6 g filament) in WT and CKO mice. *P< 0.05, vs. WT; n = 5 mice/group. (F) Time course of MyD88 expression (western blot) in DRGs following PTX treatment. Lower panel, quantification of the intensity of MyD88 bands. *P< 0.05, vs. vehicle. n = 5 mice/group. (G) Blocking the function of CD8+ T cells with a neutralizing antibody via intrathecal injections (5 μg, once a day for 3 days) reduces PTX-induced mechanical allodynia (0.16 g filament). Arrows indicate antibody injections; n = 4-5 mice/group; *P< 0.05. (H) Adoptive transfer of CD8+ T cells or Tregs via intrathecal injections (2.5 × 105 cells in 10 μl) 3 days after PTX-treatment increases or decreases mechanical allodynia (0.16 g filament), respectively. *P< 0.05; n = 8 mice/group. (I) CFA-induced enlargement of affected lymph nodes (lymphadenopathy, 7 d after CFA injection) in WT and CKO mice. n = 4-5 mice/group; Scale, 5 mm; *P< 0.05. (J) Capsaicin-induced neurogenic inflammation, measured by Evans blue extravasation, in hindpaw tissues of WT and CKO mice. n = 5 mice/group; *P< 0.05; NS, no significance. Mechanical sensitivity was measured by frequency (%) of paw withdrawal response to a von Frey filament (0.6 or 0.16 g). All data are expressed as mean ± SEM.
The role of MyD88 in adaptive immunity is not well defined. Interestingly, PTX treatment also increased the number of infiltrated immune cells implicated in adaptive immunity, including APCs (IA/IE+), T lymphocytes (CD3+), helper T cells (CD4+), and cytotoxic T cells (CD8+) in WT mice. Moreover, deletion of Myd88 in nociceptive neurons also impaired these adaptive immunity responses in DRGs (Figure 1D and Supplementary information, Table S1 and Figure S1, I-L).
We also identified several types of rare cells such as T helper type 1 cells (Th1), natural killer cells (NK), and dendritic cells (DCs) in DRGs, which showed no significant changes after chemotherapy treatment. However, we observed a significant and MyD88-dependent increase of B cells after the PTX treatment (Supplementary information, Table S1, Figure S1M). Furthermore, PTX caused down-regulation of anti-inflammatory T cells, including T helper type 2 cells (Th2; CD3+CD4+IL-4+) and regulatory T cells (Tregs; CD4+CD25+FoxP3+) in DRGs of WT mice, which was also abrogated in CKO mice (Supplementary information, Table S1 and Figure S1, N and O).
For comparison, we also carried out FACS analysis in spleen, which is highly enriched with immune cells, compared to the very low abundance of immune cells in DRGs (Supplementary information, Figure S1P). Chemotherapy did not change the distribution patterns of immune cells in the spleen, suggesting that the PNS is more vulnerable to chemotherapy. In the CKO mice, there were mild compensatory increases in several types of immune cells (Supplementary information, Figure S1P).
MyD88 was shown to regulate neuropathic pain after chemotherapy5. However, the distinct role of MyD88 in neurons vs non-neuronal cells in chronic pain has not been clearly defined. We examined whether selective loss of MyD88 in nociceptive neurons would affect chemotherapy-evoked neuropathic pain. MyD88-CKO mice have intact baseline pain by exhibiting normal thermal and mechanical nociception and intact motor function (data not shown). PTX induced rapid and persistent mechanical hypersensitivity, as indicated by enhanced response to a von-Frey hair stimulation (0.6 g), and this neuropathic pain behavior, only in the maintenance phase, was reduced in CKO mice (Figure 1E). Moreover, PTX caused persistent upregulation of MyD88 in DRGs (Figure 1F).
Several lines of evidence support a contribution of T cells to neuropathic pain. Nerve injury increases T cells in the spinal cord to promote neuropathic pain11,12. To explore the function of specific types of T cells in chemotherapy-induced neuropathic pain, we injected a neutralizing antibody to block the function of CD8+ T cells via the intrathecal route which can target pain at both spinal cord and DRG levels. PTX-treated but not control mice exhibited robust mechanical allodynia, a cardinal feature of neuropathic pain induced by normally innocuous mechanical stimulation (0.16 g filament), and notably, the CD8 neutralizing antibody significantly reversed the PTX-induced mechanical allodynia (Figure 1G). To further test the contribution of T cells to neuropathic pain, we used an adoptive transfer strategy via intrathecal injection of immune cells. Adoptive transfer of pro-inflammatory CD8+ T cells exacerbated neuropathic pain, whereas adoptive transfer of anti-inflammatory Treg cells alleviated neuropathic pain (Figure 1H). Collectively, these behavioral data suggest distinct contributions of CD8+ T cells and Treg cells to neuropathic pain following chemotherapy.
Finally, we evaluated if inflammation could be affected after deletion of Myd88 in nociceptive neurons. Intraplantar injection of complete Freund's adjuvant (CFA) induced profound inflammation, as revealed by dramatic enlargement of the affected lymph node near the inflamed paw (Figure 1I); however, this so-called lymphadenopathy was not altered in CKO (Figure 1I). Intraplantar injection of capsaicin elicited robust neurogenic inflammation in the affected hindpaw, as indicated by Evans blue plasma extravasation in hindpaw tissues, but this neurogenic inflammation was also intact in the CKO mice (Figure 1J).
This is the first study to fully characterize the distributions of different types of immune cells in DRGs of the PNS. We have made several important findings in this study. First, chemotherapy not only causes up-regulation of pro-inflammatory immune cells such as macrophages, monocytes, neutrophils, helper T cells (CD4+), and cytotoxic T cells (CD8+) but also results in down-regulation of anti-inflammatory immune cells including Th2 cells and Tregs. Second, MyD88 is expressed by primary sensory neurons in DRGs and selective deletion of Myd88 in Nav1.8-positive nociceptive neurons results in impaired innate and adaptive immune responses in DRGs. Third, MyD88 in nociceptive neurons is essential for the maintenance but not the development of chemotherapy-induced neuropathic pain. Fourth, specific types of T cells play different roles in maintaining chemotherapy-induced neuropathic pain: CD8+ T cells promote neuropathic pain, whereas Treg cells suppress neuropathic pain after PTX treatment. Taken together, our data suggest that MyD88 in nociceptive neurons maintains neuropathic pain by regulating innate and adaptive immunity in the DRG. Since nociceptive neurons also express chemokines that are critical for the trafficking of immune cells2,3, future studies are warranted to examine whether MyD88 is involved in the expression of chemokines (e.g., CCL2, CXCL1, and CXCL10) in DRG nociceptive neurons. However, there are two potential pitfalls in this study. First, Nav1.8-positive neurons may also include a small portion of neurons that are not nociceptive13. Second, intrathecal injections of T-cells and antibody may also modulate neuropathic pain at the spinal cord level, and PTX treatment was shown to cause glial activation in the spinal cord14. Thus, caution must be taken to interpret the results of this study.
Recent studies have demonstrated a critical role of nociceptive neurons in the control of inflammation: deletion of nociceptive neurons leads to exaggerated8 or reduced9 inflammation, depending on different animal models of inflammation. Our data failed to support an activating role of nociceptive neuron-MyD88 in peripheral inflammation: both capsaicin-induced neurogenic inflammation and CFA-induced lymphadenopathy are intact in Myd88-CKO mice. Given the distinct roles of inflammation (in non-neuronal tissue) and neuroinflammation (in neural tissue) in the initiation and maintenance of chronic pain15, we conclude that MyD88 in nociceptive neurons might sustain chronic pain by controlling neuroinflammation (infiltration of immune cells) in the PNS.
Acknowledgments
We thank Dr Rohini Kuner of University of Heidelberg for providing Nav1.8-Cre mice. This study was supported by NIH grants R01DE17794, DE22743, and NS67686 to R-R J, and P01HL108793 to D J.
Footnotes
(Supplementary information is linked to the online version of the paper on the Cell Research website.)
Supplementary Information
Supplementary information Figures, Methods and Tables
References
- Sternberg EM. Nat Rev Immunol. 2006. pp. 318–328. [DOI] [PMC free article] [PubMed]
- Chiu IM, von Hehn CA, Woolf CJ. Nat Neurosci. 2012. pp. 1063–1067. [DOI] [PMC free article] [PubMed]
- Liu T, Gao YJ, Ji RR. Neurosci Bull. 2012. pp. 131–144. [DOI] [PMC free article] [PubMed]
- Liu T, Berta T, Park CK, et al. J Clin. Invest. 2012. pp. 2195–2207. [DOI] [PMC free article] [PubMed]
- Li Y, Zhang H, Zhang H, et al. J Pain. 2014. pp. 712–725. [DOI] [PMC free article] [PubMed]
- Liu T, Xu ZZ, Park CK, et al. Nat Neurosci. 2010. pp. 1460–1462. [DOI] [PMC free article] [PubMed]
- Park CK, Xu ZZ, Berta T, et al. Neuron. 2014. pp. 47–54. [DOI] [PMC free article] [PubMed]
- Chiu IM, Heesters BA, Ghasemlou N, et al. Nature. 2013. pp. 52–57. [DOI] [PMC free article] [PubMed]
- Riol-Blanco L, Ordovas-Montanes J, Perro M, et al. Nature. 2014. pp. 157–61. [DOI] [PMC free article] [PubMed]
- Guerrero AT, Cunha TM, Verri WA, et al. Eur J Pharmacol. 2012. pp. 51–57. [DOI] [PubMed]
- Costigan M, Moss A, Latremoliere A, et al. J Neurosci. 2009. pp. 14415–14422. [DOI] [PMC free article] [PubMed]
- Shi XQ, Zekki H, Zhang J. Glia. 2011. pp. 231–241. [DOI] [PubMed]
- Shields SD, Ahn HS, Yang Y, et al. Pain. 2012. pp. 2017–2030. [DOI] [PubMed]
- Ruiz-Medina J, Baulies A, Bura SA, et al. Eur J Pain. 2013. pp. 75–85. [DOI] [PubMed]
- Ji RR, Xu ZZ, Gao YJ. Nat Rev Drug Disc. 2014. pp. 533–548. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information Figures, Methods and Tables