Abstract
A number of strategies have been used to delay or prevent the development of type 2 diabetes mellitus (T2D) in high-risk adults. Among them were diet, exercise, medications and surgery. This report focuses on the nutritional lessons learned from implementation of the Intensive Lifestyle Intervention (ILI) in the DPP and its follow-up DPPOS that looked at weight loss through modification of diet and exercise. The Diabetes Prevention Program (DPP) is a large clinical trial, sponsored by the National Institutes of Health, designed to look at several strategies to prevent conversion to type 2 diabetes (T2D) by adults with prediabetes (IGT/IFG) including an Intensive Lifestyle Intervention (ILI). The ∼3800 ethnically diverse participants (46% reported non-white race) were overweight, had impaired glucose tolerance (IGT) and impaired fasting glucose (IFG). Treatments were assigned randomly. The Diabetes Prevention Program Outcomes Study (DPPOS) is a follow up study evaluating the long-term outcomes of the clinical trial.
Keywords: Lifestyle intervention, Diabetes prevention, weight loss, physical activity, prevention, diabetes, overweight, type 2 diabetes, nutrition, lifestyle, diet, genetics
Introduction
The prevention of type 2 diabetes mellitus (T2D) is a major public health challenge due to the significant impact it has on health and the economics of health care. Strategies for preventing or delaying T2D have been evaluated [1]. The Diabetes Prevention Program (DPP) and its follow-up Outcomes Study (DPPOS) have demonstrated that both ILI and metformin treatment can effectively prevent or delay the onset of T2D and improve related co-morbidities in participants who are overweight have IFG and IGT. In an intention to treat analysis, the DPP reported a 58% reduction in the incidence of T2D over 3.2 years in subjects in the ILI treatment group [2] and by 34% over a 10-year period [3]. Lifestyle intervention benefits were observed in both sexes, and in all age, BMI, racial and ethnic groups. The DPP lifestyle intervention focused on two of the major modifiable risk factors for T2D, body weight and physical activity. This report focuses on the 1079 participants randomized to the ILI treatment group during the DPP, of whom 910 enrolled in the DPPOS.
Methods
Eligibility criteria for the DPP included an age of ≥25 years, BMI ≥24 kg/m2 (BMI ≥22 kg/m2 for Asians), fasting plasma glucose of 95-125 mg/dl (≤125 mg/dl in American Indians) and a plasma glucose value of 140-199 mg/dl 2 hours after a 75-gram glucose load. The local Institutional Review Board(s) approved the protocol at each center, and all participants provided written informed consent before entering the study.
The design, lifestyle intervention methods, and characteristics of the DPP cohort have been described elsewhere [4] as have the lifestyle participants and intervention offered [5]. The lifestyle intervention goals were to reduce body weight by 7%, achieve or maintain 150 min of moderate intensity physical activity weekly, and to reduce dietary fat intake to <25% of calories; if weight loss was not achieved by lowering fat, calorie goals were introduced. The initial intervention consisted of individual meetings with a coach and periodic group classes thereafter designed to support the weight loss and physical activity goals. DPPOS provided support for the lifestyle participants at a much lower level than in the DPP [3, 6]. Incident T2D was assessed annually with an oral glucose tolerance test and semiannually with fasting glucoses that were confirmed if indicative of diabetes. The ADA diagnostic criteria were used [7]. Weight was measured semiannually. Food intake was assessed by interview at several intervals using a modified Block food frequency questionnaire [8-10]. Total MET hours per week of physical activity were assessed at the 1-year by the Modifiable Physical Activity Questionnaire [11]. Retention was excellent.
Description of the ILI
Individual case managers or “lifestyle coaches” delivered a structured 16-session core behavioral curriculum with continuing support or “Aftercore” and additional materials to address unique needs of the ethnically diverse participants that is available at http://www.bsc.gwu.edu/dpp/index.ritmlvdoc. Keys to success included 1) a goal based behavioral intervention, 2) lifestyle coaches, 3) frequent contact, 4) tailoring strategies, 5) materials and strategies to address the needs of an ethnically diverse population, and 6) an extensive local and national network [5, 12,13].
Lifestyle coaches, who were usually dietitians, tailored the intervention for individual participants [14] to address barriers and facilitate adherence among the large ethnically diverse participants. The most effective strategies were skill-building strategies for behavioral self-management. Individualization was achieved through a “toolbox” of adherence strategies and a flexible maintenance intervention of both group and individual approaches. The most frequently used items in the toolbox were the less costly such as; problem-solving, review of self-monitoring skills, and specific recommendations to increase physical activity or decrease fat and calories. Problem solving was the dominant intervention approach used by coaches to help participants achieve goals in the DPP and the DPPOS. “Problem Solving” is a 5-step behaviour change method that included: 1) maintaining a proactive attitude; 2) defining the problem/behaviour chains; 3) generating alternatives; 4) setting achievable goals and 5) evaluating success and repeating steps if necessary [15].
At the end of DPP, all participants were eligible for continued follow-up in DPPOS and 2766 of 3150 (88%) elected to continue [3]. All participants were invited to attend quarterly Healthy Eating and Lifestyle Programs (HELP). The purpose was to reinforce the original weight loss and physical activity goals by providing group classes related to healthy eating, weight management, and physical activity for diabetes prevention, the reduction of cardiovascular risk, and the promotion of optimal health and well-being. In addition, former Lifestyle participants were offered two motivational campaigns per year (BOOST) to provide structured focus on behavioral self-management strategies that are important for weight loss/maintenance and adherence to the physical activity goal. Lifestyle participants also completed a “Lifestyle Check-up” at both their annual and mid-year clinic visits to provide participants with individual feedback on their weight history and to review personal lifestyle goals and plans [3, 6].
Preventing Diabetes in the DPP
In the DPP, physical activity only had a small effect on T2D prevention and was dwarfed by the much stronger effect of weight loss [16]. For every kg of weight lost during the DPP, there was a 16% reduction in risk of developing T2D, adjusted for changes in diet and activity. Simultaneous adjustments for changes in physical activity, percent fat, IGT and elevated fasting insulin among other variables, had a negligible effect on the hazard ratio (HR) for weight loss compared with the unadjusted HR for weight loss. Compared with weight gain, a weight loss of ≥10% at 6 months was associated with an 85% reduction in the incidence of T2D after 3-years of follow-up. In addition, early weight loss was especially important in reducing T2D risk among those with fasting glucose (FG) ≥110 mg/dl at 6 months. Further results for glucose and HbA1c were similar across treatment arms with achievement of fasting glucose <100mg/dl or HbA1c <5.7% at 6 months associated with a 62 to 70% T2D risk reduction [17].
Weight loss reduced T2D incidence similarly across all race/ethnicity groups, for both sexes, for all ages, and for several levels of physical activity, regardless of initial BMI. Metformin and the lifestyle intervention were similarly effective in restoring normal fasting glucose values, but the lifestyle intervention was more effective in restoring normal post-load glucose values. The lowest risk was in the ILI subgroup meeting all treatment goals with an HR of 0.11 (95% CI 0.05-0.24; p<0.0001) representing an 89% risk reduction [16]. Table 1 outlines some of the significant benefits from the ILI in the DPP and DPPOS.
Table 1. Benefits from Lifestyle Intervention in Patients with Pre-Diabetes: Lessons Learned from the Diabetes Prevention Program and Outcomes Study.
| Benefit | Comment | KEY Findings | References |
|---|---|---|---|
| Prevent diabetes in those with IGT/IFG | 58% reduction in risk of developing T2D over 3.2 years; 34% after 10 years | Weight Loss was major predictor (1 kg weight loss predicted 16% reduction in risk); increased PA predicted weight loss and helped sustain it; if met all goals risk reduction 89%; more effective in older participants. | 1, 2, 3, 16 |
| Diabetes prevented in a population with previous GDM | Lifestyle intervention and metformin equally effective | Both intensive lifestyle and metformin prevented diabetes by approximately 50% in women with IGT and a history of GDM. Genetics did not change risk. | 25, 26 |
| Cardio metabolic risk factors improved | Blood Pressure and lipids improved and Lifestyle group used fewer medications. | Improved CVD risk factor profiles in all groups (years 3 and 10); blood pressure and lipid medication use was least for lifestyle participants. Incidence of abnormal HDL cholesterol virtually identical by treatment group. Fewer developed diabetes and more reverted to NGT in the ILS group compared with the other two interventions which improved CVD risk. | 30, 31, 32, 33 |
| Prevalence of Metabolic Syndrome (MetS) reduced | MetS risk factors improved in ILI group. | MetS increased in placebo and metformin and decreased in lifestyle at 3 years; Favorable lifestyle-associated changes in WC and HDL-C are associated with diabetes risk reduction. | 35, 36 |
| Subcutaneous fat and visceral fat reduced | Lifestyle intervention reduced subcutaneous and visceral fat. | Lifestyle intervention dramatically reduced visceral fat in both men and women. Reduction of diabetes risk with lifestyle modification was associated with reduction of body size and central adiposity. Reduction of diabetes risk with metformin appeared independent of changes in body size or central adiposity. | 28,29 |
Limitations of the data
Dietary intake and physical activity were assessed by self-report. Although this was a randomized trial, groups who achieved weight loss, diet modification and physical activity were not separately randomized and are difficult to accurately analyze outside the randomization. In the interval between DPP and DPPOS, a “lifestyle” program was offered to all participants, including the original lifestyle group, which was utilized by some participants in each of the randomized groups, which may confound later results.
Predictors of success within the ILI
The DPP quantified the relationship between early measures of weight loss success, glucose, and subsequent T2D. At 6 and 12 months, both change in body weight and glucose strongly predicted lower incidence of T2D in ILI participants. Early success at achieving weight loss predicted later success at maintaining weight loss. Participants who achieved the weight loss goal at the end of the Core Behavioral Curriculum were 3 times more likely to achieve the goal at study end [18]. However when the Core Curriculum was offered again, those individuals in the ILI group were less likely to attend classes and lost less weight than the groups who were naive to this intervention [19].
Changes in physical activity and diet (primarily reduced calorie intake from fat) also predicted weight loss; increased physical activity was associated with a reduced incidence of T2D when there was little weight loss, yielding a 46% reduction for participants who met the physical activity goal adjusted for baseline variables only. Increased physical activity also predicted sustained weight loss and became a stronger predictor with each subsequent year [16].
Achieving weight/activity goals in DPP
Demographic, psychosocial, and behavioral factors relating to achieving body weight loss and physical activity goals were examined in the DPP Lifestyle participants. Forty-nine percent met the weight loss goal and 74% met the activity goal initially, while 37% and 67%, respectively, met the goals long-term at the final intervention visit (mean =3.2 years). Meeting the weight loss goal was predicted by the number of times fat grams were self-monitored (OR= 1.08 per one record increase, p<0.0001 at the end of the core behavioral program; OR = 1.02, p= 0.005 at final visit) and by success at achieving the physical activity goal (OR=1.90, p=0.0001 for end of core; OR=4.11, p<0.0001 at final visit). Participants who achieved the activity goal at the end of the core behavioral curriculum were 1.5 times more likely to achieve the goal at the end of the final intervention visit compared to those who did not initially achieve the activity goal (75% vs. 50%, p<0.001). In univariate analyses, being male, having lower BMI, and being older were significantly associated with success at achieving the activity goal at both the end of the core behavioral curriculum and at the final visit. Ethnicity was significantly related to achieving the activity goal at the final intervention visit, with higher success rates in Hispanic Americans, Asian Americans, and Native Americans [18]. Frequency of monitoring dietary intake was also related to success at achieving the physical activity goal suggesting that adherence to one aspect of the intervention was related to adherence to other aspects [18]. Depression symptoms were assessed by the validated Beck Depression Inventory (BDI) and antidepressant medication use was measured. Psychological and depression measures were unrelated to goal achievement. After adjusting for multiple factors related to weight gain, antidepressant use, not depressive symptoms, was associated with weight regain but not rate of or success of loss or goal achievement [20-22].
Predictors of sustained reduction in energy/fat intake
The DPP ILI group showed reductions in total energy intake for up to 9 years post-randomization [9]. The median self-reported energy intake at baseline was 1,876 kcal/day compared with 1,520 kcal/day at Year 1, a 19% reduction from baseline, with a median fat reduction of 6.6% [8]. A median intake of 1,560 kcal/day was reported at Year 9, suggesting sustained reduction in energy intake, although significant amounts of weight had been regained from the nadir of weight loss. Lower energy and dietary fat intake at baseline predicted lower energy and dietary fat intake at Year 9 [9, 10]. Lower percent of calories from fat also predicted weight loss. Within the ILI group from 1 to 9 years after randomization there was a drop in those reporting use of low-fat foods “often/always” from 40.7% to 12.3% [9]. At baseline, median fat grams intake was 70.4g, which was reduced to 45.2g after Year 1, but then increased to 61.0g by Year 9. The differences in energy intake, fat gram intake and percent energy from fat at baseline and 9 years after randomization was statistically significant (P<0.0001). Although participants increased their energy and fat gram intake between Year 1 and Year 9 of the DPPOS, neither energy nor fat intake returned to baseline levels [10].
Other Effects of Intervention
Effect of Age
The incidence of T2D increases with age and the DPP provided a unique opportunity to learn about the significant age differences in response to either the lifestyle intervention or metformin in preventing T2D. The DPP found that ILI was exceptionally effective in preventing T2D in individuals aged 60-85 years who had the most weight loss and improvement in physical activity. Diabetes incidence rates did not differ by age in the control group, but the ILI was more effective with increasing age [23]. Older age was a strong predictor of success at meeting the weight loss and physical activity goal at both the end of the core curriculum and at the final intervention visit at 3.2 years. The older age group was more likely to complete self-monitoring records and report consuming a lower percentage of calories from fat than younger individuals [18].
Effect of Race/Ethnicity
The DPP was designed to oversample those at high risk of diabetes, and as a result 46.3% reported being of non-white race. Weight loss reduced diabetes incidence similarly across all racial/ethnic groups regardless of the level of initial obesity [16]. Ethnicity was significantly related to achieving the activity goal at the final intervention visit, with higher success rates in Hispanic Americans, Asian Americans, and Native Americans [18]. Participants from ethnic groups disproportionately affected by T2D showed no difference in rates of progression to T2D among the control cohort in comparison with white participants. This finding suggests that ethnic minority populations are at higher risk for the development of IGT but that further progression to T2D may be independent of ethnic risk [24].
Gestational Diabetes Mellitus (GDM)
The DPP recruited 350 women with a history of gestational diabetes mellitus (GDM). This subgroup was younger at study entry, had comparable characteristics, including similar glucose levels and ethnic distribution, to the other women. Women with a history of GDM who were randomized to the control group had a crude incidence rate of T2D that was 71% higher than for women without a history of GDM (25.7% without GDM vs. 38.4% with previous GDM) [25]. Achieving the targeted goals for lifestyle change was far less successful in those with previously reported GDM. ILI participants were less able to sustain the physical activity goals, had a lower maximal weight loss and more rapid weight gain than women in the ILI without GDM. In this cohort, the ILI reduced the incidence of T2D by approximately 50% compared with the control group. These data suggest that metformin may be more effective in preventing T2D than ILI in women with a history of GDM as compared with those without this history. Progression to T2D is more common in women with a history of GDM compared with those without such a history despite equivalent degrees of IGT at baseline. Additionally, genetic risk score was positively associated with a history of GDM, but did not predict progression to T2D or modulate response to the interventions [26].
Effect on Urinary Incontinence
Symptoms of urinary incontinence were assessed in women at the last DPP visit. The ILI participants had lower prevalence of urinary stress incontinence and weight loss was the most important mediator of this effect [27].
Effects on Body Composition
Body composition in the DPP was measured at baseline and 1 year using computed tomography (CT) at 18 of the 27 DPP field sites and included 777 of the 1106 participants who were not diagnosed with T2Ds at 6 months or 1 year and who completed both baseline and follow-up measures. Lifestyle intervention dramatically reduced visceral fat in both men and women, along with a decrease in body weight and BMI. In contrast, metformin had no effect [28, 29].
Effects on Cardio metabolic risk factors
Hypertension was identified in 30% of participants at baseline. The prevalence increased in the metformin and control groups but significantly less so in the ILI participants during the DPP. Both systolic and diastolic blood pressures were lower in the ILI Group (p<0.05) compared to control and metformin groups. At 3 years of follow up, pharmacologic therapy to achieve established goals in the ILI group was 27-28% less for hypertension and 25% less for hyperlipidemia when compared with the metformin or control groups. Dyslipidemia (either LDL-C≥130 mg/dl and/or triglyceride >200 mg/dl) was present in 12% at baseline and increased by approximately 50% in both metformin and control groups during DPP but the prevalence did not increase in the ILI participants. During the three years of the DPP, triglyceride levels fell in all treatment groups, but fell significantly more in the ILI group. Total cholesterol and LDL cholesterol levels were similar among treatment groups. ILI significantly increased HDL cholesterol levels and reduced the cumulative incidence of the pro-atherogenic LDL phenotype B (dense LDL-cholesterol) [30]. CVD risk factors increased as glucose progressed from IGT to T2Ds but improved with reversion to NGT, which was more common for those in the ILI group. Although risk factors deteriorated similarly in all intervention groups among those who developed diabetes, the risk factor profile was more favorable in the ILI group compared to the other 2 groups among those who remained with IGT or regressed to NGT. Since fewer participants in the ILI group progressed to diabetes than the other 2 groups this effect probably contributed to the observation that the ILI group experiences less deterioration of their risk factor profile over time [31]. During the median 10-year follow-up there were major reductions in all groups for systolic and diastolic blood pressures, and for LDL cholesterol and triglycerides. These improvements, however, were achieved in the ILI group with lower medication use [32].
ILI had favorable effects on all lipoprotein classes. Participants in the ILI Group had decreased large t very low-density lipoprotein, small low-density lipoprotein (LDL), and small high-density lipoprotein (HDL) particles and an increase in large HDL particles. ILI treatment had favorable effects on lipoprotein subfractions that are primarily mediated by intervention-related changes in insulin resistance, BMI, and adiponectin. ILS, an intervention that slows diabetes development by leading to favorable lipoprotein changes may also have anti-atherosclerosis effects [33].
Effect on Inflammatory Markers
The beneficial effects of an ILI on concentrations of the inflammatory markers CRP and fibrinogen in adults with IGT was demonstrated at year 1. There was ∼30% reduction in CRP levels in both sexes which appeared to be more closely related to weight loss than an increase in physical activity. Reductions in fibrinogen levels in lifestyle group relative to metformin and control group were seen after one year [34].
Effects on the incidence of Metabolic Syndrome (MetS)
Fifty-Three percent of DPP participants had MetS at baseline using the criteria from the National Cholesterol Education Programs' Adult Treatment Panel III [35]. The ILI group showed a dramatic reduction in the incidence of new cases of MetS and on participants who had MetS at study entry. Analysis of those not meeting the MetS criteria at baseline suggests that ILI reduces the incidence of all components of the MetS except low HDL-C. For those who met the criteria for MetS at baseline, 18% of the control group, 23% of the metformin group, and 38% of the ILI group no longer had MetS at 3 years [35]. MetS and some of its components were associated with increased incidence of T2D in a manner that differed according to DPP intervention. After adjusting for fasting glucoses at baseline, waist circumference (WC), and triglycerides are associated with an increased risk of developing T2D. Favorable ILI associated changes in WC and HDL-C components were associated with T2D risk reduction [36].
Genetics
Genetics studies in DPP participants have examined associations between single nucleotide polymorphisms (SNPs) and ILI treatment-specific responses. The link to these papers for further review is listed at the end of this manuscript.
In one publication, Hivert et al. [37] used a genetic score based on 34 confirmed T2D loci that was associated with risk of diabetes incidence (HR = 1.02 per risk allele [95% CI: 1.00 to 1.05]; p=0.03). There was no significant interaction between the genetic risk score and treatment arms (genetic risk score × ILI interaction p=0.13). This analysis did find that the ILI was effective even in individuals in the highest quartile of genetic risk (p<0.0001). Among individuals in the highest quartile of risk, regression to normal glucose regulation was higher in the ILI arm than the placebo arm (p<0.0001) while there was no difference in regression to normal glucose regulation between the placebo and metformin arms (p=0.062). These results suggest that ILI might be considered the frontline approach to prevent type 2 diabetes, even in individuals with the highest genetic risk and that the genetic burden does not undermine the DPP ILI. Additional genetics research in DPP is identifying variants in individual genes for interaction with treatment for effects on diabetes incidence, weight loss, or weight regain after initial weight loss (see link to DPP papers), with the hope that such findings may eventually have clinical application in selecting optimal interventions for different people.
Cost Effectiveness of Treatment
During the DPP, the lifestyle intervention was cost-saving in participants younger than 45 years of age and was cost-effective even in the oldest age groups. The metformin intervention was cost-effective in participants <65 years of age but was not cost-effective in participants ≥ 65 years of age due to its lack of effectiveness in that age group [38]. The 10-year intent-to-treat and adherence analyses of combined DPP/DPPOS follow-up have shown that, per capita non-intervention related direct medical costs were greater for control participants compared with lifestyle participants by ∼$2,200 and $4,300 respectively and also greater for control participants compared with metformin participants by ∼ $1,600 and $ 3,300 respectively [6, 38, 39].
The Adherence analysis of cumulative undiscounted per participant total direct medical costs of the DPP/DPPOS interventions and medical care received outside the DPP/DPPOS by year 10 were higher for control (∼$28, 200) than DPP group lifestyle (∼26,000) or metformin ($ 27,200). Both interventions were cost saving compared with control. At 10 years, quality-adjusted life years (QALY) accrued as health utility scores were better among adherent lifestyle (6.80) and adherent metformin participants (6.74) than control participants (6.67). With discounting at the rate of 3% per year, the cost-effectiveness of lifestyle compared with control was ∼$20,000 per QALY gained, and the cost of metformin compared with control was ∼$20,100 per QALY gained. Without discounting, from both a modified societal perspective (excluding participant time) and a full societal perspective (including participant time), lifestyle cost <$5000 per QALY gained and metformin was cost saving compared with control. If in a real-world setting a DPP lifestyle intervention could be delivered at a lower cost than they were during the randomized clinical trial using a group based intervention, the DPP interventions are likely to be even more cost effective [39].
The adoption of T2D prevention programs by health plans and society will result in important health benefits over 10 years and represents a good value for the money spent [6]. 10-year within trial analysis shows improved quality-of-life with minimal/no increase in cost. This suggests that treatments should be widely adopted.
Translation
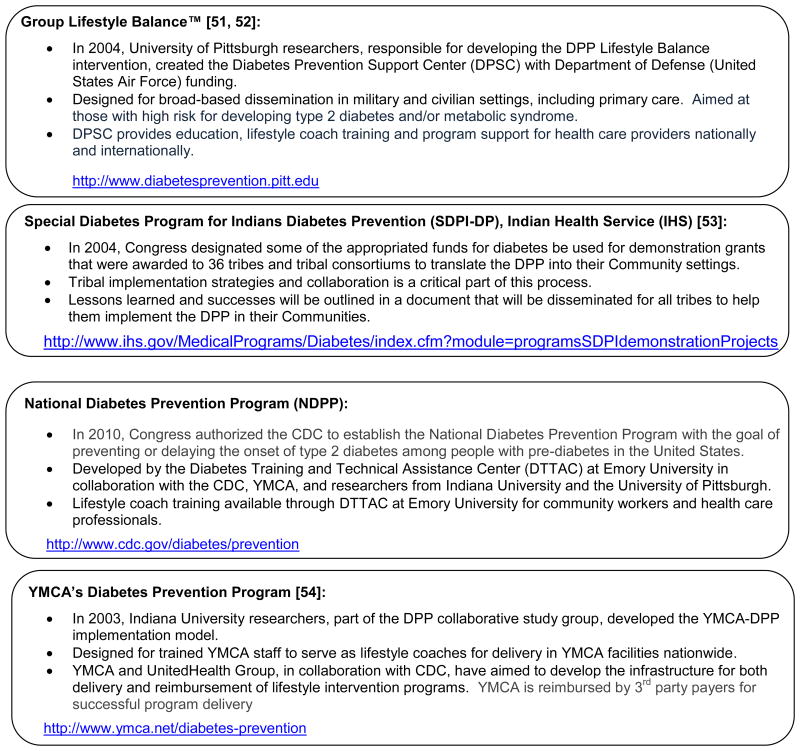
The International Diabetes Federation (IDF) has examined the wide range of community-based interventions in “real world” settings for T2D/chronic disease prevention [40]. The IDF review suggested that individual countries should develop T2D prevention programs, evaluate their cost-effectiveness and develop setting-specific T2D risk identification and prevention strategies based on available resources with the goal of reducing the burden of cardiovascular disease. Systematic reviews and Meta analyses have generally used weight change as a surrogate marker for reduced risk [41-45] to gauge program effectiveness. The Ali et al [41] systematic review and meta-analysis of twenty-eight US-based DPP translation studies found that average 12-month weight loss was about 4% and that weight loss was similar regardless of whether the intervention was delivered by clinically trained professionals or lay educators. The amount of weight loss increased as the number of sessions attended increased. A meta-analysis by Aguiar [42] examined multi-component lifestyle T2D prevention interventions and found that diet and both aerobic and resistance exercise training were modestly effective in achieving weight loss and improving impaired fasting glucose and glucose tolerance. The Dunkley et al [43] meta-analysis of 22 pragmatic real world studies found that greater adherence to guidelines [44,45] related to T2D prevention was associated with a greater weight loss. The Merlotti et al [46] meta-analysis examined the effects of lifestyle and a wide range of medical therapies including bariatric surgery, found that many of the interventions reduced T2D risk making it possible to choose an approach based on the weight and risk status of an individual patients. The systematic review and meta-analysis by Schellenberg et al [47], which addressed the progression from pre-diabetes to overt T2D and to clinical outcomes (such as cardiovascular disease and death) in overt T2D, found that lifestyle interventions effectively decrease the incidence of T2D but did not reduce all-cause mortality or cardiovascular and microvascular outcomes. Yuen [48] concluded that both intensive lifestyle change programs and medications delay progression from prediabetes to overt T2D, but both have issues with adherence and side effects that should guide practice decisions about their use. The systematic review and meta-analysis by Whittemore [49] examined delivery of the lifestyle intervention in four distinct settings: (a) hospital outpatient, (b) primary care, (c) community, and (d) work and church and compared settings' variability with regard to RE-AIM (reach, efficacy, adoption, implementation, and maintenance noting the strengths and limitations to each setting). When comparing these settings, they found that community, work and church settings have a greater potential to reach people who are not in the health care system, but risk and efficacy assessment are more likely to be based on weight in sites where obtaining blood tests may not be practical. Whittemore noted that using the RE-AIM framework could help standardize evaluation and facilitate comparisons of studies and Ruggerio [50] reviewed the evidence for a role of community health workers in translation efforts. The model that of group class delivery and coaching used during the DPP “Bridge” program [38] is widely used. Figure 1 lists some of the resources available and the ongoing translation efforts [51-54].
Figure 1. Components of the major DPP Translation Curricula current available*.
*Each program has adapted the original DPP Lifestyle Balance curriculum (http://www.bsc.gwu.edu/dpp/manuals.htmlvdoc) to a 12-month, group-based program with goals consistent with DPP; 7% weight loss and at least 150 minutes per week of physical activity.
The above curricula are CDC-approved for application to a Diabetes Prevention Recognition Program (DPRP) that recognizes organizations with demonstrated effective delivery of a lifestyle intervention program to prevent type 2 diabetes. http://www.cdc.gov/diabetes/prevention/recognition/index.htm.
An additional resource for implementation of the principles of the DPP curriculum primarily for use in clinical settings, Small Steps. Big Rewards; Your GAME PLAN to Prevent Type 2 Diabetes Health Care Provider Toolkit, is available through the National Diabetes Education Program (NDEP) at http://1.usa.gov/1jtLGug.
Conclusions
The DPP/ DPPOS landmark study showed a clear effect of ILI on preventing or delaying the development of diabetes and associated risks in as short as 3.2 years, with effects that have persisted for up to 10 years. These efforts are cost effective and are being widely translated. The potential effects on health, quality of life and the costs of health care worldwide should prove to be significant. All the papers published by the DPP and DPPOS research group can be found on https://dppos.bsc.gwu.edu/web/dppos/publications.
Acknowledgments
The Research Group gratefully acknowledges the commitment and dedication of the participants of the DPP and DPPOS. During the DPPOS, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health provided funding to the clinical centers and the Coordinating Center for the design and conduct of the study, and collection, management, analysis, and interpretation of the data. The Southwestern American Indian Centers were supported directly by the NIDDK, including its Intramural Research Program, and the Indian Health Service. The General Clinical Research Center Program, National Center for Research Resources, and the Department of Veterans Affairs supported data collection at many of the clinical centers. Funding was also provided by the National Institute of Child Health and Human Development, the National Institute on Aging, the National Eye Institute, the National Heart Lung and Blood Institute, the Office of Research on Women's Health, the National Institute on Minority Health and Health Disparities, the Centers for Disease Control and Prevention, and the American Diabetes Association. Bristol-Myers Squibb and Parke-Davis provided additional funding and material support during the DPP, Lipha (Merck-Sante) provided medication and LifeScan Inc. donated materials during the DPP and DPPOS. The opinions expressed are those of the investigators and do not necessarily reflect the views of the funding agencies. A complete list of Centers, investigators, and staff can be found in the Appendix.
Members of the DPP Research Group are listed the Appendix
Pennington Biomedical Research Center (Baton Rouge, LA)
George A. Bray, MD*
Annie Chatellier, RN, CCRC**
Crystal Duncan, LPN
Frank L. Greenway, MD
Erma Levy, RD
Donna H. Ryan, MD
University of Chicago (Chicago, IL)
David Ehrmann, MD*
Margaret J. Matulik, RN, BSN**
Kirsten Czech, MS
Catherine DeSandre, BA
Jefferson Medical College (Philadelphia, PA)
Barry J. Goldstein, MD, PhD*
Kevin Furlong, DO*
Kellie A. Smith, RN, MSN**
Wendi Wildman, RN**
Constance Pepe, MS, RD
University of Miami (Miami, FL)
Ronald B. Goldberg, MD*
Jeanette Calles, MSEd**
Juliet Ojito, RN**
Sumaya Castillo-Florez, MPH
Hermes J. Florez, MD, PhD
Anna Giannella, RD, MS
Olga Lara
Beth Veciana
The University of Texas Health Science Center (San Antonio, TX)
Steven M. Haffner, MD, MPH*
Helen P. Hazuda, PhD*
Maria G. Montez, RN, MSHP, CDE**
Carlos Lorenzo, MD, PhD
Arlene Martinez, RN, BSN, CDE
University of Colorado (Denver, CO)
Richard F. Hamman, MD, DrPH*
Dana Dabelea, MD, PhD*
Lisa Testaverde, MS**
Alexis Bouffard, MA, RN, BSN
Tonya Jenkins, RD, CDE
Dione Lenz, RN, BSN, CDE
Leigh Perreault, MD
David W. Price, MD
Sheila C. Steinke, MS
Joslin Diabetes Center (Boston, MA)
Edward S. Horton, MD*
Catherine S. Poirier, RN, BSN**
Kati Swift, RN, BSN**
Enrique Caballero, MD
Barbara Fargnoli, RD
Ashley Guidi, BS
Mathew Guido, BA
Sharon D. Jackson, MS, RD, CDE
Lori Lambert, MS, RD, LD
Kathleen E. Lawton, RN
Sarah Ledbury, Med, RD
Jessica Sansoucy, BS
Jeanne Spellman, RD
VA Puget Sound Health Care System and University of Washington (Seattle, WA)
Steven E. Kahn, MB, ChB*
Brenda K. Montgomery, RN, BSN, CDE**
Wilfred Fujimoto, MD
Robert H. Knopp, MD (deceased)
Edward W. Lipkin, MD
Anne Murillo, BS
Dace Trence, MD
University of Tennessee (Memphis, TN)
Abbas E. Kitabchi, PhD, MD, FACP*
Mary E. Murphy, RN, MS, CDE, MBA**
William B. Applegate, MD, MPH
Michael Bryer-Ash, MD
Samuel Dagogo-Jack, MD, MSc, FRCP, FACP
Sandra L. Frieson, RN
Helen Lambeth, RN, BSN
Lynne C. Lichtermann, RN, BSN
Hooman Otkaei, MD
Lily M.K. Rutledge, RN, BSN
Amy R. Sherman, RD, LD
Clara M. Smith, RD, MHP, LDN
Judith E. Soberman, MD
Beverly Williams-Cleaves, MD
Northwestern University's Feinberg School of Medicine (Chicago, IL)
Boyd E. Metzger, MD*
Mark E. Molitch, MD*
Mariana K. Johnson, MS, RN**
Mimi M.Giles, MS, RD
Diane Larsen, BS
Charlotte Niznik, MS, RN, CDE
Samsam C. Pen, BA
Pamela A. Schinleber, RN, MS
Massachusetts General Hospital (Boston, MA)
David M. Nathan, MD*
Mary Larkin, MSN*
Charles McKitrick, BSN**
Heather Turgeon, BSN
Ellen Anderson, MS, RD
Laurie Bissett, MS, RD
Kristy Bondi, BS
Enrico Cagliero, MD
Kali D'Anna
Linda Delahanty, MS, RD
Jose C. Florez, MD, PhD
Valerie Goldman, MS, RD
Alexandra Poulos
Elyse Raymond, BS
Christine Stevens, RN
Beverly Tseng
University of California-San Diego (San Diego, CA)
Elizabeth Barrett-Connor, MD*
Mary Lou Carrion-Petersen, RN, BSN**
Lauren N. Claravall, BS
Jonalle M. Dowden, BS
Javiva Home, RD
Diana Leos, RN, BSN
Sundar Mudaliar, MD
Jean Smith, RN
Simona Szerdi Janisch, BS
Karen Vejvoda, RN, BSN, CDE, CCRC
St. Luke's-Roosevelt Hospital (New York, NY)
F. Xavier Pi-Sunyer, MD*
Jane E. Lee, MS**
Sandra T. Foo, MD
Susan Hagamen, MS, RN, CDE
Indiana University (Indianapolis, IN)
David G. Marrero, PhD*
Susie M. Kelly, RN, CDE**
Ronald T. Ackermann, MD
Edwin S. Fineberg, MD
Angela Hadden
Marcia A. Jackson
Marion S. Kirkman, MD
Kieren J. Mather, MD
Paris J. Roach, MD
Madelyn L. Wheeler, RD
Medstar Research Institute (Washington, DC)
Robert E. Ratner, MD*
Vanita Aroda, MD*
Sue Shapiro, RN, BSN, CCRC**
Catherine Bavido-Arrage, MS, RD, LD
Lilia Leon
Gabriel Uwaifo, MD
Debra Wells-Thayer, NP, CDE
Renee Wiggins, RD
University of Southern California/UCLA Research Center (Alhambra, CA)
Mohammed F. Saad, MD*
Karol Watson, MD*
Medhat Botrous, MD**
Sujata Jinagouda, MD**
Maria Budget
Claudia Conzues
Perpetua Magpuri
Kathy Ngo
Kathy Xapthalamous
Washington University (St. Louis, MO)
Neil H.White, MD, CDE*
Samia Das, MS, MBA, RD, LD**
Ana Santiago, RD
Angela L. Brown, MD
Cormarie Wernimont, RD, LD
Johns Hopkins School of Medicine (Baltimore, MD)
Christopher D. Saudek, MD* (deceased)
Sherita Hill Golden, MD, MHS, FAHA*
Tracy Whittington, BS**
Jeanne M. Clark, MD
Alicia Greene
Dawn Jiggetts
Henry Mosley
John Reusing
Richard R. Rubin, PhD (deceased)
Shawne Stephens
Evonne Utsey
University of New Mexico (Albuquerque, NM)
David S. Schade, MD*
Karwyn S. Adams, RN, MSN**
Claire Hemphill, RN, BSN**
Penny Hyde, RN, BSN**
Janene L. Canady, RN, BSN, CDE
Kathleen Colleran, MD
Ysela Gonzales
Doris A. Hernandez-McGinnis
Carolyn King, MEd
Albert Einstein College of Medicine (Bronx, NY)
Jill Crandall, MD*
Janet O. Brown, RN, MPH, MSN**
Elsie Adorno, BS
Helena Duffy, MS, C-ANP
Angela Goldstein, FNP-C, NPP, CSW
Jennifer Lukin, BA
Helen Martinez, RN, MSN, FNP-C
Dorothy Pompi, BA
Harry Shamoon, MD
Jonathan Scheindlin, MD
Elizabeth A. Walker, RN, DNSc, CDE
Judith Wylie-Rosett, EdD, RD
University of Pittsburgh (Pittsburgh, PA)
Trevor Orchard, MD*
Andrea Kriska, PhD*
Susan Jeffries, RN, MSN**
M. Kaye Kramer, BSN, MPH**
Marie Smith, RN, BSN**
Catherine Benchoff
Stephanie Guimond, BS
Jessica Pettigrew, CMA
Debra Rubinstein, MD
Linda Semler, MS, RD
Elizabeth Venditti, PhD
Valarie Weinzierl, MPH
University of Hawaii (Honolulu, HI)
Richard F. Arakaki, MD*
Narleen K. Baker-Ladao, BS**
Mae K. Isonaga, RD, MPH**
Nina E. Bermudez, MS
Marjorie K. Mau, MD
Southwest American Indian Centers (Phoenix, AZ; Shiprock, NM; Zuni, NM)
William C. Knowler, MD, DrPH*
Norman Cooeyate**
Mary A. Hoskin, RD, MS**
Camille Natewa**
Carol A. Percy, RN, MS**
Kelly J. Acton, MD, MPH
Vickie L Andre, RN, FNP
Shandiin Begay, MPH
Brian C. Bucca, OD, FAAO
Sherron Cook
Matthew S. Doughty, MD
Justin Glass, MD
Martia Glass, MD
Robert L. Hanson, MD, MPH
Doug Hassenpflug, OD
Louise E. Ingraham, MS, RD, LN
Kathleen M. Kobus, RNC-ANP
Jonathan Krakoff, MD
Catherine Manus, LPN
Cherie McCabe
Sara Michaels, MD
Tina Morgan
Julie A. Nelson, RD
Robert J. Roy
Miranda Smart
Darryl P. Tonemah, PhD
Charlton Wilson, MD
George Washington University Biostatistics Center (DPP Coordinating Center Rockville, MD)
Sarah Fowler, PhD*
Marinella Temprosa, PhD*
Michael D. Larsen, PhD*
Tina Brenneman**
Hanna Sherif, MS**
Sharon L. Edelstein, ScM**
Solome Abebe, MS
Julie Bamdad, MS
Melanie Barkalow
Joel Bethepu
Tsedenia Bezabeh
Jackie Callaghan
Costas Christophi, PhD
Nicole Butler
Mary Foulkes, PhD
Yuping Gao
Robert Gooding
Adrienne Gottlieb
Nisha Grover
Heather Hoffman, PhD
Kathleen Jablonski, PhD
Richard Katz, MD
Preethy Kolinjivadi, MS
John M. Lachin, ScD
Yong Ma, PhD
Qing Pan, PhD
Susan Reamer
Alla Sapozhnikova
Lifestyle Resource Core
Elizabeth M. Venditti, PhD*
Andrea M. Kriska, PhD
Linda Semler, MS, RD
Valarie Weinzierl, MPH
Central Biochemistry Laboratory (Seattle, WA)
Santica Marcovina, PhD, ScD*
Greg Strylewicz, PhD**
John Albers, PhD
Epidemiological Cardiology Research Center- Epicare (Winston-Salem, NC)
Ronald J. Prineas, MD, PhD*
Teresa Alexander
Charles Campbell, MS
Sharon Hall
Susan Hensley
Yabing Li, MD
Margaret Mills
Elsayed Soliman, MD
Zhuming Zhang, MD
Fundus Photo Reading Center (Madison, Wl)
Ronald Danis, MD*
Matthew Davis, MD*
Larry Hubbard*
Ryan Endres**
Deborah Elsas**
Samantha Johnson**
Vonnie Gama
Anne Goulding
Carotid Ultrasound
Gregory Evans
CT Scan Reading Center
Elizabeth Stamm
Neurocognitive Assessment Group
Jose A. Luchsinger, MD, MPH
NIH/NIDDK (Bethesda, MD)
Judith Fradkin, MD
Sanford Garfield, PhD
Centers for Disease Control & Prevention (Atlanta, GA)
Edward Gregg, PhD
Ping Zhang, PhD
University of Michigan (Ann Arbor, Ml)
William H. Herman, MD, MPH
Morton B. Brown, PhD
Nutrition Coding Center (Columbia, SC)
Elizabeth Mayer-Davis, PhD*
Robert R. Moran, PhD**
Quality of Weil-Being Center (La Jolla, CA)
Ted Ganiats, MD*
Andrew J. Sarkin, PhD**
Naomi Katzir
Erik Groessl, PhD
Coronary Artery Calcification Reading Center
Matthew Budoff, MD
Chris Dailing
Genetics Working Group
Jose C. Florez, MD, PhD1, 2
David Altshuler, MD, PhD1, 2
Liana K. Billings, MD1
Ling Chen, MS1
Maegan Harden, BS2
Robert L. Hanson, MD, MPH3
William C. Knowler, MD, DrPH3
Toni I. Pollin, PhD4
Alan R. Shuldiner, MD4
Kathleen Jablonski, PhD5
Paul W. Franks, PhD, MPhil, MS6, 7, 8
Marie-France Hivert, MD9
1=Massachusetts General Hospital
2=Broad Institute
3=NIDDK
4=University of Maryland
5=Coordinating Center
6=Lund University, Sweden
7=Umeå University, Sweden
8=Harvard School of Public Health
9=Université de Sherbrooke
Footnotes
Compliance with Ethics Guidelines: Conflict of Interest: Mary A. Hoskin declares that she has no conflict of interest.
George A. Bray has received research support through a grant from the NIH National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); has received compensation from Herbalife Nutrition Institute, Jason Pharmaceuticals, and Theracos Pharmaceuticals for service as a consultant; has received payment for lectures including service on speakers bureaus from the American Association of Clinical Endocrinologists; and has received royalties from contributions to the Handbook of Obesity, Up-to-Date, and CRC Press.
Kathy Hattaway declares that she has no conflict of interest.
Prajakta A. Khare-Ranade has received research support through a grant from the NIH National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) for DPPOS.
Jeremy Pomeroy has received research support through a grant from the NIH National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Linda N. Semler has been issued a patent for the Group Lifestyle Balance™ program, but has disclaimed rights to licensing proceeds and has no personal financial interest in the licensing for the program.
Valarie A. Weinzierl declares that she has no conflict of interest.
Judith Wylie-Rosett has received research support through a grant from the NIH National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Human and Animal Rights and Informed Consent: This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published in the last three years, have been highlighted as:
*Of importance
**Of major importance
- 1.Crandall JP, Knowler WC, Kahn SE, Marrero D, Florez JC, Bray GA, Haffner SM, Hoskin M, Nathan DM Diabetes Prevention Program Research Group. The prevention of type 2 diabetes. Nat Clin Pract Endocrinol Metab. 2008;4(7):382–393. doi: 10.1038/ncpendmet0843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diabetes Prevention Program Research Group. Knowler WC, Fowler SE, Hamman RF, Christophi CA, Haffman HJ, Brenneman AT, Brown-Friday JO, Goldberg R, Venditti E, Nathan DM. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;14(374):1677–1686. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1999;22(4):623–634. doi: 10.2337/diacare.22.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6**.The Diabetes Prevention Program Research Group. The 10-year cost-effectiveness of lifestyle intervention or metformin for diabetes prevention: an intent-to-treat analysis of the DPP/DPPOS. Diabetes Care. 2012;35(4):723–730. doi: 10.2337/dc11-1468. The DPP and its Outcomes study demonstrated that both ILI and metformin could prevent diabetes in those at high risk for at least 10 years post-randomization and this investment provides good value for funds invested in prevention. These data are important for building meaningful translation of diabetes prevention strategies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 1997;20:1183–97. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 8.Mayer-Davis EJ, Sparks KC, Hirst K, et al. Dietary intake in the diabetes prevention program cohort: Baseline and 1 year post randomization. Ann Epidemol. 2004;14(10):763–772. doi: 10.1016/j.annepidem.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 9**.Jaacks LM, Ma Y, Davis N, Delahanty LM, Mayer-Davis EJ, Franks PW, Brown-Friday J, Isonaga M, Kriska AM, Venditti EM, Wylie-Rosett J for the Diabetes Prevention Program Research Group. Long-term changes in dietary intake and food behaviors in the Diabetes Prevention Program Outcomes Study. Diabetic Medicine. 2014 May 13; doi: 10.1111/dme.12500. [Epub ahead of print]. This analysis was of long term changes in food intake and diet-related behaviors in the DPP. Significant differences remained between randomized groups up to 9 years. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10**.Davis NJ, Ma Y, Delahanty LM, Hoffman HJ, Mayer-Davis E, Franks PW, Brown-Friday J, Isonaga M, Kriska AM, Venditti EM, Wylie-Rosett J for the Diabetes Prevention Program Research Group. Predictors of sustained reduction in energy and fat intake in the Diabetes Prevention Program Outcomes Study intensive lifestyle intervention. Journal Of The Academy Of Nutrition And Dietetics. 2013;113(11):1455–1464. doi: 10.1016/j.jand.2013.07.003. The DPP's Intensive Lifestyle Intervention resulted in reductions of total energy intake for up to 9 years. Initial success at goal achievement predicted long-term success at maintaining changes achieved. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kriska AM, Edelstein SL, Hamman RF, Otto A, Bray GA, Mayer-Davis EJ, Wing RR, Horton ES, Haffner SM, Regensteiner JG. Physical activity in individuals at risk for diabetes: Diabetes Prevention Program. Med Sci Sports Exerc. 2006;38(5):826–832. doi: 10.1249/01.mss.0000218138.91812.f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Delahanty L, Begay S, Cooeyate N, Hoskin M, Isonaga M, Levy E, Mikami K, Odom S, Szamos K. The effectiveness of Lifestyle Intervention in the Diabetes Prevention Program: Application in Diverse Ethnic Groups. On the Cutting Edge. 2002;23(6):30–36. http://www.dce.org/publications/on-the-cutting-edge/#order-form. [Google Scholar]
- 13.Hoskin M, Begay S, Bolin P, Hermes J, Ingraham L, Killean T, Nelson J, Percy C, Scurlock N, Shovestull LE, Tomchee C the Diabetes Prevention Program and Action for Health in Diabetes (Look AHEAD) research groups. Providing lifestyle interventions in American Indian communities. Obesity Management Journal. 2005;1(6):251–255. [Google Scholar]
- 14.Wylie-Rosett J, Delahanty L. An integral role of the dietitian: Implications of the Diabetes Prevention Program. Journal Of The American Dietetic Association. 2002;102(8):1065–1068. doi: 10.1016/s0002-8223(02)90241-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15**.Venditti E, Wylie-Rosett J, Delahanty L, Mele L, Hoskin M, Edelstein S for the Diabetes Prevention Program Research Group. Short and long-term lifestyle coaching approaches used to address diverse participant barriers to weight loss and physical activity adherence. International Journal Of Behavioral Nutrition And Physical Activity. 2014;11(1):16. doi: 10.1186/1479-5868-11-16. The coaching approaches that were critical to the success of the DPP Intensive Lifestyle Intervention are analyzed and reviewed here. This is a critical piece to the implementation of the highly effective intervention. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, Hoskin M, Kriska AM, Mayer-Davis EJ, Pi-Sunyer X, Regensteiner J, Venditti B, Wylie-Rosett J. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29(9):2102–2107. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17*.Maruthur NM, Ma Y, Delahanty LM, Nelson JA, Aroda V, White NH, Marrero D, Brancati FL, Clark JM for the Diabetes Prevention Program Research Group. Early Response to Preventive Strategies in the Diabetes Prevention Program. Journal Of General Internal Medicine. 2013;28(12):1629–1636. doi: 10.1007/s11606-013-2548-4. These researchers looked at what predicts reduced diabetes risk; weight and glucose at 6 and 12 months. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wing RR, Hamman RF, Bray GA, Delahanty L, Edelstein SL, Hill JO, Horton ES, Hoskin MA, Kriska A, Lachin J, Mayer-Davis EJ, Pi-Sunyer X, Regensteiner JG, Venditti B, Wylie-Rosett J. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes Res. 2004;12(9):1426–1434. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Venditti EM, Bray GA, Carrion-Petersen ML, Delahanty LM, Edelstein SL, Hamman RF, Hoskin MA, Knowler WC, Ma Y for the Diabetes Prevention Program Research Group. First versus repeat treatment with a lifestyle intervention program: attendance and weight loss outcome. Int J Obes (Lond) 2008;32(10):1537–1544. doi: 10.1038/ijo.2008.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Price DW, Ma Y, Rubin RR, Perreault L, Bray GA, Marrero D, Knowler WC, Barrett-Connor E, Lacoursiere DY for the Diabetes Prevention Program Research Group. Depression as a Predictor of Weight Regain Among Successful Weight Losers in the Diabetes Prevention Program. Diabetes Care. 2013;36(2):216–221. doi: 10.2337/dc12-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rubin RR, Ma Y, Peyrot M, Marrero DG, Price DW, Barrett-Connor E, Knowler WC for the Diabetes Prevention Program Research Group. Antidepressant medicine use and risk of developing diabetes during the diabetes prevention program and diabetes prevention program outcomes study. Diabetes Care. 2010;33(12):2549–2551. doi: 10.2337/dc10-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rubin RR, Knowler WC, Ma Y, Marrero DG, Edelstein SL, Walker EA, Garfield SA, Fisher EB for the Diabetes Prevention Program Research Group. Depression symptoms and antidepressant medicine use in Diabetes Prevention Program participants. Diabetes Care. 2005;28(4):830–837. doi: 10.2337/diacare.28.4.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diabetes Prevention Program Research Group. Crandall J, Schade D, Ma Y, Fujimoto WY, Barrett-Connor E, Fowler S, Dagogo-Jack S, Andres R. The influence of age on the effects of lifestyle modification and metformin in prevention of diabetes. J Gerontol A Biol Sci Med Sci. 2006;61(10):1075–1081. doi: 10.1093/gerona/61.10.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ratner R Diabetes Prevention Program Research Group. An Update on the Diabetes Prevention Program. Endocrine Practice. 2006;12(Suppl 1):20–24. doi: 10.4158/EP.12.S1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ratner RE, Chitson PA, Metzger BE, Dabelea D, Bennett PH, Pi-Sunyer X, Fowler S, Kahn SE for the Diabetes Prevention Program Research Group. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008;93(12):4774–4779. doi: 10.1210/jc.2008-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26**.Sullivan SD, Jablonski KA, Florez JC, Dabelea D, Franks PW, Dagogo-Jack S, Kim C, Knowler WC, Christophi CA, Ratner R for the Diabetes Prevention Program Research Group. Genetic Risk of Progression to Type 2 Diabetes and Response to Intensive Lifestyle or Metformin in Prediabetic Women With and Without a History of Gestational Diabetes. Diabetes Care. 2014;37(4):909–911. doi: 10.2337/dc13-0700. These data suggest that diabetes-associated GRS is associated with the development of GDM due to reduced beta cell function but did not predict progression to diabetes or modulate the response to the interventions. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown JS, Wing R, Barrett-Connor E, Nyberg LM, Kusek JW, Orchard TJ, Ma Y, Vittinghoff E, Kanaya AM for the Diabetes Prevention Program Research Group. Lifestyle intervention is associated with lower prevalence of urinary incontinence: the Diabetes Prevention Program. Diabetes Care. 2006;29(2):385–90. doi: 10.2337/diacare.29.02.06.dc05-1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bray GA, Fujimoto W, Jablonski K, Barrett-Connor E, Haffner S, Hubbard V, Stamm E, Pi-Sunyer XP Diabetes Prevention Program Research Group. Relationship of body size and shape to the development of diabetes in the Diabetes Prevention Program. Obesity (Silver Spring) 2006;14(11):2107–2117. doi: 10.1038/oby.2006.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fujimoto WY, Jablonski KA, Bray GA, Kriska A, Barrett-Connor E, Haffner S, Hanson R, Hill JO, Hubbard V, Stamm E, Pi-Sunyer FX. Body size and shape changes and the risk of diabetes in the Diabetes Prevention Program. Diabetes. 2007;56(6):1680–1685. doi: 10.2337/db07-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ratner R, Goldberg R, Haffner S, Marcovina S, Orchard T, Fowler S, Temprosa M Diabetes Prevention Program Research Group. Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the Diabetes Prevention Program. Diabetes Care. 2005;28(4):888–894. doi: 10.2337/diacare.28.4.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goldberg RB, Temprosa M, Haffner S, Orchard TJ, Ratner RE, Fowler SE, Mather K, Marcovina S, Saudek C, Matulik MJ, Price D Diabetes Prevention Program Research Group. Effect of progression from impaired glucose tolerance to diabetes on cardiovascular risk factors and its amelioration by lifestyle and metformin intervention: for the Diabetes Prevention Program randomized trial by the Diabetes Prevention Program Research Group. Diabetes Care. 2009;32(4):726–732. doi: 10.2337/dc08-0494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32**.Orchard TJ, Temprosa M, Barrett-Connor E, Fowler S, Goldberg R, Mather K, Marcovina S, Montez M, Ratner R, Saudek C, Sherif H, Watson K for the Diabetes Prevention Program Outcomes Study Research Group. Long term effects of the Diabetes Prevention Program's interventions on cardiovascular risk factors: a report from the DPP Outcomes Study. Diabetic Medicine. 2013;30(1):46–55. doi: 10.1111/j.1464-5491.2012.03750.x. CVD risk reduction is important to evaluate when looking at methods to prevent diabetes. In the DPP and DPPOS, the Intensive Lifestyle Intervention achieved, with fewer medications, a comparable CVD risk reduction as the other treatment groups. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goldberg RB, Temprosa M, Otvos J, Brunzell J, Marcovina SM, Mather KJ, Arakaki RF, Watson KE, Horton ES, Barrett-Connor E. Lifestyle and metformin treatment favorably influence lipoprotein sub-fraction distribution in the Diabetes Prevention Program. The Journal Of Clinical Endocrinology & Metabolism. 2013;98(10):3989–3998. doi: 10.1210/jc.2013-1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haffner S, Temprosa M, Crandall J, Fowler S, Goldberg R, Horton E, Marcovina S, Mather K, Orchard T, Ratner R, Barrett-Connor E for the Diabetes Prevention Program Research Group. Intensive lifestyle intervention or metformin on inflammation and coagulation in participants with impaired glucose tolerance. Diabetes. 2005;54(5):1566–1572. doi: 10.2337/diabetes.54.5.1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Orchard TJ, Temprosa M, Goldberg R, Haffner S, Ratner R, Marcovina S, Fowler SE for the Diabetes Prevention Program Research Group. The effect of metformin and intensive lifestyle intervention on the metabolic syndrome: the Diabetes Prevention Program randomized trial. Ann Intern Med. 2005;142(8):611–619. doi: 10.7326/0003-4819-142-8-200504190-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36**.Florez H, Temprosa MG, Orchard TJ, Mather KJ, Marcovina SM, Barrett-Connor E, Horton E, Saudek C, Pi-Sunyer XF, Ratner RE, Goldberg RB. Metabolic Syndrome Components and Their Response to Lifestyle and Metformin Interventions are Associated with Differences in Diabetes Risk in Persons with Impaired Glucose Tolerance. Diabetes, Obesity, And Metabolism. 2013;16(4):326–333. doi: 10.1111/dom.12220. The researchers associated MetS and its components with diabetes risk in DPP participants, all of whom had IGT at baseline. They then assessed the intervention-related changes in the components of MetS and their correlations with the development of T2D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hivert MF, Jablonski KA, Perreault L, Saxena R, McAteer JB, Franks PW, et al. Updated Genetic Score Based on 34 Confirmed Type 2 Diabetes Loci Is Associated With Diabetes Incidence and Regression to Normoglycemia in the Diabetes Prevention Program. Diabetes. 2011;60:1340–8. doi: 10.2337/db10-1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Herman WH, Hoerger TJ, Brandle M, et al. Diabetes Prevention Program Research Group. The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann Intern Med. 2005;142(5):323–332. doi: 10.7326/0003-4819-142-5-200503010-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39**.Herman WH, Edelstein SL, Ratner RE, et al. The Diabetes Prevention Program Research Group. Effectiveness and Cost – Effectiveness of Diabetes Prevention Among Adherent Participants. Am J Manag Care. 2013;19(3):194–202. The analysis of cost-effectiveness of the DPP and DPPOS treatment groups for those participants who were adherent to the treatments revealed that the treatments were cost saving or cost effective compared with placebo. Costs for individual and group classes were analyzed. These treatments to prevent diabetes represent a good value for the cost. [PMC free article] [PubMed] [Google Scholar]
- 40.Simmons RK, Unwin N, Griffin SJ. International Diabetes Federation: An update of the evidence concerning the prevention of type 2 diabetes. Diabetes Res Clin Pract. 2010 Feb;87(2):143–149. doi: 10.1016/j.diabres.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 41*.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the diabetes prevention program? Health affairs. 2012;31:67–75. doi: 10.1377/hlthaff.2011.1009. They evaluated the effectiveness of 28 US-based studies applying the DPP ILI for people at high risk of T2D. Change in weight was about 4% of initial body weight and these results were similar in programs that delivered the intervention utilizing clinically trained professionals or lay educators. [DOI] [PubMed] [Google Scholar]
- 42*.Aguiar EJ, Morgan PJ, Collins CE, Plotnikoff RC, Callister R. Efficacy of interventions that include diet, aerobic and resistance training components for type 2 diabetes prevention: A systematic review with meta-analysis. The International Journal of Behavioral Nutrition and Physical Activity. 2014;11:2. doi: 10.1186/1479-5868-11-2. These authors evaluated the efficacy and effectiveness of interventions that include diet, with both aerobic and resistance training, in behavioral weight loss programs designed to prevent diabetes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43*.Dunkley AJ, Bodicoat DH, Greaves CJ, Russell C, Yates T, Davies MJ, Khunti K. Diabetes prevention in the real world: Effectiveness of pragmatic lifestyle interventions for the prevention of type 2 diabetes and of the impact of adherence to guideline recommendations: A systematic review and meta-analysis. Diabetes Care. 2014;37:922–933. doi: 10.2337/dc13-2195. A meta-analysis of 22 studies detailing the success of the translation the studies they reviewed. These programs were effective at achieving weight loss, with greater adherence to guidelines resulting in significantly greater weight loss. [DOI] [PubMed] [Google Scholar]
- 44.Paulweber B, Valensi P, Lindström J, et al. A European evidence-based guideline for the prevention of type 2 diabetes. Horm Metab Res. 2010;42(Suppl. 1):S3–S36. doi: 10.1055/s-0029-1240928. 50. [DOI] [PubMed] [Google Scholar]
- 45.National Institute for Health and Clinical Excellence. Preventing Type 2 Diabetes: Risk Identification and Interventions for Individuals at High Risk. London: National Institute for Health and Clinical Excellence; 2012. [Google Scholar]
- 46*.Merlotti C1, Morabito A, Pontiroli AE. Prevention of type 2 diabetes; a systematic review and meta-analysis of different intervention strategies. Diabetes Obes Metab. 2014 Feb 27; doi: 10.1111/dom.12270. This review looked at interventions that used 15 different strategies to prevent T2D. Age of subject and amount of weight lost was related to the effectiveness of the interventions. [DOI] [PubMed] [Google Scholar]
- 47*.Sumamo Schellenberg E, Dryden DM, Vandermeer B, Ha C, Korownyk C. Lifestyle Interventions for Patients With and at Risk for Type 2 Diabetes: A Systematic Review and Meta-analysis. Ann Intern Med. 2013;159(8):543–551. doi: 10.7326/0003-4819-159-8-201310150-00007. Randomized clinical trials were identified that were of at least 3 months duration, included diet and exercise and at least one other component aimed at preventing T2D. Seven studies reported that lifestyle interventions decreased the risk for diabetes from the end of intervention up to 10 years after it. They concluded that comprehensive lifestyle interventions that include these components are effective in decreasing incidence of T2D in high risk patients and the benefit extends beyond the active intervention phase. [DOI] [PubMed] [Google Scholar]
- 48.Yuen A, Sugeng Y, Weiland TJ, Jelani GA. Lifestyle and medication interventions for the prevention or delay of type 2 diabetes mellitus in prediabetes: a systematic review of randomised controlled trials. Aust N Z J Public Health. 2010 Apr;34(2):172–178. doi: 10.1111/j.1753-6405.2010.00503.x. [DOI] [PubMed] [Google Scholar]
- 49.Whittemore R. A systematic review of the translational research on the Diabetes Prevention Program. Transl Behav Med. 2011 Sep;1(3):480–491. doi: 10.1007/s13142-011-0062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50*.Ruggiero L, Castillo A, Quinn L, Hochwert M. Translation of the diabetes prevention program's lifestyle intervention: role of community health workers. Curr Diab Rep. 2012 Apr;12(2):127–137. doi: 10.1007/s11892-012-0254-y. Many underserved communities affected by high rates of T2D have access to a health system that include Community Health Workers. This article provides an overview of studies involving these workers in prevention of T2D. [DOI] [PubMed] [Google Scholar]
- 51.Kramer MK, Kriska AM, Venditti EM, Miller RG, Brooks MM, Burke LE, Siminerio LM, Solano FX, Orchard TJ. Translating the Diabetes Prevention Program: a comprehensive model for prevention training and program delivery. Am J Prev Med. 2009 Dec;37(6):505–11. doi: 10.1016/j.amepre.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 52.Venditti E, Kramer M. Diabetes Prevention Program Community Outreach Perspectives on Lifestyle Training and Translation. Am J of Prev Med. 2013;44:S339–345. doi: 10.1016/j.amepre.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53*.Luohua J, Spero MM, Janette B, William HG, Haixiao H, Kelly AJ, Yvette R for the Special Diabetes Program for Indians Diabetes Prevention Demonstration Project. Translating the Diabetes Prevention Program into American Indian and Alaska Native Communities. Diabetes Care. 2013;36(9):2027–2034. doi: 10.2337/dc12-1250. Type 2 diabetes affects American Indians disproportionately, and in 2009 was twice the age-adjusted prevalence of non-Hispanic whites. Effective translation of the DPP into Native Communities with scarce resources and diverse health care settings and a highly mobile population will have an important positive impact. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vojta D, Koehler T, Longjohn M, Lever J, Caputo N. A Coordinated National Model for Diabetes Prevention: Linking Health Systems to an Evidence-Based Community Program. Am J of Prev Med. 2013;44:S301–S306. doi: 10.1016/j.amepre.2012.12.018. [DOI] [PubMed] [Google Scholar]