Abstract
Background:
To report the diagnostic and therapeutic options of missile head and neck injuries.
Aim and Objectives:
To present our experience in the management of head and neck missile injuries as seen in our centre.
Methodology:
All the patients with head and neck missile injuries who were managed in the ENT and Dental services of Yalgado University Teaching Hospital, in Ouagadougou, the capital of Burkina Faso between January 2003 and December 2012 were reviewed. The data obtained from medical records included demographic data, history, physical findings, and site of injury, diagnosis, type of treatment/surgery, complications and outcome.
Results:
Out of a total of 32 patients in this study, there were 26 males and 6 females with a sex ratio of 4.3:1. Their ages ranged from 18 to 63 years with a mean of 32 years ± 5.2. The age range of 20-40 accounted for 68.7% of the patients. The injury was accidental in 37.5%, assault in 56.3 and self inflicted/suicide in 6.3%. Most (59.4%) of the patients had multiple injuries while in 50 % of the cases, the injuries affected the face. Surgical intervention was done in 59.4% of the patients and conservative treatment in 40.6 % of the patients. Complications were noted in 52% of the patients. Seven patients died given a mortality rate of 21.9%.
Conclusion:
The head and neck missile injuries are not uncommon in our environment with a high mortality and morbidity rates.
Keywords: Head and Neck missile injuries, Young adults , Multifocal, High mortality and morbidity
Introduction
Head and neck missile injuries are relatively uncommon in hospital practice. The resultant injuries can be simple or complex and may be multiple. Prompt diagnosis and immediate effective management are essential in order to avoid the complications including disfigurement and even death1,2. Hospital mortality has improved with increasing used of established treatment protocols3, this is however not the case in our sub-region where the morbidity and mortality of such injuries remain high. We report our experience in management of missile head and neck injuries in our environment.
Reports
PATIENTS AND METHOD
This is a retrospective study of patients with head and neck missile injuries managed at the ENT and Dental services of Yalgado University Teaching Hospital at Ouagadougou, Burkina-Faso from January 2003 to December 2012. The data obtained from the medical records included the demographics, the clinical features, site of injury, diagnosis, relevant investigations, treatment offered and outcome. These were analyzed for mean and standard deviation.
RESULTS
EPIDEMIOLOGICAL DATA:
Thirty two cases were seen over 10 years with an average of 3.2 per year. There were 26 males and 6 females with a male:female ratio of 4.3:1. Their ages ranged from 18 to 63 years with a mean of 32 years ± 5.2. The modes of admission were 18 (56.3%) cases from referrals, 8 (25%) by direct admission and 12.5%) cases were transferred from other facilities. The age range of 20-40 years had the highest frequency, with 22(68.75%) cases. Civilians made up 28(87.5%) of the cases and the remaining 4(12.5%) cases were military and paramilitary personnel. The majority of patients were farmers as was the case in 13(40.62 %) patients while 11(34.4%) cases were from the informal sector of the economy. Twenty three (71.9%) patients were from the rural areas.
DIAGNOSTIC DATA:
The circumstances of injuries was assault in 18(56.3%), accidents in 12(37.5%) cases, and self inflicted/suicide in 2(6.3%). Majority of patients, 25(78.12%) cases had no pre-morbid medical condition. Alcohol use was noted in 3(9.4%) cases and occasional use of the drugs in 2(6.3%) cases were recorded as having influenced the injury. The cardio-respiratory conditions of the patients were unstable in 21(65.6%) cases and stable in the remaining 11(34.4%) cases. The main findings were painful swelling in all cases, bleeding in 13(40.6%) cases and a gaping wound in 6 (18.8 %) cases. Single lesions were found in 9(28.1%) cases, two injuries in 4(12.5%) cases and multiple in 19 (59.4 %) cases. Their location of the injuries were in the neck in 6(18.8 %), the face in 16 (50%) cases and in both head and neck in 8(25%) cases; in addition, it involved other regions of the body in 2(6.3%) cases. According to the International Committee of the Red Cross (ICRC) prognostic score, the injuries were classified as shown in the Table 1.
Table 1: Classification of the injuries according the ICRC prognostic scores
| Score | Number of patients | Percentage (%) |
| ST-Type (soft tissue ) | 7 | 21.9 |
| F-type (fracture) | 4 | 12.5 |
| V-type (vital) | 12 | 37.5 % |
| VF- type (vital -fracture) | 9 | 28.1% |
| Total | 32 | 100 |
Visceral injuries were pharyngeal in 9 (28.1 %) cases, the eyes in 6 (18.8 %) cases and ear injuries in 5 (15.6%) cases. At exploration, the lesions were classified as M0 (without foreign body included) in 5(15.6%) cases, M1 (with a foreign body) in 11(34.3 %) cases and M2 (with multiple foreign bodies) in 16(50 %) cases. The missiles were bullets in 27(84.4 %) cases, gas canister explosions in 3(9.4%) cases and fragments of burst tyres in 2(6.3%) cases. The entry wounds were anterior in 12(44.4%) cases, lateral in 16 (59.3%) cases and posterior in 4 (14.8 %) cases.
-TREATMENT DATA
The duration of hospital care was 2 to 96 hours with an average 18 hours. Conservative treatment only was instituted in 13(40.6%) cases, while19 (59.4%) patients had surgical interventions. Principal means of treatment are as shown in Figure 1.
Figure 1 .
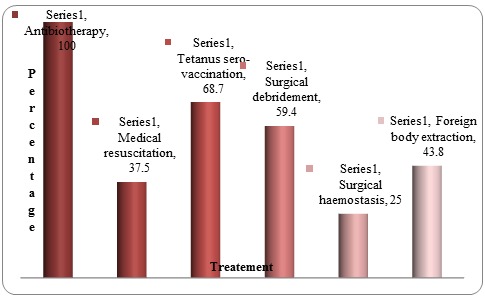
Thrapeutic options administered
Seven (21.9%) patients died from hemodynamic instability in 4(12.5%) cases and complications from infection in 3(9.4%) cases. Among those patients that survived, 13(52%) patients had residual complications: blindness in 5 cases, deafness in 3 cases, facial nerve palsy in 2 cases, keloid in 2 cases and residual dysosmia in one case.
Discussion
DISCUSSION
Missile injuries are relatively rare conditions in head and neck practice. It is highly fatal, only few patients arrive alive in a specialized centre for care because of the associated high pre-hospital deaths3. In this study, 32 cases of head and neck missile injuries were managed over a 10-year period giving an average of 3.2 cases per year in one of the main reference centres of Burkina Faso. These data are small compared to those of developed countries or in war situation where many more cases are managed annually3,4. But for us they remain quite high for a condition that is preventable especially when they occur at peace time. Unlike conventional war zones where military casualties are commonly encountered, in our context, the injured are predominantly civilians comprising of about 87.5% of the cases. They were mainly young adults in 68.75%, and commonly involves males. This could be explained by the proliferation of small arms, the development of organized crime and the growth of armed robbery commonly known as “highway robbers " in our region. These attacks occur in rural areas with relatively less security and limited health facilities. This explains in part the predominance of cases that are transferred (56.25%) to our centre mostly from rural areas (71.87 %).
Head and neck injuries from missiles have high morbidity and mortality. The severity is partly linked to the circumstances surrounding the injury which are quite variable depending on the series1,2,6. Suicide attempts and self inflicted injuries are more severe than attacks and accidental injuries1,4,7,8. In this study, suicidal/self inflicted injuries comprised 6.3% of cases compared accidents (37.5%) and assault (56.25%). The location of the injuries was mainly facial in 50% and head and neck in 25% of the cases. This could be explained by the anatomical position of the neck which is protected while the face is particularly exposed to ballistic injury is at the centre of the offending missile. Like other series from peaceful zones (civilian injuries), all the missiles were small and of about 20mm calibre or lower. This could be explained by the proliferation and availability as well as the ease of handling small and light weapons in the West African sub-region. Added to this is the trivialization of firearms with a considerable lax security measures and thus accident-prone behaviour that is increasingly becoming common. Missile injuries add an additional cost of radiological investigation and surgical explorations4,7,9,10. In this study, we observed at wound exploration that there were 5 cases without foreign body (M0), 11 cases with a single foreign body (M1) and 16 with several foreign bodies (M2); the entry wound was anterior in 59% cases and lateral in 44% of the cases.
-TREATMENT
Missile injuries of the head and neck are treated as emergency. A multidisciplinary approach is recommended for a better outcome and to prevent complications10,11,12,13. This was the approach we undertook in our series that involved intensive critical care in the ICU in 37.5% cases. In all cases, the preservation of life remained paramount and took precedence over function and aesthetics in the immediate management; function and aesthetics nevertheless remained major concerns even in the early management of any facial injury8,9,12,14,15. In all, 78% of our patients survived while the rest died. The deaths were due to hemodynamic instability and infections.
Conclusions
CONCLUSION: Head and neck missile injuries are relatively uncommon but with high morbidity and mortality in our sub-region. They primarily occur in young adults especially males and mainly from accidents or assault. The injuries are usually complex with retained foreign bodies.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Grant support: None
References
- 1.De Rotalier P, Bizeau A, Buffe P. Head and neck wounds by projectiles. EMC – Otorrhinolaringologia. 2001. pp. 1–8.
- 2.Seventh International Symposium of Weapons traumatology and Wound ballistics. J Trauma. 1996;40(suppl 3):s1–s227. [Google Scholar]
- 3.Quinot JF, Kaiser E. Before emergency cervical wound, EMC - Medicine. 2004;1:157–164. [Google Scholar]
- 4.Peleg K, Rivkind A, Aharonson-Daniel L, Israel Trauma Group; Does body armor protect from firearm injuries? J Am Coll Surg . 2006;202(4):643–648. doi: 10.1016/j.jamcollsurg.2005.12.019. [DOI] [PubMed] [Google Scholar]
- 5.Dahlberg LL, Ikeda RM, Kresnow MJ. Guns in the home and risk of a violent death in the home: findings from a national study. Am J Epidemiol. 2004;160(10):929–936. doi: 10.1093/aje/kwh309. [DOI] [PubMed] [Google Scholar]
- 6.Colombo F, Sansonna F, Baticci F, Boniardi M, Di Lernia S, Ferrari GC, Pugliese R. Penetrating injuries of the neck : review of 16 operated cases. Ann Ital Chir. 2003;74(2):141–148. [PubMed] [Google Scholar]
- 7.Tall A, Sy A, Diouf R, Ndiaye IC, Diallo BK, Loum B, Fall D, Diop EM. Notre expérience des traumatismes du cou en pratique civile: à propos de 45 cas. Medicine d’Afrique. 2004;52:1999–2002. [Google Scholar]
- 8.Verschueren DS, Bell RB, Bagheri SC, Dierks EJ, Potter BE. Management of laryngo- tracheal injuries Associated with crânio- maxillofacial trauma. J Oral Maxillofacial Surg . 2006;64(2):203–214. doi: 10.1016/j.joms.2005.10.034. [DOI] [PubMed] [Google Scholar]
- 9.Hussein Zaidi SM, Ahmad R. Penetrating neck trauma: a case for conservative approach . Am I Otolaryngol. 2011;32:591–596. doi: 10.1016/j.amjoto.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Van Waes OJ, Cheriex KC, Navsaria PH, Van Riet PA, Nicol AJ, Vermeulen J. Management of penetrating neck injuries, Br J Surg. 2012;99(Suppl 1):149–154. doi: 10.1002/bjs.7733. [DOI] [PubMed] [Google Scholar]
- 11.Duhamel P, Gauthier J, Teyssères N, Giraud O, Denhez F, Bey E. Examen d’un traumatisé facial EMC. Stomatology. 2008:1–25. [Google Scholar]
- 12.Stansfield T, Rushforth G. Uk Armed Forces unintentional fire arm injuries . J R Army Med Corps. 2009 Mar;155(1):20–23. doi: 10.1136/jramc-155-01-06. [DOI] [PubMed] [Google Scholar]
- 13.Ballistics reviews: Mechanisms of bullet wound trauma. Forensic Sci Med Pathol. 2009;5(3):204–209. doi: 10.1007/s12024-009-9096-6. [DOI] [PubMed] [Google Scholar]
- 14.Denton JS, Segovia A, Filkins JA. Practical pathology of gunshot wounds . Arch Pathol Lab Med . 2006;130(9):1283–1289. doi: 10.5858/2006-130-1283-PPOGW. [DOI] [PubMed] [Google Scholar]
- 15.Demetriades D, Hadjizacharia P, Constantinou C. Selective nonoperative management of penetrating abdominal solid organ injuries. Ann Surg. 2006;244(4):620–628. doi: 10.1097/01.sla.0000237743.22633.01. [DOI] [PMC free article] [PubMed] [Google Scholar]


