Abstract
A young male patient had been evaluated for pleural effusion at another center wherein on the basis of exudative, lymphocyte predominant pleural effusion with high pleural fluid adenosine deaminase (ADA) levels and tuberculin skin test (TST) reactivity, antituberculous medications had been administered. Reevaluation in view of worsening symptoms led to confirmation of the diagnosis of T-cell lymphoblastic lymphoma with pleuro-peritoneal lymphomatosis and tonsillar involvement. This case highlights the fact that elevated ADA levels should not be taken as surrogate for a diagnosis of TB in the absence of histopathological/microbiological confirmation even in countries with high tuberculosis (TB) prevalence. Tonsil in an uncommon site of involvement in patients with T-cell lymphoma. As the diagnosis in our patient was confirmed from biopsy of a tonsillar mass, a thorough physical examination should be performed in all patients with a suspected diagnosis of lymphoma.
KEY WORDS: Adenosine deaminase, non-Hodgkin's lymphoma, T-cell lymphoma, tuberculosis
INTRODUCTION
In high prevalence countries, it is usual to consider a diagnosis of tuberculosis (TB) when the pleural/peritoneal fluid levels of adenosine deaminase (ADA) are elevated in the setting of an exudative pleural effusion/ascites with predominance of lymphocytes on cytological examination. However, there are limitations in the sensitivity and specificity of elevated ADA levels in the diagnosis of TB. Also, tuberculin reactivity is very often inappropriately misused as an indicator for active TB.
Lymphomas are the third most important cause of malignant pleural effusion next to lung and breast cancer. Disseminated involvement with lymphoma can have a presentation that can closely mimic disseminated TB. We herein describe the case of a young male patient wherein a clinical picture resembling disseminated TB was subsequently diagnosed as disseminated involvement with T-cell lymphoblastic lymphoma (T-LL).
CASE REPORT
A young male patient presented with history of fever, shortness of breath and right sided chest pain for 4 weeks duration. Fever used to be more during the evening hours. Chest pain was pleuritic in character. There was no history of hemoptysis, wheezing, leg swelling, dysphagia, odynophagia, orthopnea, stridor, hoarseness of voice, or generalized swellings. Patient had lost 6 kg weight over the past 2 months and there was loss of appetite. Past and family history was unremarkable. The patient was a lifetime nonsmoker and nonalcoholic. There was history of contact with a patient of TB in the recent past. HIV-ELISA test was negative.
For the above symptoms, patient had been evaluated at another center where diagnosis of right pleural effusion was made and thoracentesis had been performed. Straw colored clear fluid had been aspirated. Fluid was an exudate with predominance of lymphocytes on cytological examination and pleural fluid ADA levels were elevated (70 IU/L). Tuberculin skin test demonstrated induration of 18 mm at the end of 48 h. With this profile, a possibility of tubercular pleural effusion was considered and patient was initiated on four drug antitubercular treatment (ATT) with four first line drugs namely Isoniazid, Rifampicin, Ethambutol, and Pyrazinamide. There was no improvement in symptoms and patient developed worsening shortness of breath, abdominal distension, and high grade fever within 2 weeks of initiation of treatment. He was referred to our center. A pleural pigtail catheter had been inserted for drainage of the reaccumulating right side pleural effusion.
On general physical examination, pulse rate was 92/min, blood pressure (BP) was 122/80 mmHg and there was no peripheral lymph node enlargement or venous prominences. Examination of the oral cavity showed unilateral enlargement of the left palatine tonsil. The surface of the tonsil had whitish plaques and there was no erythema or bleeding from its surface. Examination of the respiratory system was suggestive of bilateral pleural effusion and on abdominal examination shifting dullness was present suggestive of ascites. Chest radiograph demonstrated blunting of bilateral costophrenic angles suggesting bilateral pleural effusion [Figure 1, Left panel]. Review of computed tomography (CT) scan of the thorax demonstrated bilateral pleural effusion (right > left) and small mediastinal lymph node enlargement with normal appearing lungs [Figure 1, Right panel].
Figure 1.
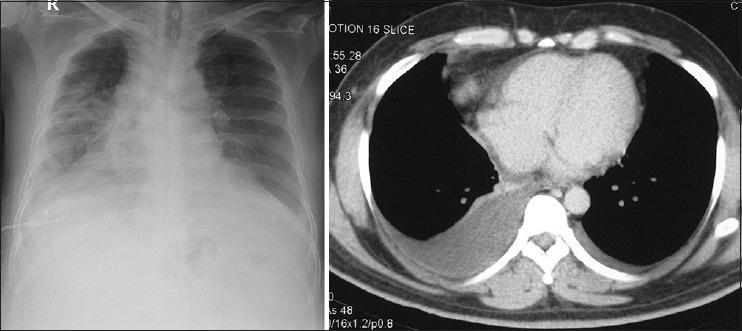
Chest radiograph showing blunting of both costophrenic angles suggestive of bilateral pleural effusion. Pleural pigtail catheter is seen in situ on the right side (Left panel). CECT scan of the thorax demonstrating bilateral pleural effusion, Right > Left side. (Right panel)
Pleural fluid and ascitic fluid examination were performed. Both fluids showed predominance of small lymphocytes with low glucose (5 mg/dl), elevated proteins (5-6 g/dl) and very high ADA (500 U/L) levels. Gram stain and cultures of both the fluids were negative. Whole body Fluorodeoxyglucose positron emission tomography computed tomography (FDG-PET-CT) examination [Figure 2] demonstrated intense uptake in left tonsillar region, along with FDG-avid mediastinal and mesenteric lymph nodes. Abdominal PET-CT images showed omental caking along with diffuse peritoneal thickening and ascites, suggestive of diffuse peritoneal infiltration.
Figure 2.
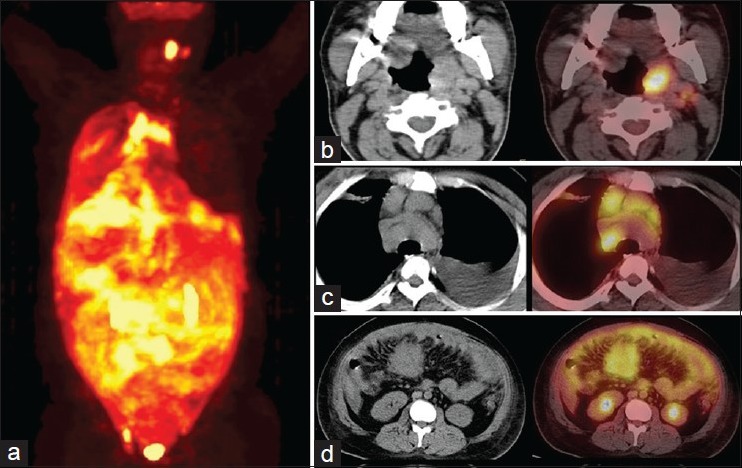
PET-CT scan showing pattern of whole body FDG uptake (Panel A). Enlargement of and intense FDG-avidity is noted in the left tonsil (Panel B). Bilateral pleural effusion and intensely FDG-avid mediastinal lymph nodes are noted (Panel C). Omental caking, with diffuse peritoneal thickening and ascites with diffuse FDG uptake is also seen. (Panel D)
In view of extremely high levels of ADA in the body fluids and radiological findings, a diagnostic possibility of lymphoma was considered and punch biopsy from left tonsillar area and repeat examination of pleural and ascitic fluid for immunocytochemical analysis were performed. Pleural and ascitic fluid examinations and examination of tonsillar biopsy [Figure 3] subsequently confirmed a diagnosis of T-LL. On immunohistopathological examination of the tonsillar biopsy, tumor cells were immunopositive for CD3 (diffusely), CD5 (diffusely), and Tdt (focally), while tumor cells were immunonegative for CD20 and CD10. A final diagnosis of T-LL with pleuro-peritoneal lymphomatosis was established. Bone marrow examination showed all normal hemopoietic cells with adequate megakaryocytes. No lymphoma deposit or granulomas was seen. The patient subsequently received chemotherapy for lymphoma but had a progressively worsening course and expired a few days later.
Figure 3.
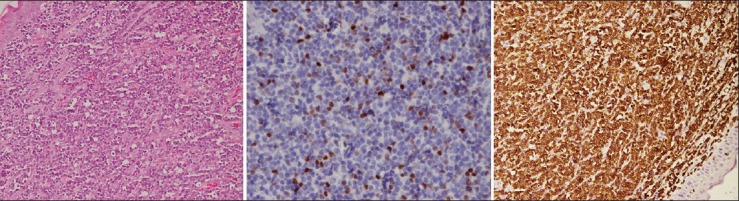
Microphotograph of tonsil biopsy shows expansion of the subepithelium by atypical lymphoid cells. H and E, ×200 (Left panel). The cells express nuclear TdT (Middle panel) and diffuse cytoplasmic CD3 (T-cell) antigen (Right panel)
DISCUSSION
Lymphomas are one of the leading causes of malignant pleural effusion. Pleural effusions and body cavity involvement with lymphoma are more commonly observed with nonHodgkin's lymphoma (NHL) especially the large cell variety. Cytological fluid examination is a sensitive modality for establishing the correct diagnosis.
T-LL is an infrequent type of NHL, representing about 2% of NHL cases. There is bimodal incidence, and patients younger than 20 years or those older than 50 years are usually affected. T-LL comprised 6% of all NHLs according to one lymphoma registry from India.[1] Patients usually present with cervical, supraclavicular or axillary lymphadenopathy (50%), or anterior mediastinal mass (50-75%). Presentation as anterior mediastinal mass is usually associated with pleural/pericardial effusions or superior vena cava syndrome. Stage IV disease (80%) and B symptoms (50%) are common. Extranodal disease is less common and abdominal dissemination is unusual. Bone marrow involvement is infrequent at the time of presentation; however, up to two-thirds of patients eventually develop marrow infiltration. Involvement of the central nervous system is uncommon and usually occurs in advanced disease with concurrent bone marrow involvement.[2] Involvement of Waldeyer's ring as was seen in our patient has been only rarely reported.[3] In treated patients, Stage II/IV disease, late achievement of remission or elevated lactate dehydrogenase (LDH) (>500) have been found to be associated with poor prognosis.[4] The unusual features in our patient were absence of peripheral lymphadenopathy and predominant involvement of the serous cavities and Waldeyer's ring (palatine tonsil) at the time of presentation. Although tonsil is not an uncommon site of involvement in lymphoma, tonsillar involvement in T-cell lymphoma is unusual.
Peritoneal lymphomatosis, as seen in our patient, is a rare condition in malignant lymphoma, which mimics metastatic carcinoma. Other radiologic differential diagnoses include tuberculous peritonitis, mesothelioma, and peritoneal desmoids. In young patients, CT findings like abdominal lymphadenopathy, aneurysmal dilatation of a gut segment with wall thickening and poor delineation at the mesenteric border or enlargement of liver/spleen should lead to the consideration of lymphoma as the leading differential diagnosis. Cytological/histopathological sampling is imperative for establishing a definitive diagnosis.[5]
Apart from TB, high levels of ADA have also been reported in various noninfectious conditions associated with pleural fluid lymphocytosis, including malignant conditions (like adenocarcinomas, leukemias, and lymphomas) and collagen vascular diseases (like rheumatoid pleuritis and Systemic lupus erythematosus (SLE)). Others include fungal infections like coccidioidomycosis and histoplasmosis and bacterial infections like brucellosis. It has been highlighted repeatedly in literature that none of the biomarkers in pleural fluid are specific for tubercular pleuritis therefore interpretation of pleural fluid ADA assay results should always be done in the light of clinical findings and ideally along with results of histopathological findings.[6,7] The maximum joint sensitivity and specificity of ADA for the diagnosis of tuberculous pleuritis was observed to be 93%.[8] Therefore, ADA assay should not be considered as an alternative to methods of definitive diagnosis like biopsy and mycobacterial culture. With very high levels of ADA, possibility of lymphoma should always be considered as a diagnostic possibility.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Naresh KN, Srinivas V, Soman CS. Distribution of various subtypes of non-Hodgkin's lymphoma in India: A study of 2773 lymphomas using R.E.A.L. and WHO classifications. Ann Oncol. 2000;11(Suppl 1):63–7. [PubMed] [Google Scholar]
- 2.Cortelazzo S, Ponzoni M, Ferreri AJ, Hoelzer D. Lymphoblastic lymphoma. Crit Rev Oncol Hematol. 2011;79:330–43. doi: 10.1016/j.critrevonc.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Reiter A, Schrappe M, Ludwig WD, Tiemann M, Parwaresch R, Zimmermann M, et al. Intensive all-type therapy without local radiotherapy provides a 90% event-free survival for children with T-cell lymphoblastic lymphoma: A BFM group report. Blood. 2000;95:416–21. [PubMed] [Google Scholar]
- 4.Hoelzer D, Gökbuget N, Digel W, Faak T, Kneba M, Reutzel R, et al. Outcome of adult patients with T-lymphoblastic lymphoma treated according to protocols for acute lymphoblastic leukemia. Blood. 2002;99:4379–85. doi: 10.1182/blood-2002-01-0110. [DOI] [PubMed] [Google Scholar]
- 5.Karaosmanoglu D, Karcaaltincaba M, Oguz B, Akata D, Ozmen M, Akhan O. CT findings of lymphoma with peritoneal, omental and mesenteric involvement: Peritoneal lymphomatosis. Eur J Radiol. 2009;71:313–7. doi: 10.1016/j.ejrad.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 6.Liang QL, Shi HZ, Wang K, Qin SM, Qin XJ. Diagnostic accuracy of adenosine deaminase in tuberculous pleurisy: A meta-analysis. Respir Med. 2008;102:744–54. doi: 10.1016/j.rmed.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Madan K, Singh N, Das A, Behera D. Pleural tuberculosis following lung cancer chemotherapy: A report of two cases proven pathologically by pleural biopsy. BMJ Case Rep 2013. 2013 doi: 10.1136/bcr-2012-008196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greco S, Girardi E, Masciangelo R, Capoccetta GB, Saltini C. Adenosine deaminase and interferon gamma measurements for the diagnosis of tuberculous pleurisy: A meta-analysis. Int J Tuberc Lung Dis. 2003;7:777–86. [PubMed] [Google Scholar]


