Abstract
Background
Timely access to trauma care requires that severely injured patients are ultimately triaged to trauma centers. We sought to determine triage patterns for the injured population within the state of California to determine those factors associated with under-triage.
Methods
We conducted a retrospective analysis of all hospital visits in California using the Office of Statewide Health Planning and Development Database from January 1, 2005, and December 31, 2009. All visits associated with injury were linked longitudinally. Sixty-day and one-year mortality was determined using vital statistics data. Primary field triage was defined as field triage to a Level I/II trauma center; re-triage was defined as initial triage to a non-Level I/II center followed by transfer to a Level I/II. Regions were organized by “Local Emergency Medical Services Agencies” (LEMSAs). The primary outcomes were triage patterns and mortality.
Results
The undertriage rate was 35% (N=20,988), but was variable across regions (12% to 87%). Primary field triage ranged from 7% to 77%. Re-triage rates were overall low (6%), but also varied by region (1% to 38%). In adjusted analysis, factors associated with a lower odds ratio of primary field triage included: age≥55 (OR 0.78, p=0.001), female gender (OR 0.88, p=0.014), greater number of comorbidities (OR 0.92, p<0.001), and fall mechanism vs. motor vehicle collision (OR 0.54, p<0.001). One-year mortality was higher for under-triaged patients (25% vs. 16% and 18% for primary field and re-triage, respectively; p<0.001).
Conclusions and Relevance
This is the first study to create a longitudinal database of all emergency department visits, hospitalizations, and long-term mortality for every severely-injured patient within an entire state over a 5-year time period. Under-triage varied substantially by region and was associated with multiple factors including access to care and patient factors.
Level of Evidence
Epidemiologic study, level III
Background
Inclusive trauma systems are designed to match the needs of injured trauma patients to the resources best suited for their needs. Care of severely-injured patients at Level I & II trauma centers has been shown to reduce mortality by as much as 25%.1 Ideally, pre-hospital emergency medical service providers and the network of hospitals within a region should work together to limit the percentage of severely-injured patients taken to a non-trauma center to 5%.2
In order to ensure trauma systems are optimally functioning, it is important to know where all severely injured patients are transported as well as their associated outcomes. This requires population-level data and long-term data on mortality. California has complete data on all emergency department and hospital visits which allows for such an analysis. It is the most populous state in the United States with widely varying geography that can present challenges for the triage of severely-injured patients. As in most states, authority over California's emergency medical service is not centralized. The responsibility to develop and act on triage policy falls to California's 32 Local Emergency Medical Service Agencies (LEMSAs) that govern the 58 counties within the State. Each LEMSA develops its triage policy which is then approved by the State of California's Emergency Medical Services Agency. Given these characteristics, California can serve as a model for understanding different factors that influence triage and outcomes.
We hypothesized that under-triage would be common and that there would be significant regional variability in triage patterns. To evaluate triage patterns and outcomes, we created a longitudinal database of all hospital and emergency room visits for injured patients, which was then linked to vital statistics data.
Methods
Data source and linkage
Data for all hospital discharges and Emergency Department (ED) visits in the state of California were obtained from the California's Office of Statewide Health Planning and Development Database (OSHPD)3 for the time between January 1, 2005, and December 31, 2009. Mortality was determined using the linked ED and PDD/Vital Statistics data provided by OSHPD. Detailed information on hospital characteristics was derived from the OSPHD State Utilization Data File of Hospitals. Trauma center status was confirmed manually for each hospital for each year by comparing to California Emergency Medical Information System (CEMSIS) data and evaluation of hospitals' websites.
Hospitalizations associated with a primary diagnosis of injury were identified. These admissions were linked to ED visits and other hospitalizations using patient-specific record linkage numbers. The operating assumption was that any ED visit or hospitalization that preceded or followed the index admission date by 2 days was likely associated with the same injury event. Two days was selected as the time frame as there are some transfer processes from rural areas which may take longer than 24 hours.
Inclusion/Exclusion Criteria
We included all patients ≥18 years of age with a hospital admission listing a primary diagnosis consistent with trauma (ICD9-CM 800.00 to 959.0, excluding 905 to 909; and 910 to 924, and 930 to 939). 2 Patients were excluded if the primary diagnosis was listed as a burn injury, if the index admission was listed as “elective,” or if admission was not to a general acute care hospital (e.g. psychiatric health facility). Patients who had an ED disposition indicating death were excluded as it would have not been possible to distinguish between dead-on-arrival versus those who died in the ED. We also excluded cases where it would have been impossible to link or determine the order of subsequent hospital visits (e.g. patient records without record-linkage numbers or dates of service).
Definitions and Outcomes
We analyzed patients who were severely injured as defined by an injury severity score (ISS) >15.2 ISS was derived using a Stata module, the ICD Programs for Injury Categorization (ICDPIC, version 3.0).4,5
The primary outcomes for the study were triage patterns and long-term (60-day and 1-year) mortality. Triage patterns were categorized as field triage, re-triage, and under-triage. “Field Triage” was defined as a patient with an ISS>15 who was directly transported from the field to a Level I or II trauma center. “Re-Triage” was defined as a patient with an ISS>15 who first visited a non-Level I/II trauma center, but was subsequently taken to a Level I/II trauma center. “Undertriage” was defined as any patient with an ISS>15 who was never taken to a Level I/II trauma center.
Adjustment Variables
Demographic information including age, gender, and race/ethnicity were included in the analysis. Insurance status was classified into the following categories: uninsured/self-pay, Medicare, Medicaid, private (including commercial Insurance and commercial HMO), other (e.g., worker's compensation, TRICARE, CHAMPUS), and unknown. Elixhauser comorbidity data were derived from the ICDPIC module and was included in the analysis to control for comorbidities. 6
The ICD-9 Injury Severity Scores (ICISS) were used to adjust for likelihood of survival based on injury diagnoses.7,8 Mechanisms of injury were included in the analysis and were determined using principal E-codes (present in 97% of patients). Finally, the rural-urban designation of the index hospital was also included and was derived from Rural-Urban Commuting Area Codes (RUCA) classification system.9,10
Analysis
Statistical Analysis was performed using SAS version 9.2 (SAS Institute, Inc., Cary, NC). Categorical data was compared using chi square analysis. Continuous data were compared using Student's T-test for data satisfying normality assumptions and Wilcoxon rank sum was used for nonparametric data. We performed multivariate logistic regression using a priori determined predictor variables. A random effects model was used to cluster by hospital. These variables include age, sex, race, insurance status, injury severity (ISS and ICISS), mechanism of injury, number of Elixhauser comorbidities, and rural-urban status of the first hospital visited.
Results
A total of 550,683 injured adults were admitted to acute care hospitals for trauma over the study time period. Of this group 60,182 (11%) were severely-injured (as defined by an ISS>15). Severely-injured patients were more often older (52% were ≥ 55 years of age), male (67%), and white (59%). (Table 1) For patients who survived the ED, 60-day mortality was 14% and by one year, mortality had risen to 19%.
Table 1. Patient Demographics and Injury Characteristics.
| All Patients (N = 60182) | Primary Field Triage (N = 35299) | Re-Triage (N = 3342) | Undertriaged (N = 20988) | diff | |
|---|---|---|---|---|---|
| Demographics | |||||
|
| |||||
| Age | <0.001 | ||||
|
| |||||
| 18-24 | 7787 (12.94%) | 6066 (17.18%) | 413 (12.36%) | 1250 (5.96%) | |
| 25-34 | 6446 (10.71%) | 4926 (13.96%) | 371 (11.10%) | 1096 (5.22%) | |
| 35-44 | 6300 (10.47%) | 4564 (12.93%) | 354 (10.59%) | 1303 (6.21%) | |
| 45-54 | 8487 (14.10%) | 5737 (16.25%) | 468 (14.00%) | 2181 (10.39%) | |
| 55-65 | 7092 (11.78%) | 4280 (12.12%) | 435 (13.02%) | 2307 (10.99%) | |
| 65-74 | 6684 (11.11%) | 3203 (9.07%) | 375 (11.22%) | 3028 (14.43%) | |
| 75-84 | 9882 (16.42%) | 3901 (11.05%) | 544 (16.28%) | 5359 (25.53%) | |
| >84 | 7504 (12.47%) | 2622 (7.43%) | 382 (11.43%) | 4464 (21.27%) | |
|
| |||||
| Gender | <0.001 | ||||
|
| |||||
| Male | 40100 (66.63%) | 25193 (71.37%) | 2221 (66.46%) | 12316 (58.68%) | |
| Female | 20082 (33.37%) | 10106 (28.63%) | 1121 (33.54%) | 8672 (41.32%) | |
|
| |||||
| Race | <0.001 | ||||
|
| |||||
| White | 35745 (59.39%) | 19696 (55.80%) | 2149 (64.30%) | 13555 (64.58%) | |
| Black | 4410 (7.33%) | 3214 (9.11%) | 139 (4.16%) | 1023 (4.87%) | |
| Hispanic | 12292 (20.42%) | 8047 (22.80%) | 662 (19.81%) | 3497 (16.66%) | |
| Asian | 4742 (7.88%) | 2382 (6.75%) | 141 (4.22%) | 2184 (10.41%) | |
| Other | 2036 (3.38%) | 1386 (3.93%) | 117 (3.50%) | 493 (2.35%) | |
| Unknown | 957 (1.59%) | 574 (1.63%) | 134 (4.01%) | 236 (1.12%) | |
|
| |||||
| Insurance Status | <0.001 | ||||
|
| |||||
| Self-pay | 5340 (8.87%) | 3528 (9.99%) | 603 (18.05%) | 1195 (5.69%) | |
| Medicare | 22941 (38.12%) | 9524 (26.98%) | 1212 (36.28%) | 12052 (57.43%) | |
| Medicaid | 7667 (12.74%) | 5969 (16.91%) | 350 (10.48%) | 1331 (6.34%) | |
| Private/HMO | 17017 (28.28%) | 10235 (29.00%) | 899 (26.91%) | 5522 (26.31%) | |
| Other | 7207 (11.98%) | 6038 (17.11%) | 277 (8.29%) | 884 (4.21%) | |
| Unknown | 7 (0.01%) | 5 (0.01%) | 0 (0.00%) | 2 (0.01%) | |
|
| |||||
| Injury Characteristics | |||||
|
| |||||
| Injury Severity | <0.001 | ||||
|
| |||||
| Mean ISS | 20.41 ± 7.67 | 21.57 ± 8.36 | 20.11 ± 8.43 | 18.52 ± 5.75 | |
|
| |||||
| Severity Categories | <0.001 | ||||
|
| |||||
| 15-24 | 49031 (81.47%) | 27063 (76.67%) | 2795 (83.63%) | 18683 (89.02%) | |
| >25 | 11151 (18.53%) | 8236 (23.33%) | 547 (16.37%) | 2305 (10.98%) | |
|
| |||||
| Mechanism of Injury | |||||
|
| |||||
| Penetrating | 3879 (6.45%) | 3290 (9.32%) | 172 (5.15%) | 398 (1.90%) | <0.001 |
| Falls | 23125 (38.43%) | 9603 (27.20%) | 1419 (42.46%) | 11928 (56.83%) | <0.001 |
| Any MVC | 18459 (30.67%) | 15093 (42.76%) | 793 (23.73%) | 2291 (10.92%) | <0.001 |
| Other | 7077 (11.76%) | 4303 (12.19%) | 540 (16.16%) | 2177 (10.37%) | <0.001 |
| Missing | 7642 (12.70%) | 3010 (8.53%) | 418 (12.51%) | 4194 (19.98%) | <0.001 |
|
| |||||
| Outcomes | |||||
|
| |||||
| 60-day mortalitya | 8253 (14.17%) | 4492 (13.12%) | 413 (12.85%) | 3322 (16.41%) | <0.001 |
| 1-year mortalityb | 9125 (19.27%) | 4603 (16.42%) | 451 (17.61%) | 4034 (24.70%) | <0.001 |
Censored at admission date of 10.31.2009;
Censored at admission date of 12.31.2008
HMO=Health Maintenance Organization; ICISS=ICD9 Injury Severity Score; MVC=Motor Vehicle Collision; LEMSA=Local EMS agency
The undertriage rate for the state during the study time period was 35% (N=20,988). Only 3,342 of 24,330 (14%) of patients with an ISS>15 initially brought to a non-trauma center were later transferred to a trauma center (i.e. “re-triaged”). Undertriage rates were higher in LEMSAs without trauma centers (58%) compared to those with trauma centers (32%). There was substantial variability in triage patterns between all of the LEMSAs. (Figures 1A&B)
Figure 1.
A & B: Triage patterns by Local Emergency Medical Services Agencies (LEMSA). Figure 1A shows only LEMSAs without trauma centers and Figure 1B shows LEMSAs with trauma centers.
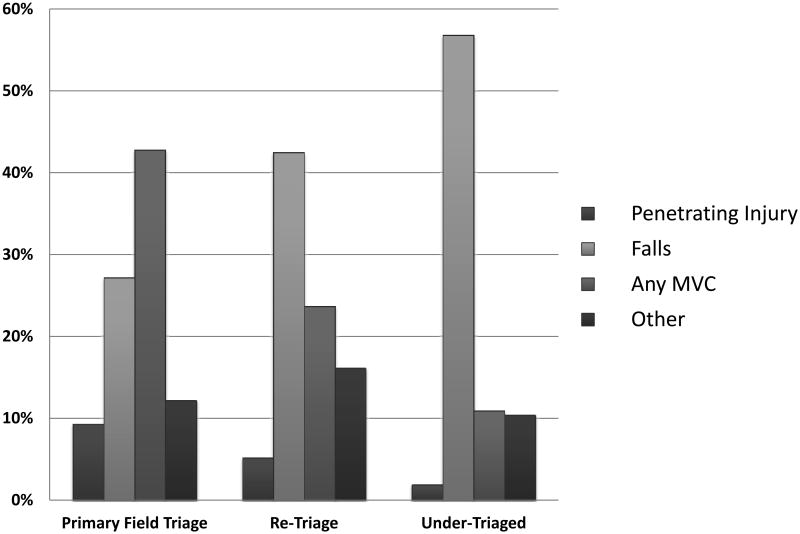
There were significant differences between patients who were treated at trauma centers compared to patients who were undertriaged. On average, undertriaged patients were older. Patients aged ≥ 55 comprised 52% of all patients with an ISS>15, but comprised 72% of the undertriaged population (vs. 40% of patients who were treated in a trauma center, p<0.001). Patients who were undertriaged were more often female (41% vs. 33% for all patients with ISS>15, respectively, p<0.001), and more often white (65% vs. 59% for all patients with ISS>15, p<0.001). Patients not taken to trauma centers were less severely-injured compared to primary field triage and re-triage patients (11% had an ISS ≥ 25 vs. 24% and 16%, respectively; p<0.001) and more often injured by a fall mechanism (57%, vs. 27% and 42% in primary field triage and re-triage patients, respectively, p<0.001). (Figure 2) In adjusted analysis, characteristics associated with likelihood of primary field triage including younger age, male gender, self-pay insurance status, lower ICISS (i.e. lower likelihood of survival), penetrating mechanism of injury, and fewer number of comorbidities. (Table 2)
Figure 2.
Proportion of mechanism by triage pattern.
Table 2. Determinants for Primary Field Triage.
| Odds Ratio | p value | Low 95% CI | High 95% CI | |
|---|---|---|---|---|
| Demographics | ||||
|
| ||||
| Age >55 (vs. <55) | 0.78 | <0.001 | 0.68 | 0.90 |
| Female (vs. male) | 0.88 | 0.01 | 0.79 | 0.97 |
|
| ||||
| Race (vs. white) | ||||
|
| ||||
| Black | 1.27 | 0.07 | 0.98 | 1.65 |
| Hispanic | 1.05 | 0.49 | 0.91 | 1.21 |
| Asian | 0.82 | 0.08 | 0.65 | 1.03 |
| Other | 1.54 | <0.001 | 1.16 | 2.06 |
| Unknown | 5.18 | <0.001 | 3.71 | 7.24 |
|
| ||||
| Insurance Status (vs. self-pay) | ||||
|
| ||||
| Medicare | 0.32 | <0.001 | 0.26 | 0.39 |
| Medicaid | 0.53 | <0.001 | 0.43 | 0.66 |
| Private/HMO | 0.44 | <0.001 | 0.36 | 0.52 |
| Other | 0.47 | <0.001 | 0.37 | 0.59 |
|
| ||||
| Injury Characteristics | ||||
|
| ||||
| Injury Severity | ||||
|
| ||||
| ICISS | 0.47 | <0.001 | 0.35 | 0.62 |
|
| ||||
| Mechanism of Injury vs. | ||||
|
| ||||
| Penetrating | 0.95 | 0.73 | 0.72 | 1.26 |
| Falls | 0.54 | <0.001 | 0.46 | 0.62 |
| Other | 0.63 | <0.001 | 0.53 | 0.74 |
|
| ||||
| Comorbidities | ||||
|
| ||||
| Number Elixhauser comorbidities | 0.92 | <0.001 | 0.89 | 0.95 |
|
| ||||
| LEMSA location (vs. urban) | ||||
|
| ||||
| Rural | 1.14 | 0.20 | 0.94 | 1.38 |
HMO=Health Maintenance Organization; ICISS=ICD9 Injury Severity Score; MVC=Motor Vehicle Collision; LEMSA=Local EMS agency
Undertriage was associated with higher unadjusted 60-day and 1-year mortality compared to primary field triage and re-triage. Sixty-day mortality rates were 16% for undertriaged patients vs. 13% for those who underwent primary field triage and re-triage (p<0.001). One-year mortality was 25% for patients who were undertriaged vs. 16% and 18% for primary field triage and re-triage, respectively (p<0.001). However, after adjusting for demographics, comorbidities, insurance status, urban/rural designation, mechanism of injury, and ICISS, mortality was not different for patients who were undertriaged vs. those who were treated in a trauma center (adjusted 60-day mortality odds ratio(OR) 1.04, 95% CI 0.94-1.14). Similarly, residing in a LEMSA that did not have a trauma center was not associated with higher adjusted odds of death for patients with an ISS>15 when compared to patients living in a LEMSA with a trauma center (adjusted OR 1.07, 95% CI 0.97-1.18). When comparing adjusted odds ratios for 60-day mortality across all LEMSAs, there was no statistical difference in outcomes between most of the regions. Only 4 of the 32 LEMSAs had significantly higher odds for 60-day mortality compared to the reference LEMSA. (Figure 3; reference LEMSA is “LL”)
Figure 3.
Adjusted odds for 60-day mortality for each LEMA, using LEMSA “LL” as the reference. Point marks the adjusted odds and bars represent the 95% confidence interval. Arrows mark the LEMSAs that are significantly different than the reference LEMSA.
Discussion
This is the first study to create a longitudinally-linked database for all injured patients in the most populous state in the United States from 2005 to 2009. We found that undertriage rates in California averaged 35% and that undertriage varied substantial between the different EMS regions. We know of no explicit policy differences between EMS regions to explain the observed variability. The high rate of undertriage is comparable to findings from two other statewide trauma triage studies. In 1988, Maryland was found to have an undertriage rate of 34%.11 In California, Vassar et al. found an undertriage rate of 44% from 1995-1997. Both of these previous studies used statewide administrative hospital discharge data; however, they differed slightly from the current study in that the definition for undertriage was based on a set of injury criteria thought to represent conditions best served by trauma centers.12 We chose to use an ISS>15 to be consistent with the definition used by the ACS-COT to determine trauma center need.13 Despite the differences in methodology, undertriage rates for the 3 studies are similar and provide some degree of validation.
The reasons for the observed rates of undertriage are likely multifactorial. Access to trauma centers likely plays a role as one-half of the LEMSAs do not have trauma centers and overall and undertriage is higher for LEMSAs without trauma centers. However, this cannot be the only determinant. There are high rates of under-triage (>20%) in all but one of the LEMSAs that have trauma centers. Of those LEMSAs that have trauma centers, some of the highest rates of under-triage (>30%) occur in urban areas that have easy access to a trauma centers. (Population density is not shown to maintain LEMSA anonymity.) Furthermore, two of the LEMSAs without trauma centers have under-triage rates that are lower than any of the LEMSAs with trauma centers. This argues that other factors other than having a trauma center in a LEMSA play a role in determining under-triage.
Patient factors suggest a possible cause for the observed rates of under-triage. Over 70% of the undertriaged patients were ≥55 years of age and almost 60% had a fall mechanism as the cause of their injuries. We also found that the adjusted odds for transfer to a trauma center were 0.78 for patients ≥55 compared to those younger than 55. These data suggest that under-triagemay be driven largely by the under-triage of severely injured elderly patients. Geriatric undertriage has been well-described in the literature. Nakamura et al. have shown a linear relationship between age and undertriage in a population-based study.14 Hsia et al. showed the odds of care at a trauma center was 0.30-0.35 for severely-injured elderly patients, even after controlling for patient and geography.15 Therefore, it may be that the severity of injuries in elderly patients who fall is under-appreciated by first responders who then transport patients to non-trauma centers. With a growing elderly population, this results in a large number of patients and therefore high under-triage rates overall for the trauma system. Further work is required to better understand how the trauma system performs for the young versus the old.
Another finding was that severely-injured patients that are initially transported to non-trauma centers are infrequently re-triaged (14%), and that these rates are also low in LEMSAs with trauma centers. This suggests that non-trauma hospitals are “sticky” with regards to transferring trauma patients with severe injuries. Since statewide trauma systems have limited influence over non-trauma hospitals, any policy changes will need to focus on improving primary field triage or find a way to encourage re-triage from non-trauma hospitals.
We also evaluated the association between triage patterns and mortality. Several studies have documented improved outcomes when severely-injured patients are treated in designated trauma centers.1,16-18 The landmark National Study on the Costs and Outcomes of Trauma (NSCOT) showed that the risk of death is 25% lower when care is provided in a regional, Level I trauma center than when it is provided in a non-trauma center hospital.13 We found higher unadjusted 60-day and 1-year mortality in the undertriaged population, but did not see mortality benefit after adjusting for patient and injury characteristics. One possible reason for this may be due to the large proportion of under-triaged patients who were elderly. The inclusion of elderly patients in trauma outcome analyses can affect results. When trauma center performance is subjected to risk-adjusted benchmarking, concordance for center performance across age strata shows poor agreement (kappa, 0.23). 19 This is likely due to the complexity of risk-adjustment in the setting of chronic conditions and varying levels of frailty. Furthermore, a recent population-based analysis of elderly trauma patients also failed to demonstrate a mortality benefit for severely injured elderly patients treated at trauma centers vs. non-trauma centers.20 Since the elderly comprise the vast majority of under-triaged patients and because outcomes for the elderly are worse than for they young, the observed outcomes may be driven by the poor outcomes of the elderly population.
The current study has several limitations. The first is that this represents a retrospective study based on administrative data. Because these are administrative data, we were limited in the amount of clinical data available to us. We were not able to include variables commonly used to risk adjust in trauma, such as admission blood pressure, pulse, or Glasgow Coma Score (GCS). These predictors have been recommended as necessary variables to accurately risk-adjust for mortality after trauma. 21 Another limitation was that we relied upon OSHPD-provided patient-specific linkage numbers and were unable to validate linkages against other patient identifiers.
In conclusion, this is the first study to create a longitudinal database of all ED visits, hospitalizations, and long-term mortality for every severely-injured patient in California over a 5-year time period. We have found that patients are often under-triaged, and that there is variability between regions. Different mechanisms are likely at play. In particular, it is clear that elderly patients who fall are commonly undertriaged, despite having sufficiently severe injuries to warrant trauma center care. Improving timely access to trauma center care must involve a multi-faceted strategy incorporating policymakers, pre-hospital personnel, non-trauma hospitals, and trauma centers. Since California has varying population densities and geography, findings from this study have relevance for other regions of the country.
Acknowledgments
Funding/Support: This publication was supported by the NIH/NCRR/OD UCSF-CTSI grant number KL2 RR024130 (RYH), and the Robert Wood Johnson Foundation Physician Faculty Scholars (RYH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of any of the funding agencies.
Role of the Sponsors: NA
Footnotes
Author Contributions: Dr. Hsia and Feng Lin had full access to all of the data in the study and takes responsibility for the integrity of the data. Dr. Staudenmayer and Feng Lin take responsibility for the accuracy of the data analysis.
Study concept and design: Staudenmayer, Mackersie, Hsia.
Acquisition of data: Hsia.
Analysis and interpretation of data: Staudenmayer, Lin, Mackersie, Spain, Hsia, Sinz.
Drafting of the manuscript: Staudenmayer, Hsia.
Critical revision of the manuscript for important intellectual content: Staudenmayer, Mackersie, Spain, Hsia, Sinz.
Statistical analysis: Staudenmayer, Lin, Hsia.
Obtained funding: Hsia.
Administrative, technical, or material support: Staudenmayer.
Study supervision: Hsia.
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr. Mackersie reported a relationship with the California State Emergency Medical Services Authority. No other authors reported disclosures.
Disclaimer: The views expressed in this article do not reflect positions of Stanford University, the University of California, San Francisco, or the California State Emergency Medical Services Authority.
Contributor Information
Kristan Staudenmayer, Email: kristans@stanford.edu.
Feng Lin, Email: flin@psg.ucsf.edu.
Robert Mackersie, Email: rmackersie@sfghsurg.ucsf.edu.
David Spain, Email: bonnie.sinz@emsa.ca.gov.
Renee Hsia, Email: renee.hsia@emergency.ucsf.edu.
References
- 1.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006 Jan 26;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 2.Resources for Optimal Care of the Injured Patient. Chicago: American College of Surgeons; 2006. [PubMed] [Google Scholar]
- 3.Office of Statewide Health Planning and Development (OSHPD) [Accessed February 1, 2013]; web site. http://www.oshpd.ca.gov/
- 4. [Accessed February 1, 2013];ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. http://ideas.repec.org/c/boc/bocode/s457028.html.
- 5.icdpic -- International Classification of Diseases Programs for Injury Categorization [computer program]. Version Version 3.0.
- 6.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998 Jan;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Osler T, Rutledge R, Deis J, Bedrick E. ICISS: an international classification of disease-9 based injury severity score. J Trauma. 1996 Sep;41(3):380–386. doi: 10.1097/00005373-199609000-00002. discussion 386-388. [DOI] [PubMed] [Google Scholar]
- 8.Rutledge R, Osler T, Emery S, Kromhout-Schiro S. The end of the Injury Severity Score (ISS) and the Trauma and Injury Severity Score (TRISS): ICISS, an International Classification of Diseases, ninth revision-based prediction tool, outperforms both ISS and TRISS as predictors of trauma patient survival, hospital charges, and hospital length of stay. J Trauma. 1998 Jan;44(1):41–49. doi: 10.1097/00005373-199801000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005 Jul;95(7):1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morrill R, Cromartie J, Hart LG. Metropolitan, urban, and rural communting areas: toward a better depiction of the U.S. settlement system. Urban Geogr. 1999;20(8):727–748. [Google Scholar]
- 11.MacKenzie EJ, Steinwachs DM, Ramzy AI. Evaluating performance of statewide regionalized systems of trauma care. J Trauma. 1990 Jun;30(6):681–688. doi: 10.1097/00005373-199006000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Vassar MJ, Holcroft JJ, Knudson MM, Kizer KW. Fractures in access to and assessment of trauma systems. J Am Coll Surg. 2003 Nov;197(5):717–725. doi: 10.1016/S1072-7515(03)00749-X. [DOI] [PubMed] [Google Scholar]
- 13.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006 Jan 26;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 14.Nakamura Y, Daya M, Bulger EM, et al. Evaluating age in the field triage of injured persons. Ann Emerg Med. 2012 Sep;60(3):335–345. doi: 10.1016/j.annemergmed.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsia RY, Wang E, Torres H, Saynina O, Wise PH. Disparities in trauma center access despite increasing utilization: data from California, 1999 to 2006. J Trauma. Jan;68(1):217–224. doi: 10.1097/TA.0b013e3181a0e66d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haas B, Jurkovich GJ, Wang J, Rivara FP, Mackenzie EJ, Nathens AB. Survival advantage in trauma centers: expeditious intervention or experience? J Am Coll Surg. 2009 Jan;208(1):28–36. doi: 10.1016/j.jamcollsurg.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Nathens AB, Jurkovich GJ, Cummings P, Rivara FP, Maier RV. The effect of organized systems of trauma care on motor vehicle crash mortality. Jama. 2000 Apr 19;283(15):1990–1994. doi: 10.1001/jama.283.15.1990. [DOI] [PubMed] [Google Scholar]
- 18.McConnell KJ, Newgard CD, Mullins RJ, Arthur M, Hedges JR. Mortality benefit of transfer to level I versus level II trauma centers for head-injured patients. Health Serv Res. 2005 Apr;40(2):435–457. doi: 10.1111/j.1475-6773.2005.00366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haas B, Gomez D, Xiong W, Ahmed N, Nathens AB. External benchmarking of trauma center performance: have we forgotten our elders? Ann Surg. 2011 Jan;253(1):144–150. doi: 10.1097/SLA.0b013e3181f9be97. [DOI] [PubMed] [Google Scholar]
- 20.Staudenmayer KL, Hsia RY, Mann NC, Spain DA, Newgard CD. Triage of elderly trauma patients: a population-based perspective. J Am Coll Surg. 2013 Oct;217(4):569–576. doi: 10.1016/j.jamcollsurg.2013.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haider AH, Saleem T, Leow JJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? J Am Coll Surg. 2012 May;214(5):756–768. doi: 10.1016/j.jamcollsurg.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]