Abstract
AIM: To understand factors associated with quality of life (QOL), examine types of QOL instruments, and determine need for further improvements in QOL assessment.
METHODS: The method used databases (Pubmed, Google scholar) and a bibliographic search using key words QOL, end stage renal disease, Hemodialysis, Peritoneal dialysis, instruments to measure QOL, patients and qualitative/quantitative analysis published during 1990 to June 2014. Each article was assessed for sample size, demographics of participants, study design and type of QOL instruments used. We used WHO definition of QOL.
RESULTS: For this review, 109 articles were screened, out of which 65 articles were selected. Out of 65 articles, there were 19 reports/reviews and 12 questionnaire manuals. Of the 34 studies, 82% were quantitative while only 18% were qualitative. QOL instruments measured several phenomenon such as physical/psychological health, effects and burdens of kidney disease, social support etc. those are associated with QOL. Few studies looked at spiritual beliefs, cultural beliefs, personal concerns, as per the WHO definition. Telemedicine and Palliative care have now been successfully used however QOL instruments seldom addressed those in the articles reviewed. Also noticed was that longitudinal studies were rarely conducted. Existing QOL instruments only partially measure QOL. This may limit validity of predictive power of QOL.
CONCLUSION: Culture and disease specific QOL instruments that assess patients’ objective and subjective experiences covering most aspects of QOL are urgently needed.
Keywords: Quality of Life, Hemodialysis, Peritoneal dialysis, Patient, End stage renal disease, Quality of life instruments
Core tip: Quality of life (QOL) in end stage renal disease patients is an important outcome measure. This study tried to understand the dimensions of various QOL instruments and association of various risk factors with QOL. Since each instrument measures specific aspect of QOL, use of any one of these instruments allows studies to measure QOL only partially compromising on the validity of the predictive power of QOL. Furthermore, less attention has been given on conduct of qualitative and longitudinal studies. There is an urgent need to develop disease and culture specific instrument that covers most aspects of QOL.
INTRODUCTION
In medicine most assessments are conducted by laboratory tests or examinations from healthcare workers. Quality of Life (QOL), though equally important to assess the quality and outcomes of medical care, is not routinely measured. QOL instruments measure individual’s own views of his wellbeing. The core components of QOL are physical, functional, psychological/emotional, and work/occupational[1]. This review will discuss QOL of adult end stage renal disease (ESRD) patients. For this review, we used the World Health Organization’s (WHO) definition of QOL which is “individuals’ perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns”. It is a broad ranging concept affected by the person’s complex physical health, psychological state, level of independence, social relationships, personal beliefs and their relationship to salient features of their environment[2]. QOL can be used to gauge health system performance, mortality indicators, and compare health of groups[3].
This review focused on adult ESRD patients since renal disease is a serious illness and treatment is challenging and prolonged. Globally, the estimated prevalence of chronic kidney disease (CKD) (the first four stages out of five) is 7.2% in adults over the age of 30 years[4]. CKD is a major determinant of poor health outcome of noncommunicable diseases affecting 5% to 8% of world’s population[5]. Despite the substantial resources committed to the treatment of ESRD and significant improvements in the quality of dialysis therapy, patients continue to experience significant mortality and morbidity and a reduced quality of life[6]. With improved medication, medical treatment, medical care and health technology, patients may be living longer but are they living a better life? The effect of the treatment is not only measured in terms of survival, but also in terms of well-being. There is an ever expanding body of literature related to various factors that affect QOL, like genetic, environmental, psychosocial, stress, emotional, and co-morbidities. Findings have shown that lower scores on QOL were strongly associated with higher risk of death and hospitalization[7,8] than clinical parameters such as serum albumin levels8 in cases of ESRD patients. It is also noticed that QOL in ESRD is most affected in the physical domains, and nutritional biomarkers are most closely associated with these domains compared to Kt/V (marker of dialysis adequacy), mineral metabolism indices, and inflammatory markers which are poor health related quality of life (HRQOL) correlates[9]. These findings demand more attention towards patients’ essential QOL measures and indicators.
While assessing QOL, both subjective and objective information is necessary since they derive distinct types of information. Objective measures may be more suitable in detecting treatment effects, such as the number of days on dialysis. Subjective information (such as happiness, satisfaction, spiritual and religious beliefs) is also necessary to complete the QOL picture and enhance the interpretation of objective data. Both the illness and the treatment of ESRD influence subjective QOL factors.
Recently (2014), Boudreau JE has talked about the functional definition of concept of QOL by discussing three attributes: (1) the ability to engage in vigorous activities; (2) the ability to engage in social and occupational roles; and (3) the ability to perform activities of daily living (ADL)[10]. Reviews were conducted that included the type of measures, the instrument development process, study sample characteristics, particular quality of life domains, and reliability and validity testing. Some reviews provided an overview of the instruments used and judged the instruments in terms of their comprehensiveness, reliability, and validity[11]. Few studies sought to establish which domains of QOL are most affected by ESRD[9]. Review by Gentile[12] did provide a variety of generic and disease targeted health related QOL instruments for patients suffering from ESRD. Yet, reviews have rarely discussed whether existing QOL instruments have covered both objective and subjective patient experiences as per the WHO definition of QOL.
Based on this background, the aim of this review was to understand the factors associated with QOL of adult ESRD patients, examine the various dimensions that QOL instruments measure, and identify if there is a need to expand the measurements of QOL.
MATERIALS AND METHODS
The search strategy detailed in Figure 1 was used to identify published literature in the English language during the years 1990 to June 2014. The search was conducted during March - June 2014 using the search criteria (key words, year and language) as mentioned in Figure 1. The search was conducted with MEDLINE, PubMed and was further expanded with Google Scholar using the same search criteria mentioned above. Title and abstracts of the studies were checked with the key words to screen the articles. This process generated 109 studies including research papers, reviews, reports and manuals relevant to our scope of interest.
Figure 1.
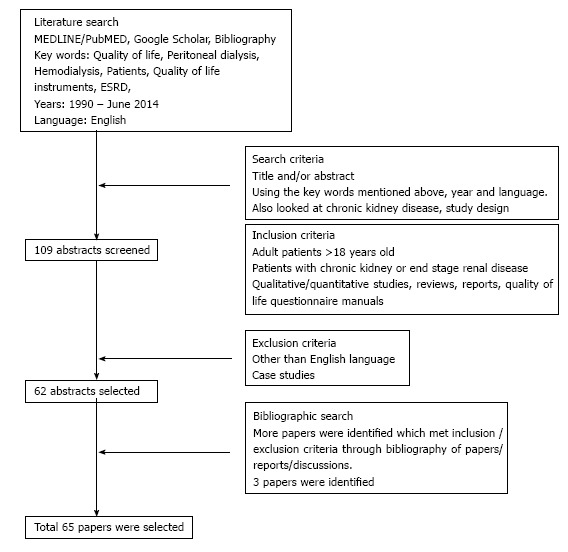
Literature search strategy. Flow chart below shows how the studies were selected for this article.
Inclusion and exclusion criteria (as mentioned in Figure 1) were applied to the selected abstracts for relevance. If the author was not satisfied with the content of the abstract, the full paper was accessed and the same inclusion/exclusion criteria were applied. A total of 62 research papers met the criteria. The bibliography of the research papers was then reviewed to identify additional literature published in English that met the inclusion criteria. Three more research studies were identified by this process. In total, 65 research papers, reports, reviews and quality of life questionnaire manuals were included in this review
These 65 research papers were then arranged into four principal categories as follows: (1) Reports, reviews, published series, discussion articles; (2) Quantitative studies; (3) Qualitative studies; and (4) Quality of life questionnaire manuals (Table 1).
Table 1.
First Author, year of publication, study design and questionnaire used
| Ref. | Study design | |
| Reviews, Published series, Reports, Discussion articles | ||
| Donald[1], 2009 | Published Series article | |
| POFS ABUSE[2], 1997 | WHOQOL Instruments Report | |
| Romero et al[3], 2013 | Discussion article | |
| EpiCast[4], 2014 | Report | |
| Couser et al[5], 2012 | Policy Forum | |
| Obrador et al[6], 2014 | Review | |
| Schatell et al[7], 2012 | Report | |
| Berman et al[9], 2008 | Systematic Review | |
| Edgell et al[11], 1996 | Review | |
| Gentile et al[12], 2003 | Review | |
| Kimmel et al[21], 2006 | Review | |
| Johansen[30], 2007 | Report | |
| Kutner[31], 2010 | Rehabilitation Report | |
| Valderrábano et al[46], 2001 | In-depth Review | |
| Fleck et al[53], 2007 | Discussion | |
| Carver et al[57], 1995 | Review | |
| Blinkhorn[61], 2012 | Review | |
| O’Connor et al[64], 2012 | Review | |
| Catania et al[65], 2013 | Report | |
| Quantitative | Study design | Questionnaire used |
| Mapes et al[8] | Longitudinal | KDQOLSF-36 |
| Kao et al[13], 2009 | Cross sectional | SF-36 |
| Abraham et al[14], 2008 | Case control, follow up | WHOQOL-BREF |
| Kimmel et al[15], 2008 | Prospective | Satisfaction with Life Scale (SLS), McGill QOL, Single item |
| Patel et al[16], 2002 | Prospective | McGill QOL, Beck Depression |
| Griva et al[17], 2009 | Cross sectional | SF-36 |
| Elder et al[19], 2008 | Cross sectional, case mix | KDQOLSF-36 |
| Sanner et al[20], 2002 | Cross sectional | SF-36, Nottingham Health Profile |
| Tondra[22], 2014 | Conceptual Framework, CS | Quality of Life Index Dialysis, |
| Mingardi et al[23], 1999 | Prospective | SF-36 |
| Seica et al[24], 2009 | Cross sectional | SF-36, KDQOLSF-36 |
| Bakewell et al[25], 2002 | Longitudinal /intervention | KDQOLSF-36 |
| Theofilou[26], 2012 | Cross sectional/ Observational | WHOQOL-BREF, GHQ-28 |
| Kim et al[28], 2013 | Cross sectional | KDQOLSF-36 |
| White et al[29], 2002 | Retrospective cohort | SF-36 |
| Painter et al[32], 2000 | Experimental/Intervention | SF-36 |
| Ouzouni et al[33], 2009 | RCT | SF-36, Quality of Life Index |
| Agakhani et al[34], 2012 | Case control/comparative | SF-36 |
| Hegazy et al[35], 2013 | Intervention/Pre-post | Karnofsky performance scale |
| Abraham et al[36], 2009 | Prospective, intervention | Karnofsky performance scale |
| Moattari et al[37], 2012 | RCT | SF-12 |
| Brennan et al[38], 2007 | Intervention, report | SF-36 |
| Cukor et al[39], 2013 | RCT | KDQOLSF-36, Beck Depression Inventory |
| Lii et al[40], 2007 | Intervention/Experimental | SF-36 |
| Sathvik et al[52], 2008 | Cross sectional | WHOQOL-BREF |
| Pagels et al[50], 2012 | Cross sectional | SF-36 |
| WHOQOL-SRPB[54], 2005 | Cross cultural/sectional study | WHOQOL-SRPB |
| Yong et al[63], 2009 | Prospective cross sectional | SF-36, Charlson Comorbidity Index |
| Qualitative | ||
| Baudeau et al[10], 2014 | Concept analysis | |
| Fennegan-John et al[18], 2013 | Interviews, FGD | |
| Arabi[41], 2006 | Interview | |
| Rygh et al[59], 2012 | Interviews with patients | |
| Stroetmann et al[60], 2000 | Observational | |
| Jablonski[62], 2007 | Observational | |
| QOL instruments | ||
| Choices for Healthy Outcomes In Caring for End Stage Renal Disease[27] | ||
| Sickness Impact profile[42] | ||
| SF-36[43] | ||
| SF-12[44] | ||
| Nottingham Health Profile[45] | ||
| EQ-5D[47] | ||
| McGill Quality of Life Questionnaire[48] | ||
| GHQ-28[49] | ||
| WHO-BREF[51] | ||
| Dialysis Symptom Index[55] | ||
| KDQOL-SF36[56] | ||
| CKD Questionnaire[58] |
QOL: Quality of life; CKD: Chronic kidney disease.
RESULTS
For this review 109 articles were screened, out of which 65 articles were selected. Out of 65 articles, there were 19 reports/reviews and 12 questionnaire manuals. Of these 34 studies, 82% were quantitative while only 18% were qualitative. Most quantitative studies were cross sectional. Only two studies used longitudinal design.
Association of various factors with QOL and outcome
The treatment for ESRD patients imposes heavy restrictions that affect QOL. QOL usually includes both objective and subjective evaluations of both the positive and negative aspects of life. Researchers have reported demographic, clinical, social, psychological, and treatment related associations with QOL[1].
It has been proven that the patient’s perception is more important than the clinical assessment in determining QOL[15]. Figure 2 illustrates several factors having linear, inverse or no association with QOL. Studies have commented that QOL can be enhanced by intervention techniques as mentioned in Figure 2. The same figure further shows that lower scores on all three summary scores of QOL (physical component summary, mental component summary and kidney disease component summary) were strongly associated with death and hospitalization as revealed by Mapes in DOPPS study[8] (predictive power of QOL).
Figure 2.
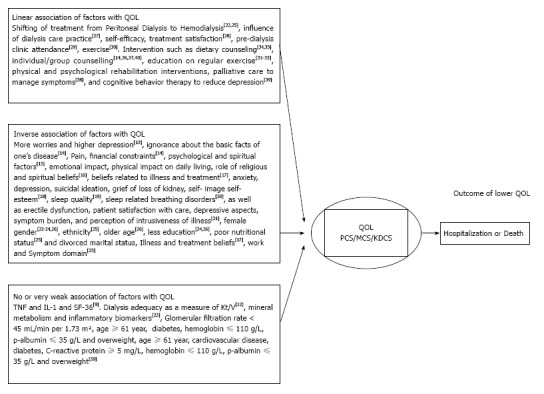
Factors associated with quality of life and predictive power of quality of life. Quality of life (QOL) is assessed based on several factors that show linear / inverse/no relationship with QOL. Based on these relationships QOL predicts Hospitalization or death. QOL: Quality of life; PCS: Physical component summary; MCS: Mental component summary; KDCS: Kidney disease component summary.
Qualitative research
Qualitative research produces rich information that is not possible to get by quantitative research. Qualitative research conducted on ESRD patients has reported some of the themes (subjective measures) for QOL. These themes were physiological impact, impact of treatment, impact on daily life, psychological impact, impact on relationships, social impact and coping responses[20]. Another study came up with three themes and sub themes as: (1) “life restricted” with sub-themes “being tied down”, “feeling left out”, and “doing without”; (2) “staying alive” with sub-themes “love from others”, “accept illness as part of life”, and “trust in God”; and (3) “feeling good” with sub-themes “personal satisfaction” and “being happy”[41].
QOL instruments
Some QOL instruments provide a standard assessment of health. These instruments include questionnaires designed to be applicable for general population such as the Sickness Impact Profile (SIP)[42], the SF-36[43], SF-12[44], the Nottingham Health Profile[45,46] (used for primary care), the European Quality of Life Instrument - EQ-5D[47], the McGill QOL (MQOL)[48] scale and GHQ- 28[49]. Instruments designed by WHO such as WHOQOL[50] WHOQOL-BREF[51,52] are used by researchers. WHOQOL-SRPB[53,54] is also used to assess spiritual, religious and personal beliefs (SRPB) within quality of life. In the CHOICE study, the research team is conducting several research projects for the development of patient-centered instruments for assessment of health-related quality of life[27].
There are three disease-targeted questionnaires developed for ESRD patients undergoing dialysis. Dialysis Symptom Index (DSI)[55], the Kidney Disease Quality of Life instrument Short Form- KDQOL-SF36[56]. The Choices for Healthy Outcomes in Caring for End-Stage Renal Disease ([ESRD] CHOICE)[27]. Additionally, few researchers use The Kidney Disease Questionnaire - KDQ[58], Renal Quality of Life Health Profile (RQLP), and Quality of Life Index-D. Each QOL tool covers a number of domains (measurements of different characteristics) and they measure quantitative outcomes13. Culture specific validation has been reported for these instruments in many countries. Every instrument is scored on different domains. There is no one instrument that measures all the domains or most of the patients’ perceptions towards their disease or life. The most common instruments used were SF-36 and KDQOL. Data collected by administering these questionnaires was analyzed using quantitative methods. Most studies use descriptive cross sectional design[57]. In this review, out of 65 articles, 48% had used SF-36, 20% had used KDQOL, 16% had used WHOQOL and the remaining 16% had used GHQ-12, GHQ-28, McGill, DSI, QOLI (Table 1).
DISCUSSION
Researchers have reported a linear or inverse relationship between factors that improve or lower QOL. Researchers have defined attributes[10] or used frameworks[22] or models[3] that encompasses certain aspects of QOL, such as demographic data, information on diet, treatments and their impact, anthropometric biomarkers[50], and data related to mental health such as depression or anxiety. Most of the existing QOL instruments derived mainly quantitative information. Since QOL is subjective, more qualitative evidence needs to be gathered, assessed and understood. Although it is expensive and time consuming, incorporating qualitative methods will generate rich information.
Considering the WHO definition of QOL and its multidimensional aspects, the instruments and models reviewed only partly assess QOL. Some of the domains were omitted, such as patients’ thinking, learning, memory concentration, self-esteem, patient’s perception about his body image, patient’s feelings about his health and the surrounding environment, patient’s age, patient’s dependence on medication or treatments, financial burden of treatment, and spiritual/religious beliefs[57]. While studies that have used WHO QOL have covered some of the above-mentioned characteristics, they have not specifically covered these in relation to kidney disease. Although Paul Kimmel has commented that there is a need for proper measurements for judging QOL for chronic kidney disease patients[21], not much attention has been given. There remains a need for an instrument that will capture the greatest number of QOL characteristics to get a broader understanding.
The results also reveal the need to conduct more longitudinal studies where researchers are able to detect changes in the characteristics of the population at a group level. Few longitudinal studies were conducted to report the usefulness of these instruments to find improvement in QOL over time. With longitudinal studies it would be possible to detect Minimal Clinically Important Difference (MCID) i.e., a smallest change in treatment outcome that a patient himself would identify as important.
Culture plays a vital role in shaping individual QOL. An individual’s values affects perception of QOL and this can differ between cultures as shown in DOPP study[8].
Furthermore, the current instruments were developed some time ago. [KDQOL-SF36 (1995), KDQOL-36, SF-36 (2002), SF-12, EQ-5D (2004)] Since then (1995), medical technologies (e-health) and medical services have improved. Although telemedicine[59], electronic/digital processes in health, healthcare practice using the Internet, video conferencing with patients, and electronic medical records have been implemented, these services are not evaluated for QOL. For example, there is little published research on telehealth in renal units[61]. Patients generally prefer to stay at home and telecare can extend homecare to peritoneal dialysis patients[60], but use of telehealth is under researched[61]. QOL instruments may be incorporated into telehealth assisted technologies for wider understanding and application.
For those who are not able to receive dialysis treatment, non dialytic management of ESRD seems to be a viable option. Patients managed conservatively had reported high symptom burden underscoring the need for concurrent palliative care[64]. Hence, physicians are now considering palliative care services that specialize in symptom management for ESRD patients[62,63]. This is especially important in frail, illiterate, elderly multi-morbid patients with limited physical activity, where prognosis may not be altered by dialytic therapy. In such scenarios, palliative care will help improve quality of life. Though Catania G. has come up with a frame work to assess QOL with palliative care intervention[65], he has explained the complexity involved in measuring palliative care as an intervention. The existing QOL instruments have rarely looked at palliative care aspects for improvement of patient well-being. Inclusion of newer technologies and therapies measured over time may also help to establish the minimally important differences that would constitute a real change in scores as well as clinically meaningful differences.
Studies have shown that QOL has improved with hemodialysis treatment as compared to peritoneal dialysis[22,25]. Another study has shown that QOL is better for patients treated at home[60]. In most cases peritoneal dialysis treatment is given at home. These two results may look contradictory but they are reported by two different studies. Is it the type of treatment or the place of treatment that affects QOL? It will be interesting to know what will be the result when both aspects are looked at by the same study. When several other factors are studied and included in the model, with the help of statistical analysis it will be possible to identify which factor affects QOL the most. Most instruments do not cover health literacy, which also has an impact on QOL. In the case of illiterate patients, sufficient data may not be available, so pictorial forms of the instruments may help.
Since patient-reported baseline QOL levels provide additional predictive information[7], it is important to consider a patient’s evaluation of their own QOL along with other aspects. A possible limitation of the study is that we were only able to review a portion of the research studies.
In summary, QOL is multidimensional where many indicators are intertwined and that affect person’s overall QOL. Indicators based solely on certain characteristics of the patients pose serious restrictions to the measure of QOL. Ultimately, this may limit the predictive power of QOL. In examining QOL of ESRD patients, much work remains. The challenge for the next decade will be to continue to design a QOL instrument that takes both disease specific and culture specific subjective and objective factors into account so that it would be possible to get the complete assessment of QOL of ESRD patients.
ACKNOWLEDGMENTS
Author would like to acknowledge the contribution of Ms. Abigail Levin Tatake for editing this article for English grammar and clarity.
COMMENTS
Background
Quality of life (QOL) is considered as an important outcome measure. Researchers have claimed that it is even better than clinical parameters. Understanding QOL of end stage renal disease patients is necessary because renal disease is a serious illness and treatment is challenging and prolonged. Though there are various instruments to measure QOL, it is necessary to understand the dimensions used for assessment by these instruments and if there is a need to improve the existing QOL instruments.
Research frontiers
There are several instruments to measure QOL. Each instrument measures certain dimensions of human characteristics. Most of the instruments record objective information and measure QOL quantitatively. Most of the studies use cross sectional design that gives only snap shot information. An instrument designed by WHO measure subjective information but do not assess information related to kidney disease. These instruments rarely record the modern technologies such as telemedicine, e-health, conservative care etc.
Innovations and breakthroughs
There is an urgent need to develop QOL instrument that will try to look at the majority of (objective and subjective) characteristics of patients as well as the effect of new technologies like e-health and therapies like palliative care. QOL instruments, those are currently in use, have been developed some time ago. [KDQOL-SF36 (1995), KDQOL-36, SF-36 (2002), SF-12, EQ-5D (2004)] Since then (1995), medical technologies (e-health) and medical services have improved.
Applications
The newly designed QOL instrument that takes both diseases specific and culture specific, objective and subjective factors into account will help physicians to plan targeted intervention strategies based on strongest and weakest factors that affect QOL. With availability of complete QOL assessment, it will be possible to predict disease outcome effectively.
Terminology
Studies have reported that QOL can be used as an outcome measure in terms of hospitalization and mortality. The strength of this prediction would depend on how rigorously and comprehensively QOL was assessed. This is indicated as validity of the predictive power of QOL.
Peer review
This is an interesting topic.
Footnotes
P- Reviewer: Hammes M, Malhotra DK, Scarpioni R S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
References
- 1.Fellowfield L. What is Quality Of Life. Available from: http://www.medicine.ox.ac.uk/bandolier/painres/download/whatis/WhatisQOL.pdf.
- 2.Fellowfield L WHOQOL. Measuring Quality of Life, Program on Mental Health. Available from: http://www.who.int/mental_health/media/68.pdf.
- 3.Romero M, Vivas-Consuelo D, Alvis-Guzman N. Is Health Related Quality of Life (HRQoL) a valid indicator for health systems evaluation? Springerplus. 2013;2:664. doi: 10.1186/2193-1801-2-664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Available from: www.reportbuyer.com.
- 5.Couser WG, Remuzzi G, Mendis S, Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80:1258–1270. doi: 10.1038/ki.2011.368. [DOI] [PubMed] [Google Scholar]
- 6.Obrador GT, Pereira B. Epidemiology of chronic kidney disease. Wolters Klover. Available from: http://www.uptodate.com/contents/epidemiology-of-chronic-kidney-disease.
- 7.Schatell D, Witten B. Measuring Dialysis Patients’ Health-Related Quality of Life with the KDQOL-36TM. Medical Education Institute, Inc. (608) 833-8033, KDQOL COMPLETE. 2012. Available from: http://www.kdqol-complete.org. [Google Scholar]
- 8.Mapes DL, Bragg-Gresham JL, Bommer J, Fukuhara S, McKevitt P, Wikström B, Lopes AA. Health-related quality of life in the Dialysis Outcomes and Practice Patterns Study (DOPPS) Am J Kidney Dis. 2004;44:54–60. doi: 10.1053/j.ajkd.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 9.Spiegel BM, Melmed G, Robbins S, Esrailian E. Biomarkers and health-related quality of life in end-stage renal disease: a systematic review. Clin J Am Soc Nephrol. 2008;3:1759–1768. doi: 10.2215/CJN.00820208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boudreau JE, Dubé A. Quality of life in end stage renal disease: a concept analysis. CANNT J. 2004;24:12–20. [PubMed] [Google Scholar]
- 11.Edgell ET, Coons SJ, Carter WB, Kallich JD, Mapes D, Damush TM, Hays RD. A review of health-related quality-of-life measures used in end-stage renal disease. Clin Ther. 1996;18:887–938. doi: 10.1016/s0149-2918(96)80049-x. [DOI] [PubMed] [Google Scholar]
- 12.Gentile S, Delarozière JCh, Fernandez C, Tardieu S, Devictor B, Dussol B, Daurès JP, Berland Y, Sambuc R. [Review of quality of life instruments used in end-stage renal disease] Nephrologie. 2003;24:293–301. [PubMed] [Google Scholar]
- 13.Kao TW, Lai MS, Tsai TJ, Jan CF, Chie WC, Chen WY. Economic, social, and psychological factors associated with health-related quality of life of chronic hemodialysis patients in northern Taiwan: a multicenter study. Artif Organs. 2009;33:61–68. doi: 10.1111/j.1525-1594.2008.00675.x. [DOI] [PubMed] [Google Scholar]
- 14.Abraham S, Ramachandran A. Estimation of quality of life in haemodialysis patients. Indian J Pharm Sci. 2012;74:583–587. doi: 10.4103/0250-474X.110624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kimmel PL, Emont SL, Newmann JM, Danko H, Moss AH. ESRD patient quality of life: symptoms, spiritual beliefs, psychosocial factors, and ethnicity. Am J Kidney Dis. 2003;42:713–721. doi: 10.1016/s0272-6386(03)00907-7. [DOI] [PubMed] [Google Scholar]
- 16.Patel SS, Shah VS, Peterson RA, Kimmel PL. Psychosocial variables, quality of life, and religious beliefs in ESRD patients treated with hemodialysis. Am J Kidney Dis. 2002;40:1013–1022. doi: 10.1053/ajkd.2002.36336. [DOI] [PubMed] [Google Scholar]
- 17.Griva K, Jayasena D, Davenport A, Harrison M, Newman SP. Illness and treatment cognitions and health related quality of life in end stage renal disease. Br J Health Psychol. 2009;14:17–34. doi: 10.1348/135910708X292355. [DOI] [PubMed] [Google Scholar]
- 18.Finnegan-John J, Thomas VJ. The psychosocial experience of patients with end-stage renal disease and its impact on quality of life: findings from a needs assessment to shape a service. ISRN Nephrol. 2013;2013:308986. doi: 10.5402/2013/308986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elder SJ, Pisoni RL, Akizawa T, Fissell R, Andreucci VE, Fukuhara S, Kurokawa K, Rayner HC, Furniss AL, Port FK, et al. Sleep quality predicts quality of life and mortality risk in haemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS) Nephrol Dial Transplant. 2008;23:998–1004. doi: 10.1093/ndt/gfm630. [DOI] [PubMed] [Google Scholar]
- 20.Sanner BM, Tepel M, Esser M, Klewer J, Hoehmann-Riese B, Zidek W, Hellmich B. Sleep-related breathing disorders impair quality of life in haemodialysis recipients. Nephrol Dial Transplant. 2002;17:1260–1265. doi: 10.1093/ndt/17.7.1260. [DOI] [PubMed] [Google Scholar]
- 21.Kimmel PL, Patel SS. Quality of life in patients with chronic kidney disease: focus on end-stage renal disease treated with hemodialysis. Semin Nephrol. 2006;26:68–79. doi: 10.1016/j.semnephrol.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 22.Tondra I. Quality of Life in patients with ESRD on hemodialysis. Available from: http: //www.lagrange.edu/resources/pdf/citations/2011/16_Ivey_and_Lane_Nursing.pdf.
- 23.Mingardi G, Cornalba L, Cortinovis E, Ruggiata R, Mosconi P, Apolone G. Health-related quality of life in dialysis patients. A report from an Italian study using the SF-36 Health Survey. DIA-QOL Group. Nephrol Dial Transplant. 1999;14:1503–1510. doi: 10.1093/ndt/14.6.1503. [DOI] [PubMed] [Google Scholar]
- 24.Seica A, Segall L, Verzan C, Văduva N, Madincea M, Rusoiu S, Cristea S, Stefan M, Serbănescu D, Morosanu P, et al. Factors affecting the quality of life of haemodialysis patients from Romania: a multicentric study. Nephrol Dial Transplant. 2009;24:626–629. doi: 10.1093/ndt/gfn506. [DOI] [PubMed] [Google Scholar]
- 25.Bakewell AB, Higgins RM, Edmunds ME. Quality of life in peritoneal dialysis patients: decline over time and association with clinical outcomes. Kidney Int. 2002;61:239–248. doi: 10.1046/j.1523-1755.2002.00096.x. [DOI] [PubMed] [Google Scholar]
- 26.Theofilou P. The Impact of Socio Demographic and Psychological variables on QOL of patients with Renal Disease: Findings of a cross sectional study in Greece. WJNU. 2012;I:101–106. [Google Scholar]
- 27.Powe NR, Klag MJ, Sadler JH, Anderson GF, Bass EB, Briggs WA, Fink NE, Levey AS, Levin NW, Meyer KB, et al. Choices for Healthy Outcomes In Caring for End Stage Renal Disease. Seminars in Dialysis. 1996;9:9–11. [Google Scholar]
- 28.Kim JY, Kim B, Park KS, Choi JY, Seo JJ, Park SH, Kim CD, Kim YL. Health-related quality of life with KDQOL-36 and its association with self-efficacy and treatment satisfaction in Korean dialysis patients. Qual Life Res. 2013;22:753–758. doi: 10.1007/s11136-012-0203-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.White CA, Pilkey RM, Lam M, Holland DC. Pre-dialysis clinic attendance improves quality of life among hemodialysis patients. BMC Nephrol. 2002;3:3. doi: 10.1186/1471-2369-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johansen KL. Exercise in the end-stage renal disease population. J Am Soc Nephrol. 2007;18:1845–1854. doi: 10.1681/ASN.2007010009. [DOI] [PubMed] [Google Scholar]
- 31.Centre for Rehabilitation Research Information and Exchange (CIRRIE), 2010 [Google Scholar]
- 32.Painter P, Carlson L, Carey S, Paul SM, Myll J. Physical functioning and health-related quality-of-life changes with exercise training in hemodialysis patients. Am J Kidney Dis. 2000;35:482–492. doi: 10.1016/s0272-6386(00)70202-2. [DOI] [PubMed] [Google Scholar]
- 33.Ouzouni S, Kouidi E, Sioulis A, Grekas D, Deligiannis A. Effects of intradialytic exercise training on health-related quality of life indices in haemodialysis patients. Clin Rehabil. 2009;23:53–63. doi: 10.1177/0269215508096760. [DOI] [PubMed] [Google Scholar]
- 34.Aghakhani N, Samadzadeh S, Mafi TM, Rahbar N. The impact of education on nutrition on the quality of life in patients on hemodialysis: a comparative study from teaching hospitals. Saudi J Kidney Dis Transpl. 2012;23:26–30. [PubMed] [Google Scholar]
- 35.Hegazy IS, El Raghy HA, Abdel-Aziz SB, Elhabashi EM. Study of the effect of dietary counselling on the improvement of end-stage renal disease patients. East Mediterr Health J. 2013;19:45–51. [PubMed] [Google Scholar]
- 36.Abraham S, Venu A, Chandran PM, Raman S. Assessment of quality of life in patients on hemodialysis and impact of counseling. Saudi J Kidney Dis Transpl. 2012;23:853–857. doi: 10.4103/1319-2442.100875. Available from: http: //www.sjkdt.org/text.asp?2012/23/5/953/100875. [DOI] [PubMed] [Google Scholar]
- 37.Moattari M, Ebrahimi M, Sharifi N, Rouzbeh J. The effect of empowerment on the self-efficacy, quality of life and clinical and laboratory indicators of patients treated with hemodialysis: a randomized controlled trial. Health Qual Life Outcomes. 2012;10:115. doi: 10.1186/1477-7525-10-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brennan F, Brown M. The Evolving integration of Palliative Care into End Stage Renal Failure Management, St George Hospital Sydney, Australia. Available from: http: //www.palliativecare.org.au/Portals/46/Together conference/D3 Frank Brennan.pdf.
- 39.Cukor D, Ver Halen N, Asher DR, Coplan JD, Weedon J, Wyka KE, Saggi SJ, Kimmel PL. Psychosocial intervention improves depression, quality of life, and fluid adherence in hemodialysis. J Am Soc Nephrol. 2014;25:196–206. doi: 10.1681/ASN.2012111134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lii YC, Tsay SL, Wang TJ. Group intervention to improve quality of life in haemodialysis patients. J Clin Nurs. 2007;16:268–275. doi: 10.1111/j.1365-2702.2007.01963.x. [DOI] [PubMed] [Google Scholar]
- 41.Al-Arabi S. Quality of life: subjective descriptions of challenges to patients with end stage renal disease. Nephrol Nurs J. 2006;33:285–292. [PubMed] [Google Scholar]
- 42.Sickness impact profile Available from: http: //www.parqol.com/page.cfm?id=92 [Google Scholar]
- 43.Ware JE. SF-36 Health Survey Update. Available from: http: //www.sf-36.org/tools/sf36.shtml. [DOI] [PubMed]
- 44. Available from: http: //www.sf-36.org/tools/sf12.shtml.
- 45. Available from: http: //www.primarycarecore.org/PDF/247.pdf.
- 46.Valderrábano F, Jofre R, López-Gómez JM. Quality of life in end-stage renal disease patients. Am J Kidney Dis. 2001;38:443–464. doi: 10.1053/ajkd.2001.26824. [DOI] [PubMed] [Google Scholar]
- 47.Gusi N, Olivares PR, Rajendram R. The EQ-5D Health Related Quality Of Life Questionnaire, Handbook of Disease Burden and Quality Of Life Measure [Internet] 2010. Available from: http: //link.springer.com/referenceworkentry/10.1007/978-0-387-78665-0_5.
- 48.McGill RC. Quality Of Life Questionnaire [Internet] Available from: http: //www.who.int/mental_health/media/68.pdf.
- 49. Available from: http: //www.scireproject.com/outcome-measures-new/scaled-general-health-questionnaire-28-ghq-28.
- 50.Pagels AA, Söderkvist BK, Medin C, Hylander B, Heiwe S. Health-related quality of life in different stages of chronic kidney disease and at initiation of dialysis treatment. Health Qual Life Outcomes. 2012;10:71. doi: 10.1186/1477-7525-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 52.Sathvik BS, Parthasarathi G, Narahari MG, Gurudev KC. An assessment of the quality of life in hemodialysis patients using the WHOQOL-BREF questionnaire. Indian J Nephrol. 2008;18:141–149. doi: 10.4103/0971-4065.45288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fleck MP, Skevington S. Explaining the meaning of the WHOQOL-SRPB. Rev Psiquiatr Clín. 2007:34 suppl1. [Google Scholar]
- 54.A cross-cultural study of spirituality, religion, and personal beliefs as components of quality of life. Soc Sci Med. 2006;62:1486–1497. doi: 10.1016/j.socscimed.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 55. Available from: http: //www.kidneysupportivecare.org/Files/DialysisSymptomIndex.aspx.
- 56.Hays RD. Kidney Disease Quality Of Life Questionnaire short form, A manual for use and scoring. Version 1.3. RAND; 1997. [Google Scholar]
- 57.Carver DJ, Rockwood KJ. Evaluation of methods for measuring quality of life in the elderly with end stage renal disease. Geriatr Nephrol Urol. 1995;4:165–175. [Google Scholar]
- 58. Available from: http: //www.kidney-cares.org/ckd-question.html.
- 59.Rygh E, Arild E, Johnsen E, Rumpsfeld M. Choosing to live with home dialysis-patients’ experiences and potential for telemedicine support: a qualitative study. BMC Nephrol. 2012;13:13. doi: 10.1186/1471-2369-13-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stroetmann KA, Gruetzmacher P, Stroetmann VN. Improving quality of life for dialysis patients through telecare. J Telemed Telecare. 2000;6 Suppl 1:S80–S83. doi: 10.1258/1357633001934249. [DOI] [PubMed] [Google Scholar]
- 61.Blinkhorn TM. Telehealth in nephrology health care: a review. RSAJ. 2012;8 suppl3:132–139. [Google Scholar]
- 62.Jablonski A. Level of Symptom Relief and the Need for Palliative Care in the Hemodialysis Population. JHPN. 2007;9:50–58. [Google Scholar]
- 63.Yong DS, Kwok AO, Wong DM, Suen MH, Chen WT, Tse DM. Symptom burden and quality of life in end-stage renal disease: a study of 179 patients on dialysis and palliative care. Palliat Med. 2009;23:111–119. doi: 10.1177/0269216308101099. [DOI] [PubMed] [Google Scholar]
- 64.O’Connor NR, Kumar P. Conservative management of end-stage renal disease without dialysis: a systematic review. J Palliat Med. 2012;15:228–235. doi: 10.1089/jpm.2011.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Catania G, Costantini M, Beccaro M, Bagnasco A, Sasso L. Does quality of life assessment in palliative care look like a complex screening program? Health Qual Life Outcomes. 2013;11:7. doi: 10.1186/1477-7525-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


