Abstract
OBJECTIVE:
To determine potential risk factors for developing positional plagiocephaly in infants seven to 12 weeks of age in Calgary, Alberta.
METHODS:
A prospective cohort design was used. Healthy term infants (n=440), seven to 12 weeks of age, from well-child clinics at four community health centres in Calgary, Alberta were assessed by the primary author and a registered nurse research assistant using Argenta’s plagiocephaly assessment tool. Parents completed a questionnaire surveying risk factors.
RESULTS:
The incidence of positional plagiocephaly was estimated to be 46.6%. The following risk factors were identified using multiple logistic regression: right-sided head positional preference (OR 4.66 [95% CI 2.85 to 7.58]; P<0.001), left-sided head positional preference (OR 4.21 [95% CI 2.45 to 7.25]; P<0.001), supine sleep position (OR 2.67 [95% CI 1.58 to 4.51]; P<0.001), vacuum/forceps assisted delivery (OR 1.88 [95% CI 1.02 to 3.49]; P=0.04) and male sex (OR 1.55 [95% CI 1.00 to 2.38]; P=0.05).
CONCLUSION:
Advice to vary infants’ head positions needs to be communicated to parents/guardians well before the two-month well-child clinic visit. This could occur in the prenatal period by prenatal care providers or educators, or during the neonatal period by postpartum and public health nurses. Prevention education may be emphasized for parents/guardians of male infants and infants who have had assisted deliveries.
Keywords: Deformational plagiocephaly, Nonsynostotic plagiocephaly, Positional plagiocephaly, Prevention, Risk factors
Abstract
OBJECTIF :
Déterminer les facteurs de risque potentiels de plagiocéphalie positionnelle chez les nourrissons de sept à 12 semaines à Calgary, en Alberta.
MÉTHODOLOGIE :
Dans une cohorte prospective, des nourrissons à terme et en santé (n=440) de sept à 12 semaines provenant de cliniques d’enfants en santé de quatre centres de santé communautaire de Calgary, en Alberta, ont été évalués par l’auteur principal et une infirmière adjointe à la recherche au moyen de l’outil d’évaluation de la plagiocéphalie d’Argenta. Les parents ont rempli un questionnaire pour déterminer les facteurs de risque.
RÉSULTATS :
L’incidence de plagiocéphalie positionnelle a été évaluée à 46,6 %. Les facteurs de risque suivants ont été déterminés au moyen de la régression logistique multiple : préférence positionnelle de la tête à droite (RC 4,66 [95 % IC 2,85 à 7,58]; P<0,001), préférence positionnelle de la tête à gauche (RC 4,21 [95 % IC 2,45 à 7,25]; P<0,001), position de sommeil en décubitus dorsal (RC 2,67 [95 % IC 1,58 à 4,51]; P<0,001), accouchement assisté par ventouses ou forceps (RC 1,88 [95 % IC 1,02 à 3,49]; P=0,04) et sexe masculin (RC 1,55 [95 % IC 1,00 à 2,38]; P=0,05).
CONCLUSION :
Il faut conseiller aux parents ou aux tuteurs de modifier la position de la tête du nourrisson bien avant le rendez-vous à la clinique pour enfants en santé à deux mois. Ces conseils pourraient être donnés pendant la période prénatale par les dispensateurs ou les éducateurs de soins prénatals ou par des infirmières postnatales ou des infirmières de santé publique pendant la période néonatale. On peut donner des conseils de prévention aux parents ou aux tuteurs des nourrissons de sexe masculin et de ceux qui ont eu un accouchement assisté.
In February 1999, a joint statement was released in Canada recommending that infants be placed to sleep on their backs to prevent sudden infant death syndrome (SIDS) (1). Subsequently, concerns have been raised about a consequent increase in positional plagiocephaly across Canada. Plagiocephaly is defined as a deformation of the skull producing the appearance of a lopsided head (2). Plagiocephaly is of concern because, if not diagnosed and treated early, the associated changes in skull shape and facial features can be permanent (3). Literature regarding risk factors for developing positional plagiocephaly indicates variation according to infant age. Only two published studies address risk factors for infants six to seven weeks of age (4,5). The objective of the present study was to identify risk factors for developing positional plagiocephaly in infants seven to 12 weeks of age in Calgary, Alberta. We used the modifiable risk factors to identify areas for messages for parents to prevent plagiocephaly from developing.
METHODS
A prospective cohort design was used to identify risk factors for developing positional plagiocephaly. Ethics approval was received from the University of Calgary Conjoint Health Research Ethics Board (Calgary, Alberta) on June 3, 2010. Healthy full-term infants (born at ≥37 weeks’ gestation) ranging from seven to 12 weeks of age who presented for immunization at two-month well-child clinics in Calgary were included in the study. Data collection occurred in four community health centres (CHCs) from July to September 2010. Each CHC was situated in one quadrant of the city, increasing the likelihood that the results would be representative of the larger population in Calgary. A sample size of 384 was adequate to detect population incidence (6). After receiving informed consent, plagiocephaly assessments using Argenta’s five-point scale (7) were completed by the primary author or a trained registered nurse. Parents were asked to complete a questionnaire surveying risk factors that was developed for the present study. Seven nonmodifiable risk factors generated from the literature review were included: infant birth order; maternal delivery type; infant sex; multiple gestation; infant age; maternal age; and maternal number of years lived in Canada. Six modifiable risk factors generated from the literature were considered in the present study: infant sleep position; infant head positional preference; infant feeding position; infant tummy time; maternal education; and maternal language barrier.
Statistical analysis
PASW version 17 (IBM Corporation, USA) was used to perform the analysis. χ2 tests, independent-sample t tests and Mann-Whitney tests were performed. In all cases, P≤0.05 was considered to be statistically significant.
After determining which variables were multicollinear, the following predictive factors of plagiocephaly were used in this analysis: infant sleep position; infant tummy time; birth order; sex; multiple gestation; left head positional preference; right head positional preference; vacuum/forceps delivery; Cesarean section delivery; and maternal education. The following multiple logistic regression model was used in the present study:
in which p = P (Y=1). For every independent variable in the model, at least 10 cases are needed (8). Because 205 infants who participated in the study were observed to have positional plagiocephaly, this convention would allow for up to 20 variables to be included in the multiple regression model. Therefore, the 10 variables identified above were an acceptable number to be included in the model. For this exploratory research, the ‘all variables in’ method was used for model building to avoid the risk of eliminating or not selecting a variable that was on the causal pathway to the outcome in favour of a variable that was a confounder (8). A variable with P<0.05 was considered to be statistically significant.
RESULTS
During the data collection time frame, 1712 infants were eligible to participate in the study. Of the 486 (28.4% of eligible) parents/guardians of infants approached to participate in the study, 440 met the inclusion criteria and were consecutively recruited (Figure 1). Of the 440 infants, plagiocephaly was identified in 205 (9). Right-sided flattening was present in 63.8% of plagiocephaly cases, whereas 36.2% were observed to have left-sided flattening. Of all infants assessed, 48.6% were first born, 53.2% were delivered vaginally, 59.3% were male and 3.9% were part of a multiple pregnancy. The mean age of infants in the study was nine weeks. Mothers’ ages ranged from 17 to 47 years, with a mean of 30.3 years for mothers whose infants presented with plagiocephaly and a mean age of 31.3 years for mothers with infants without plagiocephaly. The average length of time lived in Canada for mothers whose infants presented with plagiocephaly was 21.6 years and 22.6 years for mothers with infants without plagiocephaly.
Figure 1).
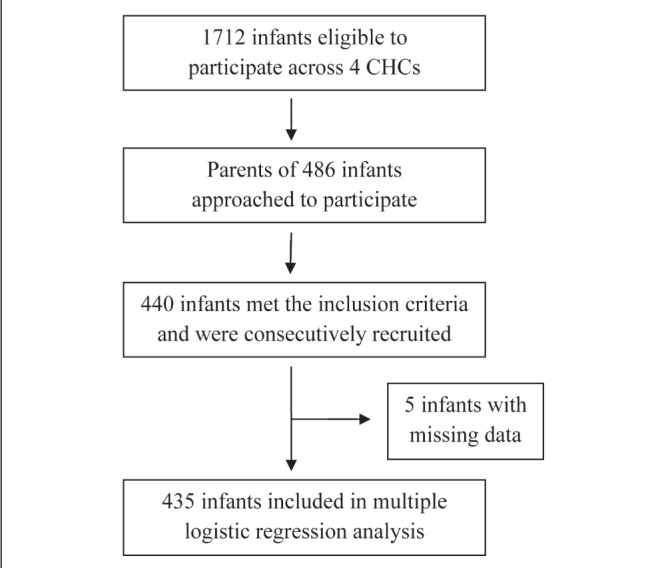
Flow chart for sample used in statistical modelling
Multiple regression analysis included 435 infants. There was no difference in the incidence of plagiocephaly between infants who were first born compared with not first born (χ21=0.19; P=0.66); according to sex (χ21=1.55; P=0.21); among delivery types (vaginal, vacuum/forceps or Cesarean section) (χ21=2.46; P=0.29); between multiple gestation and singleton pregnancies (χ21=0.90; P=0.34); and average length of time in Canada (t438=0.94; P=0.35).
Of all infants assessed, 76.1% were usually placed supine to sleep; 58.0% of parents noticed a positional preference while their infant(s) were positioned supine; 91.8% of infants were fed while in the caregivers’ arms, 57.5% of the infants received tummy time <3 times per day. The majority of mothers (76.2%) had completed education beyond high school. Two percent (n=9) of mothers were observed to have a language barrier while communicating with the authors.
There was no association between plagiocephaly and infant feeding position (χ21=0.07; P=0.76); length of tummy time received (χ21=0.05; P=0.83); and infants of mothers who had a language barrier compared with those who did not (χ21=3.59; P=0.09). There was a difference in the incidence of plagiocephaly in infants who were placed supine to sleep compared with those who were placed to sleep in other positions including prone, side or a combination of supine, prone or side (χ21=11.90; P=0.001). Fifty-one percent of infants placed supine to sleep developed positional plagiocephaly compared with 31.7% of infants placed in other sleep positions. There was a significant difference in incidence of plagiocephaly between the infants who exhibited a head positional preference compared with those who did not (χ22=52.17, P<0.001). Sixty-one percent of infants with a preference were found to have plagiocephaly compared with 26.5% of infants with no preference. There was a difference in incidence of plagiocephaly according to maternal education, with infants of mothers with the equivalent of grade 12 education or less having a greater incidence of plagiocephaly (χ21=4.74; P=0.03).
Results of the multivariate logistic regression analysis are presented in Table 1. Comparing infants who did not sleep supine, infants who slept supine had 2.7 times the odds of developing positional plagiocephaly. Male infants had 1.55 times the odds of developing positional plagiocephaly. Compared with infants delivered vaginally with no assistance, infants who had an assisted delivery (forceps or vacuum) had almost two times the odds of developing positional plagiocephaly. Compared with infants who did not have a head positional preference, infants with either a right-sided head positional preference or a left-sided head positional preference had >4 times the odds of developing positional plagiocephaly.
TABLE 1.
Adjusted multivariable logistic regression model of risk factors predictive of positional plagiocephaly (n=435)
| Variable | B | SE | Wald | Df | P | OR | 95% CI |
|---|---|---|---|---|---|---|---|
| Supine sleep position | 0.98 | 0.27 | 13.51 | 1 | <0.001* | 2.67 | 1.58–4.51 |
| Tummy time | −0.08 | 0.22 | 0.12 | 1 | 0.73 | 0.93 | 0.61–1.41 |
| First birth | −0.15 | 0.22 | 0.44 | 1 | 0.51 | 0.86 | 0.56–1.33 |
| Male infant sex | 0.44 | 0.22 | 3.91 | 1 | 0.05* | 1.55 | 1.00–2.38 |
| Multiple pregnancy | −0.33 | 0.57 | 0.33 | 1 | 0.57 | 0.72 | 0.24–2.19 |
| Maternal postsecondary education | −0.35 | 0.25 | 1.89 | 1 | 0.17 | 0.71 | 0.43–1.16 |
| Delivery type | |||||||
| Vaginal | 6.43 | 2 | 0.04* | ||||
| Vacuum/forceps | 0.63 | 0.32 | 4.05 | 1 | 0.04* | 1.88 | 1.02–3.49 |
| Cesarean section | −0.23 | 0.25 | 0.87 | 1 | 0.35 | 0.80 | 0.49–1.23 |
| Head positional preference | |||||||
| Overall | 46.23 | 2 | <0.001* | ||||
| Right | 1.54 | 0.25 | 38.59 | 1 | <0.001* | 4.66 | 2.85–7.58 |
| Left | 1.44 | 0.28 | 26.91 | 1 | <0.001* | 4.21 | 2.45–7.25 |
| Constant | −1.72 | 0.40 | 18.34 | 1 | <0.001 | 0.180 |
Significant at 0.05 level. B Beta regression coefficient
DISCUSSION
Five factors in the adjusted multivariable model were found to be associated with plagiocephaly: supine sleep positioning; sex; delivery type; right-sided head positional preference; and left-sided head positional preference.
Supine sleep positioning
The results of the present study revealed that infants who sleep in the supine position had approximately 2.7 times the odds of developing positional plagiocephaly compared with infants who were not placed supine. Similar results were found by Hutchinson et al (4) and Glasgow et al (10) with regard to supine sleep positioning. Given that supine sleep positioning is recommended to reduce the incidence of SIDS (1), this sleep position is not regarded as a modifiable risk factor. The importance of continuing to recommend that all healthy infants be placed supine to sleep to prevent SIDS cannot be overemphasized. Supine sleep position has been reported to reduce the risk of SIDS and, indeed, SIDS mortality in Canada decreased from 144 deaths (26% of all post-neonatal deaths) in 1999 to 76 deaths (18% of all postneonatal deaths) in 2004 (11). Consequently, although supine sleep positioning increases the risk of developing positional plagiocephaly, its benefit of decreasing the risk of infant mortality far outweighs potential gains in reducing the incidence of positional plagiocephaly. In addition, there are reliable techniques to reduce the risk of developing positional plagiocephaly (12), and treatment options exist to correct it (13,14).
Sex
Males are at an increased risk for developing positional plagiocephaly. Male infants had 1.5 times higher odds of developing positional plagiocephaly compared with females. In the present study, males were slightly over-represented and comprised 59.3% of the sample. Male sex is a plausible risk factor that can be explained by the occurrence of generally larger head circumferences. The larger and less flexible male head makes it more susceptible to compression in utero and deformational forces during delivery (15). The more rapidly growing male head may increase gravitational forces postdelivery that contribute to the development of positional plagiocephaly (5), especially when a position of comfort has already been established. Similar results have been found in other studies (5,16–19).
Delivery type
We compared unassisted vaginal deliveries with assisted deliveries (forceps and vacuum) and Cesarean section. In the present study, 30.2% of mothers underwent a Cesarean section. This is higher than the national average rate of Cesarean deliveries of 25.6 per 100 deliveries (20). In addition, 16.6% of mothers in the present study had assisted deliveries including either forceps or vacuum. Again, this is higher than the national average, wherein 14.8% of deliveries included forceps or vacuum extraction of the infant (21). Infants with an assisted delivery (forceps or vacuum) had 1.9 times the odds of developing positional plagiocephaly than infants who were delivered vaginally with no assistance. Delivery type is a plausible risk factor because the instruments used may compress the skull of the infant being delivered. Positional plagiocephaly may develop if the infant is continuously placed on the side of the head that had been compressed during assisted vaginal delivery. Similar results were found in other studies (16,17).
Head positional preference and the side of head that plagiocephaly was observed
Our results indicate that when an infant had a right-sided or left-sided head positional preference, he/she had >4 times the odds of developing positional plagiocephaly than an infant who did not have a head positional preference. In our study, right-sided flattening was present in 63.8% of plagiocephaly cases. The right-sided preference may result from events toward the latter period of pregnancy when the fetus turns and engages the birth canal, usually head down. Frequently, the vertex of the head lies within the birth canal with a left occipital anterior presentation (15). Thus, the fetus’ right occiput is compressed against the maternal pelvis and the left forehead against the lumbosacral spine (15,16). This position may initiate a preference for postnatal supine sleep positioning or feeding positioning, resulting in the preference for right-sided head turning and allowing for a position of comfort to be established (15). It is this position of comfort that contributes to the compressive force on the right occiput that may result in positional plagiocephaly. Other studies have also reported that occipital cranial flattening is more frequently observed on the right side (15,18,22).
Positional preference may develop as a result of not varying infant head positions when putting them to sleep or offering feeding consistently from either the left or right side (23). Infants with plagiocephaly are significantly less likely to have their head positions varied when put to sleep (4,5,10,18,24). Glasgow et al (10) found that varying infants’ sleep position served as a protective factor and decreased the risk of deformational plagiocephaly. This evidence suggests that varying infants’ head positions after they have been placed supine to sleep would assist in preventing the development of positional plagiocephaly.
Appropriate timeframes for prevention messaging
It is imperative for prevention messaging to begin during pregnancy and be reinforced during the postpartum period. Prevention messages need to focus on varying infants’ head positions, with special emphasis for parents/guardians of male infants and infants who have had assisted deliveries. The use of tummy time as a prevention technique is plausible because it decreases prolonged periods of pressure on one area of the skull. Tummy time assists the infant to develop head control and upper body strength, which promotes supine-to-prone rolling (23). Currently, there are no guidelines regarding the frequency and duration of tummy time an infant should receive. Various avenues for communicating prevention techniques for plagiocephaly exist across different groups of health professionals (12). It would be ideal if parents/guardians could receive this information first from prenatal educators and prenatal care providers (midwives, obstetricians, family doctors). Postpartum nurses could reinforce this information before discharge from the hospital, and public health nurses could explain the importance of such prevention activities and demonstrate strategies in the home environment. Ideally, information pertaining to preventing the development of a head positional preference could be delivered by family physicians and pediatricians who see infants during the first few weeks of life.
Study limitations
One limitation to the present study was that equal representation from all four sites could not be obtained. The majority of study participants were recruited from two of the four community health centres that were located in more affluent neighbourhoods, which may have affected the external validity of the study. Another limitation was that torticollis assessments were not completed due to insufficient space and time available at the centres. Becauses torticollis is a common anomaly that has been linked with plagiocephaly, its impact could then be assessed in terms of a risk factor for the development of positional plagiocephaly (25–29).
CONCLUSION
The present analysis was the first population-based study using a large sample size to identify risk factors for developing positional plagiocephaly in infants seven to 12 weeks of age. The present study provides additional support for the following associations: supine sleep position; male sex; assisted delivery; head positional preference to the right side; and infant head positional preference to the left side. Prevention messages need to focus on varying infants’ head positions with special emphasis for parents/guardians of male infants and infants who have had assisted deliveries. Further research could be completed at well-child clinics to gather information about changes in risk factors over time and across various age ranges.
Footnotes
FUNDING SOURCE: The Faculty of Graduate Studies, University of Calgary provided $3000.00 for data collection for this study. No external funding was secured for this study.
DISCLOSURES: The authors have no financial relationships relevant to this article or conflicts of interest to disclose.
REFERENCES
- 1.Government of Canada, Canadian Paediatric Society, Canadian Institute of Child Health & Canadian Foundation for the Study of Infant Deaths Joint statement on safe sleep: Preventing sudden infant deaths in Canada, 2006. 2011. < www.phac-aspc.gc.ca/hp-ps/dca-dea/stages-etapes/childhood-enfance_0-2/sids/pdf/jsss-ecss2011-eng.pdf> (Accessed June 20, 2012)
- 2.Thomas CL, editor. Taber’s Cyclopedic Medical Dictionary. 18th edn. Philadelphia: FA Davis Company; 1997. [Google Scholar]
- 3.Najarian SP. Infant cranial molding deformation and sleep position: Implications for primary care. J Pediatr Health Care. 1999;13:173–7. doi: 10.1016/S0891-5245(99)90036-6. [DOI] [PubMed] [Google Scholar]
- 4.Hutchison BL, Hutchison LA, Thompson JM, Mitchell EA. Plagiocephaly and brachycephaly in the first two years of life: A prospective cohort study. Pediatrics. 2004;114:970–80. doi: 10.1542/peds.2003-0668-F. [DOI] [PubMed] [Google Scholar]
- 5.van Vlimmeren LA, van der Graaf Y, Boere-Boonekamp MM, et al. Risk factors for deformational plagiocephaly at birth and at 7 weeks of age: A prospective cohort study. Pediatrics. 2007;119:e408–e418. doi: 10.1542/peds.2006-2012. [DOI] [PubMed] [Google Scholar]
- 6.Daniel WW. Biostatistics: A Foundation for Analysis in the Health Sciences. 7th edn. New York: John Wiley & Sons; 1999. [Google Scholar]
- 7.Argenta L. Clinical classification of positional plagiocephaly. J Craniofac Surg. 2004;15:368–72. doi: 10.1097/00001665-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Katz MH. Multivariable analysis: A practical guide for users. New York: Cambridge University Press; 2006. [Google Scholar]
- 9.Mawji A, Robinson Vollman A, Hatfield J, McNeil DA, Sauvé R. The incidence of positional plagiocephaly. Pediatrics. 2013;132:298–304. doi: 10.1542/peds.2012-3438. [DOI] [PubMed] [Google Scholar]
- 10.Glasgow TS, Siddiqi F, Hoff C, Young PC. Deformational plagiocephaly: Development of an objective measure and determination of its prevalence in primary care. J Craniofac Surg. 2007;18:85–92. doi: 10.1097/01.scs.0000244919.69264.bf. [DOI] [PubMed] [Google Scholar]
- 11.Smylie J, Sauvé R. Infant sleep position. What mothers say: The Canadian maternity experiences survey. Ottawa: Public Health Agency of Canada; 2009. Chapter 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cavalier A, Picot M, Artiaga C, et al. Prevention of deformational plagiocephaly in neonates. Early Hum Dev. 2011;87:537–43. doi: 10.1016/j.earlhumdev.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 13.Xia JJ, Kennedy KA, Teichgraeber JF, et al. Nonsurgical treatment of deformational plagiocephaly: A systematic review. Arch Pediatr Adolesc Med. 2008;162:719–27. doi: 10.1001/archpedi.162.8.719. [DOI] [PubMed] [Google Scholar]
- 14.Katzel EB, Koltz PF, Sbitany H, Emerson C, Girotto JA. Real versus perceived improvements of helmet molding therapy for the treatment of plagiocephaly. Plast Reconstr Surg. 2010;126:19e–21e. doi: 10.1097/PRS.0b013e3181dab573. [DOI] [PubMed] [Google Scholar]
- 15.Losee JE, Mason AC, Dudas J, Hua LB, Mooney MP. Nonsynostotic occipital plagiocephaly: Factors impacting onset, treatment, and outcomes. Plast Reconstr Surg. 2007;119:1866–73. doi: 10.1097/01.prs.0000259190.56177.ca. [DOI] [PubMed] [Google Scholar]
- 16.Peitsch WK, Keefer CH, LaBrie RA, Mulliken JB. Incidence of cranial asymmetry in healthy newborns. Pediatrics. 2002;110:e72–e79. doi: 10.1542/peds.110.6.e72. [DOI] [PubMed] [Google Scholar]
- 17.Rubio AS, Griffet JR, Caci H, et al. The moulded baby syndrome: Incidence and risk factors regarding 1,001 neonates. Eur J Pediatr. 2009;168:605–11. doi: 10.1007/s00431-008-0806-y. [DOI] [PubMed] [Google Scholar]
- 18.Hutchison BL, Thompson JM, Mitchell EA. Determinants of nonsynostotic plagiocephaly: A case-control study. Pediatrics. 2003;112:e316–e322. doi: 10.1542/peds.112.4.e316. [DOI] [PubMed] [Google Scholar]
- 19.McKinney CM, Cunningham ML, Holt VL, Leroux B, Starr JR. A case-control study of infant, maternal and perinatal characteristics associated with deformational plagiocephaly. Paediatr Perinatal Epidemiol. 2009;23:332–45. doi: 10.1111/j.1365-3016.2009.01038.x. [DOI] [PubMed] [Google Scholar]
- 20.Liu S, Liston R, Lee L. Rate of Caesarean delivery. In: Bartholomew S, Dzakpasu S, Huang L, et al., editors. Canadian Perinatal Health Report. Ottawa: Public Health Agency of Canada; 2008. [Google Scholar]
- 21.Liu S, Young D, Liston R. Rate of operative vaginal delivery. In: Bartholomew S, Dzakpasu S, Huang L, et al., editors. Canadian Perinatal Health Report. Ottawa: Public Health Agency of Canada; 2008. [Google Scholar]
- 22.Pivar SJ, Scheuerle A. Variable co-diagnosis of plagiocephaly and torticollis in Texas health care facilities. J Craniofac Surg. 2006;17:236–40. doi: 10.1097/00001665-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Dubé K, Flake ML. Early prevention: Occipital flattening of positional origin. Can Nurse. 2003;99:16–21. [PubMed] [Google Scholar]
- 24.Boere-Boonekamp M, van der Linden-Kuiper LT. Positional preference: Prevalence in infants and follow-up after two years. Pediatrics. 2001;107:339–43. doi: 10.1542/peds.107.2.339. [DOI] [PubMed] [Google Scholar]
- 25.Clarren SK. Plagiocephaly and torticollis: Etiology, natural history, and helmet treatment. J Pediatr. 1981;98:92–5. doi: 10.1016/s0022-3476(81)80549-5. [DOI] [PubMed] [Google Scholar]
- 26.Golden KA, Beals SP, Littlefield TR, Pomatto JK. Sternocleidomastoid imbalance versus congenital muscular torticollis: Their relationship to positional plagiocephaly. Cleft Palate Craniofac J. 1999;36:256–61. doi: 10.1597/1545-1569_1999_036_0256_sivcmt_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 27.Pivar SJ, Scheuerle A. Variable co-diagnosis of plagiocephaly and torticollis in Texas health care facilities. J Craniofac Surg. 2006;17:236–40. doi: 10.1097/00001665-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Rogers GF, Oh AK, Mulliken JB. The role of congenital muscular torticollis in the development of deformational plagiocephaly. Plast Reconstr Surg. 2009;123:643–52. doi: 10.1097/PRS.0b013e318196b9be. [DOI] [PubMed] [Google Scholar]
- 29.van Vlimmeren L, Helders P, van Adrichem L, Engelbert R. Torticollis and plagiocephaly in infancy: Therapeutic strategies. Pediatr Rehabil. 2006;9:40–6. doi: 10.1080/13638490500037904. [DOI] [PubMed] [Google Scholar]


