Key messages
Ageing, acute illness and poorly managed long term conditions increase falls risk
Primary care staff are the first line in falls prevention
Primary care staff can identify and modify many risk factors
Modifying risk factors reduces the risk of falls and improves quality of life
If falls continue or staff are unable to identify risk factors the person should be referred to a falls clinic.
Why this matters to me
In my last post as a nurse consultant I ran a falls clinic with a physiotherapy colleague. We found that many of the problems that increased falls risk were small problems that added up to one large falls risk. Many clinicians working in primary care did not appreciate how valuable their knowledge of patients was in preventing falls and how they could use their skills to cut falls risk and improve quality of life. Other colleagues did not appreciate the value of nurse and therapy led clinics in carrying out detailed assessments that could complement their work in primary care and lead to patients experiencing improved quality of life.
In my current post at Ealing and Harrow Community Services I am nurse consultant and am clinically responsible for a nurse-led intermediate care ward. The ward admits people who require a higher level of care than can be provided at home and aims to prevent acute hospital admission. Around 50% of patients are admitted because of falls.
Keywords: assessment, falls, quality of life, risk factors, treatment
Abstract
Each year 1.57 million older people fall more than three times and 70 000 fracture their hips. Falls can lead to disability and even death. The NSF for Older People identified falls prevention as a major health priority. This paper explains how primary care practitioners can contribute to falls prevention, reduce falls risk and improve quality of life for the older person.
Introduction
Primary care staff often encounter people who have sustained a fall. Falls are the commonest cause of accidental death in older people. Every five hours someone dies as a result of a fall. Each year 1.57million people aged over 65 have three or more falls, 310 000 sustain fractures, 70 000 of these are hip fractures. Hip fractures increase the risk of death by 16 times in women and 12 times in men in the 30 days after fracture.1
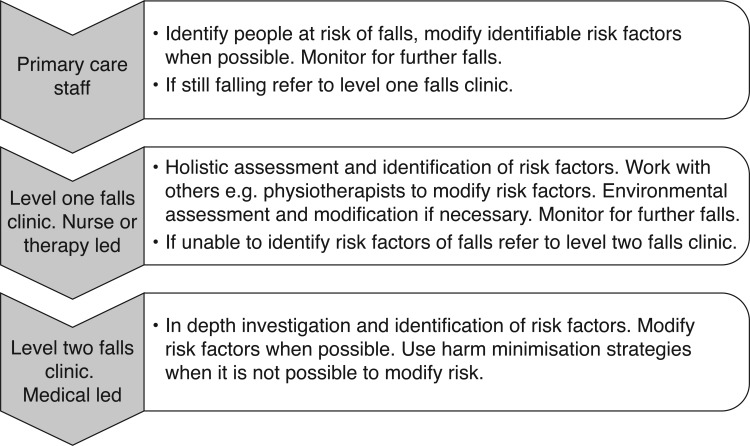
The National Service Framework for Older People identifies prevention of falls as an important health priority and requires NHS trusts to set up falls prevention services.2 Although falls prevention services are vitally important the contribution that primary care staff can make to preventing falls is equally important. This paper aims to enable primary care staff to understand why older people fall and what can be done to reduce a person's risk of falls. Figure 1 illustrates the role of primary care staff in falls prevention.
Figure 1.
The role of primary care staff in falls prevention
Why do older people fall?
Although there are literally hundreds of reasons why people fall, some risk factors are more common and easily remedied that others.3 Table 1 outlines the main risk categories and how these can be checked.
Table 1.
Checklist on factors affecting falls risk
| What is increasing fall risk | Check |
|---|---|
| Acute illness | Chest infection, ear infection. |
| Undiagnosed disease | Stroke, Parkinson's diabetes, poor nutrition and hydration |
| Long term conditions | Can disease management be optimised to risk of falls |
| Malnutrition and dehydration | Acute and chronic fluid and nutritional deficits |
| Visual problems | Date of last eye test. Is person wearing glasses when needed? |
| Problems with gait, balance, mobility | Gait, foot problems, suitable shoes, if aids used check suitability and ferrules |
| Continence problems | What the person was doing when falls occurred. If the person has urinary frequency, especially at night |
| Postural hypotension | Sitting and standing BP. Medication that can affect blood pressure. Normal level activity |
| Medication | Medication that may be contributing to falls risk |
| Hazardous or unmodified environment | Where falls take place |
Acute illness
Falls can be an indication that the person is unwell. The person who develops an acute illness such as a chest or ear infection may well present with a fall. Treating identified infection reduces falls risk. It's important to be aware that many older people have asymptomatic bacteriuria. A urine dipstick reading is an unreliable indicator of urinary tract infection in older people 4 and treating an older person for urinary tract infection in the absence of urinary symptoms exposes them unnecessarily to the hazards of antibiotic therapy. Erroneous diagnosis or urinary tract infection also causes delays in finding out the reasons why the person is really falling.
Undiagnosed disease
Falls can indicate that the person has suffered a mild stroke or is developing Parkinson's disease. Observation of facial changes such as a lopsided smile or a face that is devoid of expression can alert you to such problems. Simple checks of limb function and power can confirm such suspicions and enable you to make an appropriate referral.
Long term conditions
The person with a long term condition may be falling because the condition is worsening, or because they are not complying with medication and treatment. If you suspect this check, optimise treatment if you are able or refer for further investigations and treatment.
Poor nutrition and hydration
Falls can occur if a person is dehydrated or malnourished. Observing how clothes fit and if rings seem loose can alert you to the possibility of weight loss and enable you to address this. You can also observe for signs of dehydration and enquire about fluid intake. Correction nutritional and fluid deficits improves health and reduces falls risk.
Visual problems
Poor vision increases the risk of falls.5 If a person cannot see clearly he or she is at greater risk of falls. Some age related changes are not yet treatable. The best we can do is to prevent further deterioration. Many older people have treatable eye conditions. Researchers found that 76% of hospital inpatients admitted following a fall had poor vision; 40% needed glasses, 37% had cataracts, 14% senile macular degeneration. Seventy nine percent of individuals with poor vision were treatable.6 If the person has fallen check when they last had an eye test and recommend an eye test if they have not had one within the last year. If the person is housebound their optician may offer a domiciliary service. If this is not possible then you can recommend a specialist domiciliary optician (see further information). If the person is diagnosed as having an eye disease the optician will inform the GP and recommend a specialist referral if necessary.
Gait balance and mobility problems
Foot problems are common in older people, 80% of older people have at least one foot problem. Foot pain makes people walk more slowly. It impairs balance and stability and increases the risk of falling.7 Observation of the person's gait, expression on walking and choice of footwear can help to identify foot problems. If the person is wearing oversized slippers, footwear with slits or holes cut in it to accommodate bunions, foot deformities or swelling this will increase the risk of falls.You can encourage the older person to buy suitable shoes that are wide enough to accommodate these problems (see further information) and refer them to a podiatrist. Podiatrists are skilled in treating common foot problems, correcting gait abnormalities and reducing foot pain. Podiatry treatment improves gait and reduces falls risk.
Osteoarthritis of the knee and hip can cause pain and lead to the person developing an arthralgic gait. This unbalances the body and increases the risk of falls. In severe cases the person may require a joint replacement. In many cases aids such as a walking stick help to provide additional support and stability. Physiotherapists are expert in providing appropriate treatment or aids for such patients.
If the person has a walking aid, observe the person using it. Sometimes people acquire walking sticks and walking frames. These can be the wrong size and the person may have to stretch or stoop to use the aid. This increases falls risk. It's also worth checking the ferrules on any aid. Ferrules are the rubber stoppers on the end of walking sticks and frames. The ferule should have a whorl pattern on it. If the pattern has worn off or the rim of the ferrule has worn through then the aid is dangerous and can increase the risk of falls. The community physiotherapist can supply and fit new ferrules.
Ageing and inactivity leads to muscle loss and increases falls risk. Only 14% of 75 year olds are sufficiently active to maintain health.8 Ageing and inactivity leads to poor posture. The person often walks with the head forward and bottom sticking out. This leads to the centre of balance changing and the person becoming more unstable. The person may have poor proprioception and may have to look at feet and legs to work out where they are. Walking speed is reduced. The quadriceps muscles in the thighs can waste. This leads to the knees being poorly supported and more likely to give. Calf muscles can waste. The person tires easily, doesn't lift the feet, shuffles and is more likely to trip. Poor mobility increases the risk of falls. The person who is less mobile looses muscle strength and balance deteriorates.9
Much of what is considered to be the ageing process is really caused not by ageing but by inactivity. Older people can regain 27% of muscle strength reversing age related decline by 15 years by attending one exercise class a week and doing home exercises.10 If the person has poor posture or poor mobility you should recommend exercise classes. People who are very frail may benefit from the OTAGO exercise programme specially designed for frail older people. These programmes are usually run by community physiotherapists.
Continence
Ageing leads to the kidneys becoming less efficient at concentrating urine and a reduction in bladder capacity. These changes mean that is normal for the older person to get up once or twice in the night to pass urine. The older person may develop continence problems such as urgency and continence problems can contribute to falls risk. Continence assessment can address any treatable problems, reduce falls risk and improve quality of life.
Postural hypotension
Postural hypotension is normally defined as a fall in systolic blood pressure of 20mm of mercury or more, when rising from sitting to standing. This makes a person feel dizzy on standing and increases falls risk. Addressing the cause is often straightforward. Inactivity and deconditioning can lead to postural hypotension. Increased activity and exercise often corrects the problem. Dehydration can lead to postural hypotension, correcting dehydration and reviewing diuretic therapy if prescribed often helps. Medication given to treat hypertension can lead to postural hypotension and will require review. If postural hypotension persists compression stockings can help. The person should have a Doppler ultrasound to check for arterial problems. If compression hosiery is required then grade three full length stockings are most effective. In my experience many older people struggle with grade three compression stockings and grade two compression though less effective is better tolerated. If all other measures fail then medication such as fludrocortisone may be prescribed.
Medication
Any medication that sedates, causes confusion, hypotension or dehydration may increase the risk of falls.11 Unfortunately, older people consume 43% of all prescribed medicines, more than any other group.12 More than 90% of people aged 75 or over are prescribed regular medicines.13 Older people are prescribed an average of four medicines.14 Older people who are receiving four or more medicines are now to have those medications reviewed twice a year and the review is to be recorded.2 Medication review has been shown to significantly reduce the number of falls in people living in care homes.15 Box 1 provides details of some medicines that can increase the risk of falls.
Box 1. Medicines that can increase falls risk.
Benzodiazepines
Psychotropics
Sedatives
Diuretics
Digoxin and other anti-arrhythmics
Hypotensives
Codeine and morphine based analgesics
More than four medicines
Antidepressants
Antidepressants increase the risk of falling by between 50% and 200%.16,17 Tricyclic antidepressants can cause a fall in standing blood pressure which can lead to dizziness and fainting.18 When serotonin reuptake inhibitor antidepressants such as fluoxetine were introduced, they were considered safer.19 Unfortunately a study of over 2000 people living in Tennessee nursing homes proved that there was little difference in fall rates in those treated with tricyclics and newer antidepressants. Every person receiving antidepressants had a higher rate of falls than those who were not. The rate of falls increased as the dose of antidepressant rose.20 Older people receiving antidepressants are more likely to fall and fracture a hip than those who are not.21 Antidepressants are frequently prescribed to older people and clinicians must balance the risks of untreated depression against the risk of falls. Recent research indicates that the benefits of antidepressants have been exaggerated and that depressed people can recover without the use of drugs.22
Sedatives and benzodiazepines
Sedatives and benzodiazepines increase the risk of falling. The risk is dose related and increases in line with the number of sedatives and antidepressants taken.23 These are not recommended for long term use and should be discontinued gradually.
Hypotensive drugs
Hypotensive drugs are commonly prescribed for hypertension and heart failure. Heart failure is difficult to diagnose, not all cases of swollen feet and ankle oedema are caused by cardiac failure. Accurate diagnosis and appropriate treatment is essential.24–26 The standard therapy for people with heart failure is ACE inhibitors, beta blockers and diuretic therapy; GPs should consult a specialist before prescribing them to frail older people.27 Side effects include dry cough, hypotension, which can cause falls, high levels of potassium, which can lead to cardiac arrest and renal failure. It is important that drugs are only given when clinically indicated and dosage is carefully titrated to avoid side effects.
Beta-blockers
Beta-blockers reduce pulse rate. This may help people with angina or tachycardia but causes problems in patients who have pre-existing bradycardia or heart block. The excessive slowing of the pulse may result in dizziness and fatigue. This can increase the risk of falls. Beta-blockers should not be used in patients with heart block (unless they have a pacemaker) or anyone with a pulse below 60 beats a minute. Non-selective beta-blockers such as propranolol are potentially harmful in diabetics prone to hypoglycaemia. Cardioselective beta-blockers are less risky. All beta-blockers can mask the tremor, tachycardia and sweating that warn diabetics of hypoglycaemia. Beta-blockers should never be stopped suddenly – they should be tailed off.28
Diuretics
Diuretics are prescribed to treat hypertension, heart failure and sometimes oedema caused by immobility. Diuretic therapy should be prescribed with care and monitored to reduce risks of falls and other adverse effects.
Analgesics
Analgesics, especially codeine based analgesics such as cocodamol and codydramol, can cause confusion in older people. This can increase the risk of falls. Some analgesics such as Tramadol and morphine based analgesia also increase falls risk.
It is important to be aware that older people often don't take prescribed medication, only about 60% of adults with long term conditions take medicines regularly enough to obtain any benefit.29 Medication review and minimising medication can increase the chances of the person taking prescribed medication and cut the risk of falls.
Environmental hazards
It is worth enquiring where the falls are taking place. Some times the person's home may have hazards, such as a step into the kitchen, that increase fall risk. The Australian government has offered older people free home safety checks and has subsidised the cost of modifications required. Modifications included nonslip flooring, improved lighting and fitting grab rails. Over a 12 month period the total number of falls fell by 63%.30
Conclusion
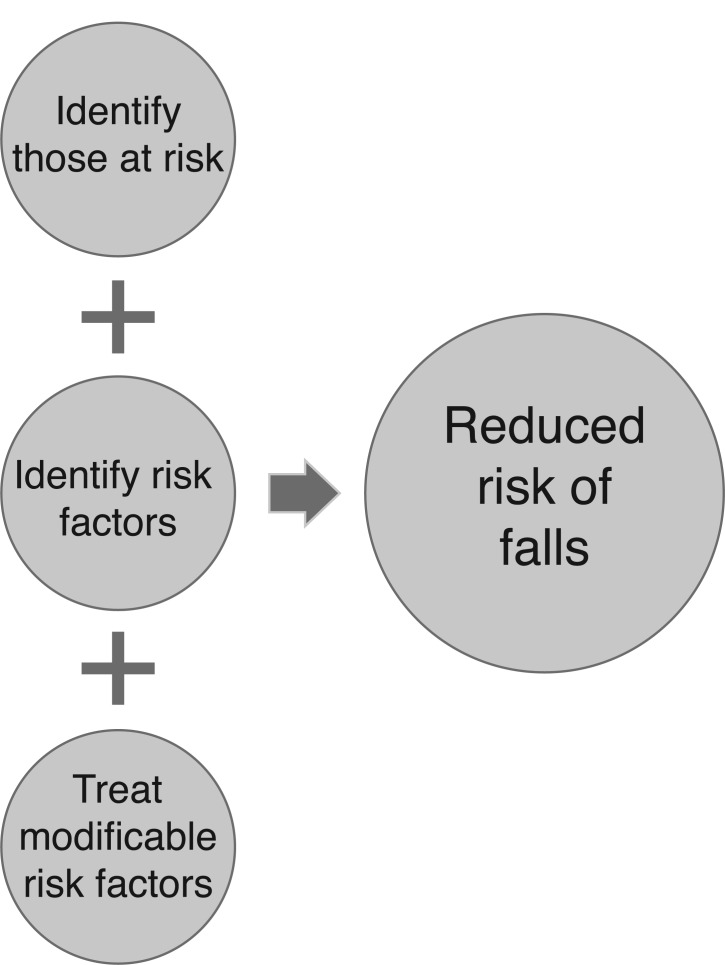
Ageing, illness, care and treatment and lifestyle factors can increase the risk of an older person falling. Often the older person has more than one falls risk factor. Primary care staff who work closely with older people are in an ideal position to identify, treat risk factors and to ask others to treat risk factors. These actions can make a huge difference to the person's quality of life and may spare them the pain and complications related to falls. If primary care staff are unable to identify falls risk factors or if the person continues to fall despite interventions then it important to refer them to a specialist falls clinic. Figure 2 illustrates how simple interventions can reduce falls risk.
Figure 2.
Interventions to reduce risk of falls
Resources
Domiciliary opticians
The Outside Clinic provides domiciliary eye tests to older people.
Vision Call specialise in providing domiciliary eye tests to people in care homes but has just launched a domiciliary service. They also provide staff training on caring for older people with visual problems www.vision-call.co.uk/DomiciliaryServices.asp
Footwear
Cosy Feet provide a range of footwear for people requiring wide footwear and people with foot problems. They provide catalogues and a mail order service. www.cosyfeet.com/footwear-c-88.html?gclid=CMXyJDzoZICFQ8HQwodkySaQg
Hotter provide a range of footwear for people requiring wide footwear and people with foot problems. They provide catalogues and a mail order service. www.hottershoes.com/
REFERENCES
- 1.Roberts SE, Goldacre MJ. Time trends and demography of mortality after fractured neck of femur in an English population, 1968–98: database study. BMJ 2003; 327:771–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Department of Health. National Service Framework: Older People. London: Department of Health, 2001. [Google Scholar]
- 3.Woolf AD, Akesson K. Preventing fractures in elderly people. BMJ 2003;327:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ducharme J, Neilson S, Ginn JL. Can urine cultures and reagent test strips be used to diagnose urinary tract infection in elderly emergency department patients without focal urinary symptoms? Canadian Journal of Emergency Medical Care 2007; 9(2):87–92. [DOI] [PubMed] [Google Scholar]
- 5.Abdelhafiz AH, Austin CA. Visual factors should be assessed in older people presenting with falls or hip fracture. Age and Ageing 2003;32:26–30. [DOI] [PubMed] [Google Scholar]
- 6.Jack CI, Smith T, Neoh C, Lye M, McGalliard JN. Prevalence of low vision in elderly patients admitted to an acute geriatric unit in Liverpool; elderly people who fall are more likely to have low vision. Gerontology 1995; 41(5):280–5. [DOI] [PubMed] [Google Scholar]
- 7.Menz HB, Lord SR. Foot pain impairs balance and functional ability in community dwelling older people. Journal American Podiatric Medical Association 2001; 91:5. [DOI] [PubMed] [Google Scholar]
- 8.Skelton DA, Young A, Walker A, Hoinville E. Physical activity in later life. Further analysis of the Allied Dunbar National fitness Survey and the Health Education Authority National Survey on Activity and Health. London: Health Education Authority, 1999. [Google Scholar]
- 9.Gialloreit LE, Marazzi MC. Risk for falls in the elderly. Role of activities of daily living and of subjective assessment of health status. A case controlled study. Recenti Prog Med 1996;87(9):405–11. [PubMed] [Google Scholar]
- 10.Skelton DA, McLaughlin AW. Training functional ability in old age. Physiotherapy 1996;82(3):159–67. [Google Scholar]
- 11.Hayes N. Prevention of falls among older people in the hospital environment. British Journal of Nursing 2004; 13(15):896–901. [DOI] [PubMed] [Google Scholar]
- 12.Audit Commission. A Prescription for Improvement. Towards more rational prescribing in general practice. London: Audit Commission, Stationery Office, 1994. [Google Scholar]
- 13.Harris CM, Darjda R. The scale of repeat prescribing. British Journal of General Practice 1996;46(412): 649–53. [PMC free article] [PubMed] [Google Scholar]
- 14.Purves I, Kennedy J. The Quality of General Practice Repeat Prescribing. Newcastle upon Tyne; University of Newcastle upon Tyne, 1994. [Google Scholar]
- 15.Zermansky AG, Alldred DP, Petty DR. et al. Clinical medication review by a pharmacist of elderly people living in care homes: randomised controlled trial. Age and Ageing 2006;35:586–91. [DOI] [PubMed] [Google Scholar]
- 16.Myers AH, Baker SP, Van Natta M, Abbey H, Robinson EG. Risk factors associated with falls and injuries among elderly institutionalised persons. American Journal of Epidemiology 1991;133:1179–90. [DOI] [PubMed] [Google Scholar]
- 17.Ray WA, Griffin MR, Malcolm E. Cyclic antidepressants and the risk of hip fracture. Archives of Internal Medicine 1991;151:754–6. [PubMed] [Google Scholar]
- 18.Roose SP, Glassman AH, Giardina EGV. et al. Tricyclic antidepressants in depressed patients with cardiac disease. Archives of General Psychiatry 1987;44:273–5. [DOI] [PubMed] [Google Scholar]
- 19.Li X, Hamdy R, Sandborn W, Chi D, Dyer A. Long term effects of antidepressants on balance, equilibrium, and postural reflexes. Psychiatry Research 1996;63:191–6. [DOI] [PubMed] [Google Scholar]
- 20.Parashottam B Thapa, Gideon P, Milam AB, Ray WA. Antidepressants and the risk of falls among nursing home residents. New England Journal of Medicine 1998; 339:857–82. [DOI] [PubMed] [Google Scholar]
- 21.Liu B, Anderson G, Mittman N. et al. Use of selective seratonin reuptake inhibitors of tricyclic antidepressants and the risk of hip fractures in elderly people. Lancet 1998;351:1303–7. [DOI] [PubMed] [Google Scholar]
- 22.Kirsch I, Brett JD, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial Severity and Antidepressant Benefits: A Meta-Analysis of Data Submitted to the Food and Drug Administration. PLOS Medicine 2008. http://medicine.plosjournals.org/perlserv/?request=get-document&doi=10.1371/journal.pmed.0050045&ct=1 [DOI] [PMC free article] [PubMed]
- 23.Weiner DK, Hanlon JT, Studenski SA. Effects of central nervous system polypharmacy on falls liability in community dwelling elderly. Gerontology 1998;44(4):217–21. [DOI] [PubMed] [Google Scholar]
- 24.Clarke KW, Gray D, Hampton JR. Evidence of inadequate investigation and treatment of patients with heart failure. British Heart Journal 1994;71:584–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wheeldon NM, McDonald TM, Flucker CJ. et al. Echocardiography in chronic heart failure in the community. Quarterly Journal of Medicine 1993;86:17–23. [PubMed] [Google Scholar]
- 26.Michalsen A, Konig G, Thimme W. Preventative causative factors leading to hospital admission with decompensated heart failure. Heart 1998;80:437–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institute for Health and Clinical Excellence. Management of Chronic Heart Failure in Adults in Primary and Secondary Care. Clinical Guideline No. 5 London: NICE, 2003. www.nice.org.uk [Google Scholar]
- 28.Hall S, Cigarroa C, Marcoux L. et al. Time course of improvement in left ventricular function, mass and geometry in patients with congestive heart failure treated with beta-adrenergic blockade. Journal of the American College of Cardiology 1995;25(5):1154–61. [DOI] [PubMed] [Google Scholar]
- 29.McGavock H. A Review of the Literature on Drug Adherence. London: Royal Pharmaceutical Society of Great Britain, 1997. [Google Scholar]
- 30.Thompson PG. Preventing falls in the elderly at home; a community based approach. Medical Journal of Australia 1996;164:530–32. [PubMed] [Google Scholar]