Abstract
Thanks to the recent improvements in thoracoscopy, a great deal of complex lung resections can be performed without performing thoracotomies. During the last years, experience gained through video-assisted thoracoscopic techniques, enhancement of the surgical instruments and improvement of high definition cameras have been the greatest advances. The huge number of surgical videos posting on specialized websites, live surgery events and experimental courses has contributed to the rapid learning of minimally invasive surgery during the last years. Nowadays, complex resections, such as post chemo-radiotherapy resections, lobectomies with chest wall resection, bronchial and vascular sleeves are being performed by thoracoscopic approach in experienced centers. Additionally, surgery has evolved regarding the thoracoscopic surgical approach, allowing us to perform these difficult procedures by means of a small single incision, with excellent postoperative results.
Keywords: Sleeve lobectomy, bronchoplasty, bronchial anastomosis, uniportal VATS, single-port lobectomy
Although the first thoracoscopic lung resection was performed in 1991 (1), the development and expansion of video surgery has been greater in the last 10 years. Internet and specialized web pages have been critical in this expansion, for they have given access to a great number of videos showing surgical techniques. Nowadays, more complex resections, such as post chemo-radiotherapy resections, lobectomies with chest wall resection, bronchial sleeves or vascular reconstructions are being performed and published. The experience acquired in the last years, as well as the development of thoracoscopic equipment (especially the introduction of the high definition) and the improvements of the surgical instruments have contributed to this.
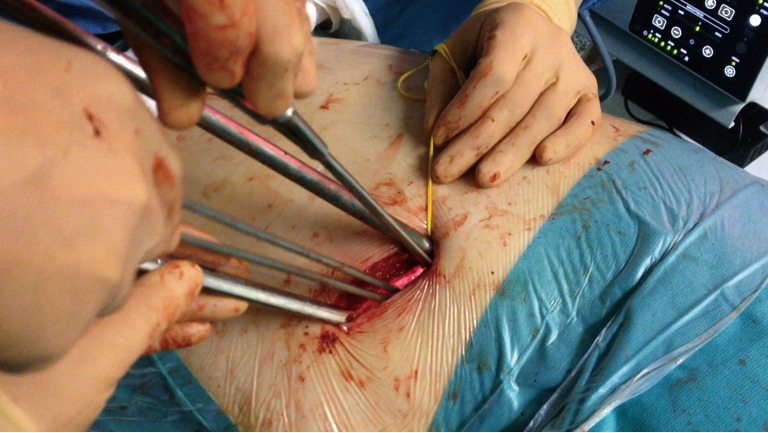
The bronchial or vascular reconstruction procedures are usually planned to preserve the lung parenchyma, avoiding pneumonectomies. Generally, these are complex procedures even with open surgery, but they can be performed thoracoscopically obtaining similar postoperative results in expert hands. During the last years, many groups have published their experience with sleeve procedures by conventional VATS (2,3). Most surgeons use a 3-4 incision VATS technique for sleeve anastomosis but the surgery can be performed by using only one incision (4,5). When performing bronchial suturing using single port VATS, it’s very important to maintain the camera on the posterior part of the incision, operating with both hands below the camera. Here we apply the same principle as when performing an anterior thoracotomy in open surgery: to have a direct view with the surgeon’s eyes above his/her hands. Using a plastic wound protector is helpful when dealing with obese patients because fatty tissue could interfere with the suture threads.
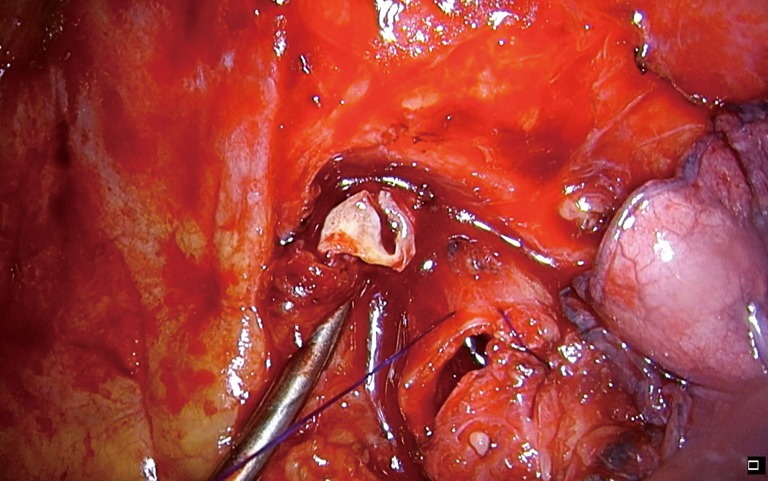
The use of material with proximal and distal articulation (Scanlan International Inc.) is crucial (Figure 1). The surgeon ties the knot outside of the chest with the right hand, holding both ends of the thread with the left hand’s index and little fingers and pushing down the knots using a thoracoscopic knot pusher (Figure 2). We usually don’t buttress the suture except in cases of preoperative radiotherapy. In these cases we use an intercostal muscle flap or a pedicle pericardial or mediastinal fat pad.
Figure 1.
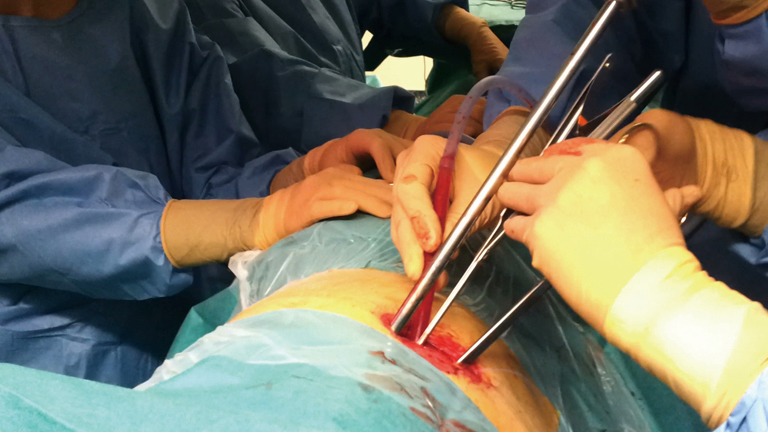
Surgical image of instrumentation during sleeve procedures.
Figure 2.

Technique for knot pushing through a single port (6). Available online: http://www.asvide.com/articles/352
The operating table’s position makes the lung exposure easier to perform the anastomosis (the anterior rotation of the table 45° to the surgeon places the lung on an anterior position and makes easier the posterior bronchial suture, especially the membranous portion).
Suture may be performed with single stitches or continuous suture. The usage of monofilament suture makes the thread movement easier, as well as the tying. The bronchial edge must be assessed during the operation, the suture is checked at the end of the surgery using insufflation under water and bronchoscopic control to check integrity and secretion aspiration.
We can classify three types of bronchoplastic procedures according to the resection type:
Simple bronchoplasty. The bronchus is cut in its origin using a scalpel, when the tumor is located to the bronchial base (due to this the use of an endostapler is not possible). For the closure, we use single double PDS 3/0 stitches (flushed shape) (Figure 3). Flap protection is not usually needed. When doing a simple bronchoplasty on the inferior right lobe, the suture must be carefully handled to avoid stenosis of the middle lobe bronchus.
Wedge bronchoplasty. In this case the bronchial cut is made deeper in wedge shape to the main bronchus (Figure 4). This kind of suture may call for a transverse closure, but if the wedge is large and doesn’t allow the approximation, it may be reconstructed using a lateral closure (Figure 5). We recommend the subcarinal lymph node dissection (lymphadenectomy) before the bronchoplasty in order to free the main bronchus and avoid an excessive traction once the suture is done.
Figure 3.

Simple bronchoplasty (7). Available online: http://www.asvide.com/articles/353
Figure 4.
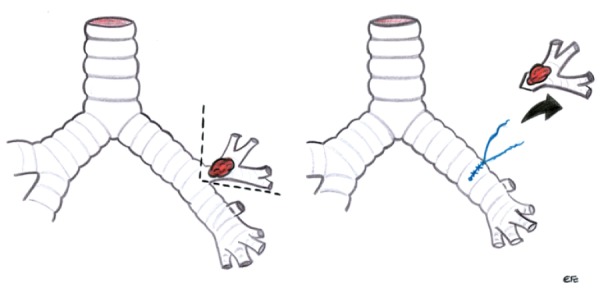
Drawing showing wedge bronchoplasty.
Figure 5.

Wedge bronchoplasty (8). Available online: http://www.asvide.com/articles/354
The suture is made without tension, with approximation to the mucosa using monofilament absorbable interrupted or continuous suture (PDS 3/0), with all knots preferably placed externally. The monofilament suture facilitates the movement through the bronchus and the tying of the knots.
Sleeve bronchoplasty. The bronchial sleeve resections with end to end anastomosis are the most complex bronchoplastic procedures (Figure 6). The right upper lobe bronchoplasty is normally the less difficult procedure, due to the alignment of the main and the intermediate bronchi (4). This location makes operating with both hands easier. The liberation of the pulmonary ligament, as well as the subcarinal lymph node dissection facilitate the lung mobility and avoid tension during the anastomosis.
Figure 6.
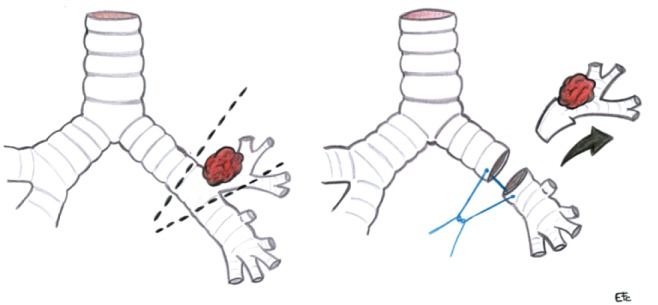
Drawing showing sleeve bronchoplasty.
The bronchus may be cut initially using a long scalpel, the bronchial circumference section may be completed using scissors.
We can use single stitches for the cartilage part and continuous suture for the membranous portion. It’s best to tie the single suture one by one, to avoid that the threads touch each other, and it’s preferable to tie the knot outwards (Figure 7). Another, more simple option (and with identical results) is to make the whole anastomosis using continuous PDS 3/0 suture. Usually, the posterior bronchus wall is stitched first and the anterior wall, from behind so that both edges are tied at the anterior level.
Figure 7.

Sleeve bronchoplasty (9). Available online: http://www.asvide.com/articles/355
The most complex sleeve procedures are usually those of the left side, due to the presence of the aortic arch and the bigger size of the pulmonary artery (Figure 8) (5). For left-sided bronchial resections, it’s best to use a right-sided double-lumen tube, in order to make suture easier and reduce the bronchus tension.
Figure 8.
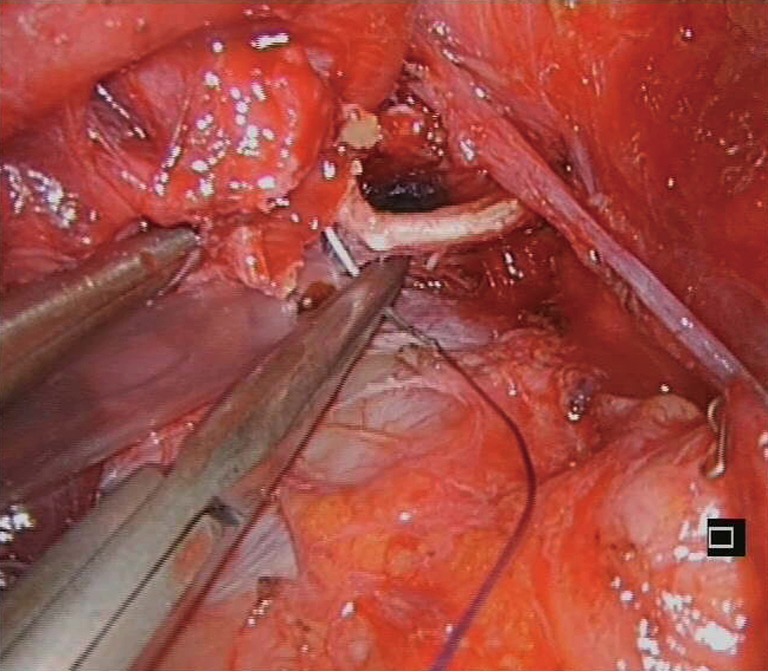
Surgical image of left lower sleeve anastomosis (main bronchus to left upper bronchus).
Segmental bronchial sleeve reconstruction (Figure 9)
Figure 9.
Sleeve segmental bronchoplasty (10). Available online: http://www.asvide.com/articles/356
In this particular case, In order to avoid a full sleeve, we perform a resection of the right main bronchus and right upper bronchus after a lower bilobectomy. The reconstruction is more complex in these cases, with anastomosis of the main bronchus to the right upper individual segmental bronchi. A careful reconstruction of the main bronchus’ suture is especially important, in order to avoid that the small segmental bronchi be closed after the anastomosis. In this scenario is better to perform interrupted sutures to adjust the segmental bronchi
Vascular resections
These procedures are complex and usually performed by open surgery or by conventional VATS by experienced and skilled thoracoscopic surgeons. However the same operation can be accomplished by using only a single incision VATS approach.
When the tumour invades the pulmonary artery, the artery as well as the basal trunk must first be controlled and dissected. Sometimes it’s necessary to perform an intrapericardial control. Before the pulmonary artery clamping, 5,000 UI heparine iv must be administered to prevent thrombosis. We prefer the pulmonary artery clamping with a large thoracoscopic clamp (D’Amico Clamp, Scanlan International, Inc.), which is placed on the inferior part of the wound. For distal clamping it’s better to use bulldog clamps on the most distal part of the basal trunk, or clamping the inferior pulmonary vein to interfere as less as possible with the instruments. Sometimes, a double vessel loop is enough for distal clamp, especially in the less complex reconstructions (Figure 10).
Figure 10.
Surgical image of instrumentation during right vascular reconstruction.
There are three types of vascular reconstructions:
Partial resection of the pulmonary artery
It’s a less complicated vascular reconstruction and it’s performed especially when the tumor invades the base of one of the mediastinal branches but without a large involvement into the main pulmonary artery (11).
After heparinization and clamping of the main artery and basal trunk we perform a tangential incision on the pulmonary artery and a direct closure by means of a running suture with prolene 5/0 or with several interrupted double sutures (Figure 10).
Once the suture is completed we release the most distal clamp to release any air thanks to the return flow and we tie once the artery is full. Then we do a progressive release of the proximal clamp. The clamp will not be entirely removed until we confirm that there is no bleeding (Figure 11).
Figure 11.
Vascular reconstruction (12). Available online: http://www.asvide.com/articles/357
Patch reconstruction
It’s a complicated procedure with VATS. Bovine pericardium may be used as well as a patch from the patient’s pericardium. The use of patches should be avoided as it could increase the risk of thrombosis. In the case of an extensive end-to-end resection, a tube may be created out of the pericardium in order to do an end-to-end anastomosis at each end of the resection. To our knowledge, these procedures have not been reported yet by VATS.
End-to-end anastomosis
Is probably the most complex procedure that can be done through VATS and it requires special skills and an extensive experience with video-assisted thoracoscopic surgery. In these cases of vascular reconstruction, it is advisable that this be the last step of the lobectomy (first divide the veins, bronchus and fissure) in order to have a larger surgical field and more control of the section of the pulmonary artery. Once the arterial trunk is clamped we cut the proximal and distal side using scissors and we position the lobe in the costodiaphragmatic angle, over the diaphragm in order to be extracted once the suturing is complete.
Vascular sleeve is more frequent on the left side, with tumors that invade the main pulmonary artery or the mediastinal branches that lead to the upper lobe.
For the end-to-end anastomosis it is important to free up the pulmonary ligament and sometimes open up the pericardium to free up tension. Due to the fragility of the pulmonary artery and in order to avoid ruptures during the anastomosis, special care must be given to the manipulation of sutures as well as a correct traction of the pulmonary artery.
It’s very important to adjust the diameters of the main artery to the lobar branches during anastomosis, in order to avoid kinking or stenosis. We start anastomosis with an anterior and posterior traction suture to adjust the diameters by using prolene 4/0 or 5/0. For the posterior suture, both needles are kept and once the knot is tied one of them is kept separately in the interior of the chest cavity (it will be used for suturing the superior face). A running suture is done on the inferior side of the artery from a posterior to anterior direction and we tie it to the anterior traction end. Then we use the other needle from the posterior traction end to complete the suture of the superior side and it is then tied to the anterior suture. Before tying we must release air and check the flow after opening the distal clamp (Figure 12).
Figure 12.
Sleeve end to end vascular anastomosis (13). Available online: http://www.asvide.com/articles/358
In case of the double sleeve, it is better to do the bronchial suturing first and after that the arterial reconstruction in order to avoid traction on the arterial suture (14) (Figure 13).
Figure 13.
Surgical image of double bronchovascular procedure.
Other complex resections
The single port technique allows us to make other complex procedures, such as Pancoast tumors (hybrid approach is necessary), superior sulcus tumors, and tumors with chest wall invasion or contralateral nodule resections on patients with previous pneumonectomy.
Sulcus tumors
The approach for Pancoast tumors approach is hybrid. We make the incision at the fifth intercostal space for the lobectomy and a high posterior incision or anterior superior Dartevelle or Grünenwald incision for the resection at apical level and vascular control. We can perform the superior approach first in order to free the lobe to the superior level or we can begin with the lobectomy and then perform the superior approach for resection, once the lobe has been freed.
For sulcus tumors without bone or vascular involvement, sometimes it’s enough to perform a deep extrapleural resection. We present the following case: a 50-year-old man with a sulcus tumor, treated with chemotherapy and concomitant radiotherapy, having good response. A right upper lobectomy was done, from anterior to posterior using the fissureless technique with the lung fixed to the apex. Once the lobectomy was done, a partial resection of the healthy lobe zone was performed in order to obtain more space to accomplish the resection of the tumor. It’s important to use energy devices to perform a more secure apical and extrapleural liberation. Surprisingly, the final pathological examination of this case confirmed a complete tumoral Junker regression. After 3 years there hasn’t been any sign of the tumor growing again (Figure 14).
Figure 14.
Superior sulcus tumor (15). Available online: http://www.asvide.com/articles/359
Tumors with chest wall involvement
When dealing with tumors that invade the chest wall we use a combined approach: single port for the lobectomy (fifth intercostal space) and a small lateral or posterior incision for the costal resection, according to the location of involvement (16). After evaluation of costal invasion and the tumor’s size (better or worse lobe mobility), we will perform either the lobectomy or the costal resection first. On this video we performed the right inferior lobectomy first using single port, once the lobe was freed the chest wall was resected and a mesh was placed thanks to the thoracoscopic vision (Figure 15).
Figure 15.
Lower lobectomy with chest wall resection (17). Available online: http://www.asvide.com/articles/360
Tumors on patients with previous pneumonectomy
Surgery on these patients must be extremely careful. Therefore, the resection must be as limited as possible. It’s important that the lobe to be operated is collapsed. A good option is the endotracheal intubation with a single tube and fogarty catheter directed with bronchoscopy to collapse the selected lobe. In this case we present a video of a patient with previous pneumonectomy (10 years before) and a new primary tumor. The patient presented costal fractures and hemothorax (which needed chest tube) in the past, as well as a previous intervention of pericardiectomy caused by a chronic constrictive pericarditis. These findings increased the difficulty and risk of the case. However the patient was proposed for a uniportal VATS resection. After a difficult extrapleural liberation of the lung (maintaining the superior lobe ventilation), we palpated the tumor into the left lower lobe and we resected it with endostaplers (Figure 16).
Figure 16.
Nodule resection in a patient with contralateral pneumonectomy (18). Available online: http://www.asvide.com/articles/361
Discussion
Uniportal VATS is not only indicated to initial stages or easy cases. With gained experience the most complex cases can be performed in the same manner as with double or triple port approach (19,20). Previous experience in VATS is necessary to perform these advanced cases with success (21). We have performed lobectomies with strong adherences after TB, redo-VATS, tumors with chest wall involvement, cases after high doses of chemo-radiotherapy, anatomic complex segmentectomies, vascular reconstruction, sleeve lobectomies, double sleeve, pneumonectomies and huge tumors by single incision VATS.
Despite the multiple advantages of conventional or uniportal VATS compared with thoracotomy as decreased postoperative pain, decreased hospitalization, diminished inflammatory response or faster access to chemotherapy, the uniportal VATS approach for advanced stages of lung cancer is still infrequent. The concern about an intraoperative thoracoscopic major bleeding or the technical complication of performing a radical oncologic resection by single port VATS in advanced cases are the main reasons for the low adoption. We recently assessed and published the feasibility of uniportal VATS approach in the treatment of advanced NSCLC and compared the perioperative outcomes with early-stage tumors with excellent postoperative results (21).
Since we developed our uniportal technique for VATS lobectomies in 2010 we have increased the application of this technique to more than 90% of cases in our routine surgical practice. The experience we acquired with the uniportal technique during the last years, as well as technological improvements in high definition cameras, development of new instruments, vascular clips and more angulated staplers have made this approach safer, incrementing the indications for single-port thoracoscopic resections. We believe it is important to minimize the surgical aggressiveness especially in advanced stage lung cancer patients where the immune system is weakened by the disease or by induction treatments (22). The minimally invasive surgery represents the least aggressive form to operate lung cancer and the single-port or uniportal technique is the final evolution in these minimally invasive surgical techniques.
The most complex resections are the thoracoscopic sleeve procedures. There are few articles published in the literature describing bronchial sleeve, vascular sleeve or combined bronchovascular sleeve by VATS, and all of these resections are reported by using conventional thoracoscopic techniques (23,24). As our experience has grown with the single-port VATS approach (4,20) we have increased the rate of thoracoscopic sleeve procedures and decreased the incidence of pneumonectomy, and even we have performed bronchovascular sleeve procedures by uniportal VATS (14,25). We found several advantages of the single incision thoracoscopic technique especially for sleeve procedures. The geometrical explanation of the approach, the direct view and bimanual instrumentation could explain the excellent results we have obtained with this technique (26).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed] [Google Scholar]
- 2.Agasthian T.Initial experience with video-assisted thoracoscopic bronchoplasty. Eur J Cardiothorac Surg 2013;44:616-23. [DOI] [PubMed] [Google Scholar]
- 3.Li Y, Wang J.Video-assisted thoracoscopic surgery sleeve lobectomy with bronchoplasty: an improved operative technique. Eur J Cardiothorac Surg 2013;44:1108-12. [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Left lower sleeve lobectomy by uniportal video-assisted thoracoscopic approach. Interact Cardiovasc Thorac Surg 2014;18:237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Technique for knot pushing through a single port. Asvide 2014;1:339. Available online: http://www.asvide.com/articles/352
- 7.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Simple bronchoplasty. Asvide 2014;1:340. Available online: http://www.asvide.com/articles/353
- 8.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Wedge bronchoplasty. Asvide 2014;1:341. Available online: http://www.asvide.com/articles/354
- 9.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Sleeve bronchoplasty. Asvide 2014;1:342. Available online: http://www.asvide.com/articles/355
- 10.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Sleeve segmental bronchoplasty. Asvide 2014;1:343. Available online: http://www.asvide.com/articles/356
- 11.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Single-port video-assisted thoracoscopic lobectomy with pulmonary artery reconstruction. Interact Cardiovasc Thorac Surg 2013;17:889-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Vascular reconstruction. Asvide 2014;1:344. Available online: http://www.asvide.com/articles/357
- 13.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Sleeve end to end vascular anastomosis. Asvide 2014;1:345. Available online: http://www.asvide.com/articles/358
- 14.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Superior sulcus tumor. Asvide 2014;1:346. Available online: http://www.asvide.com/articles/359
- 16.Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Single-incision thoracoscopic right upper lobectomy with chest wall resection by posterior approach. Innovations (Phila) 2013;8:70-2. [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Lower lobectomy with chest wall resection. Asvide 2014;1:347. Available online: http://www.asvide.com/articles/360
- 18.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Nodule resection in a patient with contralateral pneumonectomy. Asvide 2014;1:348. Available online: http://www.asvide.com/articles/361
- 19.Gonzalez-rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5:S234-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [DOI] [PubMed] [Google Scholar]
- 21.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hennon M, Sahai RK, Yendamuri S, et al. Safety of thoracoscopic lobectomy in locally advanced lung cancer. Ann Surg Oncol 2011;18:3732-6. [DOI] [PubMed] [Google Scholar]
- 23.Han Y, Zhou S, Yu D, et al. Video-assisted thoracic surgery (VATS) left upper sleeve lobectomy with partial pulmonary artery resection. J Thorac Dis 2013;5Suppl 3:S301-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu L, Mei J, Pu Q, et al. Thoracoscopic bronchovascular double sleeve lobectomy for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;46:493-5. [DOI] [PubMed] [Google Scholar]
- 25.Gonzalez-Rivas D, Fieira E, de la Torre M, et al. Bronchovascular right upper lobe reconstruction by uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2014;6:861-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5Suppl 3:S214-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


