Primary care, according to the American Association of Family Physicians, is “care provided by physicians specifically trained for and skilled in comprehensive first contact and continuing care for persons with any undiagnosed sign, symptom, or health concern (the “undifferentiated” patient) not limited by problem origin (biological, behavioral, or social), organ system, or diagnosis.”1 Primary care forms the backbone of our health care system, providing the first line of contact for innumerable patients who may be referred to specialists based on specific clinical needs.
In the United States, there is a shortage and maldistribution of primary care providers,2 and the increasing number of urgent care clinics that are frequently staffed with mid-level providers adds further testimony to the growing problem of disparities in health care.2,3 It is believed that in the United States, the impact of this shortage will be felt much more in the coming years because of the rising proportion of elderly people, who present with chronic medical illnesses.4
One suggestion to alleviate the primary care shortage is to effectively utilize the available para-medical workforce that includes nurses and other ancillary personnel as points of entry to primary care.5 Among them, dentists, as de facto oral physicians who already play a pivotal role in monitoring medical conditions such as hypertension during patient visits, can be a valuable medical resource.6 Many elderly patients see their dentists more routinely than their medical health care providers (HCPs).7 If dentists or their staffs are adequately trained to identify, monitor, and refer common chronic medical ailments, they can be a good first line of contact in the existing health care system.8
It is equally important that HCPs have the knowledge and training to diagnose common dental conditions. Because of the intricate relationship between diabetes and dental conditions such as periodontitis and the high prevalence of both conditions in the United States, it is crucial for members of the medical and dental communities to understand these interrelationships, inform patients of these conditions, and make appropriate referrals.9
The objective of this article is to provide insights into how both dental and medical professionals can expand their roles to include identifying and referring chronic oral and medical conditions for appropriate care. Specifically, this article will describe and discuss the opportunities and responsibilities of the dental community with regard to the early detection, monitoring, and referral of people with diabetes to an appropriate health care team and the ways in which HCPs can be mindful of the relationship between periodontitis and diabetes and make appropriate referrals to dentists as needed.
Diabetes-Periodontitis Connection
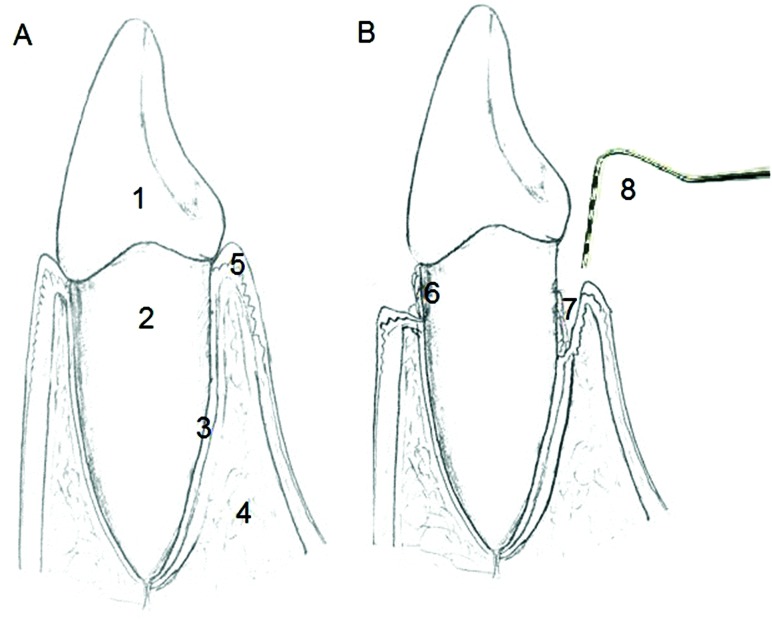
Periodontal diseases are among the most common noncommunicable chronic diseases in the United States.10 Chronic periodontitis, the most common form of periodontal disease, affects the attachment apparatus of the tooth, which includes gingival attachment, periodontal ligament, cementum, and alveolar bone11 (Figure 1). It is caused by gram-negative anaerobes present in dental plaque, but much of the tissue destruction in periodontitis is mediated by the patient’s immune system.11 Of the various local and systemic risk factors for chronic periodontitis, diabetes is considered to be one of the most well-established and validated, aside from tobacco usage, after accounting for various confounders.12 Recent epidemiological studies clearly indicate that close to 47% of the U.S. population has periodontitis,10 with a large proportion of elderly people having severe forms of periodontitis.10
Figure 1.
Diagrammatic illustration of healthy (A) and diseased (B) periodontium. The crown of the teeth is covered by enamel (1). Cementum covering the root (2), periodontal ligament (3), alveolar bone (4), and gingival attachment (5) are the four tissues that comprise the periodontium. In periodontitis subjects, dental plaque is usually seen attached to the root surface, which gets calcified over time (6), deep in the periodontal pocket (7). A periodontal probe is used clinically to diagnose periodontitis (8).
Patients with chronic periodontitis are usually asymptomatic, although some complain of bleeding while brushing (indicative of gingival inflammation), discomfort from extensive mobility of a tooth (resulting from bone loss), or fetid odor.11 Clinically, chronic periodontitis in the earlier stages presents as gingivitis. The classical signs of gingivitis include gingival redness, edema, and bleeding (upon slight clinical manipulation). With appropriate modifications in oral hygiene measures and with professional cleaning, gingivitis usually resolves and therefore is reversible, but when untreated in certain individuals, the gingivitis progresses to chronic periodontitis.11
For diagnosing periodontal conditions, a thorough medical and dental history-taking precedes clinical and radiographic examinations. Clinically, a periodontal probe, a calibrated metal instrument with gradations (in mm), is used to determine the sites affected by chronic periodontitis (Figure 1). The instrument is inserted into the gingival sulcus (space between the teeth and the gingiva), and the distance from the margin of the gingiva to the depth of the sulcus is measured and is termed the “probing depth.” As a general rule, clinically, a probing depth of up to 3 mm is considered normal. With advanced periodontitis, deeper probing depths are noted. Radiographically, clinicians look for bone loss surrounding the tooth affected by periodontitis. The nature and extent of bone loss observed in chronic periodontitis are carefully recorded. The patient’s history, clinical findings, and radiographic findings form the basis for diagnosis, prognosis, and treatment planning. Other than clinical and radiographic examinations, some patients may require additional diagnostics such as microbiological and immunological testing.
Oral manifestations associated with diabetes include periodontitis, dental caries, burning mouth syndrome, candidiasis, salivary dysfunction, and other neurosensory disorders.13 A wide range of soft tissue abnormalities ranging from stomatitis to lichen planus are also noted in people with diabetes. People with diabetes exhibit xerostomia (dry mouth), leading to dysfunction in taste and also increased prevalence of dental caries resulting from reduced clearance of dental plaque microorganisms.13 Patients with diabetes also develop a range of oral bacterial and fungal infections, with a higher prevalence of maxillofacial space infections noted.13 Oral candidiasis is a common finding in individuals with poor glycemic control.13
The interrelationship between diabetes and chronic periodontitis has been studied extensively during the past two decades.14 After controlling for confounders, a significantly higher prevalence of severe periodontitis was noted in patients with poorly controlled diabetes than in those without diabetes (odds ratio 2.90, 95% CI 1.40–6.03).15 Confirming the bi-directional relationship between diabetes and periodontitis, chronic periodontitis was also shown to affect glycemic control in individuals with diabetes, and treatment of chronic periodontitis was shown to modestly improve glycemic control.16
Biologically, diabetes influences chronic periodontitis in multiple ways, with inflammation acting as a bridge between the two conditions.16 Diabetes was shown to upregulate proinflammatory cytokine production and matrix proteases and to alter neutrophil function.17 Diabetes also leads to the formation of advanced glycation endproducts (AGEs), which are “complex, heterogeneous molecules” caused by the linkage of glucose to the amino groups in proteins.17 These molecules interact with several receptors, the best known of which is the receptor for AGE (RAGE), “a multi-ligand receptor . . . found on smooth muscle cells, macrophages, endothelial cells and astrocytes.”17 The interaction of AGEs with RAGE has been shown to initiate a pro-inflammatory response, and the accumulation of AGEs is known to affect both soft and hard tissue healing. The apoptosis of matrix-synthesizing cells such as fibroblasts is common in diabetes and affects overall tissue dynamics, leading to an increased risk of periodontitis.
In addition, obesity, which is very common in people with diabetes, was independently shown to be associated with periodontitis.18 In obese individuals, adipose tissue is known to produce adipokines, which have been shown to have a systemic influence in the oral cavity.19 In addition, the dental plaque of obese individuals tends to harbor more putative periodontal pathogens then that of nonobese individuals.19,20
All of the above mechanisms, in concert, increase the likelihood for chronic periodontitis in people with diabetes.
Potential Role of Dentists
Diabetes is a serious public health concern affecting close to 366 million adults worldwide, a number that is projected to increase to half a billion by 2030.21 In the United States in 2010, close to 8% of the population had diabetes, which increased to 27% among those ≥ 65 years of age.22 Of the 8% of the total population with diabetes, close to 25% are undiagnosed.22 Recent estimates indicate that close to 79 million people in the United States have prediabetes.23 The U.S. Department of Health and Human Services considers testing and early diagnosis of diabetes to be one of the four transition points to reduce the health and economic burden of diabetes by 2020.24
It is known that in 2011, close to 58% of those ≥ 65 years of age visited a dentist compared to 38% of the same age-group who visited a primary care physician.25,26 Because of the several oral manifestations of diabetes and the great impact diabetes has on their treatment outcomes, dentists are well-positioned to and particularly interested in identifying patients with diabetes who are at risk.9 In the United States, it is a common practice to place patients on a dental maintenance (recall) program after completion of active treatment or, in healthy patients, as a preventive measure for their entire lives. This recall program provides a unique opportunity for dentists to closely monitor patients’ chronic medical conditions such as diabetes on a periodic basis.
Diabetes screening
Because of the gradual development of symptoms in patients with type 2 diabetes, a large proportion of patients with the disease are unaware of their condition, just as a large proportion of patients with periodontitis are unaware of their condition. Although type 1 diabetes is a not a preventable condition, many of the risk factors for type 2 diabetes, which accounts for the bulk of diabetes diagnoses nationwide, are modifiable (Table 1).9
Table 1.
Risk Factors for Developing Diabetes

In a study involving 506 dental patients, dentists were able to identify people with diabetes with an accuracy of 92% using periodontal examination (criteria: ≥ 5-mm pocket depths in at least 26% of teeth or missing four teeth) and a point-of-care (POC) A1C value ≥ 5.7%).27 As previously mentioned, the dental office setting, with its frequent follow-up visits, provides the ideal opportunity not only to identify patients with undiagnosed diabetes, but also to monitor glycemic control in people with known diabetes. A recent study28 of blood glucose testing for random plasma glucose levels in community dental practices identified a large proportion of dental patients with diabetes or prediabetes, confirming the promise that the community dental centers hold for diabetes screening and monitoring. More than 80% of patients in that study supported the idea of incorporating blood glucose testing in dental offices.28 Orthodontists, who see their patients once monthly during the patients’ formative years, might also be able to perform screening, particularly as the prevalence of type 2 diabetes increases in the adolescent population.
It is therefore extremely important for dentists to have the knowledge and training necessary to recognize patients who are at high risk for developing diabetes and those with undiagnosed diabetes. More time spent on thorough medical and dental examination and increased interactions with patients’ health care team are essential to providing such coordinated care. In recent years, more dental schools have been incorporating interprofessional educational activities into the dental curriculum to create a dental workforce that will have the training to work with different types of HCPs to render comprehensive care. A mandatory, 1-year general practice residency with a focus on interprofessional care was also suggested as a possible means to facilitate dentists managing medically compromised patients in an interprofessional setting.29
Diabetes monitoring and referral
At the completion of therapy, the dental care provider determines the interval for the patient’s future visits based on both local and systemic factors, and the presence of diabetes is certainly one of the key factors considered in deciding the recall interval. Typically, patients who undergo periodontal therapy are then seen in a 3- to 4-month interval, during which medical and dental records are updated and a professional cleaning is rendered. Periodontally healthy patients are seen typically once every 6 months in the dental office. Therefore, these visits would provide ideal time points for performing tests such as POC A1C or random blood glucose monitoring to assess diabetes control status.
Two recent field trials confirmed the acceptability and feasibility of measuring A1C in dental offices and successfully unveiling previously undiagnosed diabetes.30,31 The screening was shown to be well accepted by the dentist, health care team, and, most importantly, patients.30 When electronic medical and dental records are available to enable the sharing of data and information among different providers, this will also facilitate the sharing of diagnostic tests.
For decades, dentists and their auxiliary staff have been involved in modifying lifestyle habits in patients regarding smoking cessation and reinforcing measures to improve poor oral hygiene, both of which are strong risk factors for the development of chronic periodontitis. With additional training, these dental care providers could definitely join the medical workforce in guiding patients, working with them to set goals to overcome social and environmental barriers, and rendering self-management training9 to help patients attain glycemic control.
Obesity is a major epidemic that is intricately and independently associated with diabetes and periodontitis. It is expected that more obese patients with periodontitis will be visiting dental offices in the near future. Pediatric dentists already check on the nutritional/dietary habits of their patients to assess the risk for developing caries. Therefore, dentists and their staff could also play an important role in helping patients modify their dietary and lifestyle habits to improve their overall well-being.
Potential Role of Medical HCPs
In a recent article, Lalla and Lamster9 suggested that the medical community can be involved in the following ways to enhance early detection and treatment of periodontal diseases in patients with diabetes: 1) by discussing with patients the importance of oral health and its relationship to diabetes; 2) by advising patients with poorly controlled diabetes to see a dentist on a regular basis; 3) by immediately referring to a dentist patients with diabetes who report that they have not seen a dentist in the past year, as well as those who have seen a dentist in the past year but present with detectable signs or symptoms of oral infections; 4) by screening for oral/periodontal changes similar to screening for other complications, asking about symptoms and performing a simple visual assessment of the mouth; and 5) by facilitating communication with the treating dentist by offering information about patients’ medical background and being available to offer advice on medical management modifications that may be necessary. With additional HCP training about the oral-systemic connections between diabetes and periodontal disease and about how to perform a basic periodontal examination, these goals are attainable.
A recent systematic review32 clearly pointed out that, by asking patients the right questions or by using a validated questionnaire, periodontal status can be accurately ascertained. Questions about whether a patient has had periodontal or gum disease or has ever had periodontal or gum surgery in the past were shown to have adequate sensitivity and specificity to detect periodontal disease.32 Recent studies using emergency department (ED) databases point to the rising number of ED visits by patients for dental ailments, including chronic periodontitis, further justifying the need for additional training about dental conditions for the medical health care team.33
In summary, with the projected rise in chronic diseases, including diabetes, and the growing shortage of primary care physicians, it is ever more important for dental and medical HCPs to work together closely to tackle this public health crisis. The nature of dental treatment protocols in the United States and the systemic link between dental conditions such as periodontitis and diabetes will allow for fruitful bidirectional collaboration between the medical and dental care workforce. Cross-training and interprofessional education are becoming increasingly important to accomplish these collaborative tasks.
REFERENCES
- 1.American Academy of Family Physicians : Primary care. Available from http://www.aafp.org/about/policies/all/primary-care.html#1. Accessed 10 October 2013
- 2.McCarthy M: U.S. production of new primary care doctors falls far short of need, study finds. BMJ 346:f4018, 2013. (doi: 10.1136/bmj.f4018) [DOI] [PubMed] [Google Scholar]
- 3.Ferris AH, McAndrew TM, Shearer D, Donnelly GF, Miller HA: Embracing the convenient care concept. Postgrad Med 122:7–9, 2010 [DOI] [PubMed] [Google Scholar]
- 4.Vogeli C, Shields AE, Lee TA, Gibson TB, Marder WD, Weiss KB, Blumenthal D: Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med 22 (Suppl. 3):391–395, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheldon GF, Ricketts TC, Charles A, King J, Fraher EP, Meyer A: The global health workforce shortage: role of surgeons and other providers. Adv Surg 42:63–85, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Lamster IB, Eaves K: A model for dental practice in the 21st century. Am J Public Health 101:1825–1830, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giddon DB, Swann B, Donoff RB, Hertzman-Miller R: Dentists as oral physicians: the overlooked primary health care resource. J Prim Prev 34:279–291, 2013 [DOI] [PubMed] [Google Scholar]
- 8.Lamster IB, Wolf DL: Primary health care assessment and intervention in the dental office. J Periodontol 79:1825–1832, 2008 [DOI] [PubMed] [Google Scholar]
- 9.Lalla E, Lamster IB: Assessment and management of patients with diabetes mellitus in the dental office. Dent Clin North Am 56:819–829, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ, Beck J, Douglass G, Page R: Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res 91:914–920, 2012 [DOI] [PubMed] [Google Scholar]
- 11.Williams RC: Periodontal disease. N Engl J Med 322:373–382, 1990 [DOI] [PubMed] [Google Scholar]
- 12.Preshaw PM, Alba AL, Herrera D, Jepsen S, Konstantinidis A, Makrilakis K, Taylor R: Periodontitis and diabetes: a two-way relationship. Diabetologia 55:21–31, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Maskari AY, Al-Maskari MY, Al-Sudairy S: Oral manifestations and complications of diabetes mellitus: a review. Sultan Qaboos Univ Med J 11:179–186, 2011 [PMC free article] [PubMed] [Google Scholar]
- 14.Stabholz A, Soskolne WA, Shapira L: Genetic and environmental risk factors for chronic periodontitis and aggressive periodontitis. Periodontol 2000 53:138–153, 2010 [DOI] [PubMed] [Google Scholar]
- 15.Tsai C, Hayes C, Taylor GW: Glycemic control of type 2 diabetes and severe periodontal disease in the U.S. adult population. Community Dent Oral Epidemiol 30:182–192, 2002 [DOI] [PubMed] [Google Scholar]
- 16.Sgolastra F, Severino M, Pietropaoli D, Gatto R, Monaco A: Effectiveness of periodontal treatment to improve metabolic control in patients with chronic periodontitis and type 2 diabetes: a meta-analysis of randomized clinical trials. J Periodontol 84:958–973, 2013 [DOI] [PubMed] [Google Scholar]
- 17.Ahmed N: Advanced glycation endproducts: role in pathology of diabetic complications. Diabetes Res Clin Pract 67:3–21, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Mealey BL, Ocampo GL: Diabetes mellitus and periodontal disease. Periodontol 2000 44:127–153, 2007 [DOI] [PubMed] [Google Scholar]
- 19.Suvan J, D’Aiuto F, Moles DR, Petrie A, Donos N: Association between overweight/obesity and periodontitis in adults: a systematic review. Obes Rev 12:e381–e404, 2011 [DOI] [PubMed] [Google Scholar]
- 20.D’Aiuto F, Suvan J: Obesity, inflammation, and oral infections: are microRNAs the missing link? J Dent Res 91:5–7, 2012 [DOI] [PubMed] [Google Scholar]
- 21.International Diabetes Foundation Diabetes Atlas. 6th ed. Available from http://www.idf.org/diabetesatlas/5e/the-global-burden. Accessed 10 October 2013
- 22.Centers for Disease Control and Prevention : National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2010. Atlanta, Ga, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011 [Google Scholar]
- 23.Centers for Disease Control and Prevention: National diabetes fact sheet , 2011 Available from http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed 10 November 2013 [Google Scholar]
- 24.U.S. Department of Health and Human Services: Healthy People 2020: Diabetes Available from http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=8. Accessed 10 October 2013.
- 25.Centers for Disease Control and Prevention : National Center for Health Statistics data, table 98. Available from http://www.cdc.gov/nchs/data/hus/2011/098.pdf. Accessed 25 November 2013
- 26.Centers for Disease Control and Prevention : National Center for Health Statistics data, table 97. Available from http://www.cdc.gov/nchs/data/hus/2011/097.pdf. Accessed 25 November 2013
- 27.Dye BA, Genco RJ: Tooth loss, pocket depth, and HbA1c information collected in a dental care setting may improve the identification of undiagnosed diabetes. J Evid Based Dent Pract 12 (3 Suppl.):12–14, 2012 [DOI] [PubMed] [Google Scholar]
- 28.Barasch A, Safford MM, Qvist V, Palmore R, Gesko D, Gilbert GH; Dental Practice-Based Research Network Collaborative Group: Random blood glucose testing in dental practice: a community-based feasibility study from The Dental Practice-Based Research Network. J Am Dent Assoc 143:262–269, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Formicola AJ, Redding S, Mito RS: A national system to support a mandated PGY-1 year: how to get there from here. J Dent Educ 65:221, 2001 [PubMed] [Google Scholar]
- 30.Genco RJ, Schifferle RE, Dunford RG, Falkner KL, Hsu WC, Balukjian J: Screening for diabetes mellitus in dental practices: a field trial. J Am Dent Assoc 145:57–64, 2014 [DOI] [PubMed] [Google Scholar]
- 31.Franck SD, Stolberg RL, Bilich LA, Payne LE: Point-of-care HbA1c screening predicts diabetic status of dental patients. J Dent Hyg 88:42–52, 2014 [PubMed] [Google Scholar]
- 32.Blicher B, Joshipura K, Eke P: Validation of self-reported periodontal disease: a systematic review. J Dent Res 84:881–890, 2005 [DOI] [PubMed] [Google Scholar]
- 33.Elangovan S, Nalliah R, Allareddy V, Karimbux NY: Outcomes in patients visiting hospital emergency departments in the United States because of periodontal conditions. J Periodontol 82:809–819, 2011 [DOI] [PubMed] [Google Scholar]