Abstract
Following the onset of maturation, female athletes have a significantly higher risk for anterior cruciate ligament (ACL) injury compared with male athletes. While multiple sex differences in lower-extremity neuromuscular control and biomechanics have been identified as potential risk factors for ACL injury in females, the majority of these studies have focused specifically on the knee joint. However, increasing evidence in the literature indicates that lumbopelvic (core) control may have a large effect on knee-joint control and injury risk. This review examines the published evidence on the contributions of the trunk and hip to knee-joint control. Specifically, the sex differences in potential proximal controllers of the knee as risk factors for ACL injury are identified and discussed. Sex differences in trunk and hip biomechanics have been identified in all planes of motion (sagittal, coronal and transverse). Essentially, female athletes show greater lateral trunk displacement, altered trunk and hip flexion angles, greater ranges of trunk motion, and increased hip adduction and internal rotation during sport manoeuvres, compared with their male counterparts. These differences may increase the risk of ACL injury among female athletes. Prevention programmes targeted towards trunk and hip neuromuscular control may decrease the risk for ACL injuries.
1. Introduction
The number of females participating in sports has increased by over 900% in high school and 500%[1] in collegiate athletics over the last few decades. This large increase in participation, combined with a 4- to 6-fold higher anterior cruciate ligament (ACL) injury rate in females[2–4] has led to a corresponding increase in ACL injuries. ACL ruptures lead to chronic knee pain and disability, a significantly greater risk of radiographically diagnosed knee osteoarthritis,[5–8] high costs for management,[9–12] loss of entire sports seasons, possible loss of scholarship funding and significantly lowered academic performance.[13,14]
Sex differences in ACL injury rates may be explained by anatomical,[15–23] hormonal[4,7,24–30] and/or neuromuscular factors.[11,31–34] Even though anatomical and hormonal factors may contribute to an ACL injury, the implications of both factors are not yet clear.[35] Moreover, modification of these parameters would be both difficult and controversial. In contrast, neuromuscular adaptations are readily achievable and have been used extensively to lower ACL injury risk in female athletes.[7,33,36–38]
There is increasing evidence that insufficient or abnormal neuromuscular control of the lower limbs during athletic movements, in particular over the knee joint, is a primary contributor to non-contact ACL injuries, especially in the female athlete.[39] The knee is not an isolated joint, but is part of the body in which the trunk, hips, knees and ankles constitute the body’s kinetic chain that controls lower-extremity movements. The proximal and distal segments of the body’s kinetic chain can have significant effects on knee-joint biomechanics.[35,37] The kinetic chain model refers to the body as a linked system of interdependent segments, often working in a proximal-to-distal sequence, to achieve the desired movement in an efficient manner.[40] Hence, considering the relationship between the trunk and the lower-extremity joints during a dynamic task, it is important to consider the effects of the trunk and hip on the control of the knee. Specifically, the trunk-to-hip system will be referred to as core, throughout the review. This review reports the existing evidence on the contributions of the trunk and hip to neuromuscular control of the knee joint.
A systematic review of the literature was performed by utilizing an electronic database literature search in PubMed MEDLINE (1985–2009). The keyword selection was designed to capture all aspects of the contributions of the trunk and hip to neuromuscular control of the knee joint and the search terms included: ‘ACL prevention’, ‘ACL biomechanics’, ‘ACL and trunk’, ‘ACL and hip’, ‘non-contact ACL injuries’, ‘mechanisms of ACL injuries’ and ‘prevention non-contact ACL injuries’. The search was supplemented by a review of the bibliographies of retrieved articles, personal correspondence with authors of retrieved articles and hand searching of journals to identify any additional studies addressing this topic of interest. Articles included in this review were limited to those published in English.
2. The Concept of ‘Core Stability’
Despite the growing interest in the body’s core during the last decade, ‘core stability’ remains an often ambiguous or misused term. It has been incorrectly used synonymously and interchangeably with core strength, hip strength, balance and spine stability. In this review, the term ‘core musculature’ will be referred to as those muscles that surround and insert into the lumbopelvic region. These muscles act synergistically to stabilize the trunk and hip and contribute to the stability of more distal joints, including the knee joint. The term ‘core stability’ is considered the ability of passive (ligaments and vertebral facets) and active stabilizers involved in the lumbopelvic region to maintain appropriate trunk and hip posture, balance and control during static and dynamic movements.[41] Neuromuscular control consists of sensory input (muscle spindles, Golgi tendon organs and receptors within the core ligaments),[42,43] CNS processing and motor (the neuromuscular signal) output. The output is targeted to the core musculature, thus optimal recruitment, strength and endurance of the 29 muscles attached to the pelvis are necessary to maintain and restore joint (core) homeostatic stability in response to internal or external forces from expected or unexpected perturbations in all planes of motion. The need for an adequate intermuscular coordination between such a large number of muscles shows the complex nature existing under the concept of core. Core stability, a critical component of the entire body kinetic chain, is especially important during unexpected dynamic situations, where insufficient control of the core may affect the control of other joints through the multi-segment system and possibly lead to injury at other joints in the system.[39] The concepts of ‘robustness’ and ‘performance’ are important for the proper investigation of dynamic stability of the core during athletic manoeuvres.[44] According to the definition of robustness of Reeves et al., the core is considered to be robust if it remains stable after perturbation.[44] In contrast, performance is defined as how close the disturbed trajectory of the core remains to the undisturbed and expected trajectory. Both concepts depend on the neuromuscular control of all the muscles that attach to the lumbopelvic region.
The main function of the core during sports manoeuvres is to maintain the stability of the whole system and allow optimal production, transfer and control of force and motion to the terminal segment (proximal to distal) for integrated kinetic chain activities in order to achieve the maximum efficiency.[45] Kibler et al.[45] demonstrated that >50% of the total kinetic energy and total force generated in the tennis serve is generated by the lower legs, hip and trunk. The proximal to distal muscle firing sequence has been shown in running and kicking activities, with the hip flexors being the main contributor muscles to achieve the highest velocities.[40,46]
Growing evidence for decreased neuromuscular control of the core as an underlying cause of injury[41,47–53] justifies the increased use of current trunk or core neuromuscular training as a central tenet of rehabilitation treatments and prevention.[54–59] However, some of these studies observed a reduction of force output at the hip, which may consequently result in an increased risk of lower-extremity injury. Although the hip is part of the core, measures of hip strength should not be wholly defined as, or generalized to, core stability. It is not known how isolated hip strength functions to stabilize the core. If quantitative analysis is accurate, for daily living, 10% of maximal voluntary contraction or even less of abdominal co-contraction may be sufficient to achieve spine stability. Moreover, given the relationship observed between stiffness and stability, the majority of spine stability may be achieved in the first 25% of the maximum contraction level.[60] Hence, neural control, motor firing patterns or muscular endurance are likely to be of greater importance than strength in determining overall core stability. Further studies and the use of core models that include all the muscles that attach to the pelvis are needed to elucidate the influence of each of these control components on total core stability. Ireland[61] speculated about a possible relationship between the trunk and hip with ACL injuries. The videographic sequence analyses of sports knee injuries formed the basis of the authors’ proposed ‘position of no return’ model for a non-contact ACL injury.[61] However, the link between proximal control strategies and abnormal knee-joint loading and motions specifically related to sex differences remains unclear.
In the remainder of this review, we evaluate the current evidence into the three planes of movement (sagittal, coronal and transverse) in order to create a working construct to better understand the current evidence for the connection between the proximal core neuromuscular controllers and distal knee-joint stability. Although trunk and hip are part of the core, both regions were reviewed in separate sections for didactic reasons.
In summary:
Core musculature is referred to as those muscles that surround and insert into the lumbopelvic region.
These muscles act synergistically to stabilize the trunk and hip and contribute to the stability of more distal joints, including the knee joint.
Core stability is considered the ability of passive and active stabilizers of the lumbopelvic region to achieve the minimum neuromuscular control needed, in order to maintain appropriate trunk and hip posture, balance and control during static and dynamic movements.
The link between proximal control strategies and abnormal knee-joint loading and motions specifically related to sex differences remains unclear.
3. Sagittal Plane Evidence for Proximal Control of Knee-Joint Stability
3.1 Trunk Contributions
Knee flexion-extension may be influenced by the trunk and hip proximal musculature. The trunk, arms and head comprise approximately 60% of the body mass.[62] Increases in height of the centre of mass during puberty may result in more challenging trunk neuromuscular control, especially during high-speed athletic manoeuvres.[63] Trunk, arms and head position relative to hip, knee and ankle may influence ground reaction force (GRF), energetics and knee load from a landing or cutting manoeuvre.[64] An understanding of the biomechanical relationship between the trunk and knee may be used to reduce GRF and energetic demands of passive and dynamic restraints and thus decrease the likelihood of knee injury.
Recently, Blackburn and Padua studied trunk, hip and knee biomechanics during two landing tasks, a natural landing strategy (preferred) and a landing that involved active trunk flexion upon landing (flexed). Peak trunk flexion angle was 47% greater for the flexion group compared with the preferred landing group.[65] The authors demonstrated that trunk flexion during landing produced concomitant increases in knee (22°) and hip flexion (31°) angles. An increase in knee flexion may result in decreased anterior shear forces and GRF, with a subsequent decrease in ACL load. Hamstrings lengthening and the increase in passive tension imposed by greater hip flexion may also account for the decreased tension induced by knee flexion. Coronal and transverse plane knee kinematics did not differ significantly between preferred and flexed landings. In addition, the authors did not find sex differences in landing forces and quadriceps electromyographic activity depending on trunk flexion.[66] Flexing the trunk forward or moving the mass of the upper body anterior towards the knees may result in a reduced external knee flexion and internal quadriceps moments with concomitant increase in internal hamstrings moments during landing. This may be explained by a reduction in the quadriceps moment arm (decreasing shear forces) between trunk and knee, and an increase in the hamstrings hip extensor activity.[64] Synergistically, trunk flexion in a standing position may increase posterior shear forces and enhance hamstrings activation, which can potentially decrease forces on the ACL.[67,68] This mechanical advantage can be altered by reduced stiffness derived by excessive length and laxity of hamstrings muscles. Increased laxity may reduce muscle reflex activity and fibre shortening velocity.[69,70] Both would increase latencies, decrease joint stiffness and potentially decrease dynamic knee stability.[31,69–76] Generalized joint laxity, which has been reported to be higher in female athletes, and anterior–posterior knee-joint laxity have been associated with an increased risk of non-contact ACL injury for both males and females.[77–80]
The absence of trunk control may increase ACL load and predispose one to an injury, especially with knee angles near full extension.[81–87] Altered weighting of the trunk may have direct effects on loading of the knee joint. Kulas et al.[88] recently reported lower-extremity biomechanics during drop landings with added load (10% of bodyweight) to the trunk. The study subjects were divided into either a trunk flexor or trunk extensor landing style. The trunk extensor group increased knee and ankle extensor efforts over 20% and 14–15% during landing, respectively. In contrast, the trunk flexor group did not exceed a 10% increase in either the ankle or knee extensor moments after weighting. The trunk extensor group showed an 11–18% decrease in hip extensor efforts, while flexor group increase 14–19%. These findings are in agreement with Farrokhi et al.,[89] who reported similar relationships during a lunge manoeuvre. Studies have reported that females demonstrated more erect landings postures[90–93] and less hip absorption compared with males,[90] which may be related to the decrease in hip extensor activity reported by Kulas et al.[88] From these data, it may be concluded that an increase in flexion of the trunk would be an appropriate strategy to reduce ACL injury risk. The resultant increase in hip and knee flexion alone would support this statement. However, the referred studies did not clarify whether or not the behaviour is the same for both sexes. Furthermore, the reported trunk flexion angles do not usually correspond to those angles seen in athletic manoeuvres. Excessive trunk flexion and concomitant hip flexion may influence the gluteus medius and gluteus maximus muscles attachment leading to decreased hip abduction and extension strength. This may in turn result in undesirable joint angles and moments at the knee during dynamic motion, potentially decreasing proximal control.[94] A recent injury mechanism description in the literature, based on video analysis of basketball players, reported greater hip and knee flexion angles in female players who suffered a valgus collapse with ACL injury compared with males.[93] The description of the trajectory of the trunk during landing (performance) as well as the sudden reaction movement of the trunk following the perturbation created from the GRF (robustness) may be useful to find sex differences in trunk behaviour and stability.
Neuromuscular control of the trunk is likely different between males and females.[94] Abdominal activation patterns may differ between sexes during double-leg landings, though they may be reliable for prediction of ACL injuries in females.[34] Specific local abdominal activation strategies (tranversus and internal oblique abdominal muscles) used by males during landing may be safer than general abdominal muscles activation used by females.[94] Although local activation strategies are beneficial for injury prevention,[95–98] the general activation of other muscles is also important for core stability. All the torso muscles, acting harmoniously, likely play a critical role in securing spinal stability and reacting against external perturbations.[99–103] However, further research is needed in this area to know if there are different abdominal patterns between sexes (e.g. muscle patterns that occur in the quadriceps, hamstrings, or gluteus) and how these patterns affect trunk motion and, consequently, knee load.
3.2 Hip Contributions
Increased trunk flexion during landing produced concomitant increases in knee and hip flexion compared with a more erect/extended trunk posture in a drop jump.[65] An increase in hip flexion could result in reduced shear forces and increased hip extensor effort and energy absorption.[88,104] The gluteus maximus is an important controller of trunk flexion,[105–108] and contributes to hip absorption at landing.[90] Females may land more erect compared with males,[90,91,93,109] thus decreasing the hip absorption and, consequently, increasing knee and ankle loads.[90]
Eccentric hip extensor contraction can absorb over 20% of the body’s total kinetic energy in females during soft, compared with stiff, landings.[64] Hence, the trunk and hip flexor/extensor musculatures are an important contributor to loads at the knee, and may influence the GRF from a landing. However, the relative contribution of each joint to energy absorption is poorly understood. Females have lower gluteus maximus activation[110,111] and hip extension strength compared with males.[20,112–114] This may indicate the crucial role posterior hip muscles play in preventing knee injuries. However, these data must be taken with caution because these studies did not control the influence of the trunk flexion in gluteus medius activation[94,115] nor the correlation between strength and electromyography. The potential for increased hip flexion to change the moment arm of the gluteus medius and gluteus maximus could negatively affect neuromuscular control at the hip and in consequence, at the knee.
Hewett et al., in a prospective study conducted with 205 female athletes, observed a greater peak external hip flexion moment during drop landings coupled with a tendency to lower maximum knee flexion angles (10.5° less) in the group that sustained ACL injury compared with the uninjured athletes.[34] Differences between sagittal plane knee flexion-extension moments and ACL injury status were not reported. However, since the sagittal plane may not be considered a primary predictor of ACL injury in females, it was speculated that the knee and hip joint are better prepared to act as a hinge in this plane. Thus, the musculature that limits sagittal plane trunk, hip and knee motion dissipates sagittal plane knee loads more effectively than coronal plane loads.
Similar to those findings reported by Hewett et al.,[34] Kernozek et al.[112] found no significant differences in hip flexion angles, hip extensor moments (internal) and knee moments and angles between males and females also following a drop jump. However, females demonstrated greater vertical and posterior GRF than males. This finding is in agreement with the stiffer landing style in females postulated by Decker et al.[90] Conversely, Salci et al.[116] reported decreased hip and knee flexion in female volleyball players during block and spike landings compared with males. Similar results were found by Schmitz et al.[117] in single-leg drop landings tasks, where females exhibited decreased hip and knee flexion angles compared with males. In contrast, Hewett et al.[118] did not find differences in hip sagittal plane kinetics and kinematics during single-leg horizontal hops, reinforcing the ‘hinge’ mechanism theory for sagittal plane. Theoretically, decreased hip and knee flexion may increase anterior shear forces and therefore ACL load.[81–86,119] Decreased hip flexion angles may inhibit hip extensor muscles, increasing quadriceps extensor torques. Greater GRF in combination with greater quadriceps force may increase the anterior translation force to the tibia excessively, especially near full knee extension,[81,82,84,85,119,120] where the ACL is at higher risk of injury.[31]
Only a few studies have examined sex differences in the biomechanics of the hip and knee exclusively in the sagittal plane during the cutting manoeuvre. McLean et al.[120] reported less hip and knee flexion angles in females compared with males in a side-cut manoeuvre with opposition. In contrast, Landry et al.[121] reported decreased hip flexion angles and smaller hip flexion moments in females compared with males, but no differences in knee flexion angles and moments during unanticipated side-cut manoeuvres.
Yu et al.[122] and Chappell et al.[123] reported decreased hip flexion with decreased knee flexion angles in females compared with males during vertical stop jumps. Although Yu et al.,[122] based on hip and knee angular velocities, suggested that GRF are more related to the motion than to the hip and knee angles, the role of joint positions in the risk of ACL injury has been well established, as joint angles may not only influence GRF but also force vectors of muscles. Controversially, Krosshaug et al.[93] reported greater hip and knee flexion in female basketball players than males at initial contact and at initial contact during landing tasks. Females demonstrated a 5.3-fold higher relative risk of sustaining a valgus collapse.[93] This increase in hip flexion has been previously related with greater knee valgus positions in females.[124,125]
In summary:
Trunk, arms and head position relative to hip, knee and ankle may influence GRF, energetics and knee load from a landing or cutting manoeuvre.
The gluteus maximus is an important controller of trunk flexion, and contributes to hip absorption at landing.
Females may land more erect compared with males, thus decreasing the hip absorption and, consequently, increasing knee and ankle loads.
4. Coronal Plane Evidence: Proximal Control of Knee Stability
4.1 Trunk Contributions
Minimal evidence exists regarding the influence of the trunk on the hip, knee and ankle. The video evidence of ACL injuries reported by Hewett et al.[125] shows that the female trunk usually moves lateral to the ACL-injured limb as the knee abducts, while this is not a common observation in males (figure 1). A possible close relationship between the position of the trunk and lower limb has been established by Dempsey et al.[124] The authors recently reported that sidestep cutting techniques influence peak valgus and internal rotation moments in healthy young male athletes (around 21 years old). A foot position away from the midline with the GRF lateral to the knee-joint centre and trunk leaning and rotating to the opposite direction with respect to the cut (displacing the centre of mass away from the plantar surface of the foot) may significantly increase lower-extremity valgus and internal rotation loads at the knee joint during the weight acceptance phase. Moreover, ipsilateral trunk lean may be a sign of weak hip abductors as it moves the centre of mass closer to the stance limb to reduce demand on the weak abductors,[126] therefore considerably affecting core stability and robustness.
Fig. 1.
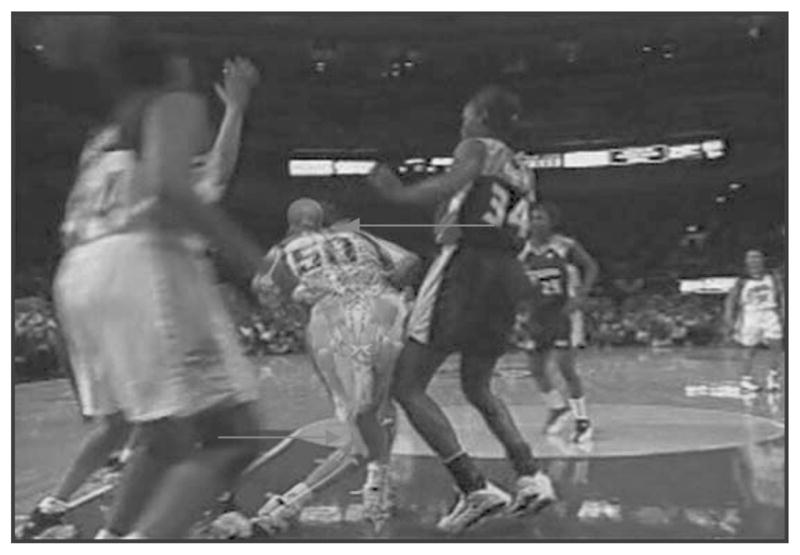
Photograph of an athlete sustaining an anterior cruciate ligament injury event, which illustrates a common mechanism of injury in female athletes, with trunk movement lateral to and away from the body’s midline as the knee collapses toward the midline.
Pollard et al.[127] speculated that females lean the trunk over the stance limb and agreed with the results of Dempsey et al.[124] who observed a displaced foot at initial contact among females who presented with greater external knee abduction during side cutting. Knee valgus has been found to be one of the strongest predictors of ACL injury in female athletes.[34] During single-leg landing and cutting, the entire body mass must be balanced over one lower extremity. Because the trunk, head and arms comprise greater than half of the body’s mass, lateral trunk motion increases GRF and knee abduction load. Therefore, technique modification and feedback would be an important element to include in prevention programmes to decrease knee valgus torque in sports involving side-step cutting.[126]
Zazulak et al.[128] reported that lateral displacement was a strong predictor of knee ligament injuries. Trunk displacement, proprioception and history of low back pain predicted knee ligament injury with 91% sensitivity and 68% specificity, and specific ACL injuries with 91% accuracy in female athletes. Low back pain may decrease force,[129–131] hip strength[132] and endurance,[133,134] and may alter activation patterns (preactivation and delayed reflex activation),[135–140] postural control,[141,142] trunk proprioception,[143–145] side-to-side weight-bearing symmetry[146] and gluteal activation.[147–149] Thus, low back pain may decrease the capability to react against a movement and may reduce trunk equilibrium and robustness. This may unexpectedly move the centre of mass and potentially excessively load the knee joint.
Zazulak et al.[128] employed open kinetic chain movements to detect proprioceptive deficits at the trunk. Most sport manoeuvres of the lower extremity are performed through closed kinetic chain movements, during which ACL injuries likely occur. Studies incorporating more functional tasks are needed to confirm these findings. However, the role of lateral trunk flexion in ACL injury risk remains controversial. Zeller et al.[150] reported that female athletes had a decreased amount of lateral trunk flexion in a kinematic study during single-legged squat compared with their male counterparts. This was related to a greater knee valgus angle presented during the same task in females.
Thus, core stability in the coronal plane may have a profound influence on distal joints. Deficits in neuromuscular control of the trunk during cutting and landing may lead to uncontrolled lateral trunk motion that may increase knee abduction motion and torque through mechanical (lateral GRF motion)[127,151] and neuromuscular (increased hip adductor torque)[34] mechanisms, consequently increasing strain on the ACL and leading to injury via either one or both of these mechanisms. Disturbances in trunk motions may increase the ACL injury risk by altering transmission of forces distally and by inducing deleterious joint positions. Core stability may be a crucial component of prevention programmes,[148] although further research is needed to better understand the exact role of coronal plane trunk biomechanics in the genesis of ACL injuries.
4.2 Hip Contributions
The contributions of the hip musculature to knee abduction have been studied in running, landing, squatting and side-step cutting manoeuvres. Female recreational athletes were found to have greater peak hip adduction angles with greater peak knee abduction angles when running compared with their male counterparts.[123,152] In contrast, hip moments may not differ between sexes for running actions.[123] During the landing preparation of a stop-jump task, Chappell et al.[123] found decreased hip abduction (also decreased hip flexion and hip external rotation) in female compared with male athletes. During the landing task itself, Blackburn and Padua[65] did not observe coronal plane biomechanical changes at hip and knee joints after increased trunk flexion during landing. A correlation between hip adduction moment and knee abduction moments in ACL-injured subjects (R = 0.69) was noted in females who subsequently injured their ACL.[34] An external hip abduction moment created by the GRF moving lateral to the centre of the femoral head is counterbalanced internally by hip adductor torque. Ford et al.[153] reported an increase in coronal excursion of the hip and knee after a single drop landing of approximately 13 cm, both medially and laterally, for females compared with males. In contrast, no sex differences for hip abduction at initial contact, maximum hip abduction or maximum hip adduction were reported. These results agree with findings of Pappas et al.,[154] who found less hip adduction in unilateral (one-legged) compared with bilateral (two-legged) landings despite similar ending position at the time of peak knee flexion. These authors did not observe differences between sexes in hip kinematics during single-legged landings. Significant correlations between coronal plane hip and knee initial contact angles during both types of landings were observed for females but not for males.[155] Considering all the presented data, hip and trunk excursions and trajectory may be more informative than the final position. Hewett et al. also assessed sex differences on hip kinetics and kinematics in single-legged landings.[155] The landing task consisted of three consecutive horizontal single-leg hops holding the position after the last one. Females demonstrated greater hip adduction angles at initial contact. The maximal adduction angles and external adduction moments at the hip were significantly greater for the first and second but not for the third hop. Landing sex differences were also reported by Jacobs et al.[156] during a more complex and functional task that mimics a high-risk posture for ACL injury. The task consisted of a double-legged, broad-jump landing on a single leg. Females had lower hip abduction compared with males, and moderate correlations were shown between hip abduction strength and knee valgus kinematics for females, but not for males.[156] In contrast, Padua et al.[157] examined the relationship between hip strength measured by hand-held dynamometer and joint kinematics during a drop jump task in 63 males and 54 females. The authors reported decreased gluteus medius and gluteus maximus strength that were related to greater knee valgus at initial contact and greater peak knee valgus. Therefore, hip abduction strength assessment may be a potential method to identify those subjects at risk of ACL injury at landing. Also, hip abduction strength programmes may decrease the risk of sustaining an ACL tear at landing. Overall, female soccer players were found to have a significant side-to-side disparity in hip abductor strength not present in males.[158]
In single-legged squat kinematics, Zeller et al.[150] reported that female athletes had an increased amount of hip adduction (with concomitant increase in knee valgus) when compared with males. In contrast, Nguyen[20] only found a trend toward more hip adduction in females, but no statistically significant sex differences were demonstrated in single-legged squat. Most of the data indicate that females have difficulties with hip control and also show the potential importance of gluteus medius strength and activation in order to stabilize the pelvis in single-leg, weight-bearing sport activities.
Studies have reported a significant increase in hip adduction moments in females concomitantly with greater knee valgus moments compared with males during side-step cutting.[121,159] Sigward and Powers[160] investigated the hip coronal plane kinematics in a group of females divided by the magnitude of external moment knee valgus during side-step cutting. Contrary to their primary hypothesis, females with excessive knee valgus moment demonstrated significantly larger hip abduction position at initial contact compared with the females with a normal valgus moment. The authors argued that more hip abduction angles may translate the centre of pressure laterally to the centre of mass of the tibia increasing the valgus moment. This may be understood as a dependent task strategy for side stepping to increase the foot width at initial contact, showing that foot positions may influence the kinetics and kinematics of proximal joints.[126,161] Despite speculating on the impact of the trunk on knee position, the position of the trunk was not analysed in their study.[160] Coronal plane hip biomechanics are not only affected by the task itself, but also by the situation in which the task is performed. Houck et al.[161] found that the unanticipated side-step movement was performed with greater hip adduction compared with the anticipated situation. However, the authors included male and female subjects within a single study group, thus, conclusions on sex differences are not possible. Imwalle et al.[162] investigated the lower-extremity motions in females also assessing the unanticipated cutting manoeuvres with running actions at an angle of 45° or 90°. The authors found that hip adduction was the only significant predictor of knee abduction for both situations.
Hip abduction torque differences between females and males have been observed in some studies,[49,114,157,163] but not in others.[113,164] Sex differences in hip abduction torques may explain the higher injury incidence in females. Intervention strategies that target sex differences hip adduction torques (increasing hip abduction strength) may optimize ACL injury prevention programmes, specifically for female athletes.[148]
It has yet to be definitively determined whether there is a relationship between hip abduction strength and lower-extremity valgus positioning. Proper functioning (strength and recruitment) of the posterior-lateral hip musculature is essential to provide proximal stability for lower-extremity motion during functional activities. Little to no correlation has been found between hip abduction torque[20,111,163,164] and gluteus medius activation[108,109] with knee valgus during different tasks. Measurement methods may explain these findings. Hip abductor strength is measured using isokinetic and hand-held dynamometer devices during open chain tasks, which differs from what occurs in athletic manoeuvres. Moreover, these studies did not control the influence of the trunk flexion in gluteus medius activation, which could influence the obtained results. Therefore, neuromuscular control of the hip in the coronal plane is required not only to stabilize the trunk and pelvis, but also the knee joint.
In summary:
Females and males have significantly different trunk and hip movements in the coronal plane during landing, squatting and side-step tasks. Specifically, females appear to exhibit movement patterns at the trunk that increase knee abduction.
Studies indicate that abduction at the knee joint predicts risk for ACL injury.
Deficits in neuromuscular control of the trunk and hip during cutting and landing may lead to uncontrolled lateral trunk motion.
Targeted neuromuscular training of the trunk and hip to reduce movements that contribute knee abduction may decrease injury risk.
5. Transverse Plane Evidence for Proximal Control of Knee-Joint Stability
5.1 Trunk Contributions
Investigations about the influence of transverse plane movements on the risk of ACL injury are scarce. Dempsey et al.[124] recently reported that placing the foot away from the midline while the trunk is leaning and rotating to the opposite direction to the cut significantly increased knee abduction and internal rotation loads at the knee in the weight acceptance phase. The rotation of the trunk transfers transverse plane motions to the hip through the pelvis, potentially producing hip adduction and internal rotation that may in turn induce knee abduction. These data coincide with the ‘position of no return’ described by Ireland[61] to explain a non-contact ACL injury mechanism and where Ireland warned against flexion and rotation to the opposite side of the trunk. In contrast, Blackburn and Padua[65] found no influence of trunk flexion at the hip and knee position in the transverse plane. No studies examining sex differences in the transverse plane trunk motions were found; therefore, further research is needed in this area.
5.2 Hip Contributions
Transverse plane hip contributions to knee biomechanics have been investigated in running, side-step cutting, and landing manoeuvres. Ferber et al.[151] reported significantly greater hip internal rotation angles and hip negative work in the transverse plane during running in female recreational athletes compared with males. However, Landry et al.[121] found that females produced a greater overall hip external rotation moment than did male subjects during the early stance phase of the unanticipated straight run. Position of the foot at initial contact may explain these contradictory data.
The contribution of the hip musculature during side-step cutting is supported by findings of McLean et al.,[159] who showed that the peak knee abduction moment was more sensitive to initial hip internal rotation and knee abduction position (R = 0.76) in females compared with males. These findings are in agreement with those reported by Sigward and Powers[160] who found significantly greater hip internal rotation and greater internally rotated foot at initial contact in the excessive valgus moment compared with a normal valgus group during side-step cutting. During the same manoeuvre, Pollard et al.[149] reported that female athletes demonstrated significantly greater hip internal rotation angles at early deceleration compared with male athletes. In contrast, Landry et al.[121] reported that female subjects sustained a larger hip external rotation moment than male subjects during the early stance phase of an unanticipated side-cutting manoeuvre. However, the moment magnitudes were much smaller than the maximal moments reached later in midstance phase. It remains unclear if these moment differences at the smaller magnitudes during early stance serve as potential risk factors for ACL injury.
For landing tasks, Lephart et al.[164] found that females exhibited significantly lower leg internal rotation maximum angular displacement for both single-leg landing and forward hop. Specifically, for the single-leg land, females had significantly greater hip internal rotation maximum angular displacement, and less lower leg internal rotation time to maximum angular displacement compared with males.[164] For the forward hop, females had significantly greater hip rotation time to maximum angular displacement than males.[164] Surprisingly, Pollard et al.[149] reported changes in the hip, but not in the knee, after in-season neuromuscular training. Interestingly, the authors demonstrated how hip internal rotation may be decreased after an adequate neuromuscular training, as they found 6.2° decreases in hip internal rotation and 2.8° greater hip abduction angles during the early deceleration phase of landing following the season, without differences in knee valgus and flexion angles. Although the authors did not assess sex differences in hip contributions to knee-joint motions, these results point out the relevance of prevention programmes to decrease the risk of ACL injury. During vertical stop jump tasks, Chappell et al.[123] found decreased hip external rotation and increased knee internal rotation angles in females compared with males at landing. In contrast, Nguyen[20] did not observe significantly greater hip internal excursion in females compared with males during a single-leg squat, although differences in the assessed task may explain differing results. Sex differences in hip or trunk contribution to knee-joint motions are likely task-dependent.
The gluteus maximus and gluteus medius act synergistically to stabilize the pelvis in all planes of motion and control rotation at the hip, especially in single-leg stance. While the gluteus medius is the primary abductor of the hip, the gluteus maximus functions primarily as an extensor and, secondarily, as an external rotator of the hip. Decreased activation of proximal stabilizing muscles may lower load-bearing capacity of the knee joint and predispose it to injury. Zazulak et al.[108] found decreased gluteus maximus electromyographic activity at landing in female soccer, basketball and volleyball players compared with males. Gluteal muscles are able to change their functions depending on the hip position.[91] Therefore, it would be desirable to monitor and provide information about hip and trunk position when considering the activation of these musculatures.
Females demonstrated decreased values in hip external rotation strength compared with males measured with a hand-held dynamometer.[49,165] In contrast, Claiborne et al.[111] did not find differences in hip musculature strength measured with isokinetics when normalized to body mass. Weakness or poor neuromuscular control in hip external rotators in females may increase the injury risk of the lower extremity, as reported by Leetun et al.[49] Core stability was used synonymously with isometric hip strength.[49]
To affirm this contention, information and interrelation of all components involved in neuromuscular control of the core would be necessary. Lawrence et al.[165] studied hip external rotation strength on kinematic and kinetic variables during single-leg drop landings in females. The authors stratified the group of females according to ‘strong’ or ‘weak’ hip external rotation strength with a hand-held dynamometer. The ‘strong’ group demonstrated significantly lower peak vertical GRF and external knee flexor moment. The ‘weak’ group had significantly greater external knee adduction moment, net knee anterior shear joint reaction force and a greater hip external adduction moment. Therefore, this study demonstrated that hip strength may be related to high-risk landing strategies and highlights the importance of the hip external rotators at potentially preventing ACL injuries.[165] However, caution must be taken when interpreting these results due to the limitations of hand-held dynamometry with open kinetic chain measurements.
In summary:
The rotation of the trunk transfers transverse plane motions to the hip through the pelvis, potentially producing hip adduction and internal rotation that may in turn induce knee abduction.
There is minimal evidence examining sex differences in the transverse plane trunk motions.
Peak knee abduction moment appears to be more sensitive to initial hip internal rotation and knee abduction position in females.
Weakness or poor neuromuscular control in hip external rotators in females may increase the injury risk of the lower extremity.
6. Conclusions
This review has focused on the contributions of proximal controllers of the trunk and hip- to knee-joint motions. Sex differences in the biomechanics of trunk and hip in sagittal, coronal and transverse planes have been identified and discussed. We have used this approach to better understand the neuromuscular imbalances and the higher incidence of ACL injury observed in female athletes. Considering the increased risk of radiographically diagnosed knee osteoarthritis following ACL injury, regardless of whether the ligament is reconstructed or not, prevention is currently the only effective treatment for this devastating athletic injury. Based on the presented evidence, the following conclusions can be generated regarding sex-based differences in the proximal control of the knee joint:
The risk of ACL injury likely results from a combination of disturbances in all three planes of motion.
Females may land with less trunk and hip flexion compared with males, which results in decreased energy absorption capacity of the musculoskeletal system.
GRF (normalized) at landing may be higher in females compared with males. Greater reaction forces with the hip and knee flexion angles near extension may overload the ACL and place it at high risk of injury.
The lateral displacement of the trunk centre of mass away from the knee joint may increase knee valgus and can potentially increase ACL injury risk.
Females may show greater hip adduction while performing sport manoeuvres (running, landing, squatting and cutting), which may increase knee valgus and hip internal rotation and place the ACL at increased risk of rupture.
Hip strength training may decrease the risk of ACL injury by modifying high-risk positions about the knee.
The influence of transverse plane trunk biomechanics on the knee joint needs to be further studied, as little evidence has been reported in the literature.
Significantly greater hip internal rotation has been reported among females compared with males during running, side-step cutting and landing, and is related to knee abduction in female athletes.
Proximal control of the knee joint is sex and task dependent.
Prevention programmes targeted towards trunk and hip neuromuscular control may help decrease the risk of ACL injuries in athletes, especially female athletes.
Acknowledgments
The authors acknowledge funding support from National Institutes of Health/NIAMS Grants R01-AR049735, R01-AR05563, R01-AR056259 and R03-AR057551.
Footnotes
The authors have no conflicts of interest that are directly relevant to the content of this review.
References
- 1.NCAA. [Accessed 2010 Dec 28];NCAA injury surveillance system summary [online] Available from URL: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1941300/
- 2.Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer: NCAA data and review of literature. Am J Sports Med. 1995;23( 6):694–701. doi: 10.1177/036354659502300611. [DOI] [PubMed] [Google Scholar]
- 3.Malone TR, Hardaker WT, Garrett WE, et al. Relationship of gender to anterior cruciate ligament injuries in intercollegiate basketball players. J South Orthop Assoc. 1993;2( 1):36–9. [Google Scholar]
- 4.Myklebust G, Maehlum S, Holm I, et al. A prospective cohort study of anterior cruciate ligament injuries in elite Norwegian team handball. Scand J Med Sci Sports. 1998;8( 3):149–53. doi: 10.1111/j.1600-0838.1998.tb00185.x. [DOI] [PubMed] [Google Scholar]
- 5.Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med. 1999 Mar;27( 3):143–56. doi: 10.2165/00007256-199927030-00001. [DOI] [PubMed] [Google Scholar]
- 6.Lohmander LS, Englund PM, Dahl LL, et al. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007 Oct;35( 10):1756–69. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 7.Myklebust G, Engebretsen L, Braekken IH, et al. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003 Mar;13( 2):71–8. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 8.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004 Mar;63( 3):269–73. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cumps E, Verhagen E, Annemans L, et al. Injury rate and socioeconomic costs resulting from sports injuries in Flanders: data derived from sports insurance statistics 2003. Br J Sports Med. 2008 Sep;42( 9):767–72. doi: 10.1136/bjsm.2007.037937. [DOI] [PubMed] [Google Scholar]
- 10.de Loes M, Dahlstedt LJ, Thomee R. A 7-year study on risks and costs of knee injuries in male and female youth participants in 12 sports. Scand J Med Sci Sports. 2000;10( 2):90–7. doi: 10.1034/j.1600-0838.2000.010002090.x. [DOI] [PubMed] [Google Scholar]
- 11.Hewett TE, Stroupe AL, Nance TA, et al. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24( 6):765–73. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 12.Knowles SB, Marshall SW, Miller T, et al. Cost of injuries from a prospective cohort study of North Carolina high school athletes. Inj Prev. 2007 Dec;13( 6):416–21. doi: 10.1136/ip.2006.014720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freedman KB, Glasgow MT, Glasgow SG, et al. Anterior cruciate ligament injury and reconstruction among university students. Clin Orthop Related Res. 1998;356:208–12. doi: 10.1097/00003086-199811000-00028. [DOI] [PubMed] [Google Scholar]
- 14.Trentacosta N, Vitale M, Ahmad C. The effects of timing of pediatric knee ligament surgery on short-term academic performance in school-aged athletes. Am J Sports Med. 2009;37( 9):1684–91. doi: 10.1177/0363546509332507. [DOI] [PubMed] [Google Scholar]
- 15.Allen MK, Glasoe WM. Metrecom measurement of navicular drop in subjects with anterior cruciate ligament injury. J Athl Train. 2000 Oct;35( 4):403–6. [PMC free article] [PubMed] [Google Scholar]
- 16.Gray J, Taunton JE, McKenzie DC, et al. A survey of injuries to the anterior cruciate ligament of the knee in female basketball players. Int J Sports Med. 1985 Dec;6( 6):314–6. doi: 10.1055/s-2008-1025861. [DOI] [PubMed] [Google Scholar]
- 17.Haycock CE, Gillette JV. Susceptibility of women athletes to injury: myth vs. reality. JAMA. 1976;236( 2):163–5. [PubMed] [Google Scholar]
- 18.Loudon JK, Jenkins W, Loudon KL. The relationship between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther. 1996 Aug;24( 2):91–7. doi: 10.2519/jospt.1996.24.2.91. [DOI] [PubMed] [Google Scholar]
- 19.Muneta T, Ezura Y, Sekiya I, et al. Anterior knee laxity and loss of extension after anterior cruciate ligament injury. Am J Sports Med. 1996 Sep-Oct;24(5):603–7. doi: 10.1177/036354659602400507. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen AD. Effects of lower extremity posture on hip strength and their influence on lower extremity motion during a single leg squat [dissertation] Greensboro (NC): University of North Carolina at Greensboro; 2007. [Google Scholar]
- 21.Rizzo M, Holler SB, Bassett FH., 3rd Comparison of males’ and females’ ratios of anterior-cruciate-ligament width to femoral-intercondylar-notch width: a cadaveric study. Am J Orthop (Belle Mead NJ) 2001 Aug;30( 8):660–4. [PubMed] [Google Scholar]
- 22.Tillman MD, Bauer JA, Cauraugh JH, et al. Differences in lower extremity alignment between males and females: potential predisposing factors for knee injury. J Sports Med Phys Fitness. 2005 Sep;45( 3):355–9. [PubMed] [Google Scholar]
- 23.Zelisko JA, Noble HB, Porter M. A comparison of men’s and women’s professional basketball injuries. Am J Sports Med. 1982 Sep-Oct;10(5):297–9. doi: 10.1177/036354658201000507. [DOI] [PubMed] [Google Scholar]
- 24.Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34:86–92. [PMC free article] [PubMed] [Google Scholar]
- 25.Chaudhari AM, Lindenfeld TN, Andriacchi TP, et al. Knee and hip loading patterns at different phases in the menstrual cycle: implications for the gender difference in anterior cruciate ligament injury rates. Am J Sports Med. 2007 May;35( 5):793–800. doi: 10.1177/0363546506297537. [DOI] [PubMed] [Google Scholar]
- 26.Hewett TE, Zazulak BT, Myer GD. Effects of the menstrual cycle on anterior cruciate ligament injury risk: a systematic review. Am J Sports Med. 2007 Feb 9;35( 4):659–68. doi: 10.1177/0363546506295699. [DOI] [PubMed] [Google Scholar]
- 27.Shultz SJ, Windley TC, Kulas AS, et al. Low levels of anterior tibial loading enhance knee extensor reflex response characteristics. J Electromyogr Kinesiol. 2005 Feb;15( 1):61–71. doi: 10.1016/j.jelekin.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 28.Slauterbeck JL, Fuzie SF, Smith MP, et al. The menstrual cycle, sex hormones, and anterior cruciate ligament injury. J Athl Train. 2002;37( 3):275–8. [PMC free article] [PubMed] [Google Scholar]
- 29.Wojtys EM, Huston LJ, Boynton MD, et al. The effect of the menstrual cycle on anterior cruciate ligament injuries in women as determined by hormone levels. Am J Sports Med. 2002 Mar-Apr;30(2):182–8. doi: 10.1177/03635465020300020601. [DOI] [PubMed] [Google Scholar]
- 30.Wojtys EM, Huston LJ, Lindenfeld TN, et al. Association between the menstrual cycle and anterior cruciate ligament injuries in female athletes. Am J Sports Med. 1998 Sep-Oct;26(5):614–9. doi: 10.1177/03635465980260050301. [DOI] [PubMed] [Google Scholar]
- 31.Boden BP, Dean GS, Feagin JA, et al. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23( 6):573–8. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 32.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003 Oct;35( 10):1745–50. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 33.Hewett TE, Lindenfeld TN, Riccobene JV, et al. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999 Nov-Dec;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 34.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005 Feb 8;33( 4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 35.Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, Jan 2005. Am J Sports Med. 2006 Sep;34( 9):1512–32. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 36.Gilchrist JR, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent non-contact ACL injury in female collegiate soccer players. Am J Sports Med. 2008;36( 8):1476–83. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 37.Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: part 2 – a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006 Dec 28;34( 3):490–8. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 38.Mandelbaum BR, Silvers HJ, Watanabe D, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing the incidence of ACL injuries in female athletes: two-year follow up. Am J Sport Med. 2005;33( 6):1003–10. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 39.Zazulak B, Cholewicki J, Reeves NP. Neuromuscular control of trunk stability: clinical implications for sports injury prevention. J Am Acad Orthop Surg. 2008 Sep;16( 9):497–505. [PubMed] [Google Scholar]
- 40.Putnam CA. Sequential motions of body segments in striking and throwing skills: descriptions and explanations. J Biomech. 1993;26(Suppl 1):125–35. doi: 10.1016/0021-9290(93)90084-r. [DOI] [PubMed] [Google Scholar]
- 41.Zazulak BT, Hewett TE, Reeves NP, et al. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007 Mar;35( 3):368–73. doi: 10.1177/0363546506297909. [DOI] [PubMed] [Google Scholar]
- 42.Granata KP, Slota GP, Bennett BC. Paraspinal muscle reflex dynamics. J Biomech. 2004 Feb;37( 2):241–7. doi: 10.1016/s0021-9290(03)00249-5. [DOI] [PubMed] [Google Scholar]
- 43.Moorhouse KM, Granata KP. Role of reflex dynamics in spinal stability: intrinsic muscle stiffness alone is insufficient for stability. J Biomech. 2007;40( 5):1058–65. doi: 10.1016/j.jbiomech.2006.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reeves NP, Narendra KS, Cholewicki J. Spine stability: the six blind men and the elephant. Clin Biomech (Bristol, Avon) 2007 Mar;22( 3):266–74. doi: 10.1016/j.clinbiomech.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med. 2006;36( 3):189–98. doi: 10.2165/00007256-200636030-00001. [DOI] [PubMed] [Google Scholar]
- 46.Novacheck TF. The biomechanics of running. Gait Posture. 1998 Jan 1;7( 1):77–95. doi: 10.1016/s0966-6362(97)00038-6. [DOI] [PubMed] [Google Scholar]
- 47.Amaro A, Amado F, Duarte JA, et al. Gluteus medius muscle atrophy is related to contralateral and ipsilateral hip joint osteoarthritis. Int J Sports Med. 2007 Dec;28( 12):1035–9. doi: 10.1055/s-2007-965078. [DOI] [PubMed] [Google Scholar]
- 48.Fredericson M, Cookingham CL, Chaudhari AM, et al. Hip abductor weakness in distance runners with iliotibial band syndrome. Clin J Sport Med. 2000 Jul;10( 3):169–75. doi: 10.1097/00042752-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 49.Leetun DT, Ireland ML, Willson JD, et al. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004 Jun;36( 6):926–34. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- 50.Maffey L, Emery C. What are the risk factors for groin strain injury in sport? A systematic review of the literature. Sports Med. 2007;37( 10):881–94. doi: 10.2165/00007256-200737100-00004. [DOI] [PubMed] [Google Scholar]
- 51.Nadler SF, Malanga GA, DePrince M, et al. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med. 2000 Apr;10( 2):89–97. doi: 10.1097/00042752-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 52.Noehren B, Davis I, Hamill J. ASB clinical biomechanics award winner 2006 prospective study of the biomechanical factors associated with iliotibial band syndrome. Clin Biomech (Bristol, Avon) 2007 Nov;22( 9):951–6. doi: 10.1016/j.clinbiomech.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 53.Robinson RL, Nee RJ. Analysis of hip strength in females seeking physical therapy treatment for unilateral patello-femoral pain syndrome. J Orthop Sports Phys Ther. 2007 May;37( 5):232–8. doi: 10.2519/jospt.2007.2439. [DOI] [PubMed] [Google Scholar]
- 54.Hewett TE, Myer GD, Ford KR, et al. Dynamic neuromuscular analysis training for preventing anterior cruciate ligament injury in female athletes. Instr Course Lect. 2007;56:397–406. [PubMed] [Google Scholar]
- 55.Mascal CL, Landel R, Powers C. Management of patello-femoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J Orthop Sports Phys Ther. 2003 Nov;33( 11):647–60. doi: 10.2519/jospt.2003.33.11.647. [DOI] [PubMed] [Google Scholar]
- 56.Myer GD, Brent JL, Ford KR, et al. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. Br J Sports Med. 2008;42( 7):614–9. doi: 10.1136/bjsm.2007.046086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004 Mar;34( 3):116–25. doi: 10.2519/jospt.2004.34.3.116. [DOI] [PubMed] [Google Scholar]
- 58.Tyler TF, Nicholas SJ, Mullaney MJ, et al. The role of hip muscle function in the treatment of patellofemoral pain syndrome. Am J Sports Med. 2006 Apr;34( 4):630–6. doi: 10.1177/0363546505281808. [DOI] [PubMed] [Google Scholar]
- 59.Verrall GM, Slavotinek JP, Fon GT, et al. Outcome of conservative management of athletic chronic groin injury diagnosed as pubic bone stress injury. Am J Sports Med. 2007 Mar;35( 3):467–74. doi: 10.1177/0363546506295180. [DOI] [PubMed] [Google Scholar]
- 60.Brown SH, Vera-Garcia FJ, McGill SM. Effects of abdominal muscle coactivation on the externally preloaded trunk: variations in motor control and its effect on spine stability. Spine. 2006 Jun 1;31( 13):E387–93. doi: 10.1097/01.brs.0000220221.57213.25. [DOI] [PubMed] [Google Scholar]
- 61.Ireland ML. Anterior cruciate ligament injury in female athletes: epidemiology. J Athl Train. 1999 Apr;34( 2):150–4. [PMC free article] [PubMed] [Google Scholar]
- 62.de Leva P. Joint center longitudinal positions computed from a selected subset of Chandler’s data. J Biomech. 1996 Sep;29( 9):1231–3. doi: 10.1016/0021-9290(96)00021-8. [DOI] [PubMed] [Google Scholar]
- 63.Tanner JM, Davies PS. Clinical longitudinal standards for height and height velocity for North American children. J Pediatr. 1985;107( 3):317–29. doi: 10.1016/s0022-3476(85)80501-1. [DOI] [PubMed] [Google Scholar]
- 64.DeVita P, Skelly WA. Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Med Sci Sports Exerc. 1992;24( 1):108–15. [PubMed] [Google Scholar]
- 65.Blackburn JT, Padua DA. Influence of trunk flexion on hip and knee joint kinematics during a controlled drop landing. Clin Biomech (Bristol, Avon) 2008 Mar;23( 3):313–9. doi: 10.1016/j.clinbiomech.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 66.Blackburn JT, Padua DA. Sagittal-plane trunk position, landing forces, and quadriceps electromyographic activity. J Athl Train. 2009 Mar-Apr;44(2):174–9. doi: 10.4085/1062-6050-44.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ohkoshi Y, Yasuda K, Kaneda K, et al. Biomechanical analysis of rehabilitation in the standing position. Am J Sports Med. 1991 Nov-Dec;19(6):605–11. doi: 10.1177/036354659101900609. [DOI] [PubMed] [Google Scholar]
- 68.Withrow TJ, Huston LJ, Wojtys EM, et al. Effect of varying hamstring tension on anterior cruciate ligament strain during in vitro impulsive knee flexion and compression loading. J Bone Joint Surg. 2008 Apr;90( 4):815–23. doi: 10.2106/JBJS.F.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cramer JT, Housh TJ, Weir JP, et al. The acute effects of static stretching on peak torque, mean power output, electromyography, and mechanomyography. Eur J Appl Physiol. 2005 Mar;93( 5–6):530–9. doi: 10.1007/s00421-004-1199-x. [DOI] [PubMed] [Google Scholar]
- 70.Nelson AG, Allen JD, Cornwell A, et al. Inhibition of maximal voluntary isometric torque production by acute stretching is joint-angle specific. Res Q Exerc Sport. 2001 Mar;72( 1):68–70. doi: 10.1080/02701367.2001.10608934. [DOI] [PubMed] [Google Scholar]
- 71.Behm DG, Bambury A, Cahill F, et al. Effect of acute static stretching on force, balance, reaction time, and movement time. Med Sci Sports Exerc. 2004 Aug;36( 8):1397–402. doi: 10.1249/01.mss.0000135788.23012.5f. [DOI] [PubMed] [Google Scholar]
- 72.Cramer JT, Beck TW, Housh TJ, et al. Acute effects of static stretching on characteristics of the isokinetic angle-torque relationship, surface electromyography, and mechanomyography. J Sports Sci. 2007 Apr;25( 6):687–98. doi: 10.1080/02640410600818416. [DOI] [PubMed] [Google Scholar]
- 73.Evetovich TK, Nauman NJ, Conley DS, et al. Effect of static stretching of the biceps brachii on torque, electromyography, and mechanomyography during concentric isokinetic muscle actions. J Strength Cond Res. 2003 Aug;17( 3):484–8. doi: 10.1519/1533-4287(2003)017<0484:eossot>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 74.Ford KR. A comparison of knee joint kinematics and related muscle onset patterns observed during a 180° cutting maneuver executed by male and female soccer players. Lexington (KY): University of Kentucky; 1997. [Google Scholar]
- 75.Riemann BL, Lephart SM. The sensorimotor system, part II: the role of proprioception in motor control and functional joint stability. J Athl Train. 2002 Jan;37( 1):80–4. [PMC free article] [PubMed] [Google Scholar]
- 76.Williams GN, Chmielewski T, Rudolph K, et al. Dynamic knee stability: current theory and implications for clinicians and scientists. J Orthop Sports Phys Ther. 2001 Oct;31( 10):546–66. doi: 10.2519/jospt.2001.31.10.546. [DOI] [PubMed] [Google Scholar]
- 77.Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players, part 2: a review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009 Aug;17( 8):859–79. doi: 10.1007/s00167-009-0823-z. [DOI] [PubMed] [Google Scholar]
- 78.Myer GD, Ford KR, Paterno MV, et al. The effects of generalized joint laxity on risk of ACL injury in young female athletes. Am J Sports Med. 2008 Jun;36( 6):1073–80. doi: 10.1177/0363546507313572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ramesh R, Von Arx O, Azzopardi T, et al. The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Joint Surg Br. 2005 Jun;87( 6):800–3. doi: 10.1302/0301-620X.87B6.15833. [DOI] [PubMed] [Google Scholar]
- 80.Uhorchak JM, Scoville CR, Williams GN, et al. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003 Nov-Dec;31(6):831–42. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 81.Cerulli G, Benoit DL, Lamontagne M, et al. In vivo anterior cruciate ligament strain behaviour during a rapid deceleration movement: case report. Knee Surg Sports Traumatol Arthrosc. 2003 Sep;11( 5):307–11. doi: 10.1007/s00167-003-0403-6. [DOI] [PubMed] [Google Scholar]
- 82.DeMorat G, Weinhold P, Blackburn T, et al. Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury. Am J Sports Med. 2004 Mar;32( 2):477–83. doi: 10.1177/0363546503258928. [DOI] [PubMed] [Google Scholar]
- 83.Durselen L, Claes L, Kiefer H. The influence of muscle forces and external loads on cruciate ligament strain. Am J Sports Med. 1995 Jan-Feb;23(1):129–36. doi: 10.1177/036354659502300122. [DOI] [PubMed] [Google Scholar]
- 84.Fleming BC, Beynnon BD. In vivo measurement of ligament/tendon strains and forces: a review. Ann Biomed Eng. 2004 Mar;32( 3):318–28. doi: 10.1023/b:abme.0000017542.75080.86. [DOI] [PubMed] [Google Scholar]
- 85.Markolf KL, Burchfield DM, Shapiro MM, et al. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995 Nov;13( 6):930–5. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 86.Renstrom P, Arms SW, Stanwyck TS, et al. Strain within the anterior cruciate ligament during hamstring and quadriceps activity. Am J Sports Med. 1986 Jan-Feb;14(1):83–7. doi: 10.1177/036354658601400114. [DOI] [PubMed] [Google Scholar]
- 87.Shelburne KB, Pandy MG, Torry MR. Comparison of shear forces and ligament loading in the healthy and ACL-deficient knee during gait. J Biomech. 2004 Mar;37( 3):313–9. doi: 10.1016/j.jbiomech.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 88.Kulas A, Zalewski P, Hortobagyi T, et al. Effects of added trunk load and corresponding trunk position adaptations on lower extremity biomechanics during drop-landings. J Biomech. 2008;41( 1):180–5. doi: 10.1016/j.jbiomech.2007.06.027. [DOI] [PubMed] [Google Scholar]
- 89.Farrokhi S, Pollard CD, Souza RB, et al. Trunk position influences the kinematics, kinetics, and muscle activity of the lead lower extremity during the forward lunge exercise. J Orthop Sports Phys Ther. 2008 Jul;38( 7):403–9. doi: 10.2519/jospt.2008.2634. [DOI] [PubMed] [Google Scholar]
- 90.Decker MJ, Torry MR, Wyland DJ, et al. Gender differences in lower extremity kinematics, kinetics and energy absorption during landing. Clin Biomech. 2003 Aug;18( 7):662–9. doi: 10.1016/s0268-0033(03)00090-1. [DOI] [PubMed] [Google Scholar]
- 91.Delp SL, Hess WE, Hungerford DS, et al. Variation of rotation moment arms with hip flexion. J Biomech. 1999 May;32( 5):493–501. doi: 10.1016/s0021-9290(99)00032-9. [DOI] [PubMed] [Google Scholar]
- 92.Huston LJ, Vibert B, Ashton-Miller JA, et al. Gender differences in knee angle when landing from a drop-jump. Am J Knee Surg. 2001 Fall;14( 4):215–9. [PubMed] [Google Scholar]
- 93.Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007 Mar;35( 3):359–67. doi: 10.1177/0363546506293899. [DOI] [PubMed] [Google Scholar]
- 94.Kulas AS, Schmitz RJ, Shultz SJ, et al. Sex-specific abdominal activation strategies during landing. J Athl Train. 2006 Oct-Dec;41(4):381–6. [PMC free article] [PubMed] [Google Scholar]
- 95.Hall L, Tsao H, MacDonald D, et al. Immediate effects of co-contraction training on motor control of the trunk muscles in people with recurrent low back pain. J Electromyogr Kinesiol. 2009 Oct;19( 5):763–73. doi: 10.1016/j.jelekin.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 96.Hodges PW. Changes in motor planning of feedforward postural responses of the trunk muscles in low back pain. Exp Brain Res. 2001 Nov;141( 2):261–6. doi: 10.1007/s002210100873. [DOI] [PubMed] [Google Scholar]
- 97.Kavcic N, Grenier S, McGill SM. Determining the stabilizing role of individual torso muscles during rehabilitation exercises. Spine (Phila Pa 1976) 2004 Jun 1;29( 11):1254–65. doi: 10.1097/00007632-200406010-00016. [DOI] [PubMed] [Google Scholar]
- 98.McGill SM. Low back stability: from formal description to issues for performance and rehabilitation. Exerc Sport Sci Rev. 2001;29( 1):26–31. doi: 10.1097/00003677-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 99.Cholewicki J, Greene HS, Polzhofer GK, et al. Neuro-muscular function in athletes following recovery from a recent acute low back injury. J Orthop Sports Phys Ther. 2002 Nov;32( 11):568–75. doi: 10.2519/jospt.2002.32.11.568. [DOI] [PubMed] [Google Scholar]
- 100.Cholewicki J, McGill SM. Mechanical stability of the in vivo lumbar spine: implications for injury and chronic low back pain. Clin Biomech (Bristol, Avon) 1996 Jan;11( 1):1–15. doi: 10.1016/0268-0033(95)00035-6. [DOI] [PubMed] [Google Scholar]
- 101.Lieberman DE, Raichlen DA, Pontzer H, et al. The human gluteus maximus and its role in running. J Exp Biol. 2006 Jun;209( Pt 11):2143–55. doi: 10.1242/jeb.02255. [DOI] [PubMed] [Google Scholar]
- 102.Vera-Garcia FJ, Brown SH, Gray JR, et al. Effects of different levels of torso coactivation on trunk muscular and kinematic responses to posteriorly applied sudden loads. Clin Biomech (Bristol, Avon) 2006 Jun;21( 5):443–55. doi: 10.1016/j.clinbiomech.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 103.Zhang SN, Bates BT, Dufek JS. Contributions of lower extremity joints to energy dissipation during landings. Med Sci Sports Exerc. 1998;32( 4):812–9. doi: 10.1097/00005768-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 104.Oddsson L, Thorstensson A. Fast voluntary trunk flexion movements in standing: primary movements and associated postural adjustments. Acta Physiol Scand. 1986 Nov;128( 3):341–9. doi: 10.1111/j.1748-1716.1986.tb07987.x. [DOI] [PubMed] [Google Scholar]
- 105.Grasso R, Zago M, Lacquaniti F. Interactions between posture and locomotion: motor patterns in humans walking with bent posture versus erect posture. J Neurophysiol. 2000 Jan;83( 1):288–300. doi: 10.1152/jn.2000.83.1.288. [DOI] [PubMed] [Google Scholar]
- 106.Huston LJ, Wojtys EM. Neuromuscular performance characteristics in elite female athletes. Am J Sports Med. 1996;24( 4):427–36. doi: 10.1177/036354659602400405. [DOI] [PubMed] [Google Scholar]
- 107.Paul JA, Salle H, Frings-Dresen MH. Effect of posture on hip joint moment during pregnancy, while performing a standing task. Clin Biomech (Bristol, Avon) 1996 Mar;11( 2):111–5. doi: 10.1016/0268-0033(95)00049-6. [DOI] [PubMed] [Google Scholar]
- 108.Zazulak BT, Ponce PL, Straub SJ, et al. Gender comparison of hip muscle activity during single-leg landing. J Orthop Sports Phys Ther. 2005 May;35( 5):292–9. doi: 10.2519/jospt.2005.35.5.292. [DOI] [PubMed] [Google Scholar]
- 109.Russell KA, Palmieri RM, Zinder SM, et al. Sex differences in valgus knee angle during a single-leg drop jump. J Athl Train. 2006 Apr-Jun;41(2):166–71. [PMC free article] [PubMed] [Google Scholar]
- 110.Cahalan TD, Johnson ME, Liu SH, et al. Quantitative measurements of hip strength in different age groups. Clin Orthop. 1989;246:136–45. [PubMed] [Google Scholar]
- 111.Claiborne TL, Armstrong CW, Gandhi V, et al. Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech. 2006 Feb;22( 1):41–50. doi: 10.1123/jab.22.1.41. [DOI] [PubMed] [Google Scholar]
- 112.Kernozek TW, Torry MR, Van Hoof H, et al. Gender differences in frontal and sagittal plane biomechanics during drop landings. Med Sci Sports Exerc. 2005 Jun;37( 6):1003–12. [PubMed] [Google Scholar]
- 113.Schmitz RJ, Riemann BL, Thompson T. Gluteus medius activity during isometric closed-chain hip rotation. J Sport Rehab. 2002;11:179–88. [Google Scholar]
- 114.Wilson JD, Ireland ML, Davis IM. Core strength and lower extremity alignment during single leg squats. Med Sci Sports Exerc. 2006 May;38( 5):945–52. doi: 10.1249/01.mss.0000218140.05074.fa. [DOI] [PubMed] [Google Scholar]
- 115.Shelburne KB, Pandy MG, Anderson FC, et al. Pattern of anterior cruciate ligament force in normal walking. J Biomech. 2004 Jun;37( 6):797–805. doi: 10.1016/j.jbiomech.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 116.Salci Y, Kentel BB, Heycan C, et al. Comparison of landing maneuvers between male and female college volleyball players. Clin Biomech (Bristol, Avon) 2004 Jul;19( 6):622–8. doi: 10.1016/j.clinbiomech.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 117.Schmitz RJ, Kulas AS, Perrin DH, et al. Sex differences in lower extremity biomechanics during single leg landings. Clin Biomech (Bristol, Avon) 2007 Jul;22( 6):681–8. doi: 10.1016/j.clinbiomech.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 118.Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes, part 1: mechanisms and risk factors. Am J Sports Med. 2006 Feb;34( 2):299–311. doi: 10.1177/0363546505284183. [DOI] [PubMed] [Google Scholar]
- 119.Olsen OE, Myklebust G, Engebretsen L, et al. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004 Jun;32( 4):1002–12. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 120.McLean SG, Lipfert SW, van den Bogert AJ. Effect of gender and defensive opponent on the biomechanics of sidestep cutting. Med Sci Sports Exerc. 2004 Jun;36( 6):1008–16. doi: 10.1249/01.mss.0000128180.51443.83. [DOI] [PubMed] [Google Scholar]
- 121.Landry SC, McKean KA, Hubley-Kozey CL, et al. Neuromuscular and lower limb biomechanical differences exist between male and female elite adolescent soccer players during an unanticipated side-cut maneuver. Am J Sports Med. 2007 Nov;35( 11):1888–900. doi: 10.1177/0363546507300823. [DOI] [PubMed] [Google Scholar]
- 122.Yu B, Lin CF, Garrett WE. Lower extremity biomechanics during the landing of a stop-jump task. Clin Biomech (Bristol, Avon) 2006 Mar;21( 3):297–305. doi: 10.1016/j.clinbiomech.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 123.Chappell JD, Creighton RA, Giuliani C, et al. Kinematics and electromyography of landing preparation in vertical stop-jump: risks for noncontact anterior cruciate ligament injury. Am J Sports Med. 2007 Feb;35( 2):235–41. doi: 10.1177/0363546506294077. [DOI] [PubMed] [Google Scholar]
- 124.Dempsey AR, Lloyd DG, Elliot BC, et al. The effect of technique change on knee loads during sidestep cutting. Med Sci Sports Exerc. 2007;39( 10):1811–6. doi: 10.1249/mss.0b013e31812f56d1. [DOI] [PubMed] [Google Scholar]
- 125.Hewett TE, Torg J, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43( 6):417–22. doi: 10.1136/bjsm.2009.059162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Dempsey AR, Lloyd DG, Elliott BC, et al. Changing sidestep cutting technique reduces knee valgus loading. Am J Sports Med. 2009 Nov;37( 11):2194–200. doi: 10.1177/0363546509334373. [DOI] [PubMed] [Google Scholar]
- 127.Pollard CD, Sigward SM, Powers CM. Gender differences in hip joint kinematics and kinetics during side-step cutting maneuver. Clin J Sport Med. 2007 Jan;17( 1):38–42. doi: 10.1097/JSM.0b013e3180305de8. [DOI] [PubMed] [Google Scholar]
- 128.Zazulak BT, Hewett TE, Reeves NP, et al. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007 Jul;35( 7):1123–30. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 129.McGill S, Grenier S, Bluhm M, et al. Previous history of LBP with work loss is related to lingering deficits in biomechanical, physiological, personal, psychosocial and motor control characteristics. Ergonomics. 2003 Jun 10;46( 7):731–46. doi: 10.1080/0014013031000090134. [DOI] [PubMed] [Google Scholar]
- 130.Nadler SF, Malanga GA, De Prince M, et al. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. J Sports Med. 1999;10:89–97. doi: 10.1097/00042752-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 131.Takemasa R, Yamamoto H, Tani T. Trunk muscle strength in and effect of trunk muscle exercises for patients with chronic low back pain: the differences in patients with and without organic lumbar lesions. Spine (Phila Pa 1976) 1995 Dec 1;20( 23):2522–30. doi: 10.1097/00007632-199512000-00012. [DOI] [PubMed] [Google Scholar]
- 132.Biedermann HJ, Shanks GL, Forrest WJ, et al. Power spectrum analyses of electromyographic activity: discriminators in the differential assessment of patients with chronic low-back pain. Spine (Phila Pa 1976) 1991 Oct;16( 10):1179–84. [PubMed] [Google Scholar]
- 133.Hodges PW. The role of the motor system in spinal pain: implications for rehabilitation of the athlete following lower back pain. J Sci Med Sport. 2000 Sep;3( 3):243–53. doi: 10.1016/s1440-2440(00)80033-x. [DOI] [PubMed] [Google Scholar]
- 134.van Dieen JH, Selen LP, Cholewicki J. Trunk muscle activation in low-back pain patients, an analysis of the literature. J Electromyogr Kinesiol. 2003 Aug;13( 4):333–51. doi: 10.1016/s1050-6411(03)00041-5. [DOI] [PubMed] [Google Scholar]
- 135.Harringe ML, Halvorsen K, Renstrom P, et al. Postural control measured as the center of pressure excursion in young female gymnasts with low back pain or lower extremity injury. Gait Posture. 2008 Jul;28( 1):38–45. doi: 10.1016/j.gaitpost.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 136.Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain: a motor control evaluation of transversus abdominis. Spine (Phila Pa 1976) 1996 Nov 15;21( 22):2640–50. doi: 10.1097/00007632-199611150-00014. [DOI] [PubMed] [Google Scholar]
- 137.Hodges PW, Richardson CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. J Spinal Disord. 1998 Feb;11( 1):46–56. [PubMed] [Google Scholar]
- 138.Luoto S, Aalto H, Taimela S, et al. One-footed and externally disturbed two-footed postural control in patients with chronic low back pain and healthy control subjects: a controlled study with follow-up. Spine (Phila Pa 1976) 1998 Oct 1;23( 19):2081–9. doi: 10.1097/00007632-199810010-00008. discussion 9–90. [DOI] [PubMed] [Google Scholar]
- 139.Radebold A, Cholewicki J, Panjabi MM, et al. Muscle response pattern to sudden trunk loading in healthy individuals and in patients with chronic low back pain. Spine (Phila Pa 1976) 2000 Apr 15;25( 8):947–54. doi: 10.1097/00007632-200004150-00009. [DOI] [PubMed] [Google Scholar]
- 140.Reeves NP, Cholewicki J, Milner TE. Muscle reflex classification of low-back pain. J Electromyogr Kinesiol. 2005 Feb;15( 1):53–60. doi: 10.1016/j.jelekin.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 141.Brumagne S, Cordo P, Lysens R, et al. The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine (Phila Pa 1976) 2000 Apr 15;25( 8):989–94. doi: 10.1097/00007632-200004150-00015. [DOI] [PubMed] [Google Scholar]
- 142.Taimela S, Kankaanpaa M, Luoto S. The effect of lumbar fatigue on the ability to sense a change in lumbar position: a controlled study. Spine (Phila Pa 1976) 1999 Jul 1;24( 13):1322–7. doi: 10.1097/00007632-199907010-00009. [DOI] [PubMed] [Google Scholar]
- 143.Bullock-Saxton JE, Janda V, Bullock MI. Reflex activation of gluteal muscles in walking: an approach to restoration of muscle function for patients with low-back pain. Spine (Phila Pa 1976) 1993 May;18( 6):704–8. [PubMed] [Google Scholar]
- 144.Childs JD, Piva SR, Erhard RE, et al. Side-to-side weight-bearing asymmetry in subjects with low back pain. Man Ther. 2003 Aug;8( 3):166–9. doi: 10.1016/s1356-689x(03)00014-6. [DOI] [PubMed] [Google Scholar]
- 145.Gill KP, Callaghan MJ. The measurement of lumbar proprioception in individuals with and without low back pain. Spine (Phila Pa 1976) 1998 Feb 1;23( 3):371–7. doi: 10.1097/00007632-199802010-00017. [DOI] [PubMed] [Google Scholar]
- 146.Leinonen V, Kankaanpaa M, Airaksinen O, et al. Back and hip extensor activities during trunk flexion/extension: effects of low back pain and rehabilitation. Arch Phys Med Rehabil. 2000 Jan;81( 1):32–7. doi: 10.1016/s0003-9993(00)90218-1. [DOI] [PubMed] [Google Scholar]
- 147.Kankaanpaa M, Taimela S, Laaksonen D, et al. Back and hip extensor fatigability in chronic low back pain patients and controls. Arch Phys Med Rehabil. 1998 Apr;79( 4):412–7. doi: 10.1016/s0003-9993(98)90142-3. [DOI] [PubMed] [Google Scholar]
- 148.Myer GD, Chu DA, Brent JL, et al. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sports Med. 2008 Jul;27( 3):425–48. doi: 10.1016/j.csm.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pollard CD, Sigward SM, Ota S, et al. The influence of in-season injury prevention training on lower-extremity kinematics during landing in female soccer players. Clin J Sport Med. 2006 May;16( 3):223–7. doi: 10.1097/00042752-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 150.Zeller BL, McCrory JL, Kibler WB, et al. Differences in kinematics and electromyographic activity between men and women during the single-legged squat. Am J Sport Med. 2003;31( 3):449–56. doi: 10.1177/03635465030310032101. [DOI] [PubMed] [Google Scholar]
- 151.Ferber R, McClay Davis I, Williams DS., III Gender differences in lower extremity mechanics during running. Clin Biomech (Bristol, Avon) 2003 May;18( 4):350–7. doi: 10.1016/s0268-0033(03)00025-1. [DOI] [PubMed] [Google Scholar]
- 152.Chumanov ES, Wall-Scheffler C, Heiderscheit BC. Gender differences in walking and running on level and inclined surfaces. Clin Biomech (Bristol, Avon) 2008 Dec;23( 10):1260–8. doi: 10.1016/j.clinbiomech.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 153.Ford KR, Myer GD, Smith RL, et al. A comparison of dynamic coronal plane excursion between matched male and female athletes when performing single leg landings. Clin Biomech. 2006;21( 1):33–40. doi: 10.1016/j.clinbiomech.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 154.Pappas E, Hagins M, Sheikhzadeh A, et al. Biomechanical differences between unilateral and bilateral landings from a jump: gender differences. Clin J Sport Med. 2007 Jul;17( 4):263–8. doi: 10.1097/JSM.0b013e31811f415b. [DOI] [PubMed] [Google Scholar]
- 155.Hewett TE, Ford KR, Myer GD, et al. Gender differences in hip adduction motion and torque during a single leg agility maneuver. J Orthop Res. 2006;24( 3):416–21. doi: 10.1002/jor.20056. [DOI] [PubMed] [Google Scholar]
- 156.Jacobs CA, Uhl TL, Mattacola CG, et al. Hip abductor function and lower extremity landing kinematics: sex differences. J Athl Train. 2007 Jan-Mar;42(1):76–83. [PMC free article] [PubMed] [Google Scholar]
- 157.Padua DA, Marshall SW, Beutler AI, et al. Predictors of knee valgus angle during a jump-landing task. Med Sci Sports Exerc. 2005;37( 5):S398. [Google Scholar]
- 158.Brophy RH, Chiaia TA, Maschi R, et al. The core and hip in soccer athletes compared by gender. Int J Sports Med. 2009 Sep;30( 9):663–7. doi: 10.1055/s-0029-1225328. [DOI] [PubMed] [Google Scholar]
- 159.McLean SG, Huang X, van den Bogert AJ. Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: implications for ACL injury. Clin Biomech (Bristol, Avon) 2005 Oct;20( 8):863–70. doi: 10.1016/j.clinbiomech.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 160.Sigward SM, Powers CM. Loading characteristics of females exhibiting excessive valgus moments during cutting. Clin Biomech (Bristol, Avon) 2007 Aug;22( 7):827–33. doi: 10.1016/j.clinbiomech.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 161.Houck JR, Duncan A, De Haven KE. Comparison of frontal plane trunk kinematics and hip and knee moments during anticipated and unanticipated walking and side step cutting tasks. Gait Posture. 2006 Nov;24( 3):314–22. doi: 10.1016/j.gaitpost.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 162.Imwalle LE, Myer GD, Ford KR, et al. Relationship between hip and knee kinematics in athletic women during cutting maneuvers: a possible link to noncontact anterior cruciate ligament injury and prevention. J Strength Cond Res. 2009 Nov;23( 8):2223–30. doi: 10.1519/JSC.0b013e3181bc1a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Thijs Y, Van Tiggelen D, Willems T, et al. Relationship between hip strength and frontal plane posture of the knee during a forward lunge. Br J Sports Med. 2007;41( 11):723. doi: 10.1136/bjsm.2007.037374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Lephart SM, Ferris CM, Riemann BL, et al. Gender differences in strength and lower extremity kinematics during landing. Clin Orthop. 2002;401:162–9. doi: 10.1097/00003086-200208000-00019. [DOI] [PubMed] [Google Scholar]
- 165.Lawrence RK, 3rd, Kernozek TW, Miller EJ, et al. Influences of hip external rotation strength on knee mechanics during single-leg drop landings in females. Clin Biomech (Bristol, Avon) 2008;23( 6):806–13. doi: 10.1016/j.clinbiomech.2008.02.009. [DOI] [PubMed] [Google Scholar]


