Abstract
Frail elderly patients with advanced kidney disease experience many of the burdens associated with dialysis. Although these patients constitute the fastest-growing population starting dialysis, they often suffer loss of functional status, impaired quality of life, and increased mortality after dialysis initiation. Nephrology clinicians face the challenges of helping patients decide if the potential benefits of dialysis outweigh the risks and preparing such patients for future setbacks. A communication framework for dialysis decision-making that aligns treatment choices with patient goals and values is presented. The role of uncertainty is highlighted, and the concept of a goal-directed care plan is introduced. This plan incorporates a time-limited trial that promotes frequent opportunities for reassessment. Using the communication skills presented, the clinician can prepare and guide patients for the dialysis trajectory as it unfolds.
Keywords: CKD, children, pediatric nephrology
Introduction
Gerald is a 78-year-old man with slowly-progressive stage 4 CKD caused by hypertension and diabetes mellitus. Over the past year, he sustained an acute myocardial infarction and subsequently developed systolic congestive heart failure. After a long hospitalization and rehabilitation stay, Gerald moved into assisted living. He has dyspnea on exertion. At his last visit, he and his nephrologist discussed the news that his kidney disease has worsened to the point that dialysis options should be considered. The goal of this visit is to discuss treatment options and whether dialysis is what Gerald would want when the need arises. In the past, Gerald has stated that he would want dialysis if it could enable him to spend more time with his grandchildren.
Gerald's case highlights the challenge that nephrology clinicians encounter in the care of frail elderly patients with kidney disease: how to discuss treatment options with an individual who may not do well on dialysis. Elderly patients, defined as those ≥75 years, constitute one of the fastest-growing age groups initiating dialysis (1). Frailty is a clinical phenotype that encompasses medical complexity and functional limitations. Its presence has been associated with poor outcomes in the elderly patients with kidney disease (2,3). Frail elderly patients often experience burdens associated with dialysis, such as decrements in quality of life, loss of functional status, and increased risk for hospitalizations and institutionalized care (4–6). In the setting of marked frailty and advanced comorbidities, dialysis may not confer survival benefit and may be associated with more harm (7,8). Clinicians are tasked with helping patients decide if the potential benefits of dialysis outweigh these risks.
Discussions about dialysis decision-making can be stressful. These discussions are often perceived as time-consuming and may arouse strong emotions. Also, uncertainty exists about how well a patient will tolerate and respond to dialysis. This uncertainty may serve as a barrier to discussions that prepare patients for the potential burdens and functional losses that accompany dialysis (9). As a consequence, patients miss the opportunity for timely discussions of prognosis and advance care planning for when things do not go well.
Although dialysis withdrawal is a leading cause of death in patients on dialysis, many patients have not engaged in discussions about end-of-life or completed advance care directives (10–12). As a result, these vital conversations occur too late and are frequently left to loved ones, who may be unsure what the patient would want (13). Such patients are more likely to die in the hospital and less likely to receive timely hospice services compared with patients with other life-limiting illnesses (14,15). Early discussions of prognosis and end-of-life can lead to less intensive care at the end of life and care consistent with patient preferences (16,17).
We address two tasks for the clinician caring for frail elderly patients facing dialysis decisions: how to help patients decide if the potential benefits of dialysis outweigh the risks, and how to prepare patients who elect dialysis for potential future setbacks. We outline a patient-centered communication framework called SPIRES (setup, perceptions and perspectives, invitation, recommendation, empathize, summarize and strategize), adapted from a previously described approach for delivering bad news (SPIKES–setup, perceptions, invitation, knowledge, empathize, summarize and strategize) (18), to guide clinicians in these discussions of dialysis decision making. We further define the concept of a goal-directed care plan that incorporates patient values into defined milestones (i.e., patient goals) and pause points (i.e., undesirable outcomes and burdens).
Consideration of Treatment Paths for Patients Who May Do Poorly
For frail elderly patients, one must consider not only survival on dialysis but also, quality of life on dialysis. Although dialysis may extend life for most patients, significant burdens may accompany this additional time, thus diminishing quality of life. An understanding of both the burdens and benefits of dialysis takes into account not just if the patient will survive on dialysis but how the patient will live while undergoing dialysis (Table 1).
Table 1.
Potential benefits and burdens of dialysis for frail elderly patients
| Potential Benefits of Dialysis | Potential Burdens of Dialysis |
|---|---|
| Life extension | Procedures for access: access placement, fistulograms/stent placement, access failure, and access complications/steal syndrome |
| Symptom relief: fatigue/weight loss, loss of appetite, and sleep disturbance | Time spent undergoing dialysis: three times per week treatment for standard in-center hemodialysis and time spent traveling to and from dialysis |
| Improved quality of life: ability to do the activities that bring a patient joy and fulfillment | Increased hospitalizations and setbacks: acute illness, functional decline, and transition to skilled nursing facility |
| Social aspects of dialysis: supportive environment of the dialysis unit and support from fellow dialysis patients | Symptoms related to dialysis itself or its complications: cramping, postdialysis fatigue, pain/ischemia related to access, and bone mineral disease/calciphylaxis |
Data suggest that patients often have preferences for how they live and the kinds of treatments that they are willing to undergo for a given goal (19–21). By learning the specific preferences and goals of a given patient, the clinician has a better idea of which treatment path may be most appropriate for that individual. These treatment paths for dialysis decision making are summarized below.
Dialysis Path with a Focus on Extending Life
Patients who elect the dialysis path typically hope for improved survival in anticipation of attaining specific personal goals. The potential benefit of extended survival, however, is often associated with increased exposure to the health care system. This added exposure involves the time to undergo dialysis and also, the medical procedures associated with dialysis access (22). These patients are also at risk for common complications of dialysis, such as hospitalizations for infections and acute illness, rehabilitation stays for functional declines, and clinical setbacks from coexisting illnesses. Most elderly patients (approximately 95%) choose hemodialysis as the dialysis modality (1). For patients who elect the dialysis path, the clinician can propose a time-limited trial to reassess whether patient goals have been met (see below).
Supportive Care (Nondialysis) Path with a Focus on Quality of Life
Patients who choose supportive care focus on quality of life, despite the possibility for a shorter lifespan. Treatment involves management of the disease and its symptoms but excludes dialysis. Care is focused on symptom management and the medical issues associated with advanced CKD. Patients who choose this path typically wish to avoid intensive medical treatments and hospitalizations as health declines (23). Patients who choose this path would benefit from early referral to palliative care and hospice services.
SPIRES: Patient-Centered Communication Framework for Dialysis Decision-Making
A patient-centered framework for dialysis decision-making focuses on eliciting the goals and values of the patient (Table 2). SPIRES is a step-wise communication framework to assist the clinician in treatment decision-making for patients who may not do well with dialysis. By learning about the patient as a person, the clinician gains a sense of whether a patient’s goals are consistent with a treatment path focused on quality or quantity. If dialysis is chosen, the clinician can then incorporate these goals into a care plan. These goals will then serve as meaningful milestones to be assessed as the course unfolds.
Table 2.
SPIRES: a patient-centered framework for dialysis decision making
| SPIRES | Components | Communication Examples |
|---|---|---|
| Setup | Prepare: relevant prognostic information, consulting other physicians; describe the decision that is to be made; include relevant participants | “For some patients who are older and have other medical issues, dialysis can be associated with more side effects and burdens than benefits. To better understand if dialysis is right for you, I’d like to learn more about you as a person and what is important to you. Is that alright with you?” |
| Perceptions and perspectives (explore what the patient hopes dialysis will achieve and the kinds of concerns that they hope to avoid) | Understanding of dialysis; hopes (hoping for the best); concerns (preparing for the worst) | “What have you heard about dialysis?” (if have not had options training yet or if conversation occurred long ago). “Do you have any questions about dialysis since we last spoke?” “What is life like for you now?” “What activities bring you pleasure and enjoyment?” “As you think about your future, what are you hoping for?” “What is most important to you at this point in your life?” “What worries you as you think about the future?” “What concerns do you have about being on dialysis?” “Are you able to think of situations in which you might not want to continue dialysis?” |
| Invitation | Invite a recommendation | “From what you have said, it sounds like you hope that dialysis will help you ___. Would you like my recommendation?” |
| Recommendation | Disclose relevant prognostic information; recommendation: hope for the best and prepare for the worst | “Patients who have been in your situation sometimes experience more of the side effects of dialysis than benefits…When a patient has other medical conditions, dialysis may not significantly extend survival.” or “Based on your goals, I would recommend that we start dialysis with the hope that you are able to __. I also want to talk about the situation if dialysis does not achieve these goals or becomes too burdensome.” |
| Empathize (discussions of the future/uncertainty can cause strong emotions) | NURSE | “I can see that this is a difficult conversation.” “These conversations can be scary.” “I really appreciate that you’ve taken this decision seriously.” “I’ll stick with you throughout this.” “Tell me more about your worry.” |
| Summarize and strategize (outline the care plan that incorporates hopes and concerns into milestones and pause points to monitor over time) | Recap recommendation; check in with patient; outline a care plan that identifies what success looks like (milestones) and specific setbacks when dialysis as a treatment should be reassessed and potentially stopped (pause points); arrange a follow-up to check in; document discussion and communicate with relevant health providers | “Based on our discussion today, we will plan to prepare for dialysis and reassess things over time. Do you have any concerns about this recommendation?” “We will know dialysis is working for you if you are able to…” (name these milestones with patient). “Would it be alright to explore the situations when we should consider stopping dialysis?” “Previously, you had mentioned that you would not want to continue dialysis if …” (name prior concerns that will serve as pause points). “We will continue to meet and reassess on a regular basis whether dialysis is working for you.” |
SPIRES, setup, perceptions and perspectives, invitation, recommendation, empathize, summarize and strategize; NURSE, name, understand, respect (praise), support, and explore.
Setup: Preparing for the Conversation
Just as preparation is fundamental to the success of the procedures that we perform, preparing for a dialysis discussion is critical. To begin the process, the patient’s record should be reviewed for pertinent clinical and laboratory trends. This patient-specific information can then be considered in the context of evidence-based data regarding outcomes in comparable patients. Prognostic models, such as the Cohen 6-month mortality predictor, can identify patients who have a high risk of death on dialysis (24). This model combines four clinical variables with the surprise question (would I be surprised if this patient died in 6 months?) (25). In general, patients who are less likely to benefit from dialysis initiation include patients with marked frailty, patients in nursing homes, and elderly patients with certain comorbidities. For patients with significant comorbid illnesses (such as heart failure or cancer), seeking the input of the other physicians managing these conditions is warranted. By acquiring more information about the treatment plan and prognosis of these coexisting illnesses, the clinician has a better understanding of how likely dialysis will affect the patient’s overall clinical course.
The clinician initially extends an invitation to have the conversation: “Last visit, we discussed that your kidney function has worsened to the point that we need to talk about the next steps. Would it be alright if we did that today?” This question ensures that the patient does not feel forced to have the conversation and that both the patient and clinician are in agreement about the agenda. For such serious discussions, patients often prefer to have a loved one present for support or consultation. Therefore, the clinician should ask if the patient would like someone to be present for the discussion.
Perceptions and Perspectives: Understanding the Patient as a Person
Data suggest that treatment preferences in older seriously-ill patients depend on the expected outcomes with a given treatment. Patients will frequently elect to undergo a given treatment with the hope of achieving an anticipated outcome, despite the risk of certain burdens (19). For these patients, the accompanying risk is outweighed by the potential attainment of a certain outcome. These outcomes can vary depending on the individual and are influenced by a patient’s specific values. These values can be understood by asking open-ended questions that explore what the patient hopes to gain from the treatment. By assessing a patient’s concerns and worries, the clinician gains insight into how much burden the patient is willing to tolerate to achieve a designated goal or, conversely, what conditions the patient wishes to avoid in pursuit of a goal.
In some instances, it is helpful to frame the conversation by describing the two different treatment paths, dialysis or supportive care, very explicitly: “Some people want to live as long as possible and choose dialysis, which may entail frequent hospitalizations and less independence. Other people focus on the quality of their lives and decline dialysis knowing that this will likely limit their survival. Do you have a sense of how you feel about this matter?”
Understanding what a patient hopes to achieve with dialysis can provide meaningful goals that can be incorporated into the care plan. A patient’s response to questions that explore hopes allows the clinician insight into the goals that a patient wishes to achieve. Such hopes may include the ability to do or experience certain things and the activities that bring joy and fulfillment, as well as the ability and willingness to tolerate burdens in exchange for longevity. From this exploration, the clinician learns how a patient views his or her quality of life.
It is equally essential to elicit the patient’s worries and concerns. These include the conditions or health states that a person perceives as unacceptable or intolerable. For example, a frail elderly patient initiating dialysis has a high likelihood at some later time of requiring skilled nursing in a facility. Exploring whether living in such a state would be considered tolerable and consistent with a patient’s desired quality of life assists with making future care decisions.
The answers to questions regarding hopes and worries provide the clinician with a more expansive picture of the patient as a person (Table 2). After exploring these questions with Gerald, for example, the clinician learns that his primary goal is to spend time with his family and avoid future hospitalizations. He worries most about being a burden to his family, especially if he were in a more dependent state in which others would have to take care of him. These data assist the clinician as he or she formulates a treatment recommendation and care plan for Gerald. Gerald perceives dialysis to be a beneficial treatment path provided that he remains healthy enough to enjoy meaningful time with his family. If Gerald experiences marked decline in his functional status and becomes dependent, dialysis would no longer be considered beneficial by Gerald and ought to be reconsidered.
Sharing relevant prognostic information with the patient is an integral part of the decision-making conversation. Although tools exist to aid discussions about prognosis on dialysis, uncertainty about how a given patient’s course may unfold often causes the clinician to avoid such a discussion. Patients, however, want information about the future even when uncertainty exists and prefer that the physician offer it voluntarily (10,26). The clinician should ask the patient what type of information would be helpful to them (are you the type of person who wants specific details and statistics or would you prefer to know how others similar to you have fared?) (27,28). Importantly, prognostic conversations frequently evoke strong emotions (see below).
Invitation and Recommendation
The clinician is now ready to offer a recommendation for the treatment path that optimally accounts for both the patient’s specific goals and the clinical data. Before making this recommendation, it is helpful to extend an invitation to offer a recommendation: “Based on our conversation and my medical opinion, would you like my recommendation?” If the patient agrees, the clinician can proceed: “From what you have shared with me about your current quality of life and goals, I would recommend that we pursue preparation for dialysis. Here is why…” Here, the clinician can use the patient’s own goals and values to justify the recommendation.
Empathize: Importance of Emotion
Serious conversations, such as those pertaining to decisions about dialysis, “big picture” goals, and prognosis, evoke emotional responses in patients. It is essential for the clinician to anticipate and recognize these emotions as they arise. Such emotions may interfere with the patient’s ability to integrate necessary information (29). Paying attention to these emotions, whether they are expressed verbally or nonverbally, also enables the clinician to understand how the patient is dealing with the issues under discussion (30,31). A tool to help with responding to emotion is the acronym NURSE: naming the emotion, understanding the emotion, respecting the patient, supporting the patient, and exploring the emotion (32,33). Any one of these approaches allows the patient to feel they are heard, and cope with the information being given (Table 2).
Strategize: Time-Limited Trial of Dialysis
A goal-directed care plan views the initiation of dialysis as a time-limited trial, with continuation of the therapy dependent on attainment of meaningful goals and avoidance of the burdens of therapy (Table 3) (34). Time-limited trials are recommended when uncertainty exists as to how a patient may do on dialysis (35). However, less guidance exists as to how to conduct a time-limited trial and how long. The details and duration of a trial of dialysis will likely vary for a given patient. For a patient with AKI, a sufficient trial may be days to weeks depending on the clinical scenario. However, for a patient with progressive CKD, a sufficient trial to assess for success or failure may require weeks to months of dialysis. Each trial should include patient-specific goals and time courses. It begins with a discussion of what the treatment will be and why a time-limited trial of dialysis is being proposed. The clinician can share his or her own concerns about the kinds of burdens that may accompany dialysis (Table 1), further clarifying the reason for a goal-directed care plan that prepares for potential declines.
Table 3.
Six steps of a goal-directed care plan with time-limited trial of dialysis
| Step 1: include all relevant people in the plan: patient, family members, health care-appointed decision maker |
| Step 2: define the purpose of the time-limited trial: relevant prognostic information, discussion of the potential benefits and burdens of treatment |
| Step 3: discuss the milestones (specific goals that the patient hopes to achieve and those that they wish to avoid) |
| Step 4: discuss the pause points (specific setbacks or health conditions when dialysis as a treatment should be reassessed and potentially stopped) |
| Step 5: check for understanding and determine a meeting time to check in |
| Step 6: document steps 1–5 and notify relevant health care providers |
If dialysis is elected and a time-limited trial is suggested, the clinician reviews the articulated milestones that represent evidence of dialysis as a successful treatment and pause points that suggest that dialysis may be causing more unacceptable burden than benefit. The hopes and concerns elicited from the patient inform these particular milestones and pause points. Outlining these specific markers allows the clinician to convey to the patient that we hope for the best and prepare for the worst (36). In other words, the clinician acknowledges uncertainty and prepares the patient in the event that things do not go well.
Using Milestones and Pause Points to Define a Time-Limited Trial
Hope for the Best: Identifying Patient-Specific Milestones
The progress of a treatment, such as dialysis, is typically monitored with objective findings, such as laboratory values, nutritional status, and overall clinical condition. When discussing a treatment plan that encompasses patient-directed goals, progress should similarly be defined in terms of objective findings that are meaningful for the patient. They are specific goals that address what a patient hopes dialysis will accomplish. These milestones represent what success with dialysis would look like.
Clinician: “Earlier, you told me what you hoped to gain with dialysis and the things that you wished to avoid. Your main goal was to spend time with your family and be active enough to live outside of a skilled nursing facility. Do I have that right? Is there anything we should add?”
Gerald: “I think you have it right. Since my wife died, seeing my grandkids is my main source of happiness.”
Clinician: “From what you have told me, you have a couple of goals that you hope to achieve, one of which is to get a little stronger and remain independent enough to live at home. The ability to spend time with your family is what gives you great joy. Do I have that right?”
Gerald: “Yeah, that’s right.”
Prepare for the Worst: Identifying Patient-Specific Pause Points
Articulating the kinds of setbacks or health conditions for which a patient would not want to continue dialysis is as fundamental as outlining the goals that a patient hopes to achieve. These pause points are critical opportunities to reassess the treatment plan and determine if dialysis continues to provide benefit. For some patients, these pause points are when they become debilitated to the point that they require nursing home placement. For other patients, living in a nursing facility may be tolerable as long as they can spend meaningful time with the ones who they love. By naming these specific situations or health conditions in advance, the clinician and patient identify circumstances for which dialysis withdrawal and a shift toward comfort is reasonable and consistent with the patient's wishes. Pause points are also opportunities to assess for symptoms or burdens that may benefit from referral to services, such as palliative care for ongoing symptom management.
Clinician: “We spoke earlier about the things that you hoped that dialysis would achieve. Would it be ok to explore how things might change if you couldn’t achieve these goals?”
Gerald: “I guess that would be a good idea.”
Clinician: “You mentioned that if you had to go back and forth from the nursing home to the hospital, then all this would not be worth it. Do I have that right?”
Gerald: “There wouldn’t be any point to living if that happened. I think at that point I’d be a burden.”
Clinician: “So if we get there, we should consider stopping dialysis.”
Gerald: “I guess so…”
Clinician: “I imagine that it is hard to talk about this. I hope we do not get there for a long time.”
Gerald: “Me too. It is better to plan though, because it makes it easier on my family.”
Clinician: “Have you talked to them about all of this?”
Gerald: “I’ve mentioned it to them the last time that I was in the hospital.”
By outlining relevant milestones and pause points explicitly, the clinician and patient can better visualize the time when dialysis withdrawal may be an appropriate treatment consideration. Because patients may become too ill at some later time to make their own decisions, we recommend that the family members or a health care proxy be informed about this care plan and be present for its formulation and at future pause points.
Documenting and Revisiting the Care Plan
The verbal communication involved in determining the components of a goal-directed care plan using a time-limited trial that includes milestones and pause points should be documented in the medical record so that all members of the care team have access to it. The patient’s appointed decision-maker should also be clearly noted in the care plan documentation in the event that surrogate decision-making is needed.
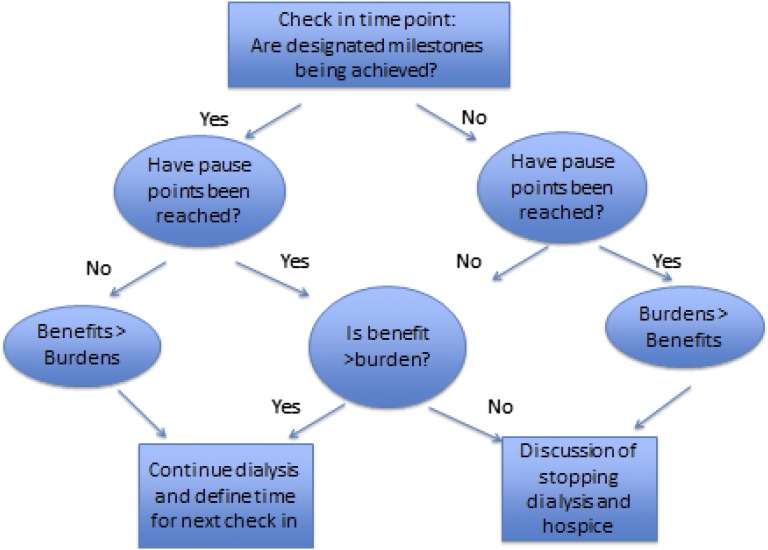
The care plan is meant to be fluid and not fixed, because patient-specific milestones and pause points may change. As the clinical course unfolds—often with unanticipated alterations in functional, cognitive, or clinical status—a given patient’s goals and preferences may also change (37). The content of the goal-directed care plan should also reflect this fluidity and be open to modification (Figure 1). Figure 1 outlines a goal-directed care plan that uses milestones and pause points to guide a time-limited dialysis trail. These care plans also encourage opportunities for the clinician to introduce palliative care and hospice services as a support for ongoing symptom management, additional advance care planning, and end-of-life care. Written documentation is particularly beneficial to guide surrogate decision-making for those patients who no longer have the capacity to participate in decisions related to treatments. Documentation includes outlining of the contents of the goal-directed care plan and completion of care preferences, such as written orders for life-sustaining therapies (38).
Figure 1.
Using milestones and pause points. Goal-directed plan of care with trial of dialysis.
Conclusion
Whether dialysis provides meaningful benefit or undue burden in frail elderly patients with progressive CKD is often unclear. Identifying those patients who may benefit from dialysis initiation is challenging and frequently fraught with uncertainty. We present a patient-centered, goal-directed framework for discussions of dialysis decision-making in seriously ill patients. We propose using open-ended questions to gain an understanding of the patient’s goals and concerns. From these discussions, the clinician is able to provide an informed, patient-specific recommendation. We define a time-limited trial of dialysis as a goal-directed treatment plan that outlines the milestones that the patient hopes to achieve with dialysis and the pause points at which time dialysis as a treatment should be reconsidered. Identifying pause points in the care plan promotes a timely shift toward comfort measures, which enables a patient to gain the fullest possible advantage from such end-of-life services as palliative care and hospice.
Disclosures
None.
Acknowledgment
We thank Dr. Robert Arnold for his expertise in communication skills education and helpful suggestions for this manuscript.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.USRDS : 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, 2013 [Google Scholar]
- 2.Johansen KL, Delgado C, Bao Y, Kurella Tamura M: Frailty and dialysis initiation. Semin Dial 26: 690–696, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roshanravan B, Khatri M, Robinson-Cohen C, Levin G, Patel KV, de Boer IH, Seliger S, Ruzinski J, Himmelfarb J, Kestenbaum B: A prospective study of frailty in nephrology-referred patients with CKD. Am J Kidney Dis 60: 912–921, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE: Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 361: 1539–1547, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh P, Germain MJ, Cohen L, Unruh M: The elderly patient on dialysis: Geriatric considerations. Nephrol Dial Transplant 29: 990–996, 2014 [DOI] [PubMed] [Google Scholar]
- 6.Jassal SV, Chiu E, Hladunewich M: Loss of independence in patients starting dialysis at 80 years of age or older. N Engl J Med 361: 1612–1613, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Chandna SM, Da Silva-Gane M, Marshall C, Warwicker P, Greenwood RN, Farrington K: Survival of elderly patients with stage 5 CKD: Comparison of conservative management and renal replacement therapy. Nephrol Dial Transplant 26: 1608–1614, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murtagh FE, Marsh JE, Donohoe P, Ekbal NJ, Sheerin NS, Harris FE: Dialysis or not? A comparative survival study of patients over 75 years with chronic kidney disease stage 5. Nephrol Dial Transplant 22: 1955–1962, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Schell JO, Patel UD, Steinhauser KE, Ammarell N, Tulsky JA: Discussions of the kidney disease trajectory by elderly patients and nephrologists: A qualitative study. Am J Kidney Dis 59: 495–503, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davison SN: End-of-life care preferences and needs: Perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol 5: 195–204, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singer PA, Thiel EC, Naylor CD, Richardson RM, Llewellyn-Thomas H, Goldstein M, Saiphoo C, Uldall PR, Kim D, Mendelssohn DC: Life-sustaining treatment preferences of hemodialysis patients: Implications for advance directives. J Am Soc Nephrol 6: 1410–1417, 1995 [DOI] [PubMed] [Google Scholar]
- 12.Wachterman MW, Marcantonio ER, Davis RB, Cohen RA, Waikar SS, Phillips RS, McCarthy EP: Relationship between the prognostic expectations of seriously ill patients undergoing hemodialysis and their nephrologists. JAMA Intern Med 173: 1206–1214, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wendler D, Rid A: Systematic review: The effect on surrogates of making treatment decisions for others. Ann Intern Med 154: 336–346, 2011 [DOI] [PubMed] [Google Scholar]
- 14.Wong SP, Kreuter W, O’Hare AM: Treatment intensity at the end of life in older adults receiving long-term dialysis. Arch Intern Med 172: 661–663, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong SP, Kreuter W, O’Hare AM: Healthcare intensity at initiation of chronic dialysis among older adults. J Am Soc Nephrol 25: 143–149, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mack JW, Weeks JC, Wright AA, Block SD, Prigerson HG: End-of-life discussions, goal attainment, and distress at the end of life: Predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol 28: 1203–1208, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, Mitchell SL, Jackson VA, Block SD, Maciejewski PK, Prigerson HG: Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300: 1665–1673, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP: SPIKES-A six-step protocol for delivering bad news: Application to the patient with cancer. Oncologist 5: 302–311, 2000 [DOI] [PubMed] [Google Scholar]
- 19.Fried TR, Bradley EH, Towle VR, Allore H: Understanding the treatment preferences of seriously ill patients. N Engl J Med 346: 1061–1066, 2002 [DOI] [PubMed] [Google Scholar]
- 20.Morton RL, Snelling P, Webster AC, Rose J, Masterson R, Johnson DW, Howard K: Dialysis modality preference of patients with CKD and family caregivers: A discrete-choice study. Am J Kidney Dis 60: 102–111, 2012 [DOI] [PubMed] [Google Scholar]
- 21.Winterbottom A, Bekker HL, Conner M, Mooney A: Choosing dialysis modality: Decision making in a chronic illness context [published online ahead of print July 2, 2014]. Health Expect 10.1111/j.1369-7625.2012.00798.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carson RC, Juszczak M, Davenport A, Burns A: Is maximum conservative management an equivalent treatment option to dialysis for elderly patients with significant comorbid disease? Clin J Am Soc Nephrol 4: 1611–1619, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morton RL, Snelling P, Webster AC, Rose J, Masterson R, Johnson DW, Howard K: Factors influencing patient choice of dialysis versus conservative care to treat end-stage kidney disease. CMAJ 184: E277–E283, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen LM, Ruthazer R, Moss AH, Germain MJ: Predicting six-month mortality for patients who are on maintenance hemodialysis. Clin J Am Soc Nephrol 5: 72–79, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moss AH, Ganjoo J, Sharma S, Gansor J, Senft S, Weaner B, Dalton C, MacKay K, Pellegrino B, Anantharaman P, Schmidt R: Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol 3: 1379–1384, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fine A, Fontaine B, Kraushar MM, Rich BR: Nephrologists should voluntarily divulge survival data to potential dialysis patients: A questionnaire study. Perit Dial Int 25: 269–273, 2005 [PubMed] [Google Scholar]
- 27.Back AL, Arnold RM: Discussing prognosis: “How much do you want to know?” talking to patients who are prepared for explicit information. J Clin Oncol 24: 4209–4213, 2006 [DOI] [PubMed] [Google Scholar]
- 28.Schell JO, Arnold RM: NephroTalk: Communication tools to enhance patient-centered care. Semin Dial 25: 611–616, 2012 [DOI] [PubMed] [Google Scholar]
- 29.Parker PA, Baile WF, de Moor C, Lenzi R, Kudelka AP, Cohen L: Breaking bad news about cancer: Patients’ preferences for communication. J Clin Oncol 19: 2049–2056, 2001 [DOI] [PubMed] [Google Scholar]
- 30.Ryan H, Schofield P, Cockburn J, Butow P, Tattersall M, Turner J, Girgis A, Bandaranayake D, Bowman D: How to recognize and manage psychological distress in cancer patients. Eur J Cancer Care (Engl) 14: 7–15, 2005 [DOI] [PubMed] [Google Scholar]
- 31.Suchman AL, Markakis K, Beckman HB, Frankel R: A model of empathic communication in the medical interview. JAMA 277: 678–682, 1997 [PubMed] [Google Scholar]
- 32.Back AL, Arnold RM, Baile WF, Tulsky JA, Fryer-Edwards K: Approaching difficult communication tasks in oncology. CA Cancer J Clin 55: 164–177, 2005 [DOI] [PubMed] [Google Scholar]
- 33.Evans WG, Tulsky JA, Back AL, Arnold RM: Communication at times of transitions: How to help patients cope with loss and re-define hope. Cancer J 12: 417–424, 2006 [DOI] [PubMed] [Google Scholar]
- 34.Back AL, Arnold RM: Dealing with conflict in caring for the seriously ill: “It was just out of the question.” JAMA 293: 1374–1381, 2005 [DOI] [PubMed] [Google Scholar]
- 35.Shared Decision-Making in the Appropriate Initiation of and Withdrawal from Dialysis, Rockville, MD, Renal Physicians Association, 2010 [Google Scholar]
- 36.Back AL, Arnold RM, Quill TE: Hope for the best, and prepare for the worst. Ann Intern Med 138: 439–443, 2003 [DOI] [PubMed] [Google Scholar]
- 37.Schell JO, Arnold RM: What are the ill effects of chronic dialysis? The benefits of a second conversation: How experience influences decision-making. Semin Dial 27: 21–22, 2014 [DOI] [PubMed] [Google Scholar]
- 38.Hickman SE, Nelson CA, Moss AH, Tolle SW, Perrin NA, Hammes BJ: The consistency between treatments provided to nursing facility residents and orders on the physician orders for life-sustaining treatment form. J Am Geriatr Soc 59: 2091–2099, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]