Abstract
OBJECTIVE
Due to data published in 2009 demonstrating improved outcomes among early- versus late-term infants, practice shifted towards delivering infants at later gestational ages. We examined the effects of this change on neonates with congenital heart disease.
DESIGN
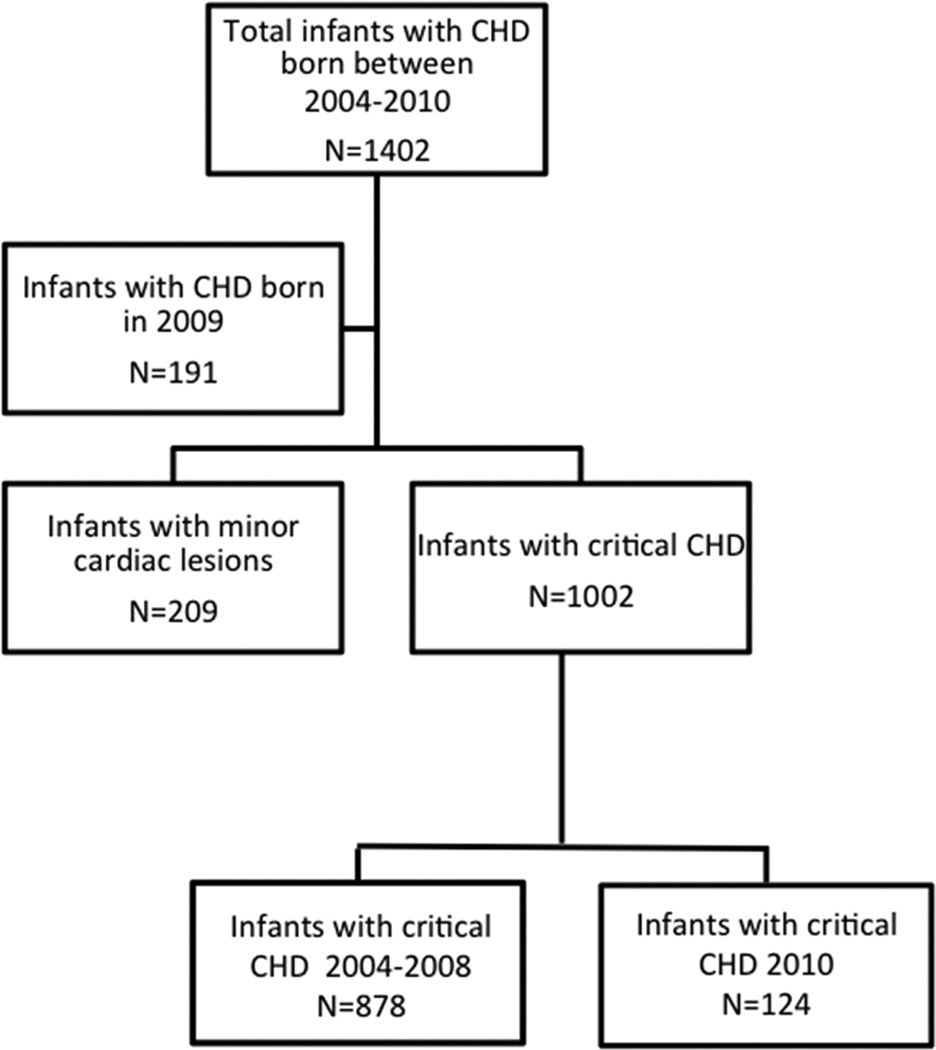
This was a retrospective cohort study. Neonates with congenital heart disease born between 2004–2008 were compared with those born in 2010. Patients born in 2009, considered to be a transitional year, were excluded.
SETTING
Tertiary care level 4 neonatal intensive care unit with comprehensive cardiac service
PATIENTS
Neonates with significant congenital heart disease admitted between 2004–2010
OUTCOME MEASURES
Mode of delivery, length of stay, neonatal morbidity and mortality.
RESULTS
There were 878 infants with congenital heart disease born in 2004–2008 and 124 in 2010. The mean gestational age was higher in 2010 than in 2004–2008 (38.4±1.9 versus 37.8±2.3 weeks, p=0.001) and there were fewer preterm births in 2010 compared with 2004–2008 (p=0.003, OR=0.4). Mean birth weight was also higher in 2010(3134±675 versus 2975±599 grams, p=0.008). In 2010, less than half as many infants were born via scheduled induction (p<0.001, OR=0.2) or scheduled cesarean delivery (p=0.002, OR=0.4) as in 2004–2008. However, in 2010 there were more urgent inductions (p=0.002, OR=3.1), cesarean deliveries after labor (p=0.01, OR=2.2), and unplanned cesarean deliveries in general (p=0.02, OR=1.7) compared with 2004–2008. In 2010, neonates were less likely to require preoperative vasopressors (p = 0.002), but there were no differences in 5 min APGAR, antibiotic administration, preoperative intubation, median length of stay, or mortality compared with 2004–2008.
CONCLUSIONS
Despite increased gestational age and birth weight following the shift in delivery practice, there was no difference in length of stay, neonatal morbidity, or mortality in infants with congenital heart disease. The resultant increase in urgent cesarean delivery and urgent inductions may confer additional maternal morbidity.
Keywords: Congenital Heart Disease, Early-Term, Late-Term, Mode of Delivery, Morbidity, fetal cardiology, prenatal diagnosis
INTRODUCTION
In 2009, research emerged citing improved neonatal outcomes for infants delivered at late-term (>39 weeks gestation) as opposed to early-term (37–38 weeks)(1, 2). These studies highlighted the need for less respiratory support, decreased neonatal intensive care unit admissions, and decreased incidence of neonatal sepsis in late-term infants. In the pediatric cardiology community, it has long been accepted that preterm and low birth weight infants with significant congenital heart disease (CHD) have worse prognoses(3). However, little research has focused on early- versus late-term deliveries in cardiac patients.
As a result of this new data, obstetric practice began to shift towards delivering infants at later gestational ages. Our objective was to investigate the effects of this change in practice on the CHD population. We hypothesized electing to deliver at late-term would lead to an increase in mean gestational age and birth weight among neonates with significant CHD which would favorably impact morbidity, mortality, and hospital length of stay. We also hypothesized mode of delivery would be affected by this change.
METHODS
The electronic medical records of neonates with significant CHD admitted to the neonatal intensive care unit (NICU) between 2004–2010 were retrospectively reviewed. Morgan Stanley Children’s Hospital of New York-Presbyterian is a tertiary care referral center with a level 4 NICU, specialized fetal diagnosis center, the Center for Prenatal Pediatrics, and a comprehensive pediatric cardiology service. Patients with minor cardiac lesions such as isolated atrial septal defects, ventricular septal defects and patent ductus arteriosus were excluded.
Obstetric data including maternal age, gravidity and parity, prenatal diagnosis of cardiac defect, prenatal ultrasound abnormalities, and mode of delivery were collected. Cesarean deliveries and inductions of labor that occurred as planned on a pre-specified date were defined as scheduled deliveries and scheduled inductions. Urgent deliveries were defined as unscheduled inductions of labor or cesarean deliveries for maternal or fetal indications as identified from obstetric records.
Neonatal variables including gestational age (GA) and birth weight were reviewed. Markers of neonatal morbidity such as 5 minute APGAR score, need for preoperative antibiotic administration, preoperative intubation, and length of stay (LOS) were recorded, along with neonatal mortality. Type of surgical intervention and surgical severity score as defined by Risk Adjustment for Congenital Heart Surgery-2 (RACHS-2) score were documented(4). Neonates were coded as preterm if GA was < 37 weeks, early-term if GA was 37–38.99 weeks, and late-term if GA was ≥39 weeks.
Statistical Analysis
Neonates born between 2004–2008 were compared with those born in 2010. The year 2009 was considered to be a transitional year in which change in practice was implemented at our institution and, therefore, patients born in 2009 were excluded from analysis. Results are displayed as mean ± standard deviations and medians with ranges as appropriate. Comparisons between groups were conducted using Student’s t-test and two by two tables with the Chi Square test statistic. Alpha level was set at 0.05. All statistical analyses were performed using SPSS(IBM, Armonk, New York).
RESULTS
Patient Characteristics
A total of 1,402 neonates with congenital heart disease were admitted to our hospital from January 1, 2004 to December 31, 2010. Of these, 878 in 2004–2008 and 124 in 2010 met criteria for significant CHD and were included in our analysis. Subject characteristics are highlighted in Table 1. There were no significant differences in RACHS-2 score, number of patients who underwent surgery, were prenatally diagnosed, or were transferred from other institutions between time periods. Maternal characteristics were similar between groups with no significant difference in maternal age or primigravid status, however, there were more multiparous mothers in the 2010 cohort. More infants in 2010 had genetic abnormalities than those in 2004–2008. The most common CHD lesions for the cohort are shown in Table 2.
Table 1.
Patient Characteristics
| 2004–2008 (n=878) |
2010 (n=124) |
p-value | |
|---|---|---|---|
| Gender | |||
| Males | 59 (517) | 60 (74) | 0.80 |
| Females | 41% (360) | 40% (49) | |
| Mean Maternal Age (years) | 30.5 ± 6.4 | 29.7 ± 6.4 | 0.15 |
| Primigravid Mother | 27% (225) | 26% (32) | 0.95 |
| Multiparous Mother | 59% (499) | 70% (85) | 0.03 |
| Prenatal Diagnosis | 68% (593) | 70% (85) | 0.55 |
| Transferred from another institution | 43% (379) | 41% (50) | 0.60 |
| Underwent Surgery | 71% (619) | 76% (94) | 0.18 |
| RACHS-2* | 0.36 | ||
| 1 | 0% (0) | 0% (0) | |
| 2 | 11% (67) | 12% (11) | |
| 3 | 36% (222) | 32% (29) | |
| 4 | 30% (183) | 38% (35) | |
| 5 | 1% (8) | 0% (0) | |
| 6 | 22% (136) | 18% (16) | |
| Genetic Abnormality | 8% (70) | 20% (20) | <0.001 |
Percentages are reflective of those who underwent surgery
Table 2.
Congenital Cardiac Lesions
| 2004–2008 (n=878) |
2010 (n=124) |
p-value | |
|---|---|---|---|
| AVC1 | 5% (44) | 4% (5) | 0.65 |
| D-TGA2 | 18% (155) | 21% (26) | 0.35 |
| DORV3 | 7% (64) | 6% (7) | 0.52 |
| Heterotaxy | 3% (26) | 4% (5) | 0.51 |
| HLHS4 | 12% (103) | 13% (16) | 0.68 |
| IAA5 | 3% (24) | 4% (5) | 0.41 |
| Isolated Arch | 15% (129) | 12% (15) | 0.45 |
| PA6 | 4% (32) | 4% (5) | 0.82 |
| TAPVR7 | 5% (43) | 4% (5) | 0.67 |
| TOF8 | 11% (100) | 14% (17) | 0.43 |
| TriAtresia9 | 3% (24) | 5% (6) | 0.19 |
| Truncus | 2% (15) | 2% (2) | 0.95 |
AV Canal,
D-Transposition of the Great Arteries,
Double Outlet Right Ventricle,
Hypoplastic Left Heart Syndrome,
Interrupted Aortic Arch,
Pulmonary Atresia,
Total Anomalous Pulmonary Venous Return,
Tetralogy of Fallot,
Tricuspid Atresia
Neonatal Outcomes as a Function of Era
The mean gestational age and mean birth weight were higher in 2010 than in 2004–2008(Table 3). There were fewer preterm births and more late-term births in 2010 compared with 2004–2008 but no change in early-term births between groups. The odds of late-term delivery in 2010 were 2.1 (95% CI 1.4-3) and odds of preterm delivery were 0.4 (95% CI 0.2-0.7) compared with 2004–2008. In 2010, neonates were less likely to require preoperative vasopressors, but we found no differences in 5 minute APGAR, antibiotic administration, preoperative intubation, median LOS or mortality compared with 2004–2008.
Table 3.
Neonatal Outcomes
| 2004–2008 | 2010 | p-value | |
|---|---|---|---|
| Gestational Age (wk) | 37.8 ± 2.3 | 38.4 ± 1.9 | <0.001 |
| Preterm Births | 20% (n=171) | 9% (n=11) | 0.003 |
| Early-Term | 35% (n=305) | 32% (n=39) | 0.46 |
| Late-Term | 41% (n=356) | 59% (n=72) | <0.001 |
| Birth Weight | 2975 ± 599 | 3134 ± 675 | 0.008 |
| Preoperative Vasopressors | 32% (n=283) | 19% (n=23) | 0.002 |
| 5 minute APGAR | 8.5 ± 0.9 | 8.6 ± 0.9 | 0.11 |
| Preoperative Antibiotic Use | 50% (n=935) | 42% (n=52) | 0.12 |
| Preoperative Intubation | 46% (n=394) | 50% (n=160) | 0.49 |
| Median LOS and Range (days) | 14 (1–197) | 16 (1–144) | 0.18 |
| Mortality | 11% (n=96) | 6% (n=7) | 0.07 |
Obstetric Outcomes as a Function of Era
There was no difference in the proportions of normal spontaneous vaginal delivery, overall vaginal delivery, or cesarean delivery between groups (Table 4). In 2010, more patients presented in spontaneous labor and fewer infants were born via scheduled induction or scheduled cesarean delivery compared with 2004–2008. In 2010 there were more urgent inductions for maternal or fetal indications, cesarean deliveries after labor, and unplanned cesarean deliveries.
Table 4.
Obstetric Outcomes
| 2004–2008 | 2010 | p-value | |
|---|---|---|---|
| Spontaneous onset of labor | 40% (n=349) | 53% (n=64) | 0.008 |
| Cesarean Delivery | 45% (n=396) | 42% (n=51) | 0.41 |
| Scheduled Delivery | 49% (n=421) | 23% (n=28) | <0.001 |
| CD1 after spontaneous labor | 6% (n=53) | 12% (n=15) | 0.01 |
| CD after IOL2 | 5% (n=44) | 7% (n=8) | 0.47 |
| Unscheduled IOL | 3% (n=27) | 9% (n=11) | 0.002 |
| Unscheduled CD* | 18% (n=160) | 28% (n=34) | 0.02 |
CD=Cesarean Delivery,
IOL=Induction of Labor,
includes conversions from vaginal deliveries
DISCUSSION
In the pediatric and obstetric literature, infants delivered at 39–40 weeks gestation are reported to have improved perinatal outcomes compared with infants delivered at early-term (37–38 weeks)(1, 2). With the emergence of this data in 2009, there was a movement among obstetricians to deliver infants in the late-term period. We sought to explore the effects of this change in practice on our population with significant CHD.
After changes in 2009 to support late-term deliveries, we found neonates with significant CHD had a higher mean gestational age and birth weight compared with infants born in the prior era. In fact, CHD infants were twice as likely to be delivered late-term in 2010 than in 2004–2008 while CHD infants born in 2004–2008 were 2.5 times as likely to be born premature (< 37 wks GA). Despite these advances, there was no difference in NICU length of stay, preoperative morbidity, or mortality between eras other than a decrease in the use of preoperative pressors.
There are multiple explanations for the difference in results between our study and prior reports. For one, the studies reporting improved outcomes at late-term gestations consisted of low-risk elective deliveries among presumably healthy fetuses and infants. The population of infants with significant CHD is high-risk and most are admitted to the NICU. While previous studies showed that infants born late-term require less respiratory support (2, 5, 6), our practice shift to deliver fetuses with significant CHD at late-term did not translate into fewer preoperative intubations. Decreased respiratory support in late-term infants is thought to be due to improved lung development. However, infants with CHD are often intubated for reasons independent of lung maturity such as pulmonary over-circulation or apnea secondary to prostaglandin administration. Finally, there was no difference in LOS between groups despite higher birth weight and gestational age. Explanations for a lack of a difference in NICU LOS are speculative. Perhaps the sample size was too small, or the differences in gestational age were not great enough to affect a significant change in LOS given the overall high level of intensive medical attention provided to all significant CHD patients.
Our study revealed a significant increase in the number of infants with genetic anomalies in 2010 compared with 2004–2008. This may be due to advances in diagnostic modalities such as chromosomal microarray and whole exome sequencing which were not previously available. Additionally, more known genetic mutations are added to the genetic testing registry each year and therefore our findings may simply reflect increased detection secondary to improved surveillance. We also saw a slightly higher proportion of multiparous women in 2010 compared with 2004–2008. Explanations for this difference are speculative and may simply be due to chance.
In accordance with our hypothesis, we found the change in practice to deliver more infants late-term translated into an overall effect on the circumstances of delivery for patients. In 2010, there was an increase in unplanned cesarean deliveries and inductions compared with 2004–2008. We speculate that by carrying pregnancies longer, women may be more likely to have complications seen at late gestation requiring intervention, such as oligohydramnios, macrosomia, or decreased fetal movement. In 2011, Erenthal et al. noted an increased incidence of macrosomia and stillbirth after the implementation of guidelines limiting delivery before 39 weeks gestation(7). It is not clear whether CHD fetuses are more likely than normal fetuses to suffer these specific complications in late gestation and we did not have the data to test this hypothesis. However, pregnant women with CHD fetuses undergo more testing during pregnancy than women with healthy fetuses and therefore the rate of detection is likely to be higher in this group. Another explanation for this finding is women slated for late-term delivery may have been scheduled for repeat cesarean, but presented in labor at an earlier date and thus required an urgent cesarean delivery. Further investigation of this increase in unplanned cesareans and inductions is needed to determine if these factors are truly causal and whether they confer additional maternal morbidity.
Our study has several limitations. It was a single center, retrospective review with a modest sample size. We did not follow patients longitudinally after NICU discharge for long-term outcomes. Several studies have reported that infants born at 39–41 weeks have higher academic achievement and IQ scores than their 37–38 week counterparts(8, 9). While there are many variables associated with cognitive outcomes in infants with CHD, including associated genetic anomalies, further research on the impact of gestational age on neurodevelopment in this high-risk population is warranted.
CONCLUSIONS
The 2009 shift in pediatric and obstetric practice to favor late-term delivery of CHD neonates resulted in an increase in gestational age and birth weight of these infants without an appreciable difference in NICU LOS, neonatal morbidity, or mortality. This coincided with a notable increase in unscheduled cesarean deliveries and inductions for maternal and fetal indications. In light of questionable neonatal benefit to late-term delivery in this high-risk population, future investigation of the potential negative impact on maternal obstetric out comes is indicated.
Figure 1.
Diagram illustrating neonates who met inclusion criteria in 2004–2008 and 2010 groups.
Acknowledgments
DICLOSURE OF GRANTS OR FUNDING
I.A. Williams received support from Grant No. 1K23HD061601 from the National Institute of Child Health & Human Development of the National Institutes of Health. The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Child Health & Human Development.
Footnotes
CONFLICT OF INTEREST STATEMENT
None
AUTHOR CONTRIBUTIONS
Nina Dadlez, MD: Concept and Design, Data Analysis/Interpretation, Drafting Article, Critical Revision of Article, Statistics
Sara Brubaker, MD: Data Analysis/Interpretation, Critical Revision of Article
Lynn Simpson, MD: Data Analysis/Interpretation, Critical Revision of Article
Betul Yilmaz, MD: Data Analysis/Interpretation, Critical Revision of Article
Ismée Williams, MD, MS: Concept and Design, Data Analysis/Interpretation, Drafting Article, Critical Revision of Article, Statistics
REFERENCES
- 1.De Luca R, Boulvain M, Irion O, Berner M, Pfister RE. Incidence of early neonatal mortality and morbidity after late-preterm and term cesarean delivery. Pediatrics. 2009 Jun;123(6):e1064–e1071. doi: 10.1542/peds.2008-2407. [DOI] [PubMed] [Google Scholar]
- 2.Tita AT, Landon MB, Spong CY, Lai Y, Leveno KJ, Varner MW, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009 Jan 8;360(2):111–120. doi: 10.1056/NEJMoa0803267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrews RE, Simpson JM, Sharland GK, Sullivan ID, Yates RW. Outcome after preterm delivery of infants antenatally diagnosed with congenital heart disease. J Pediatr. 2006 Feb;148(2):213–216. doi: 10.1016/j.jpeds.2005.10.034. [DOI] [PubMed] [Google Scholar]
- 4.Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002 Jan;123(1):110–118. doi: 10.1067/mtc.2002.119064. [DOI] [PubMed] [Google Scholar]
- 5.Cheng YW, Nicholson JM, Nakagawa S, Bruckner TA, Washington AE, Caughey AB. Perinatal outcomes in low-risk term pregnancies: do they differ by week of gestation? Am J Obstet Gynecol. 2008 Oct;199(4):370 e1–370 e7. doi: 10.1016/j.ajog.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Costello JM, Polito A, Brown DW, McElrath TF, Graham DA, Thiagarajan RR, et al. Birth before 39 weeks' gestation is associated with worse outcomes in neonates with heart disease. Pediatrics. 2010 Aug;126(2):277–284. doi: 10.1542/peds.2009-3640. [DOI] [PubMed] [Google Scholar]
- 7.Ehrenthal DB, Hoffman MK, Jiang X, Ostrum G. Neonatal outcomes after implementation of guidelines limiting elective delivery before 39 weeks of gestation. Obstet Gynecol. 2011 Nov;118(5):1047–1055. doi: 10.1097/AOG.0b013e3182319c58. [DOI] [PubMed] [Google Scholar]
- 8.Noble KG, Fifer WP, Rauh VA, Nomura Y, Andrews HF. Academic achievement varies with gestational age among children born at term. Pediatrics. 2012 Aug;130(2):e257–e264. doi: 10.1542/peds.2011-2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang S, Platt RW, Kramer MS. Variation in child cognitive ability by week of gestation among healthy term births. Am J Epidemiol. 2010 Feb 15;171(4):399–406. doi: 10.1093/aje/kwp413. [DOI] [PMC free article] [PubMed] [Google Scholar]