Abstract
Described for the first time in 2004 for performing minor lung resection, during the following ten years a growing scientific evidence supported the spread and evolution of the uni-portal video-assisted thoracic surgery (VATS). This novel approach, performed using a single thoracic incision, requires a change of perspective in relation to traditional VATS, offering on the other hand a great versatility for numerous surgical procedures. The present work reviews the literature inherent to the uni-portal VATS with the aim of highlighting the principles of this technique, the fields of application, the obtained results and the future perspectives.
Keywords: Minimally invasive, video-assisted thoracic surgery (VATS), uni-portal VATS, lung resection
Introduction
During the last fifteen years, we have seen a substantial change of course in the scenario of thoracic surgery. The minimally invasive video-assisted surgical approach has spread in a gradually wider and more rapid way, being nowadays the treatment of choice for many thoracic disease traditionally managed by open surgery.
This is the result caused by a growing scientific evidence demonstrating the effectiveness of the video-assisted thoracic surgery (VATS) at various levels: reduction of tissue damage, postoperative pain and immunological impact, lower postoperative complications rate, shortening of length of stay, more rapid postoperative recovery of physical, emotional and social role, cost containment.
In this context, the uni-portal VATS plays a prominent role, representing the VATS with the least possible trauma for thoracic operations.
It has been performed a literature search using the following MeSH terms: “lung resection” AND “uni-portal VATS” AND “single port VATS”). The obtained papers were examined by both authors, which selected those to retrieve considering the titles (first exclusion process) and then the abstracts of the remaining studies (second exclusion process). Review papers were also searched for cross-references (Figure 1). We decided of considering exclusively those papers in English language and the search was carried out in March 2014.
Figure 1.
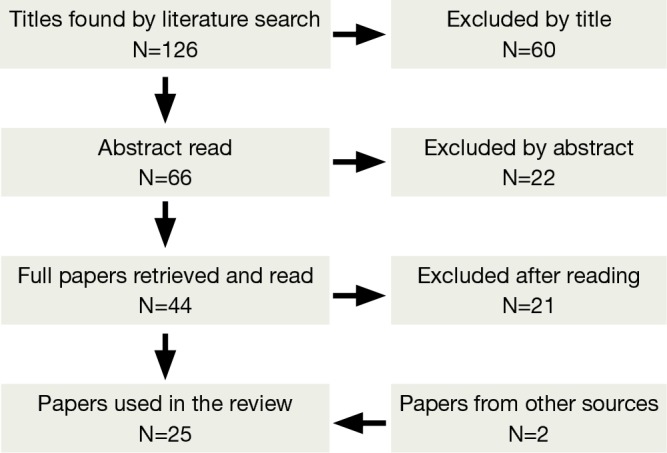
Literature search method.
Brief technique description
In 2004 Rocco et al. described for the first time a novel technique to perform pulmonary wedge resections through a single thoracic incision, with the assistance of a 5 millimeter thoracoscope (1). The theoretical and practical aspects of the so-called uni-portal VATS were more widely explained in two other papers published in 2005 (2,3) by the same group of authors.
The uni-portal approach for the treatment of thoracic diseases implies a substantial mindset change in comparison to the three-portal VATS, with consequent technical implications.
The single incision of the chest has a variable extent between 1 and 2.5 centimeters in relation to the different indications for the operation and eventually to the extent of resection. In any case the operative instruments as well as the videocamera lies in the same hole of the intercostal space, representing the fulcrum where they mutually move in. This fulcrum and the target lesion settle a unique plane, within which the surgical instrument and the thoracoscope operate. Changing the fulcrum point (varying the intercostal space, or the location in the same intercostal space) dependently to the target, it is possible to create infinite planes, able to reach virtually all the positions and lesions inside the chest cavity (1-4). As a result, this approach offers a considerable freedom of movement in spite of only one access point, that is further increased by the use of reticulating instruments and videocamera with 30 degrees vision. Figure 2 shows the different working planes and the strategy to reach the target lesion for the uni-portal and traditional three-portal VATS.
Figure 2.

(A) Different approach to the target lesion in three-portal uni-portal (B) VATS. VATS, video-assisted thoracic surgery.
The geometrical and optical benefits of the uni-portal VATS have been recently described by Bertolaccini et al. (5). In 2013 they published a paper that describes the advantage of the uni-portal approach, offering a projective plane with a cranio-caudal perspective that maintain the depth of intraoperative visualization and a more intuitive instrumentation movement.
Literature revision
The first paper published by Rocco et al. about the use uni-portal VATS in 2004, described the feasibility of wedge pulmonary resection (1). The authors reported fifteen cases performed by a single port approach without complication intra- or postoperatively, and without any conversion to three-port VATS or thoracotomy.
Since then the indications of this technique have increased considerably.
In 2007 Rocco described the use of this technique for the sympathectomy in the treatment of hyperhidrosis (6). Chen et al. published in 2009 the results of a comparison between 20 patients submitted to video-assisted thoracoscopic sympathectomy by a single port and 25 treated by a bi-portal approach (7). For both groups the treatment was effective (hands warm and dry for all patients), without any conversion to a more invasive procedure for the uni-portal patients. Moreover the authors found a reduction of the operative time (uni-portal 39.5 min vs. bi-portal 49.7, P=0.02) and inpatient pain scores (uni-portal 0.8 vs. bi-portal 1.6, P=0.02) in favor of the uni-portal approach, with comparable results in terms of mean hospital stay, compensatory sweating, and patient satisfaction.
The uni-portal VATS was then used for performing wedge lung biopsy in order to obtain specific diagnosis in patients affected by interstitial lung disease, as reported by Rocco et al. in 2005 (3). They were able to perform a median of two lung biopsies for each of the 20 patient treated, obtaining a diagnosis that altered the therapeutic management in 14 of them.
In 2005 and 2008 two different papers assessed the advantages of the uni-portal VATS for the treatment of primary spontaneous pneumothorax in comparison to the traditional three-portal approach (8,9). Jutley et al. compared 16 pneumothorax patients submitted to surgery using the uni-portal approach to 19 patients treated by the three-portal VATS. They found similar drainage time, length of stay and recurrence rate but a lower post-operative pain and paraesthesia incidence in favor to the uni-portal group. In 2008 Salati et al. reported the clinical and economic results of the use of uni-portal VATS versus the traditional three-portal approach for the treatment of primary spontaneous pneumothorax (uni-portal group: 28 patients vs. three-portal group: 23 patients). All the patients were submitted to bullectomy and pleural abrasion. The uni-portal group experienced a faster hospital stay (3.8 vs. 4.9 days, P=0.03) and a lower incidence of paraesthesia (35% vs. 94%, P<0.0001). Moreover the authors found an overall cost reduction for the uni-portal technique (1,407 Euros vs. 1,793 Euros, P=0.03).
In 2006 Rocco et al. reported the feasibility of pericardial window using an uni-portal approach (10). They described the technique to perform this procedure in four patients with malignant pericardial effusion, underlining the possibility of performing concomitant procedures (as mediastinal nodes biopsies) and the minimization of the patient discomfort.
In a paper of 2006 the uni-portal VATS was presented as a valuable technique supplementary to the conventional approach (mediastinoscopy, anterior mediastinotomy, three-port VATS) for the mediastinal nodes diagnosis (11). The authors described 13 patients operated by a single video-assisted access: the diagnosis was obtained in all cases (primary malignant nodal disease—5, secondary malignant nodal disease—6, granulomatous systemic disease—2), with a median postoperative hospital stay of 1 day.
The versatility of the uni-portal VATS technique made possible its use for the treatment of a patient affected by penetrating chest trauma (shotgun) (12). The authors reported the possibility of performing the procedure through the same incision of the chest tube inserted to evacuate the hemothorax. They were able to explore the entire thoracic cavity and remove the bullet situated in the costophrenic recess.
The last frontiers of implementation of the uni-portal VATS have made possible its use in the treatment of patients in an ambulatory setting without general anesthesia and in the execution of major anatomic pulmonary resections.
In 2010 and 2011 Rocco et al. described two different cases of pulmonary wedge resection performed through a video-assisted single access (13,14). Both patients received a mild sedation and an epidural anesthesia, moreover an intra-bronchial ballon catheter, bronchoscopically positioned, excluded from ventilation the lobe containing the target lesion. The authors performed the pulmonary resection using multiple endo staplers firings (resection of pulmonary nodule—first case and bullectomy for pneumothorax—second case), and they were able to discharge the patients the day after the surgical procedure. In 2014 Galvez et al. (15) confirmed the feasibility of the procedure, performing a metastasectomy of the left upper lobe without the necessity of endoscopic procedure for lobar collapse. It should be underline that the surgical incision was 5 cm long in this case.
In 2011 Gonzalez et al. reported a case of left lower lobectomy performed by a video-assisted single-port incision (16). This novel technique adopted several methodological aspects clearly stated by the uni-portal VATS and modulated them to perform anatomic major lung resection. The single access is 4 cm long and allows inserting all the operative instruments as well as the videocamera (usually 10-mm thoracoscope, 30-degrees), that is placed at the tail of the incision. The methodology and the operative steps of this novel technique were extensively described in a paper published in 2012, with specific annotation for each type of lobar resection (17). In the same year, Gonzalez-Rivas et al. published their initial experience of 23 patients treated by the uni-portal VATS lobectomy (18), showing a success rate of 87% with no mortality and a postoperative length of stay of about 3 days. Parallel with the refinement of the technique and the evolution of the operative armamentarium, the uni-portal VATS for major lung resection was applied for performing progressively more challenging operation, as anatomic segmentectomy (19), pneumonectomy (20), sleeve lobectomy (21) and pulmonary artery reconstruction (22).
Conclusions
From the first report published 10 years ago, the uni-portal VATS has greatly expanded its scope. The progressive refinement of the technique associated with a broader range of surgical instruments made possible the treatment of the vast majority of the pathologic intra-thoracic conditions (23), including the major anatomic pulmonary resections for primary lung malignancy (24).
Neverthless, due to its relatively recent description and implementation, this minimally invasive approach has the potential and the urgency to expand the scientific evidence about its benefits as well as to explore new areas of use.
In this sense, some papers have already demonstrated the advantage of the uni-portal VATS in comparison to the traditional multi-portal techniques. The reduction in postoperative pain and neurologic complaints was showed by more than one study which verified the uni-portal VATS outcomes in patients treated for primary spontaneous pneumothorax (4,8). Moreover it has been documented a faster postoperative hospital stay and recovery of daily life activities as well as a clear cost reduction in the same group of patients (4). At the same time, there is lack of large comparative or randomized studies aimed at verifying a reasonable positive effect of this minimally invasive approach on the above-mentioned outcomes and on the immunologic status of the patients, particularly in those submitted to major lung resection for neoplasm.
Finally, reflecting a constant evolution of the uni-portal VATS, this approach was also adopted to identify and resect peripheral lung nodules with the help of an articulating endoscopic ultrasound (25). This opens another scenario where the uni-portal VATS could play a prominent role, contributing at the identification and diagnosis of lung or mediastinal lesion not reached until now.
At the same time, it is desirable the growth of solid scientific evidence to confirm the advantages of this technique over the traditional approaches.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Rocco G, Martin-Ucar A, Passera E.Uni-portal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [DOI] [PubMed] [Google Scholar]
- 2.R Rocco G. VATS lung biopsy: the uni-portal technique. Multimed Man Cardiothorac Surg 2005;2005:mmcts.2004.000356. [DOI] [PubMed]
- 3.Rocco G, Khalil M, Jutley R.Uni-portal video-assisted thoracoscopic surgery wedge lung biopsy in the diagnosis of interstitial lung diseases. J Thorac Cardiovasc Surg 2005;129:947-8. [DOI] [PubMed] [Google Scholar]
- 4.Salati M, Brunelli A, Rocco G.Uni-portal video-assisted thoracic surgery for diagnosis and treatment of intrathoracic conditions. Thorac Surg Clin 2008;18:305-10. [DOI] [PubMed] [Google Scholar]
- 5.Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uni-portal VATS. J Thorac Dis 2013;5:S214-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rocco G. Endoscopic VATS sympathectomy: the uni-portal technique. Multimed Man Cardiothorac Surg 2007;2007:MMCTS.2004.000323. [DOI] [PubMed]
- 7.Chen YB, Ye W, Yang WT, et al. Uni-portal versus biportal video-assisted thoracoscopic sympathectomy for palmar hyperhidrosis. Chin Med J 2009;122:1525-8. [PubMed] [Google Scholar]
- 8.Jutley RS, Khalil MW, Rocco G. Uni-portal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [DOI] [PubMed] [Google Scholar]
- 9.Salati M, Brunelli A, Xiumè F, et al. Uni-portal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008;7:63-6. [DOI] [PubMed] [Google Scholar]
- 10.Rocco G, La Rocca A, La Manna C, et al. Uni-portal video-assisted thoracoscopic surgery pericardial window. J Thorac Cardiovasc Surg 2006;131:921-2. [DOI] [PubMed] [Google Scholar]
- 11.Rocco G, Brunelli A, Jutley R, et al. Uni-portal VATS for mediastinal nodal diagnosis and staging. Interact Cardiovasc Thorac Surg 2006;5:430-2. [DOI] [PubMed] [Google Scholar]
- 12.Jutley RS, Cooper G, Rocco G. Extending video-assisted thoracoscopic surgery for trauma: the uni-portal approach. J Thorac Cardiovasc Surg 2006;131:1424-5. [DOI] [PubMed] [Google Scholar]
- 13.Rocco G, Romano V, Accardo R, et al. Awake single-access (uni-portal) video-assisted thoracoscopic surgery for peripheral pulmonary nodules in a complete ambulatory setting. Ann Thorac Surg 2010;89:1625-7. [DOI] [PubMed] [Google Scholar]
- 14.Rocco G, La Rocca A, Martucci N, et al. Awake single-access (uni-portal) video-assisted thoracoscopic surgery for spontaneous pneumothorax. J Thorac Cardiovasc Surg 2011;142:944-5. [DOI] [PubMed] [Google Scholar]
- 15.Galvez C, Bolufer S, Navarro-Martinez J, et al. Awake uni-portal video-assisted thoracoscopic metastasectomy after a nasopharyngeal carcinoma. J Thorac Cardiovasc Surg 2014;147:e24-6. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez D, Delgado M, Paradela M, et al. Uni-incisional video-assisted thoracoscopic left lower lobectomy in a patient with an incomplete fissure. Innovations 2011;6:45-47. [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Thoracoscopic lobectomy through a single incision. Multimed Man Cardiothorac Surg 2012;2012:mms007. [DOI] [PubMed]
- 18.Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. [DOI] [PubMed] [Google Scholar]
- 19.Gonzalez-Rivas D, Mendez L, Delgado M, et al. Uni-portal video-assisted thoracoscopic anatomic segmentectomy. J Thorac Dis 2013;5:S226-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Uni-portal video-assisted thoracoscopic pneumonectomy. J Thorac Dis 2013;5:S246-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Left lower sleeve lobectomy by uni-portal video-assisted thoracoscopic approach. Interact Cardiovasc Thorac Surg 2014;18:237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Single-port video-assisted thoracoscopic lobectomy with pulmonary artery reconstruction. Interact Cardiovasc Thorac Surg 2013;17:889-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uni-portal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [DOI] [PubMed] [Google Scholar]
- 24.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uni-portal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5:S234-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rocco G, Cicalese M, La Manna C, et al. Ultrasonographic identification of peripheral pulmonary nodules through uni-portal video-assisted thoracic surgery. Ann Thorac Surg 2011;92:1099-101. [DOI] [PubMed] [Google Scholar]


