Abstract
In Brief
Postpartum follow-up for patients with gestational diabetes mellitus (GDM) is essential to manage future disease risk. In a diverse, urban population of GDM patients at a major medical center, high fasting glucose, high BMI at diagnosis, and low education level were associated with not following up in the endocrinology clinic after delivery; patients least likely to follow up are, therefore, also at greatest risk of GDM complications. Although race/ethnicity was not a significant predictor of follow-up, Hispanic/Latina and African-American patients were more likely to have risk factors for postpartum clinical attrition.
In the context of increasing prevalence of metabolic syndrome, risk of decreased insulin sensitivity is becoming more widespread among women of reproductive age.1 Pregnancy results in a series of metabolic changes that serve to optimize fetal growth conditions; however, these changes can also result in the development of diabetes in women with predisposing risk factors.2 One study3 identified an increase in the percentage of pregnancies complicated by gestational diabetes mellitus (GDM) from 2.9% in 1999 to 3.6% in 2006 (P < 0.01). Another study4 found an increase in GDM prevalence from 1.9% in 1989–1990 to 4.2% in 2003–2004. Overall, the prevalence of GDM is estimated to have increased by 10–100% in the past 20 years among several racial/ethnic groups.5 In 2010, the International Association of Diabetes in Pregnancy Study Groups established new criteria for GDM diagnosis, which, if adopted, would increase the number of cases to 18% of all pregnancies.6
GDM is associated with a host of complications, including preeclampsia, polyhydramnios, fetal macrosomia, fetal organomegaly, birth trauma, operative delivery, and neonatal respiratory and metabolic complications or death.7 Tight glycemic control decreases the risks of spontaneous abortion and congenital malformations, which are twice as likely to occur in the setting of maternal diabetes.8 Infants who survive a birth complicated by GDM may be at increased risk of childhood obesity and diabetes, impaired motor function, and higher rates of inattention and/or hyperactivity.9,10 These conditions compromise the child’s cognitive and physical development. For mothers, there is a rapid increase in the risk of type 2 diabetes during the first 5 years after delivery.11 The risk of overt diabetes immediately after pregnancy is 10%.12 Women with a history of GDM remain at an increased long-term risk of developing type 2 diabetes compared to their counterparts with no GDM history (risk ratio 7.43).13 They also have a higher likelihood of developing GDM in a subsequent pregnancy.
Several risk factors mediate postpartum type 2 diabetes risk among women with a history of GDM. These include elevated fasting blood glucose (FBG) in a diagnostic glucose tolerance test (GTT) during pregnancy; FBG > 121 mg/dl is associated with a 21-fold risk.4,14,15 High BMI at the time of diagnosis is also positively correlated with postpartum risk of type 2 diabetes.8,16 One study17 found that African-American women with GDM and, secondarily, Hispanic/Latina women are at the highest risk of developing postpartum type 2 diabetes compared to Asian/Pacific Islander and non-Hispanic/non-Latina women. This disparity was only partially decreased after accounting for BMI. In another study of Hispanic/Latina women with GDM,18 80% of women developed type 2 diabetes within 5 years of delivery. Physiological and demographic factors, therefore, mediate postpartum type 2 diabetes risk.
Given its potential for long-term sequelae, GDM is a disease that requires close clinical follow-up at least every 3 years, beginning with a postpartum GTT within 6–12 weeks of delivery.19 Follow-up allows for diagnosis and appropriate treatment of patients who develop diabetes early in the postpartum period. Timely diagnosis also serves as secondary prevention of long-term complications associated with diabetes, and early postpartum follow-up is crucial for establishing or maintaining lifestyle changes that decrease the risk of type 2 diabetes later in life or delay its onset. Tight glycemic control is also crucial for the health of future pregnancies. Spontaneous abortions in the first semester are more common in pregnancies complicated by diabetes.8 Maternal diabetes increases the risk of congenital malformations, most notably cardiac anomalies and neural tube defects.20 This risk remains elevated for mothers with diabetes even when glycemic control is good.
Given the importance of close postpartum follow-up of patients with GDM, identification of those most at risk of attrition is a significant clinical question. In one study,21 negative predictors of postpartum follow-up included obesity and higher parity. On the other hand, older age, Asian or Hispanic/Latina ethnicity, greater contact with medical providers, and higher education were identified as predictors of postpartum follow-up. In another study,22 older age, nulliparity, and higher income or education were positive predictors of completing GTT screening. Women who fail to follow up for postpartum care often have more severe GDM and a higher prepregnancy weight than those who do, suggesting that underlying causes of clinical attrition may be associated with risk factors for postpartum type 2 diabetes.23 A report on postpartum GTT screening from the Translating Research Into Action for Diabetes study21 found that the rate of postpartum screening has increased since the mid-1990s, but as of 2006, it is still only 53.8%.
GDM has rapidly increased in incidence in recent years, in keeping with the global upward trend of obesity, type 2 diabetes, and other metabolic diseases. Type 2 diabetes is an important sequela of GDM, and close postpartum follow-up is key to preventing or treating this disease in a timely manner. This study adds to the literature describing characteristics of patients least likely to follow up for a postpartum clinic visit. The results may serve as a starting point for targeted interventions aimed at patients at high risk of postpartum attrition and subsequent preventable morbidity after an episode of GDM.
Methods
We conducted a retrospective chart review of 373 postpartum GDM patients seen at a major academic medical center between January 2010 and November 2012. Institutional review board approval was obtained before data collection began. Variables of interest included race/ethnicity, level of formal education, income, age, history of GDM or delivery of a large-for-gestational-age baby, BMI at diagnosis, gestational age at diagnosis, type of treatment received, infant birth weight, pre- and postpartum GTT results, and follow-up at a postpartum visit within 4 months of delivery.
Means and standard deviations were calculated to summarize continuous variables; counts and percentages were calculated to summarize categorical variables. The comparisons between groups were performed with the use of Kruskal-Wallis or Wilcoxon rank-sum tests for continuous variables and Pearson’s χ2 test for categorical variables. A logistic regression model was also fit to assess the association between keeping a follow-up visit appointment and prespecified confounding variables.
Results
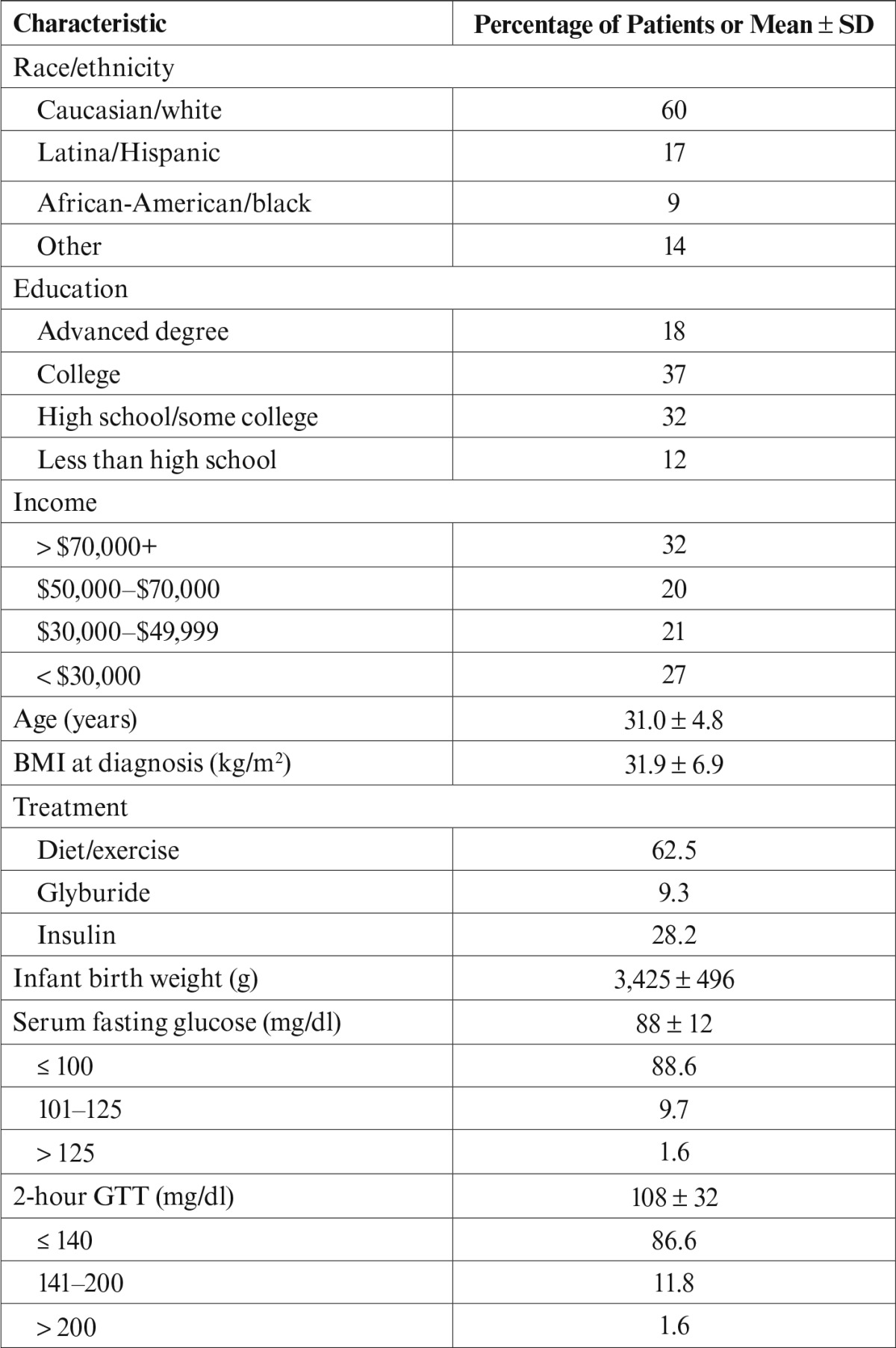
The mean age was 31.0 years (n = 373). Sixty percent of patients were identified as Caucasian/white, 17% as Hispanic/Latina, 9% as African-American/black, and 14% as other backgrounds, including Asian, Middle Eastern, and African. The majority of patients received only diet and exercise counseling for treatment; the next most common form of treatment was insulin therapy, followed by glyburide. Other demographic characteristics of patients can be found in Table 1.
Table 1.
Demographics (n = 373)
Descriptive statistics and analysis of variance were used to identify characteristics of patients who did not attend their postpartum follow-up appointment in the endocrinology clinic. The overall follow-up rate was 50%. Patients with less than a high school education were significantly less likely to complete a follow-up visit (defined as a return to the endocrinology clinic within 4 months of delivery for the purposes of GDM follow-up) than patients with an advanced degree (odds ratio [OR] 4.36, 95% CI 1.42–13.41). Furthermore, education level was inversely correlated with fasting glucose at time of diagnosis, which is a significant predictor of postpartum diabetes risk. The OR of having a higher fasting glucose for a patient with a high school education versus an advanced degree was 2.77 (95% CI 1.09–7.00).
Average BMI at diagnosis was 31.7 kg/m2 among patients who did not follow up and 29.9 kg/m2 among those who did follow up (P = 0.01); patients with a higher BMI were less likely to keep their follow-up visits (OR 0.69). Of note, a prepregnancy BMI > 30 kg/m2 is associated with an increased risk of postpartum diabetes among women with GDM.12 These data suggest that a lower level of formal education and higher BMI at diagnosis are associated with a decreased likelihood of completing a follow-up visit. Incidentally, patients with lower levels of education have higher fasting glucose levels at diagnosis. Both higher fasting glucose and higher prepregnancy BMI are linked to greater postpartum diabetes risk, suggesting that GDM patients least likely to follow up are also the patients at the highest risk for postpartum type 2 diabetes.
Although race/ethnicity was not independently associated with postpartum follow-up, associations between racial/ethnic categories and the observed risk factors existed. Average BMI at diagnosis was 33.3 kg/m2 for Hispanic/Latina and African-American patients and 31.0 kg/m2 for Caucasian patients (P < 0.001). Nearly 20% of Caucasian patients had an advanced degree compared to 12.9% of African-American patients and 1.8% of Hispanic/Latina patients (P < 0.001). Therefore, Hispanic/Latina and, to a lesser extent, African-American patients may be more likely to have risk factors for not following up in populations similar to the one in this study.
Discussion
Postpartum follow-up for GDM patients is essential to identify and treat those who develop diabetes early in the postpartum period. Early diagnosis and treatment serve as secondary prevention of long-term complications associated with diabetes. Follow-up is also crucial for establishing or maintaining lifestyle changes that decrease type 2 diabetes risk.
This retrospective chart review demonstrated that the patients least likely to follow up were those with lower levels of formal education (less than a high school degree). These patients were at the highest risk of developing postpartum type 2 diabetes given that they also had higher BMIs and fasting glucose levels at diagnosis. Although race was not independently associated with postpartum follow-up, Hispanic/Latina and, secondarily, African-American patients had higher BMIs and lower levels of education than Caucasian patients in this population. Other studies have found that African-American and Hispanic/Latina women with a history of GDM are at higher risk of postpartum type 2 diabetes, which highlights the intersection of demographic and physiological risk factors for both clinical attrition and later morbidity.15,24
These findings could serve as a starting point for targeted intensive postpartum outreach. Primary care providers (PCPs) and obstetricians may play an important role in identifying women at high risk of GDM in the preconception and early prenatal periods. Lifestyle changes to encourage weight loss and prevent hyperglycemia in early pregnancy may be particularly important for this population. A systematic review of interventions to increase postpartum testing rates among GDM patients found that proactive programs featuring reminders to both patients and their PCPs, as well as patient tracking systems, were the most effective.25
Because women interact with pediatricians frequently during the months after delivery, pediatricians may be another important provider group to engage. Just as they administer postpartum depression screenings, pediatricians could administer maternal and child chronic disease risk screenings and recommend appropriate clinical and community resources to promote healthy lifestyles. Maternal lifestyle risk factors may directly affect child health; a study of Hispanic/Latino families26 found that parental physical activity was strongly correlated with toddler physical activity. Pediatricians may be ideal providers to promote family health, particularly in the first 5 years of a child’s life, when maternal risk of conversion to type 2 diabetes after GDM is highest and excessive infant weight gain is particularly deleterious.11,27 This study identifies opportunities to target patients with lower levels of formal education, higher fasting glucose levels, and BMIs > 30 kg/m2 for more intensive efforts at ensuring follow-up. Collaborative clinical efforts to engage this subgroup may be particularly effective in terms of morbidity prevention.
Prevention is also important for reducing health care costs. One study28 found that pregnancies complicated by GDM were associated with costs of care 34% greater than for uncomplicated pregnancies; women with GDM had significantly higher rates of emergency caesarean section, and their infants were more likely to require neonatal intensive care. After delivery, women with GDM face an increased risk of developing diabetes and contributing to the $245 billion spent annually on diabetes care in the United States.29 In a setting of increased health care costs, preventive measures to reduce both perinatal complications and long-term disease morbidity are crucial. Prevention includes systemic solutions to social determinants of health. Our findings demonstrate that minority women, in particular Hispanic/Latina and African-American patients, are more likely to have higher BMIs and lower levels of formal education, factors associated with a higher likelihood of postpartum clinical attrition. Decreasing disparities in GDM care, therefore, also involves preventive efforts and advocacy outside the clinical setting.
Limitations of this study include its descriptive nature and the limited number of cases (n = 373). With a larger cohort, the racial/ethnic category of “other” could be further stratified into discrete categories, providing more information by race/ethnicity. A prospective study would provide opportunities to explore trends in the development of postpartum type 2 diabetes, perinatal complications, or other sequelae. Directions for future research may include exploring barriers to postpartum follow-up among patients who fail to return to the clinic after delivery. Such research could inform the development of effective interventions to increase postpartum follow-up rates among patients identified as being at high risk in this population. GDM is an increasingly important problem related to the recent rise in obesity. Its potential to affect long-term individual, as well as intergenerational, health calls for expanded research efforts to elucidate persistent gaps and disparities in treatments and outcomes.
ACKNOWLEDGMENTS
The authors acknowledge the assistance of Elaine Boswell King, MSN, APRN, FNP-BC, CDE, of the Vanderbilt Center for Advanced Practice Nursing and Allied Health and Mario Davidson, PhD, of the Vanderbilt Biostatistics Department.
REFERENCES
- 1.Mozumdar A, Liguori G: Persistent increase in prevalence of metabolic syndrome among U.S. adults: NHANES III to NHANES 1999–2006. Diabetes Care 34:216–219, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Butte NF: Carbohydrate and lipid metabolism in pregnancy: normal compared with gestational diabetes mellitus. Am J Clin Nutr 71 (5 Suppl.):1256S–1261S, 2000 [DOI] [PubMed] [Google Scholar]
- 3.Dietz PM, Vesco KK, Callaghan WM, Bachman DJ, Bruce FC, Berg CJ, England LJ, Hornbrook MC: Postpartum screening for diabetes after a gestational diabetes mellitus-affected pregnancy. Obst Gynaecol 112:868–874, 2008 [DOI] [PubMed] [Google Scholar]
- 4.Getahun D, Nath C, Ananth CV, Chavez MR, Smulian JC: Gestational diabetes in the United States: temporal trends 1989 through 2004. Am J Obstet Gynecol 198:525.e1–525.e5, 2008 [DOI] [PubMed] [Google Scholar]
- 5.Ferrara A: Increasing prevalence of gestational diabetes mellitus. Diabetes Care 30 (Suppl. 2):S141–S146, 2007 [DOI] [PubMed] [Google Scholar]
- 6.Moses RG: New consensus criteria for diagnosis of GDM: problem solved or Pandora’s box? Diabetes Care 33:690–691, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dodd JM, Crowther CA, Antoniou G, Baghurst P, Robinson JS: Screening for gestational diabetes: the effect of varying blood glucose definitions in the prediction of adverse maternal and infant health outcomes. Obstet Gynaecol 47:307–312, 2007 [DOI] [PubMed] [Google Scholar]
- 8.Greene MF: Spontaneous abortions and major malformations in women with diabetes mellitus. Semin Reprod Endocrinol 17:127–136, 1999 [DOI] [PubMed] [Google Scholar]
- 9.Hillier TA, Pedula KL, Schmidt MM, Mullen JA, Charles MA, Pettitt DJ: Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia. Diabetes Care 30:2287–2292, 2007 [DOI] [PubMed] [Google Scholar]
- 10.Ornoy A: Growth and neurodevelopmental outcome of children born to mothers with pregestational and gestational diabetes. Pediatr Endocrinol Rev 3:104–113, 2005 [PubMed] [Google Scholar]
- 11.Kim C, Newton KM, Knopp RH: Gestational diabetes and the incidence of type 2 diabetes. Diabetes Care 25:1862–1868, 2002 [DOI] [PubMed] [Google Scholar]
- 12.Buchanan TA, Xiang AH: Gestational diabetes mellitus. J Clin Invest 115:485–491, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bellamy L, Casas JP, Hingorani AD, Williams D: Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 373:1773–1779, 2009 [DOI] [PubMed] [Google Scholar]
- 14.Ratner RE: Prevention of type 2 diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab 93:4774–4779, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nicholson WK, Wilson LM, Witkop CT, Baptiste-Roberts K, Bennett WL, Bolen S, Barone BB, Golden SH, Gary TL, Neale DM, Bass EB: Therapeutic management, delivery, and postpartum risk assessment and screening in gestational diabetes. Evidence Reports Technology Assessments, No. 162. Rockville, Md, Agency for Healthcare Research and Quality, 2008. Available from: http://www.ncbi.nlm.nih.gov/books/NBK27011. Accessed 4 August 2014 [PMC free article] [PubMed] [Google Scholar]
- 16.Löbner K, Knopff A, Baumgarten A, Mollenhauer U, Marienfeld S, Garrido-Franco M, Bonifacio E, Ziegler AG: Predictors of postpartum diabetes in women with gestational diabetes mellitus. Diabetes 55:792–797, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Xiang AH, Li BH, Black MH, Sacks DA, Buchanan TA, Jacobsen SJ, Lawrence JM: Racial and ethnic disparities in diabetes risk after gestational diabetes mellitus. Diabetologia 54:3016–3021, 2011 [DOI] [PubMed] [Google Scholar]
- 18.Kjos SL, Peters RK, Xiang A, Henry OA, Montoro M, Buchanan TA: Predicting future diabetes in Latino women with gestational diabetes mellitus: utility of early postpartum glucose tolerance testing. Diabetes 44:586–591, 1995 [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association: Standards of medical care in diabetes—2014. Diabetes Care 37 (Suppl.1):S14–S80, 2014 [DOI] [PubMed] [Google Scholar]
- 20.Macintosh MC, Fleming KM, Baron JA, Doyle P, Modder J, Acolet D, Golightly S, Miller A: Perinatal mortality and congenital anomalies in babies of women with type 1 or type 2 diabetes in England, Wales, and Northern Ireland: population based study. BMJ 333:177–182, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferrara A, Peng T, Kim C: Trends in postpartum screening and subsequent diabetes and impaired fasting glucose among women with histories of gestational diabetes mellitus. Diabetes Care 32:269–274, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tovar A, Chasan-Taber L, Eggleston E, Oken E: Postpartum screening for diabetes among women with a history of gestational diabetes mellitus. Prev Chronic Dis 8:A124, 2011 [PMC free article] [PubMed] [Google Scholar]
- 23.Hunt KJ, Conway DL: Who returns for postpartum glucose screening following gestational diabetes mellitus? Am J Obstet Gyn 198:404.e1–404.e6, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y, Chen L, Horswell R, Xiao K, Besse J, Johnson J, Ryan DH, Hu G: Racial differences in the association between gestational diabetes mellitus and risk of type 2 diabetes. J Women’s Health 21:628–633, 2012 [DOI] [PubMed] [Google Scholar]
- 25.Carson MP, Frank MI, Keely E: Postpartum testing rates among women with gestational diabetes: systematic review. Prim Care Diabetes 7:177–186, 2013 [DOI] [PubMed] [Google Scholar]
- 26.Ruiz R, Gesell SB, Buchowski MS, Lambert W, Barkin SL: The relationship between Hispanic parents and their preschool-aged children’s physical activity. Pediatrics 127:888–895, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leunissen RW, Kerkhof GF, Stijnen T, Hokken-Koelega A: Timing and tempo of first-year rapid growth in relation to cardiovascular and metabolic risk profile in early adulthood. JAMA 301:2234–2242, 2009 [DOI] [PubMed] [Google Scholar]
- 28.Gillespie P, Cullinan J, O’Neill C, Dunne F; ATLANTIC DIP Collaborators: Modeling the independent effects of gestational diabetes mellitus on maternity care and costs. Diabetes Care 36:1111–1116, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Diabetes Association : Economic costs of diabetes in the U.S. in 2012. Diabetes Care 36:1033–1046, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]


