Abstract
Intravenous iron is widely used for the treatment of iron deficiency anemia when oral iron is inappropriate, ineffective or poorly tolerated. Acute hypersensitivity reactions during iron infusions are very rare but can be life-threatening. This paper reviews their frequency, pathogenesis and risk factors, and provides recommendations about their management and prevention. Complement activation-related pseudo-allergy triggered by iron nanoparticles is probably a more frequent pathogenetic mechanism in acute reactions to current formulations of intravenous iron than is an immunological IgE-mediated response. Major risk factors for hypersensitivity reactions include a previous reaction to an iron infusion, a fast iron infusion rate, multiple drug allergies, severe atopy, and possibly systemic inflammatory diseases. Early pregnancy is a contraindication to iron infusions, while old age and serious co-morbidity may worsen the impact of acute reactions if they occur. Management of iron infusions requires meticulous observation, and, in the event of an adverse reaction, prompt recognition and severity-related interventions by well-trained medical and nursing staff.
Introduction
Intravenous (IV) iron is increasingly used for the treatment of iron deficiency anemia (IDA) when oral iron is ineffective or poorly tolerated and when it or blood transfusion is inappropriate.1,2 It is also indicated in combination with erythropoiesis-stimulating agents in chronic kidney disease and chemotherapy-induced anemia. While acute reactions during iron infusions are very infrequent, they can be life threatening.
In 2013, the European Medicines Agency (EMA) published a report of their 2-year investigation of the adverse drug reactions to all IV iron drugs available in Europe3 (Table 1). The formulations considered were sodium ferric gluconate, iron sucrose, iron (III)-hydroxide dextran complex, ferric carboxymaltose, and iron (III) isomaltoside 1000.
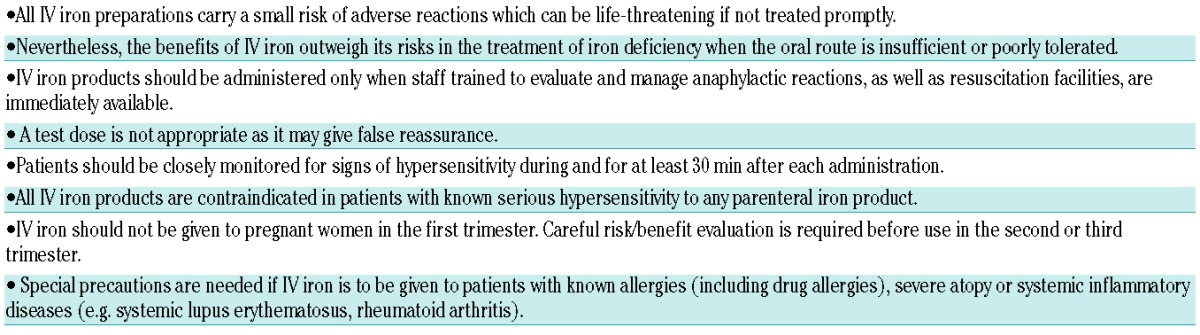
Table 1.
Summary of conclusions of the 2013 EMA report3 on IV iron products.
The aims of the present article are:
to outline the frequency and outcomes of reactions to IV iron;
to summarize current views about the pathogenesis of such reactions;
to indicate the risk factors for reactions to IV iron; and
to provide detailed guidance on risk minimization and management of iron infusions and acute reactions to them.
We are unaware of any existing guidance on how to prevent and manage hypersensitivity reactions (HSRs) to this increasingly used treatment, and intend this paper primarily for healthcare professionals, whether they be doctors or nurses, who prescribe and administer IV iron. Our aim is to offer advice that has been developed from a comprehensive literature search and iterative expert review about best practice before, during and after administration of IV iron to patients with IDA.
Terminology
Current nomenclature relating to acute adverse reactions to IV drugs is confusing, inconsistent and sometimes contradictory. In this report, we refer to all acute reactions to IV iron as hypersensitivity reactions (HSRs), sub-dividing them into mild, moderate or severe/life-threatening, depending on their clinical presentation. We have adopted the World Allergy Organisation proposal that the term “anaphylaxis” is reserved for severe HSRs,4 irrespective of pathogenesis, and avoid the term “anaphylactoid”, which historically has been used loosely to denote either non-immunological or even mild HSRs.
Methods
We undertook literature searches in PUBMED and EMBASE using the search terms “intravenous”, “anaphylaxis”, “anaphylactic”, “anaphylactoid”, “iron” as major subject headings or occurring in the title/abstract. These searches were supplemented by refined drug-class specific searches with the term “infusion reactions”. Secondary searches were made manually by screening articles retrieved by the online searches. Articles giving experimental data on adverse reactions to IV drugs were selected along with major anaphylaxis guidelines.
We concluded from these searches that: a) no existing anaphylaxis treatment guideline is strictly evidence-based, since the very rare occurrence of severe acute infusion reactions precludes randomized clinical trials as to how they should be managed; and b) there is so little information specifically relating to IV iron reactions that indirect evidence relating to acute reactions to other intravenous drugs had to be considered in preparing the present guidance.
We, therefore, assembled a panel of experienced clinicians from fields of medicine in which IDA is common (gastroenterology, hematology, immunology, internal medicine, nephrology, obstetrics and gynecology), as well as experts in the pharmacology of drug reactions and IV iron. Our recommendations result from development of a consensus in which the working group went through an iterative process of literature review and discussion of current clinical practice about each measure proposed.
Preparation of paper and declaration of interests
One of the authors (DSR) initiated this review but considered that it could not be undertaken without administrative and financial support to assemble the necessary international clinical expertise. The pharmaceutical company Pharmacosmos funded two one-day meetings in Copenhagen for the initial preparation of the paper. All available IV iron drugs were considered and no distinctions have been made between them in terms of safety or efficacy (see below). The pharmaceutical company had no editorial influence on the study and were not invited to approve the manuscript. No medical writer or unacknowledged authors were involved.
Frequency and outcomes of hypersensitivity reactions to intravenous iron infusions
Unlike previous authors, who had used a range of methodologies and assessed products that included poorly-tolerated high molecular weight dextran preparations which are no longer available,5–8 the EMA were unable to differentiate between current IV iron products in relation to the risk of severe HSRs. In this context, Wysowski et al.9 also concluded, from US data, that “because of under-reporting, possible differential reporting, absence of iron dextran brand names, and incomplete use (denominator) data, incidence rate and relative risk estimates cannot be calculated”. Death and other severe long-term sequelae arising from use of IV iron are very rare. In the largest such study to date, death certificate data from the US National Center for Health Statistics between 1979–2005 showed that there were around 3 deaths/year ascribed to iron infusions in the US, approximating 1 for every 5 million doses of IV iron sold.9,10
Pathogenesis of hypersensitivity reactions to intravenous iron
Mechanisms by which iron infusions induce adverse reactions may vary with the iron preparation used and with the pre-existing morbidity of the recipient. They cannot be distinguished by their clinical presentation. The two main possibilities are immunological IgE-mediated responses, for example, to the dextran component of IV iron preparations containing this molecule, and complement activation-related pseudo-allergy (CARPA).11 There are, however, no data to support the concept that IgE-mediated hypersensitivity commonly accounts for reactions to current formulations of IV iron.12,13 CARPA may be the most common mechanism of acute HSRs provoked by any infusion containing nanoparticles, of which all existing IV iron preparations consist.14 The final common pathway of these processes is likely to include activation of mast cells and basophils, either directly, or via anaphylatoxins (C3a and C5a) that increase in blood as a consequence of complement activation. The secretion products of these cells, which include histamine, thromboxanes, leukotrienes and platelet-activating factor,11 trigger smooth muscle contraction, increased capillary permeability and loss of fluid from the intravascular space. Subsequent bronchospasm, laryngeal edema, tachycardia, hypo- or hypertension, hypoxia and reduced tissue perfusion can culminate, in severe HSRs, in loss of consciousness, circulatory collapse (shock), and cardiac and respiratory arrest.15
A fast iron infusion rate is a well-recognized risk factor, one possible explanation being the rapid increase in labile free iron observed in this situation.16 However, prevention of HSRs by reducing the speed of infusion is an effective practice not only with IV iron but also with other reactogenic drugs, so the phenomenon is unlikely to be solely due to higher levels of free iron. For example, it is also possible that, after rapid injection of IV iron, the clearance rate from the blood of anaphylatoxins by carboxypeptidase N and by uptake by blood and other cells is exceeded by their rate of production, leading to exacerbation of the CARPA pathogenic sequences described above.11,15
Risk factors for hypersensitivity reactions to intravenous iron
Several factors have been suggested, on an evidence base of varying robustness, as predisposing to, on the one hand, an increased risk of an HSR occurring in patients given IV iron, and on the other, to a reaction, which if it occurs, has a worse outcome in the iron recipient. These factors have recently been re-stated by the EMA3 and represent a relative contraindication to the administration of IV iron to patients presenting them (Table 2). If IV iron is to be given to individuals with any of these risk factors, an extremely slow infusion rate and meticulous observation is recommended (see below).
Table 2.
Factors increasing risk and/or severity of hypersensitivity reactions (HSRs) in patients given iron infusions.
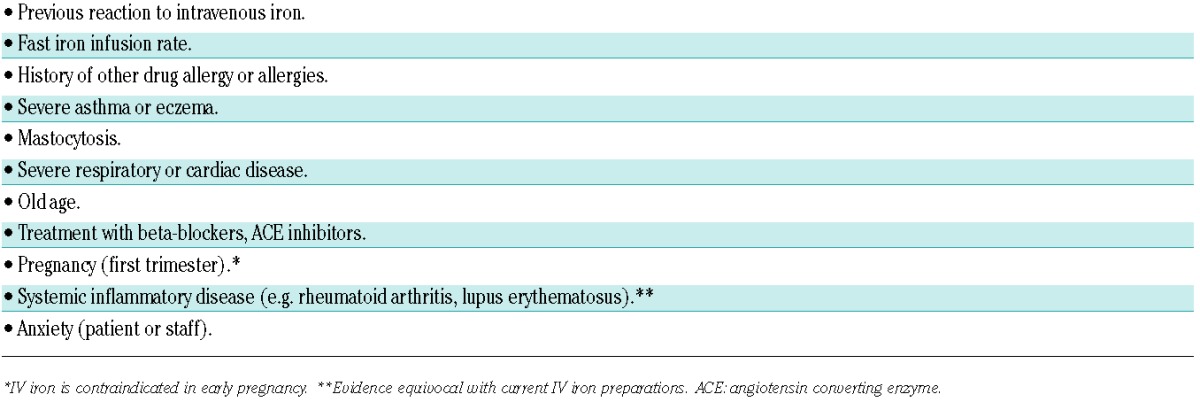
Some of the factors, such as a previous adverse reaction to IV iron or other drugs, a fast iron infusion rate (see above), a history of severe atopy and systemic mastocytosis, appear to increase both the incidence and severity of HSRs.3,11
In contrast, pre-existing severe respiratory or cardiac disease, old age and the use of beta-blockers or ACE inhibitors, may worsen the outcome of an HSR if it occurs.17 In pregnancy, IV iron is contraindicated in the first trimester3,18 since there are no trials confirming its safety during this time: existing data suggest that its use should be confined to the second or third trimester of pregnancy if the benefit is judged to outweigh the risks for both mother and fetus.18,19 While earlier anecdotal reports suggested that iron dextran may worsen disease activity in patients with rheumatoid arthritis and lupus erythematosus,20 more recent data indicate that IV iron could even have a beneficial effect on the underlying disease.21
Lastly, it has been suggested that anxiety on the part of healthcare professionals giving IV drugs increases the risk of HSRs.22
Management of intravenous iron infusions and hypersensitivity reactions
-
How can we reduce the risk of HSRs to intravenous iron? Hypersensitivity reactions may occur in anyone given IV iron, and it is essential that every effort is made to prevent these being poorly managed if they occur, whether due to inadequate facilities or staff being undertrained. The following factors require attention before and during any IV iron infusion.
Location: iron infusions should be given only on appropriately staffed sites equipped with resuscitation facilities.3 If IV iron is to be given outside hospital, there should be arrangements in place for immediate treat-and-transfer to an intensive care facility in the event of a severe reaction. The EMA3 states that iron should not be infused in the home.
Personnel: in most countries, IV iron is given by nursing staff with immediate access to on-site medical help in the event of an adverse reaction. All staff should have regularly up-dated training in management of IV infusions and adverse reactions to them. The confidence and competence provided by regular training should help reduce any anxiety on the part of the healthcare professional (HCP) and, conceivably, the risk of HSRs.22 The HCP administering the iron infusion should be in the infusion area and easily accessible by the patient throughout its course, as HSRs can develop rapidly.
The patient: information should be provided about the risk of an HSR before the iron infusion, if possible using a visual aid to indicate its rarity.23 The relevant symptoms should be described, with instructions to tell the HCP administering the infusion immediately if any occur.
Administration of intravenous iron: this should be preceded by a (re-)check for risk factors for an HSR (Table 2), the general condition of the patient and base-line observations including pulse rate, blood pressure and respiratory rate. The infusion should be prepared as stated in the manufacturer’s instructions. No test dose of IV iron is necessary, because it can give false reassurance about the safety of the subsequent therapeutic infusion.3 However, on the basis of clinical experience, we recommend that the iron infusion should be initiated at less than 50% of the rate recommended by the manufacturer and not increased to the recommended rate until it is clear that it is being well-tolerated (usually 10–15 min). We suggest observation/monitoring every 15 min and for 30 min after the infusion finishes.
Risk minimization: while anyone having IV iron should be regarded as susceptible to HSR, some people are at higher risk than others (Table 2). In such individuals, the prescribing clinician should take a carefully considered decision as to whether the potential risks associated with an iron infusion are outweighed by its benefits.3 If so, in addition to the requirements itemized above, it is recommended that, in case of urgent need by the HCP giving the infusion, an experienced doctor is in close proximity throughout the infusion. The infusion should be given at 10% of the recommended rate for the first 15 min. Monitoring should continue for 30–60 min after the infusion. A previous HSR to IV iron increases the risk of an adverse response to a subsequent iron infusion. In line with the EMA’s conclusions,3 we recommend that, unless their previous reaction was due to exceptional circumstances (e.g. very rapid iron infusion), no-one who has had a severe HSR to IV iron should have a subsequent infusion of any iron products. After a mild-moderate previous HSR, the same IV iron preparation should not be used again, and a different one used only after careful consideration by the clinician responsible and the patient, as to whether the potential benefits exceed the risks.3
-
How are HSRs diagnosed and graded¿
For ease of recognition and prompt and appropriate management, acute HSRs to iron infusions, as to other IV drugs, are best classified as mild, moderate or severe/life-threatening (or anaphylactic) (Figure 1).24,25
Reactions can be identified on the basis of subjective symptoms, objective signs and bedside monitoring. Diagnosis of an HSR does not require the presence of every feature shown in Figure 1. Mild reactions can progress rapidly through moderate to severe; the latter can also occur from the outset without progression through the milder syndromes. Symptoms such as metallic taste and mild headache are part of the normal pharmacological response to IV iron and are not of clinical significance.
A further mild acute adverse reaction has been described by Fishbane.1,26 This occurs in approximately 1 in 100 of those given intravenous drugs and is characterized by transient flushing and truncal myalgia (pains in the back and chest) with joint pains. Its pathogenesis has not been investigated. The symptoms abate spontaneously over a few minutes and do not usually recur on re-challenge.
-
How should hypersensitivity reactions to intravenous iron be managed¿
Management of an HSR to IV iron depends on the severity of the event and is out-lined in the algorithm shown in Figure 1. As stated at the outset, there is scanty evidence relating specifically to management of iron infusions: the recommendations made below are drawn from other contexts in which IV drugs are given.17,27–31
The selection of individual drugs for treatment of HSRs and their doses and routes of administration vary and can be modified according to local practice.
-
Mild HSR: the features of a mild HSR tend to be more subjective than objective (Figure 1). The patient often feels increasingly anxious: a calm explanation of what is being felt will provide reassurance and the realization that the HCP is experienced and knows how to proceed (Figure 1).
Our stepwise advice to the HCP dealing with a mild HSR is:
stop the infusion for at least 15 min and assess the response;
if the member of staff giving the infusion is not medically qualified, immediately alert the attending physician, recheck the vital signs, and watch for progression or resolution of the HSR;
if there is an improvement over a few minutes, cautiously resume the iron infusion after 15 min at no more than 50% of the initial infusion rate;
if all goes well, complete the infusion and continue observations for at least 1 h to ensure there are no recurrent symptoms;
if there is no resolution in 5–10 min, or if at any time the symptoms and signs worsen, manage as for a moderate HSR (Figure 1).
-
Moderate HSR: moderate HSRs may develop from mild reactions, or start without any prodrome. Transient cough is a common initial feature. The symptoms include those of a mild HSR, with more marked chest tightness and shortness of breath (Figure 1). The pulse rate may rise and blood pressure fall.
Management is as for a mild HSR with immediate additional measures (Figure 1):
stop the iron infusion immediately if it is still running;
if there has been a rise in heart rate and fall in blood pressure, give an isotonic fluid load (e.g. 500 mL 0.9% saline, Ringer’s or Hartmann’s solution) and lie the patient horizontally. Although not clearly evidence-based, an IV corticosteroid (e.g. hydrocortisone 100–500 mg) can be considered;
if there is improvement, continue monitoring for at least 1 h;
-
in the event of deterioration, immediately implement the measures applying to management of a severe HSR.
While previously recommended by some, both as pre-medication against and treatment of HSRs, the role of IV H1 blockers has recently been questioned.30 Their therapeutic benefit is unclear, and indeed, by sometimes potentiating tachycardia, hypotension and somnolence, H1 antagonists can make an HSR appear more hemodynamically significant.
-
Severe/life-threatening HSR (anaphylaxis): an anaphylactic reaction may be of sudden onset, or occur as a rapid worsening of the features of a moderate HSR. There will be increasing wheeze, due to bronchospasm, sometimes with stridor associated with laryngeal edema. Increasing tiredness and distress will occur, and periorbital edema may develop. Increasing hypoxia leads to confusion. If the HSR worsens, pallor, clamminess, cyanosis and loss of consciousness progress quickly to cardiac and respiratory arrest. During this time, the pulse accelerates and the blood pressure and oxygen saturation fall.
A severe HSR is a major medical emergency:
if the HSR occurs in a hospital, call the emergency response team immediately;
if hypotension is severe, give IV adrenaline [epinephrine; 0.1 mg (1 mL) as a 1/10,000 solution over 5 min]. Continuous ECG and blood pressure monitoring is essential in case of arrhythmia or a hypertensive response to the adrenaline;
if the iron infusion is being given outside a hospital, adrenaline by intramuscular injection into the anterolateral thigh [0.3–0.5 mg (0.3–0.5 mL) 1/1000 solution] may be safer.26
give oxygen at a high rate (>10 L/min) initially by face mask, with a nebulized β2-adrenergic agonist and/or ipratropium to combat wheezing;
rapid volume load with 1–2 L 0.9% saline or similar isotonic fluid (see Moderate HSR above);
give an IV corticosteroid (see Moderate HSR above) if not already administered as part of management of a moderate HSR;
-
the on-site advanced cardiac and life support (ACLS) team should implement standard protocols in the event of cardiac or respiratory arrest.
If the patient responds well to initial measures, they should be observed carefully for at least 4 h after resolution; observation for up to 24 h may be necessary for elderly or frail patients or those in high-risk categories (Table 1). While there is a theoretical risk of a biphasic event in patients having HSRs, this has not been clearly described after iron infusions. Where response is not immediate and complete, prompt transfer for further management to an appropriate high dependency or intensive care facility is necessary.
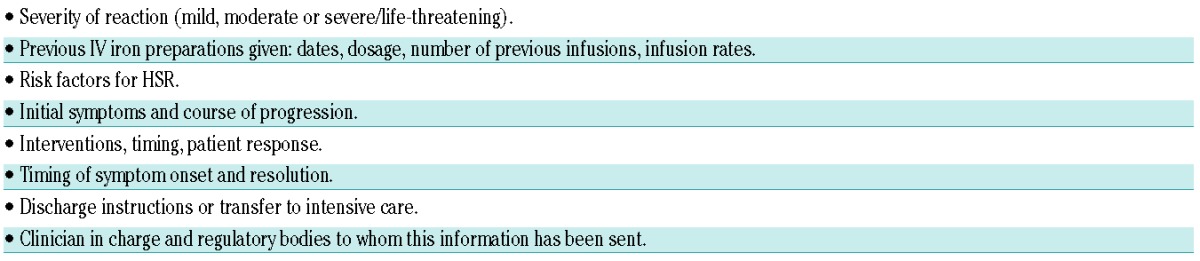
Documentation of hypersensitivity reaction after resolution: in every HSR, the clinician responsible should be notified promptly and the event carefully documented using a pro forma designed along the lines suggested in Table 3. The report should be filed in the patient’s case records; this will help the clinician to decide how to treat the anemia in the future. A report of every HSR should also be submitted to the appropriate national regulatory body.
-
Figure 1.
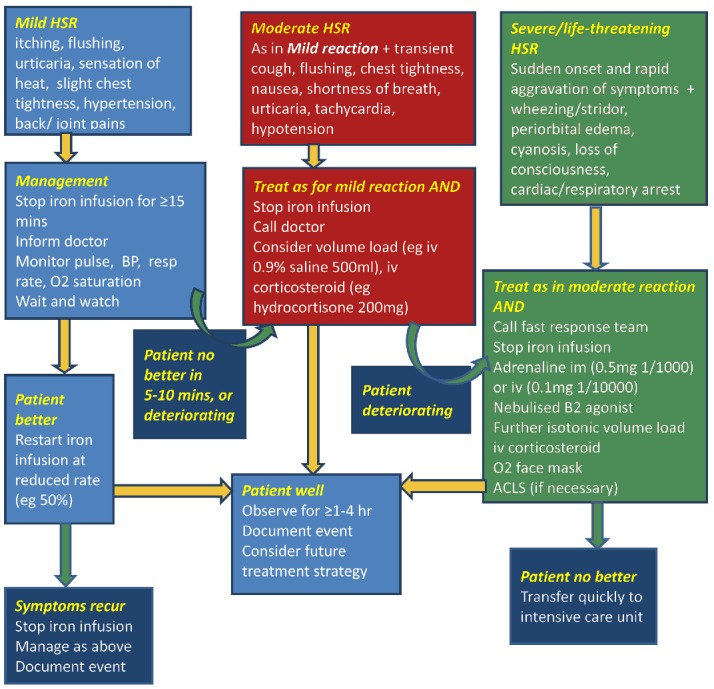
Algorithm outlining grading and management of acute hypersensitivity reactions to intravenous iron infusions. Details are given in the text.
Table 3.
Information to be recorded in patients’ case records immediately after any IV iron-related hypersensitivity reaction (HSR) (adapted from Vogel29). This information helps to determine future treatment strategies.
Conclusions
There is a paucity of evidence about how to manage HSRs to iron infusions. The rarity of HSRs means that there will never be a formal clinical trial to assess optimal therapeutic measures. Areas in which further research is needed and could be productive, however, include clarification of the pathogenesis of HSRs, risk definition in individual patients and in different diseases, and the role of pre-medication and risk reduction protocols in high-risk patients.
Hypersensitivity reactions to IV iron are rare but potentially life-threatening. They are at least partly preventable by implementation of risk minimization measures. Their management requires prompt recognition and grading of severity, together with meticulous monitoring and immediate treatment. All staff involved in giving iron infusions need regular training to ensure that when these rare events develop they are dealt with calmly and expeditiously.
Footnotes
Authorship and Disclosures
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Auerbach M, Ballard H, Glaspy J. Clinical update: intravenous iron for anaemia. Lancet. 2007;369(9572):1502–4. [DOI] [PubMed] [Google Scholar]
- 2.Auerbach M, Ballard H. Clinical use of intravenous iron: administration, efficacy, and safety. Hematology Am Soc Hematol Educ Program. 2010;2010:338–47. [DOI] [PubMed] [Google Scholar]
- 3.European Medicines Agency. New recommendations to manage risk of allergic reactions with intravenous iron-containing medicines. European Medicines Agency 2013. EMA/579491/2013:1–3 Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/IV_iron_31/WC500151308.pdf
- 4.Johansson SG, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol. 2004;113(5):832–6. [DOI] [PubMed] [Google Scholar]
- 5.Chertow GM, Mason PD, Vaage-Nilsen O, Ahlmen J. Update on adverse drug events associated with parenteral iron. Nephrol Dial Transplant. 2006;21(2):378–82. [DOI] [PubMed] [Google Scholar]
- 6.Critchley J, Dunbar Y. Adverse events associated with intravenous iron infusion (low-molecular-weight iron dextran and iron sucrose): a systematic review. Transfusion Altern Transfusion Med. 2007;9(1):8–36. [Google Scholar]
- 7.Bailie GR, Verhoef JJ. Differences in the reporting rates of serious allergic adverse events from intravenous iron by country and population. Clin Adv Hematol Oncol. 2012;10(2):101–8. [PubMed] [Google Scholar]
- 8.Bailie GR. Comparison of rates of reported adverse events associated with i.v. iron products in the United States. Am J Health Syst Pharm. 2012;69(4):310–20. [DOI] [PubMed] [Google Scholar]
- 9.Wysowski DK, Swartz L, Borders-Hemphill BV, Goulding MR, Dormitzer C. Use of parenteral iron products and serious anaphylactic-type reactions. Am J Hematol. 2010;85(9):650–4. [DOI] [PubMed] [Google Scholar]
- 10.Cherlow GM, Winkelmayer WC. Commentary: on the relative safety of intravenous iron formulations. New answers, new questions. Am J Hematol. 2010;85(9): 643–4. [DOI] [PubMed] [Google Scholar]
- 11.Szebeni J. Complement activation-related pseudoallergy: a new class of drug-induced acute immune toxicity. Toxicology. 2005; 216(2–3):106–21. [DOI] [PubMed] [Google Scholar]
- 12.Novey HS, Pahl M, Haydik I, Vaziri ND. Immunologic studies of anaphylaxis to iron dextran in patients on renal dialysis. Ann Allergy. 1994;72(3):224–8. [PubMed] [Google Scholar]
- 13.Fleming LW, Stewart WK, Parratt D. Dextran antibodies, complement conversion and circulating immune complexes after intravenous iron dextran therapy in dialysed patients. Nephrol Dial Transplant. 1992;7(1):35–9. [PubMed] [Google Scholar]
- 14.Szebeni J. Hemocompatibility testing for nanomedicines and biologicals: predictive assays for complement mediated infusion reactions. Eur J Nanoparticles. 2012;1(1); 33–53. [Google Scholar]
- 15.Szebeni J, Baranyi L, Sávay S, Bodó M, Milosevits J, Alving CR, et al. Complement activation-related cardiac anaphylaxis in pigs: role of C5a anaphylatoxin and adenosine in liposome-induced abnormalities in ECG and heart function. Am J Physiol Heart Circ Physiol. 2006;290(3):H1050–8. [DOI] [PubMed] [Google Scholar]
- 16.Jahn MR, Andreasen HB, Fütterer S, Nawroth T, Schünemann V, Kolb U, et al. A comparative study of the physicochemical properties of iron isomaltoside 1000 (Monofer), a new intravenous iron preparation and its clinical implications. Eur J Pharm Biopharm. 2011;78(3):480–91. [DOI] [PubMed] [Google Scholar]
- 17.Simons FE, Ardusso LR, Bilo MB, El-Gamal YM, Ledford DK, Ring J, et al. World allergy organization guidelines for the assessment and management of anaphylaxis. World Allergy Organ J. 2011;4(2):13–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pavord S, Myers B, Robinson S, Allard S, Strong J, Oppenheimer C, British Committee for Standards in Haematology. UK guidelines on the management of iron deficiency in pregnancy. Br J Haematol. 2012;156(5):588–600. [DOI] [PubMed] [Google Scholar]
- 19.Reveiz L, Gyte GML, Cuervo LG, Casasbuenas A. Treatments for iron-deficiency anaemia in pregnancy. Cochrane Database Syst Rev. 2011. October 5;(10):CD003094. [DOI] [PubMed] [Google Scholar]
- 20.Blake DR, Lunec J, Ahern M, Ring EF, Bradfield J, Gutteridge JM. Effect of intravenous iron dextran on rheumatoid synovitis. Ann Rheum Dis. 1985;44(3):183–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weiss G, Schett G. Anaemia in inflammatory rheumatic diseases. Nat Rev Rheumatol. 2013;9(4):205–15 [DOI] [PubMed] [Google Scholar]
- 22.Runge VM. Safety of magnetic resonance contrast media. Top Magn Reson Imaging. 2001;12(4):309–14. [DOI] [PubMed] [Google Scholar]
- 23.Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. BMJ. 2002;324(7341):827–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ring J, Messmer K. Incidence and severity of anaphylactoid reactions to colloid volume substitutes. Lancet. 1977;1(8009):466–9. [DOI] [PubMed] [Google Scholar]
- 25.Brown SG. Clinical features and severity grading of anaphylaxis. J Allergy Clin Immunol. 2004;114(2):371–6. [DOI] [PubMed] [Google Scholar]
- 26.Fishbane S, Ungureanu VD, Maesaka JK, Kaupke CJ, Lim V, Wish J. The safety of intravenous iron dextran in hemodialysis patients. Am J Kidney Dis. 1996;28(4):529–34. [DOI] [PubMed] [Google Scholar]
- 27.Resuscitation Council UK Emergency treatment of anaphylactic reactions. Guidelines for healthcare providers. Available from: https://www.resus.org.uk/pages/reaction.pdf [DOI] [PubMed]
- 28.Ring J, Grosber M, Mohrenschlager M, Brockow K. Anaphylaxis: acute treatment and management. Chem Immunol Allergy. 2010;95:201–10. [DOI] [PubMed] [Google Scholar]
- 29.Vogel WH. Infusion reactions, diagnosis assessment, management. Clin J Oncol Nurs. 2010;14(2):E10–21. [DOI] [PubMed] [Google Scholar]
- 30.Goss JE, Chambers CE, Heupler FA., Jr Systemic anaphylactoid reactions to iodinated contrast media during cardiac catheterization procedures: guidelines for prevention, diagnosis, and treatment. Laboratory Performance Standards Committee of the Society for Cardiac Angiography and Interventions. Cathet Cardiovasc Diagn. 1995;34(2):99–104. [DOI] [PubMed] [Google Scholar]
- 31.Gafter-Gvili A, Steensma DP, Auerbach M. Should the ASCO/ASH guidelines for the use of intravenous iron in cancer- and chemotherapy-induced anemia be updated? J Nat Compr Cancer Netwk. 2014; 12(5):657–64. [DOI] [PubMed] [Google Scholar]


