Abstract
Aim
To examine challenges contributing to disruptions in care during the transition from paediatric to adult care among young adults with Type 1 diabetes who are primarily in ethnic minority groups and have low socio-economic status.
Methods
Participants (n = 20) were newly enrolled patients in a transition clinic for young adults with Type 1 diabetes with a history of loss to medical follow-up. Participants completed qualitative semi-structured interviews detailing their transition experiences in addition to demographic, HbA1c and psychosocial measures. Descriptive statistics were completed for quantitative data, and narrative thematic analysis of interviews was used to identify common themes. A mixed-method analysis was used to identify the associations between stressors identified in interviews and clinical and psychosocial variables.
Results
Three categories of challenges contributing to loss to follow-up were identified: psychosocial challenges, health provider and health system challenges and developmental challenges. Participants experienced a high degree of stressful life circumstances which were associated with higher HbA1c (r = 0.60, P = 0.005), longer duration of loss to follow-up (r = 0.51, P = 0.02), greater emergency department utilization (r = 0.45, P = 0.05), and lower life satisfaction (r = −0.62, P = 0.003).
Conclusions
A confluence of challenges, including stressful life circumstances, healthcare system barriers and the developmental trajectory of young adulthood, contributes to a high risk of loss to follow-up and poor health in this population of young adults with Type 1 diabetes. An integrated approach to transition addressing medical and psychosocial needs may facilitate improved follow-up and health outcomes in clinical settings.
Introduction
Transition, the purposeful and coordinated transfer of care from paediatric to adult healthcare settings, has attracted increased attention owing to evidence that young adults with diabetes are at high risk of poor health outcomes during, and following, this transition [1–3]. Research conducted to date has found high rates of loss to medical follow-up and increased hospitalization rates after discharge from paediatric care [4–6], with one recent study finding that among young adults with Type 1 diabetes, 34% had a gap of >6 months and 12% a gap of >12 months, between paediatric and adult care [1].
Numerous studies have documented factors contributing to transition challenges, including inadequate preparation [1,7], poor availability of appropriate adult care [2,8] and high rates of psychological distress in this population [9,10]; however, few studies have examined the actual experiences of young adults who had difficulty transitioning. Studies that have examined young adults’ experiences focused primarily on healthcare system factors that hindered the process, including a lack of information and preparation for transfer [1,5,7], a desire to transfer earlier or later [5,7] and dissatisfaction with adult care providers [5,7]. What remains understudied is how factors outside the healthcare system contribute to transition challenges and how multiple factors in different life domains may interplay to contribute to difficult transitions.
Young adults have a difficult time maintaining control of diabetes, often because of competing priorities, psychosocial issues and participation in high-risk activities which create barriers to diabetes self-care [2,11]. Few young adults achieve the <53 mmol/mol (7.0%) HbA1c goal for adults (aged ≥20 years) recommended by the American Diabetes Association [12,13]. Ethnic minority populations with diabetes and with low socio-economic status have poorer health compared with other groups [14–16] and face additional barriers to diabetes care, including poor access to healthy foods [17], lower quality of care [15] and less access to diabetes education [18]. We believe, therefore, that these populations are likely to be at particularly high risk for poor health outcomes during the transition from paediatric to adult care.
The purpose of the present study was to investigate the experiences of young adults with low socio-economic status and who are primarily in ethnic minority groups who had lapses in care after their discharge from paediatric care, and to identify the challenges contributing to their disrupted transition. In the present paper, we report findings related to three specific aims: 1) to describe, quantitatively, the clinical status, psychosocial adjustment and quality of life of young adults who experienced lapses in care; 2) to describe, through qualitative interview data, transition challenges from the perspective of young adults who experienced lapses in care; and 3) to explore correlates of young adults’ psychosocial stressors (identified through qualitative interviews), clinical status, psychosocial adjustment and quality of life.
Research design and methods
The present paper describes a mixed-method analysis of interviews and survey data collected as part of a diabetes transition study (Helmsley T1D Transition ‘Let’s Empower and Prepare’ (LEAP) Program; Leona and Harry Helmsley Charitable Trust #2010PG-T1D011; PI: A. Peters). The LEAP study is evaluating the efficacy of a structured transition programme in improving clinic attendance, glycaemic control and psychosocial outcomes during the transition from paediatric to adult care. The three study arms include (1) an intervention group, who receive tailored diabetes education and transition support during their last year in paediatric care; (2) a control group, also in their last year of paediatric care, but not receiving additional transition support; and (3) the ‘rescue group’, young adults who had been lost to follow-up for >3 months after discharge from paediatric care, or were discharged from paediatric care without an identified adult care provider. The present paper henceforth refers only to: the rescue participants, who were recruited through urgent care clinics, community clinics and emergency departments; referrals of former patients by paediatric providers; and snowball sampling among enrolled participants. Study procedures were approved by the University of Southern California Institutional Review Board and conducted in accordance with the Declaration of Helsinki. All participants completed informed consent before study participation.
Quantitative data collection
At study enrolment, participants completed validated instruments assessing clinical status, psychosocial adjustment and quality of life. Clinical data were collected on metabolic control (HbA1c) and healthcare utilization. HbA1c levels were measured using the DCA 2000 analyzer (Bayer, Tarrytown, NY, USA) at the time of survey administration. Healthcare utilization, including emergency department visits over the past 6 months and last routine diabetes care visit, was assessed via self-report.
Psychosocial measures included a modified version of the Perceived Stress Scale [19], a 14-item measure assessing the perception of stress within the past month. The modified version altered the wording of some items for comprehension, and added three items, based on feedback from adolescents from diverse backgrounds in a previous study [20]. The Patient Health Questionnaire-9 [21] is a nine-item scale evaluating the severity of depressive symptoms. Quality-of-life measures included the Satisfaction with Life Scale [22], a five-item scale assessing global life satisfaction as a measure of general well-being, and the Arizona Integrative Outcomes Scale-24 h [23], a single-item visual analogue scale measuring a person’s global state of physical, emotional and spiritual well-being in the preceding 24 h. Cronbach’s α for all scales ranged from 0.83 to 0.85. Removing the three additional items from the Perceived Stress Scale did not substantially change its Cronbach’s α (0.85 as administered; 0.83 without additional items).
Quantitative analysis
Summary scores were calculated for all measures, and those scores were used for analysis. Descriptive statistics were calculated using SPSS 20 (SPSS Statistics for Windows; IBM Armonk, NY, USA). Because of the small sample size, some measures did not meet assumptions of normality; therefore, non-parametric tests (Spearman correlation coefficients) were used. A two-tailed α-level of 0.05 was used for all analyses.
Interview data collection
Upon enrolment in the LEAP study, rescue participants were interviewed regarding their experiences leading up to, and following, their discharge from paediatric care. Interviews were conducted with 20 of the 24 rescue participants. Of the remaining four, one declined to be interviewed and three enrolled after we had determined that saturation of interview findings had been reached. Interviews were semi-structured [24], following an interview guide addressing participants’ diabetes care history (including care providers; treatment regimens; how, why and when participants left paediatric care) and diabetes care challenges and strategies while out of routine care. Interviews were conducted in participants’ homes when possible (n=15), or the clinic or researcher’s office when necessary for logistical reasons (n=5). Interviews were completed by one investigator (E.A.P.; n=16) or a trained research assistant (n=4), audiotaped, transcribed verbatim, and de-identified for analysis.
Interview analysis
Analysis was conducted using a narrative thematic approach [24], which seeks to discern patterns across cases while preserving participants’ own words as the unit of analysis rather than reducing them to descriptive codes. The lead author and two trained research assistants reviewed transcripts to identify and establish consensus around recurring themes, which were reviewed by the investigative team. NVIVO qualitative analysis software (version 9; QSR International Pty Ltd, Doncaster, Australia) 2010 was used to organize interview excerpts and develop a framework for interpretation.
Mixed-method analysis
To complement the study’s qualitative findings, we conducted a post hoc mixed-method analysis examining the relationship between psychosocial stressors and the survey measures described above. The number of psychosocial stressors was determined through coding interview transcripts for passages indicating stressors, and surveying the treating endocrinologist and case manager (blinded to interview data and one another’s ratings) for stressors disclosed in clinical settings [25]. The number of stressors was separately correlated with demographic, clinical and psychosocial measures using zero-order Spearman correlation.
Results
Clinical status, psychosocial adjustment and quality of life
Demographic, clinical and survey data are presented in Table 1. At the time of study enrolment, participants had a mean (SD) age of 21.1 (1.1) years. As the study site was a diabetes clinic in a public healthcare system, no participants had private health insurance and most were of low socio-economic status. Most participants had previously been insured through entitlement programmes such as California Children’s Services, a state programme for children with chronic health conditions, and MediCal, California’s Medicaid programme. These programmes are automatically discontinued at age 18 years, although young adults can reapply for continuing coverage through to age 21 years.
Table 1.
Baseline demographic data, healthcare utilization and psychosocial survey results
| Mean (SD) age | 21.1 (1.1) |
|
| |
| Mean (SD) age at diagnosis | 9.0 (4.7) |
|
| |
| Mean (SD) HbA1c | |
| mmol/mol | 95 (26) |
| % | 10.8 (2.4) |
|
| |
| Race/ethnicity, n (%) | |
|
| |
| Hispanic/Latino | 14 (70) |
|
| |
| Other/Multiracial | 4 (20) |
|
| |
| White | 1 (5) |
|
| |
| Asian | 1 (5%) |
|
| |
| Healthcare utilization | |
|
| |
| Mean (SD) no. months since last regular MD visit | 12.0 (10.4) |
|
| |
| Mean (SD) no. emergency department visits in past 6 months | 0.65 (1.0) |
|
| |
| Psychosocial survey results | |
|
| |
| Median (interquartile range) depression score: range: 0–27; higher indicates more depressive symptoms | 5 (3–10) |
|
| |
| Median (interquartile range) global well-being score: range: 0–100; higher indicates better well-being | 77 (66.5–87.8) |
|
| |
| Mean (SD) life satisfaction score: range: 5–35; higher indicates better life satisfaction | 23.8 (6.0) |
|
| |
| Mean (SD) perceived stress score: range 0–68; higher indicates greater perceived stress | 32.8 (6.4) |
Participants had a mean (SD) HbA1c level of 95 (26) mmol/mol [10.8 (2.4)%], and had been without routine diabetes care for a mean (SD) of 12 (10.4) months. Eight participants (40%) reported diabetes-related emergency department visits in the past 6 months; the number of visits ranged from 1 to 4. On the Patient Health Questionnaire-9, 10 participants (50%) reported no or minimal depressive symptoms (score 0–4), four (20%) reported mild symptoms (score 5–9), four (20%) reported moderate symptoms (score 10–14), and two (10%) reported moderately severe depressive symptoms (score 15–19). Participants’ life satisfaction scores fell into the average range, similar to mean Satisfaction with Life Scale scores reported in a recent study of underserved minorities with Type 2 diabetes [26]. Mean Perceived Stress Scale scores indicated moderate levels of perceived stress; scores were markedly higher (32.80 vs 18.85) than a community sample of > 500 adolescents in Los Angeles County [20]. The median Arizona Integrative Outcomes Scale global well-being score was higher (77 vs 64) than mean scores of a community sample of 856 college students [27].
Patients’ perspectives on transition challenges
Participants reported a variety of challenges to transition, which fell into three thematic categories. Health provider/health system challenges were related to poor communication on the part of providers and health systems, and difficulty navigating the public healthcare system. Developmental challenges occurred when care was disrupted for reasons characteristic of young adults, such as feelings of invulnerability, poor planning and foresight, or deprioritizing medical needs due to competing priorities. Psychosocial challenges occurred when seeking care was preempted by more urgent demands stemming from participants’ psychosocial life circumstances. Within these categories, specific challenges are identified and described, including representative passages from interviews. Passages were edited for clarity and to mask potentially identifying information. Participants’ names were replaced with pseudonyms.
Health provider/health system challenges
Many participants reported receiving minimal guidance on the transition to adult care before their discharge from paediatric clinics. This was attributed to several factors. First, 12 participants (60%) reported that their paediatric providers provided ambiguous or contradictory information about transitioning to an adult provider, or did not provide appropriate referrals for patients who anticipated becoming uninsured.
Miguel: Dr. Smith told me that [after transitioning] I could still go see him every now and then, but I’m going to have to pay [out of pocket]… He told me, I’m not going to probably see you as often, but every now and then, we’ll schedule you an appointment. And he told me that I had to find another doctor around here, so I could start seeing them more often.
Second, misunderstandings regarding options for financing healthcare were reported by seven participants (35%). For example, some participants who lost entitlement coverage at age 18 years did not know they were eligible to reapply for coverage through to age 21 years. This disruption often led participants to leave paediatric care earlier than necessary.
Elisa: I had CCS [California Children’s Services insurance] and MediCal, so that was paying for everything. Apparently, the CCS [California Children’s Services insurance] got cancelled when I turned 18, but I didn’t know you were supposed to reapply, and it just got cancelled out.
After discharge from paediatric care, 14 participants (70%) encountered significant challenges in the public healthcare system, including misinformation, extended waiting times, and difficulty navigating the bureaucracy of the public health system.
Jeremy: I called for an appointment to see a doctor…They said that they charged every time you go to an appointment… Eventually, we had to go to the emergency room to get insulin. And they were like, “So why didn’t you go to a doctor [at County]?” And I told them that they wanted to charge me. And they said, no, that is not true, that it is free.
Additionally, participants described difficulties finding adult providers with knowledge of how to treat Type 1 diabetes:
Rick: Because I was out of prescriptions and pretty much on the last of my Lantus, I went to that physician and all they had was this other stuff, this 70/30 and then this other one, Humulin R, or something. So that wasn’t great.
Interviewer: How did they tell you to take that?
Rick: They didn’t really know anything… They were kind of comparing it to Lantus. He really didn’t know, so he was like, okay… take 20 [units] in the morning and 20 at night, but that … dropped me down.
Finally, the policies of health systems and third-party payers often contradicted one another, leaving young adults with the challenging task of resolving these conflicts in order to access care.
Julie: I just went to emergency rooms until I found [the transition clinic] because they – I tried to get back in Metro Hospital and they wouldn’t let me… [My insurance] kept trying to say that I had to go to Metro, but Metro said that they weren’t accepting new patients.
Developmental challenges
Some disruptions in care were attributable to typical young adult characteristics, such as feeling invincible, being embarrassed around peers, or focusing on competing priorities to the detriment of diabetes care. Developmental challenges often interacted with psychosocial or health system challenges to compound the negative impact on diabetes care. One example occurred when participants missed appointments with their paediatric providers. We attributed missed appointments to developmental factors when participants attributed their failure to attend appointments to forgetting, being ‘dumb’ or ‘lazy’, or not planning ahead for the appointment:
Aaron: I remember my last visit… They tried to set me up for an appointment right before I turned 21. And then I didn’t go to that one. I don’t know why – I guess I was just being dumb about it. Or I forgot or something. But I didn’t go to that last one and then from there on I just lost contact with them.
Because many providers had lengthy waiting times to reschedule appointments, missing a visit often meant that participants were unable to see their provider again before their insurance lapsed and they were no longer able to access paediatric care, thus missing an important opportunity to receive guidance about the transition to adult care.
A focus on competing priorities also interfered with transition. We classified competing priorities as a developmental issue when participants freely chose to prioritize other activities over diabetes care, rather than being compelled to do so out of necessity. Among our sample, 13 participants (65%) described prioritizing other pursuits over their diabetes care. Even when competing priorities were productive, such as attending school, they nonetheless interfered with self-care among young adults who had not yet learned to balance diabetes care with other responsibilities:
Karen: I do want to [get my HbA1c] below seven because I have had it high this past year. Well, this past month, just because of nursing [school], I was just so caught up, and I was disregarding my diabetes… It’s like out of balance, I guess. It’s just because I was so busy with school. It’s just the pressure from school.
Finally, young adults’ tendency to underestimate risk, and not plan for potential problems, often backfired with regard to transition. Eleven participants (55%) reported minimal planning for the transition to adult care, based on assumptions that assistance would be readily available, someone else would manage the transition, or finding an adult care provider would be a straightforward process.
Jessica: I didn’t really anticipate how much of a problem it would be. Because in the past I have had where it was like, oh, suddenly the insurance doesn’t cover this medicine but I will have a backup insurance or stuff like that. It always works out. So I just assumed, oh, it will be easier. They will help me… And it didn’t really work out that way.
Psychosocial challenges
A significant finding was the extent to which stressful psychosocial life circumstances posed a barrier to transitioning from paediatric to adult care. Participants reported a high prevalence of past or current stressors, as outlined in Table 2, including the absence of one or both parents; history of abuse or neglect; being a parent or caregiver; or substance abuse or dependence. Participants reported a median of 2.5 stressors, with a range of 0–6.
In some instances, participants explicitly attributed their difficulty in maintaining access to care to one or more of these stressors. For example, one participant reported inappropriate touching by a healthcare provider at her quarterly follow-up visits, which subsequently led her to avoid seeking care until she ran out of insulin and was admitted to the hospital in diabetic ketoacidosis.
Elisa: He actually did a breast check, so I was like, I never got one of those when I was at the [other clinic]… The first time I came home almost crying. I’m like, Mom, the doctor did this to me and I don’t know why… I asked him – if this is a physical, okay. But he wouldn’t do a physical, so I’m like… you know what, I just don’t feel comfortable.
Another participant had been incarcerated, and reported not having access to an endocrinologist while in prison. Furthermore, when he returned home, neighbourhood safety concerns and limited transportation interfered with his ability to access care.
Ernesto: Everybody is out gangbanging - so you don’t know who you’re going to run into… People just pull out the gun, start shooting at you. So, I don’t want to be at the bus stop too much. My sister’s been giving me rides, but I don’t really ask her too much.
Frequently, multiple psychosocial issues contributed to participants’ diabetes care challenges. For instance, Elisa’s traumatic experience with her healthcare provider, described above, was compounded by her lack of knowledge about how to navigate the health system to access another provider. Additionally, she was experiencing family stress and financial difficulties resulting from her parents’ divorce and father’s job loss, both of which distracted attention from her diabetes care.
While the previous examples illustrate explicit linkages between psychosocial stressors and diabetes care, in other instances, the relationship was indirect. For example, participants with low education had often left school in order to work full time to support their families; however, their lack of education limited them to low-wage, low-status employment, which often lacked the flexibility to take time off to attend medical appointments.
Roberto: If you go [to the clinic] and you say, I have just a little bit of insulin – because there’s a lot of people waiting to be seen by a doctor – they’re like, then you can come back tomorrow… [They say] come back tomorrow, and it’s going to be faster. And I was like, but I have to go to work, I have to support my family.
Many participants reported care challenges similar to Roberto’s, attributable to difficulty balancing employment, caregiving or family needs with their healthcare. In addition, psychosocial issues such as foster care or homelessness undermined participants’ overall life stability, making it more difficult to maintain consistent diabetes care.
Correlates of perceived stressors, clinical status and psychosocial adjustment
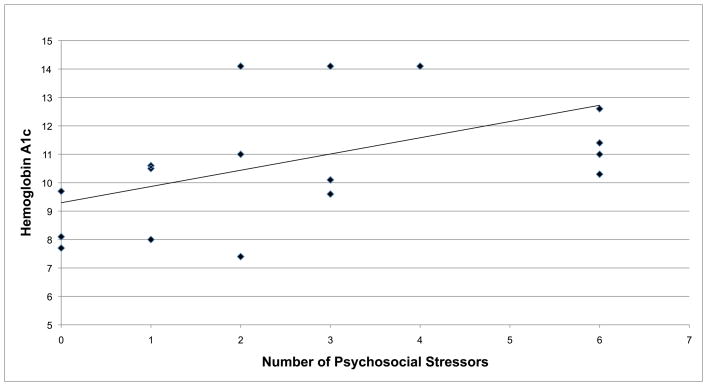
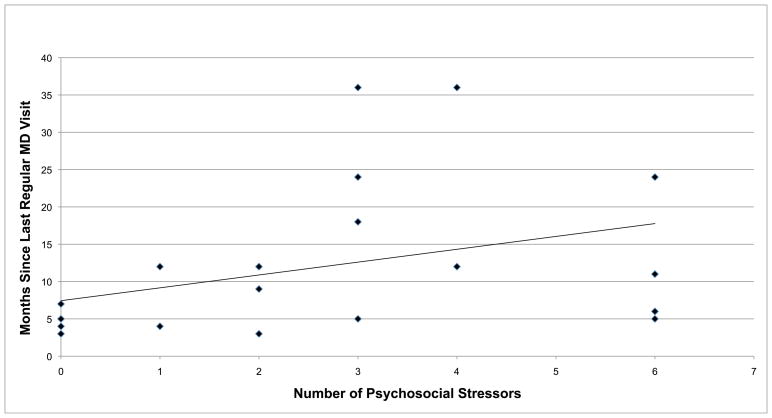
The high prevalence of psychosocial stressors reported in interviews, and participants’ assertions that these issues had disrupted their diabetes care, led us to conduct an analysis of the relationship between the number of stressors and participants’ clinical, psychosocial and quality-of-life status. The correlation matrix presented in Table 3 revealed that a higher number of psychosocial stressors was significantly associated with higher HbA1c levels, longer duration of time without routine care, more emergency department visits and lower life satisfaction. The number of stressors was not significantly associated with depression, perceived stress or global well-being. Notably, the number of stressors was the only variable significantly associated with HbA1c and the duration of time without routine care, and HbA1c was not significantly associated with the duration of time without care. Figures 1 and 2 are scatterplots of the correlations between number of psychosocial stressors and HbA1c (Fig 1) and duration of time without routine care (Fig 2), including a line of best fit.
Table 3.
Spearman correlation coefficients between psychosocial stressors, glycaemic control, healthcare utilization and psychosocial measures
| Measure | HbA1c (%) | Months since last routine MD visit | Emergency department visits | Depression | Life satisfaction | Perceived stress | Global well-being |
|---|---|---|---|---|---|---|---|
| Psychosocial stressors | 0.60** | .51* | 0.45* | 0.34 | −0.62** | −0.16 | −0.17 |
| HbA1c (%) | 1 | 0.23 | 0.39 | 0.16 | −0.35 | −0.03 | −0.18 |
| Healthcare utilization | |||||||
| Months since last routine MD visit | 1 | 0.4 | −0.07 | −0.16 | −0.34 | 0.15 | |
| Emergency department visits | 1 | −0.03 | −0.33 | −0.3 | −0.16 | ||
| Psychosocial measures | |||||||
| Depression | 1 | −0.74** | 0.37 | −0.57** | |||
| Life satisfaction | 1 | −0.32 | 0.57** | ||||
| Perceived stress | 1 | −0.69** | |||||
| Global well-being | 1 | ||||||
P < 0.05.
P < 0.01. Psychosocial stressors: number of self-reported stressors (as identified in Table 1); Healthcare utilization: chart review and self-report; HbA1c: DCA 2000 assay; Depression: Patient Health Questionnaire-9 [21]; Life satisfaction: Satisfaction with Life Scale [22]; Perceived stress: Adapted Perceived Stress Scale [19, 20]; Global well-being: Arizona Integrative Outcomes Scale-24 h [23].
FIGURE 1.
Correlation between number of psychosocial stressors and HbA1c levels.
FIGURE 2.
Correlation between number of psychosocial stressors and months since last routine diabetes care visit.
Discussion
The present findings indicate that current approaches to preparing adolescents for transition are ineffective among a segment of the population experiencing a high degree of psychosocial stress. Ideally, transition preparation is ongoing over at least a year before discharge from paediatric care [2]; however, the majority of participants felt that they had not received adequate preparation for transition, consistent with other research [1]. We posit that issues contributing to the lack of preparation may have included disruptions in paediatric care, transition discussions being preempted by more urgent clinical concerns, limitations imposed by third-party payers, and a lack of adequate resources for uninsured adults with diabetes. Future research incorporating paediatric and adult care providers’ perspectives on transition may provide insight into strategies to ensure continuity of care among patients with complex psychosocial life circumstances at high risk of loss to follow-up.
The present study supports previous research documenting the multiple social, developmental and health system factors that create challenges in the transition from paediatric to adult care for young adults with diabetes [1,4–6]. The developmental characteristics identified in this study are normal among young adults and common sources of diabetes care challenges [2,3,28] in this age group. While adolescents may also display these characteristics, they are more likely to have adult oversight which mitigates their impact on diabetes care; additionally, certain risk-taking behaviours peak in the young adult age range [29].
The present study also highlights the significant role that psychosocial stressors play in magnifying transition challenges among young adults with diabetes with low socio-economic status who are predominantly in ethnic minority groups. Although in our analysis we discussed discrete barriers to transition, participants were typically lost to follow-up because of a confluence of challenging circumstances, which had often contributed to repeated disruptions in care in the years leading up to transition. Clinicians may consider screening for the psychosocial stressors identified in Table 3 and, where available, initiate case management, more intensive diabetes self-management support, or other services which may facilitate improved glycaemic control and psychosocial well-being. Best practices identified by experts in transition care, such as providing a patient navigator and screening and providing referrals for mental health treatment [2], are particularly essential to implement among this population. Such intensive service provision, beginning well in advance and continuing throughout the transition period, may be particularly important for adolescents at high risk, who otherwise may go without needed care, or access care from more resource-intensive providers such as emergency departments.
By far the most common stressor identified in interviews was the absence of a parent, reported by 80% of participants. Previous research has documented that parent cohabitation, caregivers’ marital status and family cohesion are associated with disease management and glycaemic control [30–32]. In addition to the stress incurred by a parent’s absence, which results in increased caregiving, household management and economic burden on the remaining caregiver, several participants in this study were separated from their parents under highly stressful circumstances including death, deportation, abuse or neglect. In the present study, therefore, the absence of a parent may be a proxy for, or confounded by, stress incurred as a result of these other circumstances. Further research is needed to assess the relative contributions of these issues on young adults’ diabetes management and overall well-being.
The lack of a significant association between the number of psychosocial stressors and the measure of perceived stress is somewhat counterintuitive and merits discussion. The Perceived Stress Scale measures one’s cognitive appraisal of stress within the past month, whereas many of the stressors had taken place in the more distant past. We believe that while the reported stressors may have been perceived as stressful when they happened and undermined the participants’ ability to maintain consistent diabetes care, they may not have been a cause of acute stress within the timeframe measured by the Perceived Stress Scale. Similarly of interest are participants’ high global well-being (median score 77) as compared with a community sample of college students (mean score 64), as well as patients with polyarthritis (mean score 53.1) [33] and chronic pain (mean score 55) [34]. One possible explanation is that the assessment measures well-being over the previous 24 h, and participants may have experienced greater well-being on that day as a result of feeling relieved at finding a source of diabetes care. The other psychosocial assessments presented in this paper had greater look-back periods, and thus may have been less influenced by participants’ state of mind at that particular moment in time.
Lack of generalizability is frequently cited as a limitation of qualitative studies with small sample sizes, although this is, to some extent, a mischaracterization of the intent of qualitative research. The strength of qualitative research is in examining a topic about which little is known in detail; a concomitant limitation is the care the reader must take in translating these findings to other contexts. For the present study, the findings are most likely to be relevant to adolescents and young adults managing diabetes alongside complex psychosocial challenges, and those who are uninsured or medically under-served.
Another limitation of the study was collecting healthcare utilization data via self-report. Given participants’ stressful life circumstances, it is plausible that they were inaccurate reporters regarding the date of their last paediatric diabetes care visit; however, qualitative and quantitative data collected on participants’ other healthcare utilization (such as urgent care visits to refill medications), as well as participant referrals from paediatric care providers whose former patients were seeking assistance in finding care, provides evidence that participants did experience a gap in routine diabetes care.
The mixed-method analysis investigating the relationship of psychosocial stressors to other outcomes has several limitations. Notably, we can account for only the number of stressors, and not their severity or perceived impact on diabetes care. Furthermore, because stressors were identified inductively, they may be under-reported. Because of the limited sample size, we had minimal power to detect relationships between variables and only completed univariate analyses. Finally, as these data were cross-sectional, we could not establish causal relationships between variables. For these reasons, further research is needed to more rigorously evaluate the psychosocial stressors identified in the present study and their relationships with other health and quality-of-life indicators.
In conclusion, the present study has identified challenges to transition from paediatric to adult care in a particularly at-risk population of young adults of low socio-economic status with complex psychosocial life circumstances. The study validates previous findings regarding developmental and health system challenges to transition and illustrates how these challenges may be compounded by stressors stemming from personal and family issues. Identifying and providing resources to manage such stressors in the course of routine paediatric care may be crucial for maintaining ongoing follow-up and successful transition to adult care. In the absence of such services, loss to follow-up and deterioration of glycaemic control in young adulthood are likely outcomes.
Table 2.
Baseline prevalence of psychosocial stressors
| Psychosocial stressors* | n (%) |
|---|---|
| Absent parent (departure of parent or primary caregiver involved in participant’s upbringing; due to death, divorce, migration, abuse or neglect) | 16 (80) |
| Foster care/Group home/Left home(participant removed from home by social service agency, or left home to escape significant family conflict) | 6 (30) |
| Mental illness/Psychiatric comorbidity (participant has mental health diagnosis or history of treatment with psychiatric medication) | 5 (25) |
| Abuse by trusted adult (participant reports abuse, assault or physical violence perpetrated by parent, caregiver, or other trusted authority figure) | 5 (25) |
| Alcohol/Drug abuse or dependence (Participant reports ‘problem’ drinking or substance use, addiction, or has sought treatment for above) | 4 (20) |
| Parent, expectant parent, or legal guardian (participant is a parent or legal guardian to a minor, or participant’s partner is pregnant) | 4 (20) |
| Low education (participant did not complete high school or earn a GED) | 4 (20) |
| Learning disability/Special education (participant reports having learning disability or having been placed in special education classes in school) | 4 (20) |
| Incarceration (participant reports having served jail or prison sentence) | 3 (15) |
| Homelessness (participant reports not having had a home at some point in life; was ‘couch surfing’, sleeping in car, temporary shelter, etc.) | 2 (10) |
| Median (interquartile range) no. stressors per participant | 2.5 (1–4) |
As reported in interview, to treating physician, or to case manager/study coordinator.
What’s new?
Young adults with Type 1 diabetes encounter a confluence of developmental, psychosocial and health system barriers to timely transition to adult care.
Young adults with a history of significant psychosocial life stressors may be more likely to have longer lapses in medical care, deteriorating glycaemic control and poor life satisfaction.
An integrated approach to transition, incorporating medical and psychosocial care, may be especially important among adolescents who are exposed to significant psychosocial life stressors.
Acknowledgments
Funding sources
None.
E.A.P. takes full responsibility for the work as a whole. The authors gratefully acknowledge project assistants Lucy Montoya, Daniella Florindez, Magaly Juarez and Sergio Sandoval. This project was supported by the Helmsley T1D Transition ‘Let’s Empower and Prepare’ (LEAP) Program (Leona M. and Harry B. Helmsley Charitable Trust #2010PG-T1D011; PI: A. Peters), and the National Center for Research Resources and National Center for Advancing Translational Sciences, National Institutes of Health (NCRR/NCATS #KL2RR031991; PI: T. Buchanan). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH or the Helmsley Foundation. E.A.P. is a KL2 Scholar awarded under the KL2 Mentoring Research Career Development Award through Southern California Clinical and Translational Science Institute at University of Southern California, Keck School of Medicine. Portions of this paper were previously published in abstract form: Pyatak EA, Sequeira PA, Peters AL, Weigensberg MJ. Psychosocial risk factors in low-socioeconomic status young adults with Type 1 diabetes transitioning from pediatric to adult care Diabetes. 2012;61(Suppl 1):A200.
Footnotes
Competing interests
None declared.
References
- 1.Garvey KC, Wolpert HA, Rhodes ET, Laffel LM, Kleinman K, Beste MG, et al. Health care transition in patients with type 1 diabetes. Diabetes Care. 2012;35:1716–1722. doi: 10.2337/dc11-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peters A, Laffel L. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association. Diabetes Care. 2011;34:2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garvey K, Wolpert H. Identifying the unique needs of transition care for young adults with type 1 diabetes. Diabetes Spectrum. 2011;24:22–25. [Google Scholar]
- 4.Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a Universal Health Care System. Pediatrics. 2009;124:e1134–1141. doi: 10.1542/peds.2009-0041. [DOI] [PubMed] [Google Scholar]
- 5.Pacaud D, Yale JF, Stephure D, Trussel R, Davies HD. Problems in transition from pediatric care to adult care for individuals with diabetes. Can J Diabetes. 2005;29:13–18. [Google Scholar]
- 6.Van Walleghem N, Macdonald CA, Dean HJ. Evaluation of a systems navigator model for transition from pediatric to adult care for young adults with type 1 diabetes. Diabetes Care. 2008;31:1529–1530. doi: 10.2337/dc07-2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Busse FP, Hiermann P, Galler A, Stumvoll M, Wiessner T, Kiess W, et al. Evaluation of patients’ opinion and metabolic control after transfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Horm Res. 2007;67:132–138. doi: 10.1159/000096583. [DOI] [PubMed] [Google Scholar]
- 8.Dovey-Pearce G, Hurrell R, May C, Walker C, Doherty Y. Young adults’ (16–25 years) suggestions for providing developmentally appropriate diabetes services: a qualitative study. Health Soc Care Community. 2005;13:409–419. doi: 10.1111/j.1365-2524.2005.00577.x. [DOI] [PubMed] [Google Scholar]
- 9.Northam EA, Lin A, Finch S, Werther GA, Cameron FJ. Psychosocial well-being and functional outcomes in youth with type 1 diabetes 12 years after disease onset. Diabetes Care. 2010;33:1430–1437. doi: 10.2337/dc09-2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bryden KS, Dunger DB, Mayou RA, Peveler RC, Neil HA. Poor prognosis of young adults with type 1 diabetes: a longitudinal study. Diabetes Care. 2003;26:1052–1057. doi: 10.2337/diacare.26.4.1052. [DOI] [PubMed] [Google Scholar]
- 11.Pyatak E. Participation in occupation and diabetes self-management in emerging adulthood. Am J Occup Ther. 2011;65:462–469. doi: 10.5014/ajot.2011.001453. [DOI] [PubMed] [Google Scholar]
- 12.American Diabetes Association. Standards of medical care in diabetes–2013. Diabetes Care. 2013;36 (Suppl 1):S11–66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sparud-Lundin C, Ohrn I, Danielson E, Forsander G. Glycaemic control and diabetes care utilization in young adults with Type 1 diabetes. Diabet Med. 2008;25:968–973. doi: 10.1111/j.1464-5491.2008.02521.x. [DOI] [PubMed] [Google Scholar]
- 14.Nicklett EJ. Socioeconomic status and race/ethnicity independently predict health decline among older diabetics. BMC Public Health. 2011;11:684. doi: 10.1186/1471-2458-11-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peek ME, Cargill A, Huang ES. Diabetes health disparities: A systematic review of health care interventions. Med Care Res Rev. 2007;64:101S–56S. doi: 10.1177/1077558707305409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U.S. Department of Health and Human Services Office of Minority Health. Diabetes and Hispanic Americans. 2012 [updated 8/28/2012; cited 2012 October 2]; Available at: http://minorityhealth.hhs.gov/templates/content.aspx?lvl=3&lvlID=5&ID=3324. Last accessed.
- 17.Chaufan C, Davis M, Constantino S. The twin epidemics of poverty and diabetes: understanding diabetes disparities in a low-income Latino and immigrant neighborhood. J Community Health. 2011;36:1032–1043. doi: 10.1007/s10900-011-9406-2. [DOI] [PubMed] [Google Scholar]
- 18.Shaw K, Killeen M, Sullivan E, Bowman P. Disparities in diabetes self-management education for uninsured and underinsured adults. Diabetes Educ. 2011;37:813–819. doi: 10.1177/0145721711424618. [DOI] [PubMed] [Google Scholar]
- 19.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 20.Nguyen-Rodriguez ST, Unger JB, Spruijt-Metz D. Psychological determinants of emotional eating in adolescence. Eat Disord. 2009;17:211–224. doi: 10.1080/10640260902848543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiat Ann. 2002;32:509–515. [Google Scholar]
- 22.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 23.Bell IR, Cunningham V, Caspi O, Meek P, Ferro L. Development and validation of a new global well-being outcomes rating scale for integrative medicine research. BMC Complement Altern Med. 2004;4 doi: 10.1186/1472-6882-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riessman CK. Narrative methods for the human sciences. Thousand Oaks, CA: Sage Publications, Inc; 2008. [Google Scholar]
- 25.Pyatak EA, Sequeira P, Peters AL, Montoya L, Weigensberg MJ. Disclosure of psychosocial stressors affecting diabetes care among uninsured young adults with Type 1 diabetes. Diabet Med. 2013;30:1140–1144. doi: 10.1111/dme.12248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Phelps K, Hodgson J, Lamson A, Swanson M, White M. Satisfaction with life and psychosocial factors among underserved minorities with type 2 diabetes. Soc Indic Res. 2012;106:359–370. [Google Scholar]
- 27.Menk Otto L, Howerter A, Bell IR, Jackson N. Exploring measures of whole person wellness: integrative well-being and psychological flourishing. Explore (NY) 2010;6:364–370. doi: 10.1016/j.explore.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolpert HA, Anderson BJ, Weissberg-Benchell J. Transitions in Care: Meeting the Challenges of Type 1 Diabetes in Young Adults. Alexandria, VA: American Diabetes Association; 2009. [Google Scholar]
- 29.Helgeson VS, Palladino DK, Reynolds KA, Becker D, Escobar O, Siminerio L. Early adolescent relationship predictors of emerging adult outcomes: Youth with and without Type 1 Diabetes. Ann Behav Med. 2013 doi: 10.1007/s12160-013-9552-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hilliard ME, Wu YP, Rausch J, Dolan LM, Hood KK. Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. J Adolesc Health. 2013;52:28–34. doi: 10.1016/j.jadohealth.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cameron FJ, Skinner TC, de Beaufort CE, Hoey H, Swift PG, Aanstoot H, et al. Are family factors universally related to metabolic outcomes in adolescents with Type 1 diabetes? Diabet Med. 2008;25:463–468. doi: 10.1111/j.1464-5491.2008.02399.x. [DOI] [PubMed] [Google Scholar]
- 32.Mackey ER, Hilliard ME, Berger SS, Streisand R, Chen R, Holmes C. Individual and family strengths: an examination of the relation to disease management and metabolic control in youth with type 1 diabetes. Fam Syst Health. 2011;29:314–326. doi: 10.1037/a0026589. [DOI] [PubMed] [Google Scholar]
- 33.Grønning K, Skomsvoll JF, Rannestad T, Steinsbekk A. The effect of an educational programme consisting of group and individual arthritis education for patients with polyarthritis—A randomised controlled trial. Patient Educ Couns. 2012;88:113–120. doi: 10.1016/j.pec.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 34.Ritenbaugh C, Hammerschlag R, Dworkin SF, Aickin MG, Mist SD, Elder CR, et al. Comparative effectiveness of traditional chinese medicine and psychosocial care in the treatment of temporomandibular disorders–associated chronic facial pain. J Pain. 2012;13:1075–1089. doi: 10.1016/j.jpain.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]