Abstract
Carotid sinus syndrome (CSS) is a disease of the autonomic nervous system presenting with syncope, especially in older males who often have cardiovascular disease. The aetiology is unknown and epidemiological data is limited. Forty new patients/million population have been estimated to require pacing for CSS and these patients represent ∼9% of those presenting syncope to a specialist facility. CSS is defined as a response to carotid sinus massage (CSM) that includes reproduction of spontaneous symptoms. Cardioinhibitory CSS shows 3s asystole on CSM and vasodepressor CSS shows >50 mmHg fall in blood pressure (BP), there are mixed forms. The methodology of CSM requires correct massage in the supine and upright with continuous ECG and BP. Assessment of the vasodepressor component implies the ‘method of symptoms’ using atropine to prevent asystole. Carotid sinus hypersensitivity (CSH) is a related condition where CSM is positive in an asymptomatic patient. CSH cannot be assumed to respond to pacing. CSS patients present syncope with little or no warning. If no cause is revealed by the initial evaluation, CSM should be considered in all patients >40 years. CSM carries a small risk of thromboembolism. Therapy for cardioinhibitory CSS is dual chamber pacing, which is most effective in patients with a negative tilt test. Syncope recurrence is ∼20% in 5 years in paced patients. Therapy for the vasodepressor component of CSS, as pure vasodepression or mixed, where tilt testing will likely be positive, is often unrewarding: alternative therapeutic measures may be needed including discontinuation/reduction of hypotensive drugs.
Keywords: carotid sinus syndrome, carotid sinus hypersensitivity, carotid sinus massage, syncope, falls, pacemaker, vasodepression, cardioinhibition
Definition
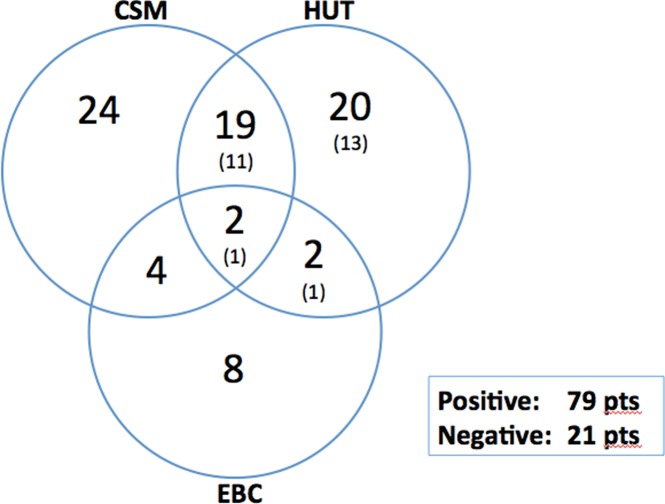
Carotid sinus syndrome is defined, by the new Guidelines of the European Society of Cardiology (ESC) 1 as syncope with reproduction of symptoms during carotid sinus massage (CSM) of 10s duration. It is cardioinhibitory (CI) when CSM generates >3s asystole (Figure 1). It is always vasodepressor but the degree of vasodepression varies and when it exists alone, the vasodepressor (VD) form, the systolic blood pressure falls >50 mmHg. 1 Intermediate or Mixed forms show both features.
Figure 1.
Case of CSS showing result of CSM. Courtesy of Dr. Michele Brignole.
For purposes of clarity, carotid sinus hypersensitivity (CSH) is not carotid sinus syndrome (CSS). CSH is present when a patient has cardioinhibitory, mixed or vasodepressor findings on CSM, with or without symptoms but is asymptomatic otherwise.
The most recent European Society of Cardiology Guidelines on Pacing 1 considered altering the previously used 3s duration of asystole to 6s (a new cut-off) for decisions concerning selection of pacing therapy as 3s is too short. The duration of asystole, which causes symptoms in CI and Mixed forms is generally much longer than the historical 3 s cut-off value. On average the duration of asystole to cause symptoms is 7.6 ± 2.2 s and the fall in blood pressure is 63 ± 24 mmHg. 2 CSS is a provocative test and like tilt testing it is difficult to be sure that the provocation reproduces what happens spontaneously. 3
Aetiology
The aetiology of CSS is unknown. It presents in older persons, with a mean age ∼75 years, and has a strong male dominance >2:1. CSS is an autonomic nervous system disease involving a pathological reflex, the pathophysiology of which has features similar to vasovagal syncope (VVS) with two main elements of its reflex involving cardioinhibition via the vagus nerve and vasodepression, which is thought to be due to sympathetic withdrawal. The abnormal reflex has been attributed to disturbance of baroreceptor function 4 and also to degeneration of the medulla. 5 CSS has overlap with VVS (Figure 2). Both may exist in the same patient, but they appear to be independent of each other. 7 Carotid sinus syndrome has its name because its initial discovery was by mechanical stimulation of the Carotid sinus as described by Roskam 8 and Weiss and Baker. 9 Their patients had the so-called spontaneous form of the disease. Tight collars and neck movements 8,9 have a particular tendency to trigger the reflex and occasionally neck tumours, neck surgery or irradiation may also act as triggers. 10 Most patients present syncope without any local trigger but the diagnosis is nevertheless made by addressing the carotid sinus by massage, CSM, as described above.
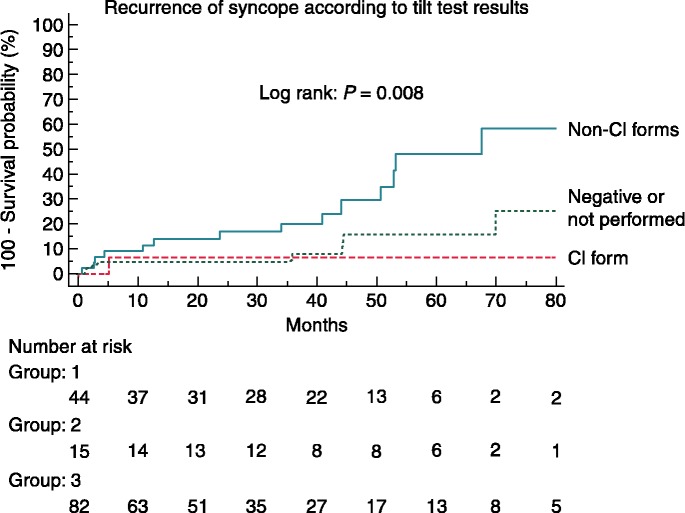
Figure 2.
Overlap of results of provocative testing in patients with unexplained syncope. The Venn diagram shows the distribution of positive responses to CSM, Eyeball compression and head-up tilt test in 100 patients with unexplained syncope with 79 having at least one positive test and 21 were negative to all provocations. The numbers in the HUT circle represent the total of positive responses with the numbers in brackets representing those positive tests without isoproterenol challenge (after Brignole and Menozzi 6 ). CSM = Carotid sinus massage, EBC = Eyeball compression, HUT = head-up tilt test.
Epidemiology
Comprehension of the epidemiology of carotid sinus syndrome is adversely affected by confusion over its definition. The only fairly precise estimates of incidence of CSS were made in the 1980s from Lavagna in Italy 11 and from Worthing, Sussex in the United Kingdom 12 which gave that of cardioinhibitory CSS as 35–40 new patients per million population per year. The reason for the restriction to cardioinhibition reflects selection of patients for treatment by pacing. To my knowledge there have been no good estimates of population incidence that include the vasodepressor form of CSS. The prevalence of CSS has been estimated to be < 4% in patients < 40 years and 41% in those >80 years attending a specialized syncope facility. 13,14 Estimates of the incidence amongst patients presenting with syncope are better than population data with the latest figures from Lavagna, Italy being 8.8% having CSS in a population of 1855 patients with unexplained syncope by initial evaluation. 2 Of these 164 patients 81% had asystole with CSM and 19% had vasodepression. CSS is more common at 8.8% of presenting patients than cardiac syncope of all types, as this represents 10% of patients unexplained by the initial evaluation but only 5% of those after the final diagnosis. 2
Clinical features
Patients present with syncope that has little or no prodrome. They are mostly males and often have evidence of cardiovascular disease. With respect to rhythm disturbances there is an association with sinus node disease ranging from 21–56% and with atrioventricular block (21–37%). Syncope recurrence is common and is reported to be 50% in 2 years. 15,16 There is also a high mortality, which is considered to be related to co-morbidities and age rather than CSS itself. 17 When monitored by a special delayed hysteresis pacemaker or by an implantable loop recorder 15,16 in cardioinhibitory patients the detected arrhythmia is sinus arrest without escape rhythm in 72%. The overlap between CSS and VVS raises difficulties in determination of which is the attributable cause of syncope. 6,17
Methodology of CSM
Carotid sinus massage should be considered in all patients with syncope over the age of 40 years when the cause of syncope is not detected by the initial evaluation of the patient using clinical history from patient and witness, physical examination, 12-lead ECG and estimation of blood pressure on standing for 3 minutes. 18 Below the age of 40, CSS is sufficiently rare to allow omission of CSM.
Carotid sinus massage is conducted in a hospital facility. When the patient undergoes the test, the possible outcome should be explained beforehand. In some countries written consent may be required. It must be regarded as a provocative test that carries a small risk of cerebral embolism almost always associated with complete recovery. 19 Nowadays, the test is often performed in a tilt test laboratory as there, supine and erect massage of the two carotids sequentially can be undertaken in a controlled and safe manner. The added diagnostic value of repeating CSM in the upright position has been well documented by Kenny's group. 20 During the test, the ECG, together with beat-to-beat blood pressure, usually non-invasively, is continuously recorded (Figure 1).
The carotid artery sinus lies at the anterior margin of the sternocleidomastoid muscle at the level of the cricoid cartilage. Usually the right artery is massaged first for no reason more than right structures are examined first with the physician approaching from the patient's right. Massage of the artery can be performed by the thumb or by the index, middle and ring fingers according to personal preference. The essence of massage is that it is massage and not extreme pressure, and certainly not occlusive pressure. If necessary, this can be monitored by a finger of the other hand on the ipsilateral temporal artery. There is some lateralisation of positive responses, with sinus arrest being the more common response to right artery massage, and atrioventricular block being seen occasionally on left massage. 12 Massage is conducted for 10s. After the right artery, the left is massaged. The tilt table is then raised to 60–80 degrees and the right and left massages are repeated. The question of whether this test should be performed before or after a formal tilt test is not, at present, answered. Our own practice is to perform it after the tilt test; Brignole prefers to perform it before tilt, as the effect of tilt on CSM findings is unknown (personal communication). The above given definitions of CSS and CSH are what constitute positive results. The results of CSM are repeatable phenomena but there is potential for fatigue. It is, therefore, recommended that only the minimum number of massages be performed (4 or 6 if the method of symptoms is employed).
Method of symptoms
The ‘Method of symptoms’ was first proposed by Thomas in 1969, 14 but clinically applied by Brignole. 21 It is clear that an asystolic response will have a major effect on blood pressure. So, in order to assess the possible contribution of vasodepression in an asystolic patient atropine can be given intravenously (1 mg or 0.02 mg/kg body weight) and the massage repeated. Asystole is then prevented by the drug and the fall in blood pressure can be measured. Atropine has side-effects and these need to be discussed with the patient at the outset of the test and included in the formal consent, if one is used. Further to the above given definitions, a mixed response to CSM is one where there is an asystolic period of >3s and a fall in blood pressure of >50 mmHg. This can only be assessed using active prevention of the asystole by atropine or possibly by temporary pacing, which is considered too invasive, except in very unusual cases. This describes the ‘Method of symptoms’ where if there is asystole in the first massage with reproduction of symptoms and symptoms are abolished by atropine in the second massage of the same artery it is revealed that the period of asystole was responsible for the symptoms, see Table 1 ‘Classification of CSS’.
Table 1.
Classification of CSS (after Brignole and Menozzi 6 ).
| Dominant Cardioinhibitory CSS |
| Initial CSM: Ventricular asystole >3s+ reproduction of spontaneous symptoms. CSM + Atropine: Absence of ventricular asystole and symptoms (Vasodepressor component either insufficient to cause symptoms or absent). |
| Mixed CSS |
| Initial CSM: Ventricular asystole >3s+ reproduction of spontaneous symptoms. CSM + Atropine: BP fall >50mmHg with reproduction of spontaneous symptoms. |
| Dominant Vasodepressor CSS |
| Initial CSM: Ventricular asystole absent or < 3s+ BP fall >50mmHg with reproduction of spontaneous symptoms. CSM + Atropine: Ventricular asystole absent, BP fall as with Initial CSM + reproduction of spontaneous symptoms. |
CSS = Carotid sinus syndrome, CSM = Carotid sinus massage, BP = Blood pressure. Atropine administered IV 0.02 mg/kg body weight.
Contraindications to CSM
Currently, it is accepted that a carotid bruit is a contraindication to CSM but it is known that carotid bruits do not correlate well with degrees of carotid stenosis. A Carotid bruit's elevation of the risk of massage has never been put to the test. However, in small series, patients with quite severe carotid stenoses have safely undergone CSM. 22 There is less controversy about recent (within 3 months) transient ischaemic attacks, strokes and myocardial infarctions providing contraindications to CSM, but the nature of the contraindication should be more considered to the autonomic changes wrought by these conditions altering the results, than the dangers of the CSM at this time. 19 CSM occasionally precipitates atrial fibrillation, which quickly reverts to sinus rhythm.
Carotid sinus hypersensitivity
As has been stated, carotid sinus hypersensitivity is a positive response to carotid sinus massage in an asymptomatic patient. It could, therefore, be construed that CSH is a precursor of CSS. While this may be true, no data exist to confirm this possibility. However, CSH has been taken to indicate the existence of an abnormal reflex, which may have importance in unexplained falls, where it is necessary to take into account that there may have been syncope but the history of syncope is unavailable due to the relatively common amnesia for the event. 23 Several studies have been performed to investigate the role of the abnormal reflex in unexplained falls and its possible treatment by pacing to prevent the expected bradycardia and thereby prevent at least some falls. 24–27 The first trial, SAFE PACE, 24 showed promise that there may be a favourable influence of pacing but this has not been substantiated in the subsequent studies. 25–27 One of the reasons for these disappointing results may be the lack of equivalence of CSH to CSS in fallers.
Treatment of cardioinhibitory CSS
Pacing was introduced for this indication in the 1970s 28 and was developed in the early 1980s when dual chamber pacing became widely available. 29,30 The results were encouraging to enthusiasts, but neither the diagnosis nor the therapy became accepted practice for an extended period. CSM was not performed in many centres and was considered dangerous until the relatively benign complications incidence was reported. 19 Syncope recurrence was also considered to be a problem. That it was higher than in atrioventricular block should have been anticipated, as CSS is a form of reflex syncope involving – in every case – some degree of vasodepression. Results in the late 1980s, showing a 9% recurrence with dual chamber pacing and 18% with ventricular pacing in 5 years gave a realistic picture at the time. 31 This was corroborated by Lopes et al in 2011, 32 using dominantly dual chamber pacing with 10.9% recurrence also in 5 years, but Brignole and Menozzi found 20% in their series over 5 years of follow-up. 33 Furthermore, in relation to current data, these figures are relatively acceptable with ∼20% in sinus node disease in 5.5 years 34 and 25% in 2 years in older vasovagal patients. 35 One randomized trial (RCT) was performed on 60 patients in 1992, with a highly significant benefit of pacing being shown (p < 0.002), 36 with a second RCT by another group in 2007 serving to confirm the earlier results. 37
CSS became fully accepted as having a strong indication for pacing and is classified as a Class 1 indication, level of evidence B in the current ESC Guidelines for Pacing. 1 The mode of pacing is advised to be dual chamber for all those in sinus rhythm, reserving VVI pacing for those in permanent atrial fibrillation. 1
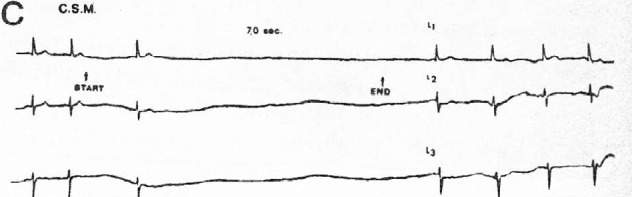
Recent earlier evidence suggests that, in both CSS and VVS, a positive tilt test implies a less positive outcome, in terms of recurrent syncope (Figure 3), from pacing, 2,38,39 which may be explained by the presence of a more potent vasodepressor component of the reflex. 40 It is in this regard that consideration of overlap between CSS and VVS is most important.
Figure 3.
Recurrence of syncope according to tilt-test results Figure reproduced with permission of Oxford University Press. From Solari et al. 2 CI = Cardioinhibitory.
There is a case to be made for use of tilt-testing in CSS to risk stratify cardioinhibitory or mixed patients in order to anticipate the likely recurrence of syncope and, perhaps, to go a step further and attempt prophylactic treatment of the vasodepressor component. However, since this treatment is less than satisfactory it may be prudent to await a first recurrence before embarking on therapy.
Therapy of vasodepressor CSS
Management of vasodepressor CSS has received relatively little attention. 41 Patients are advised to take increased volumes of fluid (2+litres/day) and, if safe, to increase salt consumption toward 6g/day. The principle difficulty in management is the frequent coincidence of hypertension. This coincidence becomes even more important when drug therapy of recurrent syncope has to be considered because those drugs, which may offer benefit in supporting low blood pressure during symptoms are likely to raise blood pressure to unacceptable levels at all other times. The first step should be to attempt reduction or cessation of hypotensive medication. 2 Following this, if unsatisfactory, fludrocortisone and midodrine are the drugs typically considered, but both are contraindicated in hypertensive patients. Little trial evidence is available to guide the physician. One trial, a RCT, included some vasodepressor CSS patients with a measure of success, but the trial was very small in size and without prolonged follow-up. 42 Recent discussions of the aggressiveness of blood pressure control are relevant to these patients 43 and it is reasonable to allow higher than recommended levels of blood pressure to gain benefit at times of hypotension. A newly-available drug, droxidopa, may have some value in these patients but no evidence is yet available in CSS management. The most frequently considered drug is midodrine but one of its common side effects in males is urinary retention, making it untenable in many who might benefit.
Conclusions
Carotid sinus syndrome is a relatively common cause of syncope in patients >40 years old but it is, even today, too infrequently sought as a possible cause. It occurs dominantly in males of advanced age and is diagnosed by CSM with reproduction of spontaneous symptoms.
Carotid sinus hypersensitivity is a positive result of massage in the absence of clinical symptoms. Thus, these two conditions must be held as distinct entities. CSS is present in 8.8% of patients with syncope unexplained after initial evaluation, cardiac syncope is present in 10% of all patients presenting syncope and in 5% of those unexplained after initial evaluation, thus CSS is more frequent than all types of cardiac syncope combined.
Cardioinhibitory CSS is treated with acceptable success by pacing dual chamber in all those showing sinus rhythm. Greatest success may be expected in those patients who are tilt-test negative. Treatment of vasodepressor CSS is difficult and often unsatisfactory. Reduction of hypotensive medication and fluid intake increase should be the first step in management if the patient has been taking anti-hypertensive therapy. If recurrent syncope cannot be controlled, careful use of midodrine together with acceptance of higher than usually accepted blood pressure levels is recommended. Tilt-test positive patients may have recurrence of syncope despite adequate pacing. They may benefit from measures to control the vasodepressor component of the reflex.
References
- 1.Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt O-A, Cleland J, Deharo J-C, Delgado V, Elliott PM, Gorenek B, Israel CW, Leclercq C, Linde C, Mont L, Padeletti L, Sutton R, Vardas PE, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Kirchhof P, Blomstrom-Lundqvist C, Badano LP, Aliyev F, Bänsch D, Baumgartner H, Bsata W, Buser P, Charron P, Daubert J-C, Dobreanu D, Faerestrand S, Hasdai D, Hoes AW, Heuzey J-YL, Mavrakis H, McDonagh T, Merino JL, Nawar MM, Nielsen JC, Pieske B, Poposka L, Ruschitzka F, Tendera M, Gelder ICV, Wilson CM. ESC Guidelines on cardiac pacing and cardiac resynchronization therapy The Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA) Europace. 2013;15(8):1070–1118. doi: 10.1093/europace/eut206. http://dx.doi.org/10.1093/europace/eut206. [DOI] [PubMed] [Google Scholar]
- 2.Solari D, Maggi R, Oddone D, Solano A, Croci F, Donateo P, Brignole M. Clinical context and outcome of carotid sinus syndrome diagnosed by means of the “method of symptoms.”. Europace. 2014;16(6):928–934. doi: 10.1093/europace/eut283. http://dx.doi.org/10.1093/europace/eut283. [DOI] [PubMed] [Google Scholar]
- 3.Moya A, Brignole M, Menozzi C, Garcia-Civera R, Tognarini S, Mont L, Botto G, Giada F, Cornacchia D. Mechanism of syncope in patients with isolated syncope and in patients with tilt-positive syncope. Circulation. 2001;104(11):1261–1267. doi: 10.1161/hc3601.095708. http://dx.doi.org/10.1161/hc3601.095708. [DOI] [PubMed] [Google Scholar]
- 4.Healey J, Connolly SJ, Morillo CA. The management of patients with carotid sinus syndrome: is pacing the answer? Clin Auton Res. 2004;14(1):i80–i86. doi: 10.1007/s10286-004-1012-2. http://dx.doi.org/10.1007/s10286-004-1012-2. [DOI] [PubMed] [Google Scholar]
- 5.Miller VM, Kenny RA, Slade JY, Oakley AE, Kalaria RN. Medullary autonomic pathology in carotid sinus hypersensitivity. Neuropathol Appl Neurobiol. 2008;34(4):403–411. doi: 10.1111/j.1365-2990.2007.00903.x. http://dx.doi.org/10.1111/j.1365-2990.2007.00903.x. [DOI] [PubMed] [Google Scholar]
- 6.Brignole M, Menozzi C. Carotid sinus syndrome: diagnosis, natural history and treatment. Eur J Card Pacing Electrophysiol. 1992;2:247–254. [Google Scholar]
- 7.Tan MP, Newton JL, Chadwick TJ, Parry SW. The relationship between carotid sinus hypersensitivity, orthostatic hypotension, and vasovagal syncope: a case–control study. Europace. 2008;10(12):1400–1405. doi: 10.1093/europace/eun278. http://dx.doi.org/10.1093/europace/eun278. [DOI] [PubMed] [Google Scholar]
- 8.Roskam J. Un syndrome nouveau: syncopes cardiaques graves et syncopes répétées par hypereflexivité sinocarotidienne. Presse Med. 1930;38:590–591. [Google Scholar]
- 9.Weiss S, Baker J. The carotid sinus reflex in health and disease: its role in the causation of fainting and convulsions. Medicine. 1933;12:293–354. [Google Scholar]
- 10.Brignole M, Benditt DG. Syncope: An evidence-based approach. London: Springer; 2011. Reflex Syncope (Neurally Mediated Syncope) p. 164. Available at: http://link.springer.com/chapter/10.1007/978-0-85729-201-8_11 Accessed June 2, 2014. [Google Scholar]
- 11.Brignole M, Menozzi C, Lolli G, Oddone D, Gianfranchi L, Bertulla A. Pacing for carotid sinus syndrome and sick sinus syndrome. Pacing Clin Electrophysiol. 1990;13(12 Pt 2):2071–2075. doi: 10.1111/j.1540-8159.1990.tb06944.x. [DOI] [PubMed] [Google Scholar]
- 12.Morley CA, Sutton R. Carotid sinus syncope. Int J Cardiol. 1984;6(3):287–293. doi: 10.1016/0167-5273(84)90188-8. http://dx.doi.org/10.1016/0167-5273(84)90188-8. [DOI] [PubMed] [Google Scholar]
- 13.Brignole M, Oddone D, Cogorno S, Menozzi C, Gianfranchi L, Bertulla A. Long-term outcome in symptomatic carotid sinus hypersensitivity. Am Heart J. 1992;123(3):687–692. doi: 10.1016/0002-8703(92)90507-r. http://dx.doi.org/10.1016/0002-8703(92)90507-R. [DOI] [PubMed] [Google Scholar]
- 14.Thomas JE. Hyperactive carotid sinus reflex and carotid sinus syncope. Mayo Clin Proc. 1969;44(2):127–139. [PubMed] [Google Scholar]
- 15.Menozzi C, Brignole M, Lolli G, Bottoni N, Oddone D, Gianfranchi L, Gaggioli G. Follow-up of asystolic episodes in patients with cardioinhibitory, neurally mediated syncope and VVI pacemaker. Am J Cardiol. 1993;72(15):1152–1155. doi: 10.1016/0002-9149(93)90985-l. http://dx.doi.org/10.1016/0002-9149(93)90985-L. [DOI] [PubMed] [Google Scholar]
- 16.Maggi R, Menozzi C, Brignole M, Podoleanu C, Iori M, Sutton R, Moya A, Giada F, Orazi S, Grovale N. Cardioinhibitory carotid sinus hypersensitivity predicts an asystolic mechanism of spontaneous neurally mediated syncope. Europace. 2007;9(8):563–567. doi: 10.1093/europace/eum092. http://dx.doi.org/10.1093/europace/eum092. [DOI] [PubMed] [Google Scholar]
- 17.Brignole M, Menozzi C, Gianfranchi L, Oddone D, Lolli G, Bertulla A. Carotid sinus massage, eyeball compression, and head-up tilt test in patients with syncope of uncertain origin and in healthy control subjects. Am Heart J. 1991;122(6):1644–1651. doi: 10.1016/0002-8703(91)90282-m. [DOI] [PubMed] [Google Scholar]
- 18.Moya A, Sutton R, Ammirati F, Blanc J-J, Brignole M, Dahm JB, Deharo J-C, Gajek J, Gjesdal K, Krahn A, Massin M, Pepi M, Pezawas T, Granell RR, Sarasin F, Ungar A, Dijk JG, van, Walma EP, Wieling W, Abe H, Benditt DG, Decker WW, Grubb BP, Kaufmann H, Morillo C, Olshansky B, Parry SW, Sheldon R, Shen WK, Vahanian A, Auricchio A, Bax J, Ceconi C, Dean V, Filippatos G, Funck-Brentano C, Hobbs R, Kearney P, McDonagh T, McGregor K, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Vardas P, Widimsky P, Auricchio A, Acarturk E, Andreotti F, Asteggiano R, Bauersfeld U, Bellou A, Benetos A, Brandt J, Chung MK, Cortelli P, Costa AD, Extramiana F, Ferro J, Gorenek B, Hedman A, Hirsch R, Kaliska G, Kenny RA, Kjeldsen KP, Lampert R, Mølgard H, Paju R, Puodziukynas A, Raviele A, Roman P, Scherer M, Schondorf R, Sicari R, Vanbrabant P, Wolpert C, Zamorano JL. Guidelines for the diagnosis and management of syncope (version) The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC) Eur Heart J. 2009;30(21):2631–2671. doi: 10.1093/eurheartj/ehp298. http://dx.doi.org/10.1093/eurheartj/ehp298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Munro NC, McIntosh S, Lawson J, Morley CA, Sutton R, Kenny RA. Incidence of complications after carotid sinus massage in older patients with syncope. J Am Geriatr Soc. 1994;42(12):1248–1251. doi: 10.1111/j.1532-5415.1994.tb06505.x. [DOI] [PubMed] [Google Scholar]
- 20.Parry SW, Richardson DA, O'Shea D, Sen B, Kenny RA. Diagnosis of carotid sinus hypersensitivity in older adults: carotid sinus massage in the upright position is essential. Heart. 2000;83(1):22–23. doi: 10.1136/heart.83.1.22. http://dx.doi.org/10.1136/heart.83.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brignole M, Sartore B, Barra M, Menozzi C, Lolli G. Ventricular and dual chamber pacing for treatment of carotid sinus syndrome. Pacing Clin Electrophysiol. 1989;12(4):582–590. doi: 10.1111/j.1540-8159.1989.tb02704.x. http://dx.doi.org/10.1111/j.1540-8159.1989.tb02704.x. [DOI] [PubMed] [Google Scholar]
- 22.Dehn TCB, Morley CA, Sutton R. A scientific evaluation of the carotid sinus syndrome. Cardiovasc Res. 1984;18(12):746–751. doi: 10.1093/cvr/18.12.746. http://dx.doi.org/10.1093/cvr/18.12.746. [DOI] [PubMed] [Google Scholar]
- 23.O'Dwyer C, Bennett K, Langan Y, Fan CW, Kenny RA. Amnesia for loss of consciousness is common in vasovagal syncope. Europace. 2011;13(7):1040–1045. doi: 10.1093/europace/eur069. http://dx.doi.org/10.1093/europace/eur069. [DOI] [PubMed] [Google Scholar]
- 24.Kenny RA, Richardson DA, Steen N, Bexton RS, Shaw FE, Bond J. Carotid sinus syndrome: a modifiable risk factor for nonaccidental falls in older adults (SAFE PACE) J Am Coll Cardiol. 2001;38(5):1491–1496. doi: 10.1016/s0735-1097(01)01537-6. http://dx.doi.org/10.1016/S0735-1097(01)01537-6. [DOI] [PubMed] [Google Scholar]
- 25.Ryan DJ, Nick S, Colette SM, Kenny RA. Carotid sinus syndrome, should we pace? A multicentre, randomised control trial (Safepace 2) Heart. 2010;96(5):347–351. doi: 10.1136/hrt.2009.176206. http://dx.doi.org/10.1136/hrt.2009.176206. [DOI] [PubMed] [Google Scholar]
- 26.Crilley JG, Herd B, Khurana CS, Appleby CA, Belder MA, de, Davies A, Hall JA. Permanent cardiac pacing in elderly patients with recurrent falls, dizziness and syncope, and a hypersensitive cardioinhibitory reflex. Postgrad Med J. 1997;73(861):415–418. doi: 10.1136/pgmj.73.861.415. http://dx.doi.org/10.1136/pgmj.73.861.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parry SW, Steen N, Bexton RS, Tynan M, Kenny RA. Pacing in elderly recurrent fallers with carotid sinus hypersensitivity: a randomised, double-blind, placebo controlled crossover trial. Heart. 2009;95(5):405–409. doi: 10.1136/hrt.2008.153189. http://dx.doi.org/10.1136/hrt.2008.153189. [DOI] [PubMed] [Google Scholar]
- 28.Voss DM, Magnin GE. Demand pacing and carotid sinus syncope. Am Heart J. 1970;79(4):544–547. doi: 10.1016/0002-8703(70)90261-9. http://dx.doi.org/10.1016/0002-8703(70)90261-9. [DOI] [PubMed] [Google Scholar]
- 29.Morley CA, Perrins EJ, Grant P, Chan SL, McBrien DJ, Sutton R. Carotid sinus syncope treated by pacing. Analysis of persistent symptoms and role of atrioventricular sequential pacing. Br Heart J. 1982;47(5):411–418. doi: 10.1136/hrt.47.5.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Madigan NP, Flaker GC, Curtis JJ, Reid J, Mueller KJ, Murphy TJ. Carotid sinus hypersensitivity: beneficial effects of dual-chamber pacing. Am J Cardiol. 1984;53(8):1034–1040. doi: 10.1016/0002-9149(84)90632-5. http://dx.doi.org/10.1016/0002-9149(84)90632-5. [DOI] [PubMed] [Google Scholar]
- 31.Sutton R. Pacing in patients with carotid sinus and vasovagal syndromes. Pacing Clin Electrophysiol. 1989;12(7):1260–1263. http://dx.doi.org/10.1111/j.1540-8159.1989.tb01982.x. [Google Scholar]
- 32.Lopes R, Gonçalves A, Campos J, Frutuoso C, Silva A, Touguinha C, Freitas J, Maciel MJ. The role of pacemaker in hypersensitive carotid sinus syndrome. Europace. 2011;13(4):572–575. doi: 10.1093/europace/euq455. http://dx.doi.org/10.1093/europace/euq455. [DOI] [PubMed] [Google Scholar]
- 33.Brignole M, Menozzi C. The natural history of carotid sinus syncope and the effect of cardiac pacing. Europace. 2011;13(4):462–464. doi: 10.1093/europace/euq516. http://dx.doi.org/10.1093/europace/euq516. [DOI] [PubMed] [Google Scholar]
- 34.Chuen MJNK, Kirkfeldt RE, Andersen HR, Nielsen JC. Syncope in paced patients with sick sinus syndrome from the DANPACE trial: incidence, predictors and prognostic implication. Heart. 2014;100(11):842–847. doi: 10.1136/heartjnl-2013-304976. http://dx.doi.org/10.1136/heartjnl-2013-304976. [DOI] [PubMed] [Google Scholar]
- 35.Brignole M, Menozzi C, Moya A, Andresen D, Blanc JJ, Krahn AD, Wieling W, Beiras X, Deharo JC, Russo V, Tomaino M, Sutton R. Pacemaker therapy in patients with neurally mediated syncope and documented asystole: Third International Study on Syncope of Uncertain Etiology (ISSUE-3): a randomized trial. Circulation. 2012;125(21):2566–2571. doi: 10.1161/CIRCULATIONAHA.111.082313. http://dx.doi.org/10.1161/CIRCULATIONAHA.111.082313. [DOI] [PubMed] [Google Scholar]
- 36.Brignole M, Menozzi C, Lolli G, Bottoni N, Gaggioli G. Long-term outcome of paced and nonpaced patients with severe carotid sinus syndrome. Am J Cardiol. 1992;69(12):1039–1043. doi: 10.1016/0002-9149(92)90860-2. http://dx.doi.org/10.1016/0002-9149(92)90860-2. [DOI] [PubMed] [Google Scholar]
- 37.Claesson J-E, Kristensson B-E, Edvardsson N, Währborg P. Less syncope and milder symptoms in patients treated with pacing for induced cardioinhibitory carotid sinus syndrome: a randomized study. Europace. 2007;9(10):932–936. doi: 10.1093/europace/eum180. http://dx.doi.org/10.1093/europace/eum180. [DOI] [PubMed] [Google Scholar]
- 38.Gaggioli G, Brignole M, Menozzi C, Devoto G, Oddone D, Gianfranchi L, Gostoli E, Bottoni N, Lolli G. A positive response to head-up tilt testing predicts syncopal recurrence in carotid sinus syndrome patients with permanent pacemakers. Am J Cardiol. 1995;76(10):720–722. doi: 10.1016/s0002-9149(99)80207-0. http://dx.doi.org/10.1016/S0002-9149(99)80207-0. [DOI] [PubMed] [Google Scholar]
- 39.Brignole M, Donateo P, Tomaino M, Massa R, Iori M, Beiras X, Moya A, Kus T, Deharo JC, Giuli S, Gentili A, Sutton R, International Study on Syncope of Uncertain Etiology 3 (ISSUE-3) Investigators Benefit of pacemaker therapy in patients with presumed neurally mediated syncope and documented asystole is greater when tilt test is negative: an analysis from the third International Study on Syncope of Uncertain Etiology (ISSUE-3) Circ Arrhythm Electrophysiol. 2014;7(1):10–16. doi: 10.1161/CIRCEP.113.001103. http://dx.doi.org/10.1161/CIRCEP.113.001103. [DOI] [PubMed] [Google Scholar]
- 40.Sutton R, Brignole M. Twenty-eight years of research permit reinterpretation of tilt-testing – hypotensive susceptibility rather than diagnosis. Eur Heart J. 2014 doi: 10.1093/eurheartj/ehu255. doi:10.1093/eurheartj/ehu255. First published online: June 30. [DOI] [PubMed] [Google Scholar]
- 41.Romme JJ, Reitsma JB, Black CN, Colman N, Scholten RJ, Wieling W, Van Dijk N. Cochrane Database of Systematic Reviews. John Wiley & Sons; 1996. Drugs and pacemakers for vasovagal, carotid sinus and situational syncope. Available at: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004194.pub3/abstract Accessed June 2, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ward CR, Gray JC, Gilroy JJ, Kenny RA. Midodrine: a role in the management of neurocardiogenic syncope. Heart. 1998;79(1):45–49. doi: 10.1136/hrt.79.1.45. http://dx.doi.org/10.1136/hrt.79.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. American Society of Hypertension: Hypertension Guidelines. Available at: http://www.ash-us.org/About-Hypertension/Hypertension-Guidelines.aspx.