Abstract
Aim:
To report the long term refractive, visual and structural outcome post-laser for zone 1 aggressive posterior retinopathy of prematurity (AP-ROP).
Materials and Methods:
A retrospective analysis was performed of refractive status of premature infants with zone 1 AP-ROP who underwent laser photocoagulation from 2002 to 2007 and followed up till 2013. Once the disease regressed, children were followed up six monthly with detailed examination regarding fixation pattern, ocular motility, nystagmus, detailed anterior segment and posterior segment examination, and refractive status including best corrected visual acuity.
Results:
Forty-eight eyes of 25 infants were included in the study. Average follow-up was 6.91 years (range, 3.8-9.5years) after laser treatment. Astigmatism was noted in 43 out of 48 eyes (89.6%). Two eyes had simple myopia whereas three eyes had no refractive error.
Conclusion:
After successful laser treatment for zone 1 retinopathy of prematurity (ROP), 94% of our cases developed refractive error. Although most had a favorable anatomical and visual outcome, long-term follow-up even after a successful laser treatment in ROP was necessary.
Keywords: Retinopathy of prematurity, refractive outcome, zone 1
Introduction
Retinopathy of prematurity (ROP) is a potentially blinding vasoproliferative retinopathy seen in premature infants with low birth weight. Blindness from ROP is a very significant problem, with an incidence of 8% in developed countries[1] and 40% in the developing countries.[2]
Evolution of laser treatment for ROP was associated with better structural and functional outcome compared to that for eyes treated with cryotherapy.[3] There are multiple reports of use of various lasers for threshold ROP with good structural and long-term refractive outcome.[4,5,6,7] However, there are no reports on long-term refractive outcome of zone 1 disease. Our data represents long term refractive and structural outcome for zone 1 ROP.
Materials and Methods
It is an interventional retrospective case series of premature infants with zone 1 aggressive posterior ROP (AP-ROP) who underwent laser photocoagulation, during the study period from 2002 to 2007. Data was analyzed in 2013. The study was approved by the ethics committee of our institute. All infants weighing ≤1800 g or with gestational age ≤34 weeks and those infants weighing >1800 g with an unstable course were screened for ROP. All infants with zone 1 AP-ROP, which regressed after laser treatment, were included in the study. Laser used was diode 810 nm (Oculight SLx, Iridex Co, LA, USA). Power settings were titrated to achieve a gray-white burn of moderate intensity, and spots were applied in a confluent manner to cover the entire avascular retina from the ridge to ora serrata. All lasers were performed under topical anesthesia with an anesthetist on standby. Treated eyes were followed up closely, often weekly or more frequently, for signs of regression or need for further laser. Once ROP regressed, children were followed up six monthly with detailed examination regarding fixation pattern, ocular motility, nystagmus, detailed anterior segment and posterior segment examination, and refractive status including best corrected visual acuity (BCVA). Spherical equivalent (SE) was calculated for all eyes with compound myopic astigmatism using the formula SE = Sphere + ½ Cylinder. High myopia was defined as spherical correction ≥ −6 diopter (D). Astigmatism was calculated in plus cylinder form and classified as with-the-rule (WTR) 75°-105°, against-the-rule (ATR) 0°-15° and 165°-180° and oblique (OBL) 16°-74° and 106°-164°. Astigmatism was defined as cylindrical correction ≥1 D whereas high astigmatism was defined as cylindrical correction ≥2 D. We defined good visual outcome as ≥6/12 on Snellen's chart.[4] Spherical equivalent of the refractive error and the degree and axis of astigmatism were evaluated.
Results
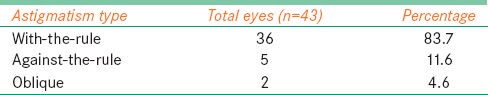
Forty-eight eyes of 25 infants with zone 1 AP-ROP were included in the study, of which 15 were males and 10 females. Mean birth weight was 1509.6 g (range, 850-2080 g) and mean gestational age was 32 weeks (range, 28-35 weeks). Average post-conceptional age at laser was 35.6 weeks. The average laser spots were 3261 spots (range, 800-6416). One patient needed additional cryotherapy to control the progression. Mean follow-up period was 6.91 years (range, 3.8-9.5 years). Three eyes had no refractive error. Two eyes had simple myopia. The average spherical equivalent in right eye was − 6.14 D (range, −18.5-1.25 D) and in left eye was − 5.11 D (range, −18.75-0.5 D). Overall astigmatism was seen in 43 out of 48 eyes (89.6%). All 43 children had a myopic astigmatism; 36 had with-the-rule (WTR) astigmatism, five eyes had against-the-rule (ATR) astigmatism, and two eyes had oblique astigmatism (16°-74° and 106°–164°) [Table 1].
Table 1.
Type of astigmatism
Thirty-nine out of 43 eyes (90.7%) had astigmatism ≥1 D, of which 21 (48.8%) had astigmatism ≥2 D. The average astigmatism in right eye was − 2.08 D (range, −4.0-−0.5 D) and in left eye was − 1.78 D (range, −4–−0.5 D).
Anisometropia ≥1 D was seen in 12 eyes (27.9%) whereas eight eyes (18.6%) had anisometropia ≥2 D. The visual outcome was good with BCVA of 6/6 in five eyes and ≥6/12 in 39 eyes (81%) on Snellen's chart.
Two cases had poor visual outcome. One infant had disc pallor in both eyes with nystagmus and another infant with birth weight of 1690 g and gestational age of 31 weeks developed very high myopia (SE both eyes: −18.5 D) with poor visual outcome. One child required additional cryotherapy with laser to control the vascular process and ended up having nystagmus with pale disc. This child had a birth weight of 1230 g and gestational age of 29 weeks. Coming to structural outcome, one eye developed fibrous proliferation with disc dragging while two eyes developed lamellar cataract.
Discussion
Our study presented the visual outcome and refractive status over a period of 6.91 years in infants treated with laser photocoagulation for zone 1 ROP. Majority of our patients had favorable anatomical and visual outcomes.
This study showed that most of the children had a myopic refraction, with mean spherical equivalent in right eye was −6.14 D (range, −18.5-1.25 D) and in left eye was − 5.11 D (range, −18.75-0.5 D). The visual outcome was good, with BCVA ≥6/12 on Snellen's chart seen in 81% children. In a study using diode laser for threshold ROP by Yang et al.,[4] 65.5% eyes achieved ≥6/12 vision. Of all eyes, 77% were myopic with mean SE of −3.87 D and 16.7% of them had myopia ≥6 D over a mean follow-up of 7.8 years. McLoone et al.[5] reported similar results with 50% of their laser-treated eyes being myopic and 35% having myopia >4 D with diode laser in children with threshold ROP with a mean follow up of 11 years.
In a study using argon laser photocoagulation for threshold ROP by Ospina et al.,[8] at a follow-up of 5 years, 30 eyes (71.4%) had a BCVA of 20/40 or better. In all, 26 (62%) eyes were myopic and the overall mean spherical equivalent was −4.95 D. In a study with 1 year follow-up of patients with laser-treated threshold ROP by Dhawan et al. in 2008,[6] mean refractive error with SE −4.71 D was seen, with myopia occurring in 80.43% of eyes.
It is known that most babies with ROP subsequently become myopic.[9] This myopic tendency is augmented by both cryotherapy and laser treatment, but its mechanism is controversial. Knight Nonan and O’Keefe in a three-year nonrandomized retrospective study demonstrated lower myopia following laser treatment.[10] This was confirmed by other studies, the most important being the 10-year prospective nonrandomized trial by Ng et al.[3] and Kent et al.,[11] which compared both the treatments and found less myopia in the laser-treated eyes. Cryotherapy-treated eyes had shallower anterior chamber depth and thicker lenses with increased axial length compared to laser-treated eyes. Cryotherapy causes larger areas of chorioretinal adhesion and destruction of normal choroidal architecture, which changes the scleral structure, making it susceptible to stretching, leading to high myopia with cryotherapy than with laser. The greater incidence of myopia in ROP is mostly associated with lens thickness and lens power with lesser contribution from corneal steepness and axial length and a more forward position of the lens center. Evidence of altered anterior segment development in ROP, as shown by the increased lens thickness with shallow anterior chamber depth and maintenance of anterior segment depth, leads to high myopia in these infants.[12] Also, it has been shown that spontaneously regressed ROP has lesser myopia compared to treatment groups.[13] Only one study by Kieselbach et al.[7] showed predominant hypermetropia seen post laser photocoagulation for ROP. Wani et al.[14] had unfavorable structural outcome in 7.4% eyes and poor visual outcome (visual acuity <20/40) in 47% eyes. They found zone I disease as the significant risk factor for unfavorable structural outcome (P < 0.0001). Katoch D[15] et al. in a retrospective review of 36 infants (69 eyes) with Type 1 pre-threshold ROP treated with laser, reported myopia in nearly one-fourth of the eyes. Harder et al.[16] compared refractive outcome between intravitreal bevacizumab and conventional retinal laser group and found that at a one-year follow-up, bevacizumab group led to less myopization and less astigmatism.
In our study, overall high astigmatism of ≥2.0 D was seen in 48.8% eyes. WTR astigmatism was seen in 36 eyes (83.7%) and ATR in five eyes (11.6%) and two eyes (4.6%) had oblique astigmatism. A study by Davitt et al.[17] in patients under Early Treatment for ROP (ETROP) study revealed that astigmatism was not influenced by zone of acute phase ROP, presence of plus disease, or retinal residua. Most often the eyes had WTR astigmatism, similar to our study. In our study, 43% developed astigmatism of ≥1 D and 20% had ≥2 D. It has been reported that most preterm infants have WTR astigmatism.[18,19] Several studies have shown that there is no difference in the prevalence of astigmatism between cryotherapy and laser photocoagulation groups.[10,20] The only difference is that patients receiving cryotherapy are more likely to have ATR astigmatism than those receiving laser photocoagulation.[20] The one case that required additional cryotherapy developed ATR astigmatism.
In our study, anisometropia ≥1 D was seen in 12 eyes (27.9%) whereas eight eyes (18.6%) had anisometropia ≥2 D. In the study by Yang et al.,[4] anisometropia was seen in 46.7% of patients. The presence of anisometropia was a significant risk factor associated with poor visual outcome ≤6/15 in laser-treated ROP.
Various types of lasers with various delivery systems have been tried for ROP treatment with good success.[4,6,7,8,21,22,23] Complications observed with laser treatment include corneal edema, anterior segment ischemia, vitreous hemorrhage, posterior synechiae, cataract, and macular ectopia. Others include abnormal liquefied vitreous with fibrillar condensation,[24] fibrovascular organization,[25] and subretinal haemorrhages.[26] Also, changes in retinal vessel diameter,[27] slight constriction of the peripheral visual fields,[28] and angle closure glaucoma[29] have been documented. Our case series showed none of the major complications, except fibrous proliferation in one case which was more due to progression of disease and lamellar cataract in both eyes of one child.
The main limitation of our study is that it is retrospective and we have not assessed progression of refractive error over the follow-up period; only the final follow-up refraction was used for analysis. Since all eyes were treated, there was no comparative group to assess refractive and visual outcome with untreated eyes. Thus pre-existing myopia and laser-induced myopia could not be classified separately.
In conclusion, majority of our patients treated with laser photocoagulation for zone 1 AP-ROP had favorable anatomical and visual outcome at an average follow-up of 6.91 years. Anisometropia and advanced refractive error are common causes of impaired visual function in these patients and emphasize the need for a long-term follow-up even after a successful laser treatment in ROP.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Jacobson L, Fernell E, Broberger U, Ek U, Gillberg C. Children with blindness due to retinopathy of prematurity- a population based study. Perinatal data, neurological and ophthalmological outcome. Dev Med Child Neurol. 1998;40:155–9. doi: 10.1111/j.1469-8749.1998.tb15439.x. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert C, Rahi J, Eckstein M, O’sullivan J, Foster A. Retinopathy of prematurity in middle income countries. Lancet. 1997;350:12–4. doi: 10.1016/S0140-6736(97)01107-0. [DOI] [PubMed] [Google Scholar]
- 3.Ng EY, Cannolly BP, McNamara JA, Regillo CD, Vander JF, Tasman W. A comparison of laser photocoagulation with cryotherapy for threshold ROP at 10 years: Part 1. Visual function and structural outcome. Ophthalmology. 2002;109:928–34. doi: 10.1016/s0161-6420(01)01017-x. [DOI] [PubMed] [Google Scholar]
- 4.Yang CS, Wang AG, Sung CS, Hsu WM, Lee FL, Lee SM. Long-term visual outcomes of laser-treated threshold retinopathy of prematurity: A study of refractive status at 7 years. Eye. 2010;24:14–20. doi: 10.1038/eye.2009.63. [DOI] [PubMed] [Google Scholar]
- 5.McLoone E, O’Keefe M, McLoone S, Lanigan B. Long term functional and structural outcomes of laser therapy for retinopathy of prematurity. Br J Ophthalmol. 2006;90:754–9. doi: 10.1136/bjo.2005.068304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhawan A, Dogra M, Vinekar A, Gupta A, Dutta S. Structural sequelae and refractive outcome after successful laser treatment for threshold retinopathy of prematurity. J Pediatr Ophthalmol Strabismus. 2008;45:356–61. doi: 10.3928/01913913-20081101-02. [DOI] [PubMed] [Google Scholar]
- 7.Kieselbach GF, Ramharter, Baldissera I, Kralinger MT. Laser photocoagulation for retinopathy of prematurity: Structural and functional outcome. Acta Ophthalmol Scand. 2006;84:21–6. doi: 10.1111/j.1600-0420.2005.00548.x. [DOI] [PubMed] [Google Scholar]
- 8.Ospina LH, Lyons CJ, Matsuba C, Jan J, Mc Cormick AQ. Argon laser photocoagulation for retinopathy of prematurity: Long-term outcome. Eye. 2005;19:1213–8. doi: 10.1038/sj.eye.6701729. [DOI] [PubMed] [Google Scholar]
- 9.Nissenkorn I, Yassur Y, Mashkowski D, Sherf I, Ben-Sira I. Myopia in premature babies with and without retinopathy of prematurity. Br J Ophthalmol. 1983;67:170–3. doi: 10.1136/bjo.67.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knight Nonan D, O’Keefe M M. Refractive outcome in eyes with retinopathy of prematurity treated with cryotherapy or diode laser: 3 year follow up. Br J Ophthalmol. 1996;80:998–1001. doi: 10.1136/bjo.80.11.998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kent D, Pennie F, Laws D, White S, Clarke D. The influence of retinopathy of prematurity on ocular growth. Eye. 2000;14:23–9. doi: 10.1038/eye.2000.6. [DOI] [PubMed] [Google Scholar]
- 12.Garcia-Valenzuela E, Kaufman LM. High myopia associated with retinopathy of prematurity is primarily lenticular. J AAPOS. 2005;9:121–8. doi: 10.1016/j.jaapos.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 13.Sahni J, Subhedar NV, Clark D. Treated threshold stage 3 versus spontaneously regressed subthreshold stage 3 ROP: A study of motility, refractive and anatomical outcomes at 6 months and 36 months. Br J Ophthalmol. 2005;89:154–9. doi: 10.1136/bjo.2004.045815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wani VB, Sabti KA, Kumar N, Raizada S, Kandari JA, Harbi MA, et al. Structural and functional results of indirect diode laser treatment for retinopathy of prematurity from 1999 to 2003 in Kuwait. Clin Ophthalmol. 2013;7:271–8. doi: 10.2147/OPTH.S38915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katoch D, Sanghi G, Dogra MR, Beke N, Gupta A. Structural sequelae and refractive outcome 1 year after laser treatment for type 1 prethreshold retinopathy of prematurity in Asian Indian eyes. Indian J Ophthalmol. 2011;59:423–6. doi: 10.4103/0301-4738.86306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harder BC, Schlichtenbrede FC, von Baltz S, Jendritza W, Jendritza B, Jonas JB. Intravitreal Bevacizumab for Retinopathy of Prematurity: Refractive Error Results. Am J Ophthalmol. 2013;155:1119–24. doi: 10.1016/j.ajo.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 17.Davitt BV, Dobson V, Quinn GE, Hardy RJ, Tung B, Good WV Early Treatment for Retinopathy of Prematurity Cooperative Group. Astigmatism in the early treatment of retinopathy of prematurity study. Ophthalmology. 2009;116:332–9. doi: 10.1016/j.ophtha.2008.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saunders KJ, McCulloch DL, Shepherd AJ, Wilkinson AG. Emmetropisation following preterm birth. Br J Ophthalmol. 2002;86:1035–40. doi: 10.1136/bjo.86.9.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Varughese S, Varghese RM, Gupta N, Ojha R, Sreenivas V, Puliyel JM. Refractive erroe at birth and its relation to gestational age. Curr Eye Res. 2005;30:423–8. doi: 10.1080/02713680590959295. [DOI] [PubMed] [Google Scholar]
- 20.Al- Ghamdi A, Albiani DA, Hodge WG, Clarke WN. Myopia and astigmatism in retinopathy of prematurity after treatment with cryotherapy or laser photocoagulation. Can J Ophthalmol. 2004;39:521–5. doi: 10.1016/s0008-4182(04)80142-x. [DOI] [PubMed] [Google Scholar]
- 21.Lira RP, Calheiros AB, Barbosa MM, Oliveira CV, Viana SL, Lima DC. Efficacy and safety of green laser photocoagulation for threshold ROP. Arg Bras Ophtalmol. 2008;71:49–51. doi: 10.1590/s0004-27492008000100010. [DOI] [PubMed] [Google Scholar]
- 22.Kobylarz J, Pinowarczyk A, Romanowska-Dixon B. Diode laser photocoagulation for retinopathy of prematurity-outcomes in one year observation. Klin Oczna. 2006;108:36–8. [PubMed] [Google Scholar]
- 23.Davis AR, Jackson H, Trew D, McHugh JD, Aclimandos WA. Transscleral diode laser in the treatment of retinopathy of prematurity. Eye. 1999;13:571–6. doi: 10.1038/eye.1999.141. [DOI] [PubMed] [Google Scholar]
- 24.Hikichi T, Nomiyama G, Ikeda H, Yoshida A. Vitreous changes after treatment of retinopathy of prematurity. Jpn J Ophthalmol. 1999;43:543–5. doi: 10.1016/s0021-5155(99)00108-2. [DOI] [PubMed] [Google Scholar]
- 25.Hartnett ME, McColm JR. Fibrovascular organization in the vitreous following laser for retinopathy of prematurity. Retina. 2006;26:S24–31. doi: 10.1097/01.iae.0000244286.56133.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marvofrides EC, Berrocal AM, Murray TG. Development of multiple subretinal haemorrhages during diode laser supplementation for retinopathy of prematurity. J Pediatric Ophthalmol Strabismus. 2006;43:110–3. doi: 10.3928/0191-3913-20060301-13. [DOI] [PubMed] [Google Scholar]
- 27.Johnson KS, Mills MD, Karp KA, Grunwald JE. Quantitative analysis of retinal vessel diameter reduction after photocoagulation treatment for retinopathy of prematurity. Am J Ophthalmol. 2007;143:1030–2. doi: 10.1016/j.ajo.2007.01.058. [DOI] [PubMed] [Google Scholar]
- 28.McLoone E, O’Keefe M, McLoone S, Lanigan B. Effect of diode laser retinal ablative therapy for threshold retinopathy of prematurity on the visual field: Results of Goldmann perimetry at a mean age of 11 years. J Pediatric Ophthalmol Strabismus. 2007;44:170–3. doi: 10.3928/0191-3913-20070301-10. [DOI] [PubMed] [Google Scholar]
- 29.Trigler L, Weaver RG, Jr, O’Neil JW, Barondes MJ, Freedman SF. Case series of angle-closure glaucoma after laser treatment for retinopathy of prematurity. JAAPOS. 2005;9:17–21. doi: 10.1016/j.jaapos.2004.10.007. [DOI] [PubMed] [Google Scholar]


