Abstract
BACKGROUND:
Hockey is played by youth across Canada, and its popularity has increased dramatically among females in the past decade. Despite this, there has been little epidemiological research comparing the injury patterns of young female and male hockey players.
OBJECTIVE:
To describe and compare injuries sustained by female and male youth hockey players using the Canadian Hospitals Injury Reporting and Prevention Program database.
METHODS:
In the present cross-sectional, retrospective comparison study, the Canadian Hospitals Injury Reporting and Prevention Program database was used to identify all hockey-related injuries sustained by children seven to 17.5 years of age over a 15-year period (January 1995 to December 2009). Exclusion criteria included paid professional players and children with injuries sustained while playing road hockey.
RESULTS:
Inclusion criteria were met by 33,233 children (2637 [7.9%] females and 30,596 [92.1%] males). Compared with males, females reported proportionately more soft tissue injuries (39.8% versus 32.6%; P<0.01) and sprains/strains (21.1% versus 17.6%; P<0.01). Males experienced more fractures (27.1% versus 18.2%; P<0.01) and were most often injured through body checking (42.8% versus 25.7%; P<0.01). Females showed a trend toward increased concussion with age, and were most often injured through collisions (28.6% versus 24.6%; P<0.01).
CONCLUSION:
Compared with males, female hockey players sustained proportionately more soft tissue injures and sprains/strains, and showed a trend toward concussions in late adolecence. Males experienced more fractures, shoulder injuries and injuries due to body checking. Further research is required to identify risk factors for injury in female youth hockey players and to target injury prevention.
Keywords: Epidemiology, Female, Hockey, Injury, Minor, Youth
Abstract
HISTORIQUE :
Des jeunes jouent au hockey partout au Canada. La popularité de ce sport a considérablement augmenté chez les filles depuis dix ans. Pourtant, peu de recherches épidémiologiques comparent les profils de blessures des jeunes joueuses de hockey à celui des jeunes joueurs.
OBJECTIF :
Décrire et comparer les blessures subies par les jeunes joueuses et joueurs de hockey à l’aide des bases de données du Système canadien hospitalier d’information et de recherche en prévention des traumatismes (SCHIRPT).
MÉTHODOLOGIE :
Dans la présente étude comparative transversale et rétrospective, la base de données du SCHIRPT a permis de dépister toutes les blessures liées au hockey dont ont été victimes des enfants de sept à 17,5 ans sur une période de 15 ans (janvier 1995 à décembre 2009). Étaient exclus les joueurs professionnels rémunérés et les enfants blessés en jouant au hockey de rue.
RÉSULTATS :
Les critères d’inclusion étaient respectés par 33 233 enfants (2 637 filles [7,9 %] et 30 596 garçons [92,1 %]). Par rapport aux garçons, les filles déclaraient proportionnellement plus de blessures des tissus mous (39,8 % au lieu de 32,6 %; P<0,01) et de foulures ou d’entorses (21,1 % au lieu de 17,6 %; P<0,01). Les garçons subissaient plus de fractures (27,1 % au lieu de 18,2 %; P<0,01), souvent lors de mises en échec (42,8 % au lieu de 25,7 %; P<0,01). Les filles présentaient une tendance à l’augmentation des commotions avec l’âge, et se blessaient davantage lors de collisions (28,6 % au lieu de 24,6 %; P<0,01).
CONCLUSION :
Par rapport aux joueurs, les joueuses de hockey étaient proportionnellement victimes de plus de blessures des tissus mous et de foulures ou d’entorses, et présentaient une tendance aux commotions à la fin de l’adolescence. Les joueurs subissaient plus de fractures, de blessures à l’épaule et de blessures causées par les mises en échec. D’autres recherches s’imposent pour déterminer les facteurs de risque de blessures chez les jeunes joueuses de hockey et pour cibler les mesures de prévention.
Ice hockey has witnessed impressive increases in female enrollment over the 14 years since the International Ice Hockey Federations’ first Women’s World Hockey Championship in 1990 (1). In 2012–2013, there were >86,000 female hockey players registered with Hockey Canada, representing 14% of registrants (2). Although there is a growing body of literature describing the injury profiles of female hockey players (3–8), there are few studies that specifically focus on the injury profiles of female youth hockey players (3,4). Published studies detailing the injuries of older hockey players have suggested that the injury profiles of male and female players are different (7–9); however, no large youth-specific studies investigating this issue have been published.
In 2013, Hockey Canada banned body checking for boys playing hockey at the PeeWee level (11 to 12 years of age) and below in all Canadian provinces (10). In the previous decade, there had been considerable variation regarding the age at which young male players learned to body check, ranging from nine to 14 years depending on the year and province (11). Although the rules of hockey are similar for both males and females, there is one significant exception: intentional body contact (ie, body checking, bumping, shoving, pushing) is not permitted at any level in female hockey and results in a penalty (12). Accidental and unintended contact between players, however, does occur and remains an important cause of injury (3,13). At the current time, there are no injury-prevention programs targeted specifically to either sex.
In the present study, our objective was to compare the injuries among youth female and male hockey players using the Canadian Hospitals Injury Reporting and Prevention Program Database (CHIRPP) over a 15-year period. We anticipated that males and females would have different injury profiles, and that this information will be useful in informing further studies regarding sex-specific injury prevention initiatives in minor hockey.
METHODS
CHIRPP is a computerized information system that collects and analyzes data regarding injuries to individuals (mainly children) who are seen at the emergency rooms of 10 paediatric and four general hospitals in Canada. CHIRPP is a unique, richly detailed database of injury information obtained by asking patients or care-givers questions such as “What was the injured person doing when the injury happened?”, “What went wrong?” and “Where did the injury occur?” in addition to patient demographic information (14). CHIRPP participation is voluntary.
A retrospective study was conducted using the CHIRPP database, with approval from the Western University Research Ethics Board (London, Ontario). For the present study, CHIRPP data pertaining to children seven to 17.5 years of age who sustained recreational hockey-related injuries between January 1, 1995 and December 31, 2009 were requested from the Public Health Agency of Canada. The lower limit of the age range represents the age at which many players enter hockey, while the upper limit represents the upper age bracket seen by most paediatric emergency departments in Canada. The information used for the analysis included age, sex, date of injury, injury type, mechanism of injury, body part(s) involved and patient disposition. Players who were injured in nonleague play (ie, games that did not involve coaches or officials) and players who were injured on the road, at home or in a yard were excluded. Professional hockey players (ie, individuals receiving a salary for playing hockey) were also excluded.
Descriptions of how injuries occurred were classified as one of four mechanisms: body checking, collision, fall or other. A research assistant involved in the study performed the injury classification, with the assistance of authors KF and GS. Narratives in the column “What happened?” that contained the terms ‘checked’, ‘check’, ‘cross checked’, ‘pushed/hit from behind’, ‘hit against/into boards’, ‘was hit by other/another player’, ‘got hit by other/another player’, ‘hit by elbow’, ‘elbowed’, ‘hit by knee’, ‘kneed’, ‘mis en échec’, ‘heurté’ and ‘plaqué’ were classified as body checking, using automated methodology described by Cusimano et al (15). Players were categorized as having had a ‘collision’ if there was reported contact with an object such as the net, goalpost, boards or another player (not body checking). Players who described a fall, slip or trip leading to their injury were classified as having experienced a ‘fall’. Those classified as having ‘other’ injury mechanisms reported a variety of injury causes that did not fall into the aforementioned categories (eg, high stick, hit by puck, run over by a skate). All players were classified according to the first potential mechanism listed in the narrative, and uncertainty regarding mechanism classification was resolved through discussion among the authors.
Statistical analysis was performed using Excel (Microsoft Corporation, USA) and SPSS version 20 (IBM Corporation, USA). Player age was described using means and SDs. Categorical variables (eg, injury types, injured body regions, injury mechanisms) were summarized as percentages and analyzed using the χ2 test with Yates’ correction for multiple testing, and the Fisher Exact test. Given the large sample size, the type 1 error rate was decreased to 1% for significance. Differences between proportions were only considered to be clinically important if there was an absolute difference of >5%.
RESULTS
In total, 33,233 children in the CHIRPP database met the study’s inclusion criteria. Of these, 2637 (7.9%) were female and 30,596 (92.1%) were male. The mean (± SD) age was 13.7±2.1 years. The distribution of players according to age group is presented in Table 1. The age groups listed correlate with Hockey Canada’s current age divisions: Novice, seven to eight years of age; Atom, nine to 10 years of age; PeeWee, 11 to 12 years of age; Bantam, 13 to 14 years of age; and Midget, 15 to 17 years of age (16). For both sexes, the majority of injured players presenting to the emergency department were in the 13 to 14 year age group. In each age cohort, no significant differences were observed in the proportion of injured female and male hockey players.
TABLE 1.
Total number of injured female and male hockey players according to age group
| Age, years | Female | Male | P |
|---|---|---|---|
| 7–8 | 73 (2.8) | 876 (2.9) | 0.85 |
| 9–10 | 245 (9.3) | 2641 (8.6) | 0.25 |
| 11–12 | 558 (21.2) | 6756 (22.1) | 0.28 |
| 13–14 | 916 (34.7) | 10,888 (35.6) | 0.39 |
| 15–17 | 845 (32) | 9435 (30.8) | 0.20 |
| Total | 2637 (100) | 30,596 (100) | – |
Data presented as n (%) unless otherwise indicated
A description of the injuries reported by players and/or care-givers is presented in Table 2. The top three injuries for females were soft tissue injuries, sprains/strains and fractures. For males, soft tissue injuries were followed by fractures and sprains/strains. Significant differences according to sex were noted in the proportion of soft tissue injuries and fractures.
TABLE 2.
Frequency of hockey-related injuries in females and males according to injury type, body region and mechanism
| Injury | Female (n=2637) | Male (n=30,596) | P |
|---|---|---|---|
| Injury type, % | |||
| Soft tissue | 1049 (39.8) | 9964 (32.6) | <0.01* |
| Sprains/strains | 556 (21.1) | 5391 (17.6) | <0.01 |
| Fractures | 480 (18.2) | 8286 (27.1) | <0.01* |
| Minor head injury | 265 (10) | 2478 (8.1) | <0.01 |
| Concussion | 205 (7.8) | 1962 (6.4) | <0.01 |
| Other | 93 (3.5) | 1155 (3.8) | 0.55 |
| Open wound | 63 (2.4) | 1788 (5.8) | <0.01 |
| Dislocation | 44 (1.7) | 725 (2.4) | 0.02 |
| Intracranial injury | 2(0.1) | 15 (0.0) | 0.64 |
| Injured body region | |||
| Upper extremity | 1033 (39.2) | 13,816 (45.2) | <0.01* |
| Head/neck | 750 (28.4) | 7693 (25.1) | <0.01 |
| Lower extremity | 611 (23.2) | 6543 (21.4) | 0.03 |
| Abdomen/thorax | 283 (10.7) | 2957 (9.7) | 0.80 |
| Systemic or multiple injuries | 10 (0.4) | 132 (0.4) | 0.88 |
| Injury mechanism | |||
| Collision | 754 (28.6) | 7528 (24.6) | <0.01 |
| Checking | 679 (25.7) | 13,086 (42.8) | <0.01* |
| Falls | 666 (25.3) | 4541 (14.8) | <0.01* |
| Other | 538 (20.4) | 5441 (17.8) | <0.01 |
Some injured players reported up to three different injuries per player.
Denotes both a statistically and clinically significant (>5%) difference between females and males
The five most common injuries from Table 2 were further examined according to player age and sex (Figure 1). The number of soft tissue injuries was fairly evenly distributed in both sexes across the age groups (Figure 1A). Males also showed a similar distribution of sprains/strains across all age groups, whereas females exhibited a spike in sprains/strains among 15- to 17-year-old players (Figure 1B). Males between 11 and 17 years of age experienced proportionately more fractures than females (Figure 1C). Concussions in male players were similarly distributed across all ages (Figure 1D), with a statistically significant difference in concussions at seven to eight years of age. The number of minor head injuries peaked in young male players (nine to 10 years of age) and decreased with age (Figure 1E). For female players, there was a trend toward more concussions in older players, with a peak among 13- to 14-year-olds (Figure 1D); however, no clear patterns were observed for minor head injuries among females (Figure 1E).
Figure 1).
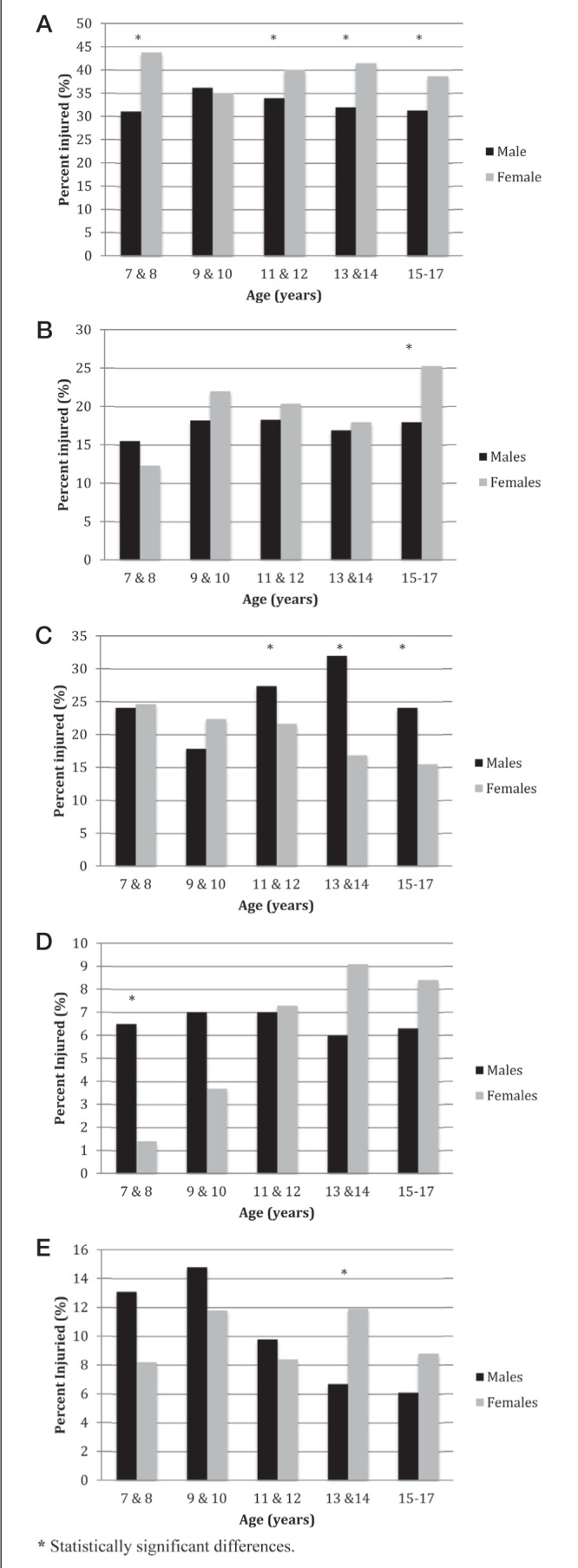
Relative percentage of injury types reported according to age and sex. A Soft tissue injuries; B Sprains and strains; C Fractures; D Concussions; E Minor head injuries
Injuries according to body region are summarized in Table 2. Injuries to the upper extremities were the most common in both sexes, followed by injuries to the head/neck. Males experienced significantly more upper extremity injuries than females. The code “multiple injuries of more than one nature” was only used in the description of injuries of two individuals: a female who collided with the boards and required admission to hospital, and a male requiring outpatient follow-up after being stepped on by a skate. Of the players who sustained systemic injuries, four male individuals required admission to hospital: three due to body checking, and one due to a fall.
The injury mechanisms are listed at the bottom of Table 2. Among females, collisions were the most common cause of injury; however, injuries were relatively evenly distributed across all mechanisms. Significantly more females than males were injured through falls. For males, body checking was the most commonly attributable cause of injury, followed by collisions.
On discharge from hospital, the majority of female (96.9%) and male (96.7%) patients had received treatment and advice in the emergency department, with or without outpatient follow-up (P=0.60). Admissions to hospital were reported by 2.6% of females and by 3.1% of males (P=0.18). Two males were admitted directly to intensive care due to their injuries: one with internal injuries secondary to an abdominal injury, and the other with a fracture/dislocation. A total of 12 females and 53 males left emergency departments without being seen.
DISCUSSION
Although previous studies have attempted to describe injury patterns in young female hockey players, they have been limited by either small sample size or localized geographical sampling (3,4). To our knowledge, the present study is the largest to date examining injury patterns in female paediatric hockey players, with 2637 reported injuries to females.
In 2010, a study by Deits et al (17), investigating the injury profiles of males and female players (all ages) presenting to United States emergency departments, showed that females most commonly sustained head injuries, followed by wrist/hand/finger and facial injuries, whereas males sustained more injuries to the face, shoulder/upper arm and wrist/hand/fingers. In both sexes, the peak age of injury occurred in adolescence (3,17). Players 13 to 17 years of age in our database represented 66% of all reported injuries, which is consistent with past research.
Females in our study presented with proportionately more soft tissue injuries and sprains/strains (among 15- to 17-year-olds), than males, who experienced proportionately more fractures and injuries to upper extremities (ie, shoulders). Previous studies have highlighted sprains/strains as being common among female hockey players. In a recent study by Dryden et al (5), sprains and strains represented 52% of all female hockey injuries, whereas Keightley et al (3) reported these to be the most common injury among competitive youth female hockey players. Risk factors for increased risk of sprains and strains in female hockey players, and the effect of age on injury is a potentially interesting area of future study. We hypothesize that among males, the increased proportion of upper body injuries, such as those involving the shoulder, as well as fractures, are partly attributable to injury mechanism – with body checking causing 42.8% of injuries among male players, and collisions (including unintentional contact) causing 24.6%. Body checking has received considerable attention for its role in contributing to severe injuries such as concussions, fractures, dislocations and other high-impact injuries (18,19). In our study, we could not determine which injury trends in males were specifically attributable to body checking. The multiple checking rule changes that have occurred in some male leagues over the long study period makes this attribution particularly challenging. In female hockey, although body checking is prohibited, we found that it was the reported cause in 25.7% of female hockey injuries. Because parents do not always indicate whether a collision with another player was intentional, it is possible that some of these ‘collisions’ were truly ‘body checks’ and vice versa. Given the retrospective nature of the present study, we are unable to determine whether this is true. Among females, 28.6% of injuries were attributable to collisions and/or unintentional body contact. The potential for injury related to unintentional body contact should not be underestimated; accidental and unintended contact between players does occur and remains an important cause of injury (3,13).
Head injuries and concussions are of great importance to children, parents and health practitioners. In our study, although not statistically significant in all ages, a trend toward more concussions and minor head injuries among older female players was noted (Figure 1D). However, without knowing the size of the population at risk, we are unable to show whether this trend reflects increased rates of concussion in this group. Among males in our study, the proportion of concussions remained relatively constant among all ages, with proportionately more males than females presenting with concussions at younger ages. This suggests that the reasons behind concussions are likely multifactorial and not simply attributable to body checking.
The trend toward proportionately more concussions in female athletes would be consistent with findings described in previous studies. Among female hockey players at the university level, concussions are the most commonly reported injury (7,20). This finding, however, is not well explained in biomechanical studies involving university female hockey players, which show female players sustain fewer hits, less forceful hits and less rotational acceleration during hits than males (21). Further research is required to explain contributory factors surrounding concussions in girls and how they can be prevented.
Although the present study was the largest to date comparing injury patterns of female and male hockey players, our study had several limitations. First, the CHIRPP database only captures patients who present to one of the 14 participating urban hospitals and who voluntarily complete the data collection form; thus, injuries seen in other emergency departments, by family physicians and minor injuries not seen by a doctor will be under-represented. Due to the limitations of our database, we did not have access to other information that would have strengthened our analysis such as province and level of competition, player position, team composition, previous injuries, practice versus game-play, patient height/weight, the size of the population at risk and follow-up information after hospital discharge. During our study period, the age at which body checking was introduced has varied dramatically: from nine years of age (between 2003 and 2009 in four of 13 provincial/territorial branches) to 14 years of age (in Quebec from 1978 to 2002). Between 2009 and 2012, body checking was introduced to 11- to 12-year-old male players in all provinces except Quebec, where it is introduced at 13 years of age (11). We also acknowledge that with a large sample size, many comparisons between groups will be statistically significant without necessarily being clinically significant. We attempted to address this issue by only considering absolute differences in proportions of >5% as being clinically significant, and by decreasing the type 1 error rate to 1%. Also, the analysis of the data was undertaken as a whole and, as such, we do not know whether over this period of time any new trends have emerged. A comparison of the past five years versus the previous fifteen years would be interesting to determine whether this would yield any differences.
In the largest study to date, we have demonstrated that female and male youth hockey players generally report similar patterns of injuries – with several important exceptions. Females report more soft tissue injuries and sprains/strains in older adolescents, as well as injuries secondary to falls. Although not permitted, body checking remains an important cause of injury for females. Males experience more fractures, upper extremity injuries and injuries due to body checking. Potential focuses for injury reduction may include modification of female-specific equipment for better protection against soft tissue injuries and strains/sprains. More studies in the areas of sprain/strain patterns in older female hockey players, concussions in females, and the effect of body checking rule changes on male hockey are warranted.
Acknowledgments
Data used in this article are from the CHIRPP and are used with the permission of the Public Health Agency of Canada. The analyses and interpretations presented in this work do not necessarily reflect the opinions of the federal government. The authors thank Cindy Langford for her role in injury classification for this analysis.
Footnotes
ETHICS: Research Ethics Board approval was granted through Western University (London, Ontario).
REFERENCES
- 1.Hockey Canada. Female Hockey: Statistics & History. < www.hockeycanada.ca/en-ca/Hockey-Programs/Female/Statistics-History.aspx> (Accessed December 3, 2013)
- 2.Hockey Canada. Hockey Canada Basics: Registration Statistics. < www.hockeycanada.ca/en-ca/Corporate/About/Basics/Registration.aspx> (Accessed December 3, 2013)
- 3.Keightley M, Reed N, Green S, Taha T. Age and competition level on injuries in female ice hockey. Int J Sports Med. 2013;34:756–9. doi: 10.1055/s-0032-1327574. [DOI] [PubMed] [Google Scholar]
- 4.Decloe MD, Meeuwisse WH, Hagel BE, Emery CA. Injury rates, types, mechanisms and risk factors in female youth ice hockey. Br J Sports Med. 2014;48:51–6. doi: 10.1136/bjsports-2012-091653. [DOI] [PubMed] [Google Scholar]
- 5.Dryden DM, Francescutti LH, Rowe BH, Spence JC, Voaklander DC. Personal risk factors associated with injury among female recreational ice hockey players. J Sci Med Sport. 2000;3:140–9. doi: 10.1016/s1440-2440(00)80076-6. [DOI] [PubMed] [Google Scholar]
- 6.Dryden DM, Francescutti LH, Rowe BH, Spence JC, Voaklander DC. Epidemiology of women’s recreational ice hockey injuries. Med Sci Sports Exerc. 2000;32:1378–83. doi: 10.1097/00005768-200008000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Agel J, Dick R, Nelson B, Marshall SW, Dompier TP. Descriptive epidemiology of collegiate women’s ice hockey injuries: National collegiate athletic association injury surveillance system, 2000–2001 through 2003–2004. J Athl Train. 2007;42:249–54. [PMC free article] [PubMed] [Google Scholar]
- 8.Agel J, Harvey EJ. A 7-year review of men’s and women’s ice hockey injuries in the NCAA. Can J Surg. 2010;53:319–23. [PMC free article] [PubMed] [Google Scholar]
- 9.Deits J, Yard EE, Collins CL, Fields SK, Comstock RD. Patients with ice hockey injuries presenting to US emergency departments, 1990–2006. J Athl Train. 2010;45:467–74. doi: 10.4085/1062-6050-45.5.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hockey Canada. Hockey Canada’s 94th Annual General Meeting concludes in Charlottetown, P.E.I.; body-checking rule change approved; Jim Hornell elected chair of Hockey Canada Board of Directors; < www.hockeycanada.ca/en-ca/news/agm-concludes-incharlottetown> (Accessed December 3, 2013) [Google Scholar]
- 11.Houghton K, Emery C, Canadian Paediatric Society, Healthy Active Living and Sports Medicine Committee Bodychecking in youth ice hockey. Paediatr Child Health. 2012;17:509. doi: 10.1093/pch/17.9.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hockey Canada. Referee’s Case Book/Rule Combination 2012–2014. < http://cdn.agilitycms.com/hockey-canada/Hockey-Programs/Officiating/Downloads/rulebook_casebook_e.pdf> (Accessed December 3, 2013)
- 13.Darling SR, Schaubel DE, Baker JG, Leddy JJ, Bisson LJ, Willer B. Intentional versus unintentional contact as a mechanism of injury in youth ice hockey. Br J Sports Med. 2011;45:492–7. doi: 10.1136/bjsm.2009.063693. [DOI] [PubMed] [Google Scholar]
- 14.Public Health Agency of Canada. CHIRPP: A Unique Source of Child Injury Information. < www.phac-aspc.gc.ca/injury-bles/chirpp/> (Accessed August 8, 2014)
- 15.Cusimano MD, Taback NA, McFaull SR, Hodgins R, Bekele TM, Elfeki N, Canadian Research Team in Traumatic Brain Injury and Violence Effect of bodychecking on rate of injuries among minor hockey players. Open Med. 2011;5:e57–64. [PMC free article] [PubMed] [Google Scholar]
- 16.Hockey Canada. Age Change General Information. < www.hockeycanada.ca/index.php/ci_id/14666/la_id/1/ss_id/63659.htm/> (Accessed February 15, 2013)
- 17.Deits J, Yard EE, Collins CL, Fields SK, Comstock RD. Patients with ice hockey injuries presenting to US emergency departments, 1990–2006. J Athl Train. 2010;45:467–74. doi: 10.4085/1062-6050-45.5.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emery CA, Hagel B, Decloe M, Carly M. Risk factors for injury and severe injury in youth ice hockey: A systematic review of the literature. Inj Prev. 2010;16:113–8. doi: 10.1136/ip.2009.022764. [DOI] [PubMed] [Google Scholar]
- 19.Macpherson A, Rothman L, Howard A. Body-checking rules and childhood injuries in ice hockey. Pediatrics. 2006;117:e143–7. doi: 10.1542/peds.2005-1163. [DOI] [PubMed] [Google Scholar]
- 20.Agel J, Harvey EJ. A 7-year review of men’s and women’s ice hockey injuries in the NCAA. Can J Surg. 2010;53:319–23. [PMC free article] [PubMed] [Google Scholar]
- 21.Brainard LL, Beckwith JG, Chu JJ, et al. Gender differences in head impacts sustained by collegiate ice hockey players. Med Sci Sports Exerc. 2012;44:297–304. doi: 10.1249/MSS.0b013e31822b0ab4. [DOI] [PMC free article] [PubMed] [Google Scholar]


