Abstract
The high degree of comorbidity among mental disorders has generated interest in identifying transdiagnostic processes associated with multiple types of psychopathology. Susan Nolen-Hoeksema conceptualized rumination as one such transdiagnostic process associated with depression, anxiety, substance abuse, binge eating, and self-injurious behavior. The degree to which rumination accounts for the co-occurrence of internalizing and externalizing psychopathology, however, has never been tested. We used a sample of early adolescents (N = 1,065) assessed at 3 time points spanning 7 months to examine (a) the reciprocal prospective associations between rumination and aggressive behavior in adolescents, (b) whether rumination explained the longitudinal associations of aggressive behavior with depression and anxiety symptoms, and (c) gender differences in these associations. Rumination predicted increases over time in aggressive behavior, and aggression was associated with increases in rumination over time only for boys. Rumination fully mediated the longitudinal association of aggression with subsequent anxiety symptoms and of both depression and anxiety symptoms with subsequent aggression in boys but not girls. Rumination did not explain the association between aggression and subsequent depressive symptoms for either boys or girls. These findings provide novel evidence for the role of rumination as a transdiagnostic factor underlying transitions between internalizing and externalizing symptoms among males during early adolescence. Interventions aimed at reducing rumination may have beneficial influences on multiple forms of psychopathology and on the development of comorbidity.
Keywords: rumination, transdiagnostic, depression, anxiety, aggression
The high rates of comorbidity among mental disorders (e.g., Kessler et al., 2005; Watson, 2009) suggest that existing diagnostic categories may share more similarities than differences. Indeed, quantitative models suggest that the underlying structure of associations between mental disorders is best characterized by a two-factor model reflecting two broad categories of internalizing and externalizing psychopathology (Krueger, 1999; Krueger & Markon, 2006). The overlap between specific diagnostic categories has led to an interest in the development of conceptual frameworks to identify cognitive, affective, and neurobiological processes that are shared across disorders (e.g., Aldao, 2012; Ehring & Watkins, 2008; Harvey, Watkins, Mansell, & Shafran, 2004; Hofmann, Sawyer, Fang, & Asnaani, 2012; Nolen-Hoeksema & Watkins, 2011). This transdiagnostic approach has gained considerable attention over the past decade, as evidenced by the growing number of empirical investigations testing transdiagnostic hypotheses (e.g., Aldao & Nolen-Hoeksema, 2010; Aldao, Nolen-Hoeksema, & Schweizer, 2010; McLaughlin & Nolen-Hoeksema, 2011, 2012). In addition, it has informed the development of novel psychosocial interventions (e.g., Barlow, Allen, & Choate, 2004; Dear et al., 2011; Hayes, Strosahl, & Wilson, 1999). These developments suggest that the next decade will be characterized by an even greater interest in transdiagnostic models of psychopathology.
Susan Nolen-Hoeksema recently conceptualized rumination as an important transdiagnostic process (Nolen-Hoeksema & Watkins, 2011). Although Nolen-Hoeksema’s early work focused on the role of rumination in depression (e.g., Nolen-Hoeksema, 1991), her more recent research demonstrated that rumination predicts multiple forms of psychopathology in adults and youth (Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008), including depression (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Rood, Roelofs, Bogels, Nolen-Hoeksema, & Schouten, 2009), anxiety (Mellings & Alden, 2000; Verstraeten, Bijttebier, Vasey, & Raes, 2011), binge eating (Nolen-Hoeksema, Stice, Wade, & Bohon, 2007), binge drinking (Nolen-Hoeksema & Harrell, 2002; Nolen-Hoeksema et al., 2007), and self-injurious behavior (Hilt, Cha, & Nolen-Hoeksema, 2008; Hoff & Muehlenkamp, 2009). Although most of these studies examined rumination in the context of a single form of psychopathology, recent cross-sectional and longitudinal investigations by Nolen-Hoeksema and colleagues provide evidence supporting the transdiagnostic nature of rumination as a factor underlying symptom co-occurrence in adults (Aldao & Nolen-Hoeksema, 2010; Watkins, 2009) and adolescents (McLaughlin & Nolen-Hoeksema, 2011, 2012).
Nolen-Hoeksema and Watkins (2011) argued that rumination is a common factor underlying the development and comorbidity of multiple forms of psychopathology. To date, studies examining rumination as a transdiagnostic factor have primarily focused on its role in explaining the co-occurrence of various forms of internalizing psychopathology. In this investigation, we sought to build on this transdiagnostic approach by examining rumination as a factor explaining temporal co-occurrence between internalizing and externalizing problems in adolescents, focusing specifically on aggressive behavior. This is particularly important because internalizing disorders frequently co-occur with aggressive behaviors in children and adolescents (Angold, Costello, & Erkanli, 1999; Biederman, Faraone, Mick, & Lelon, 1995; Kessler et al., 2012), and the majority of youth referred to treatment for aggression have comorbid internalizing diagnoses (e.g., Kazdin & Whitley, 2006). Children and adolescents with internalizing problems are more likely to develop conduct disorder and engage in aggression than their healthy counterparts (Lewinsohn et al., 1994; Offord et al., 1992), and youths with aggressive behaviors are at elevated risk of developing depression and anxiety in adolescence and young adulthood (Burke, Loeber, Lahey, & Rathouz, 2005; Kim-Cohen et al., 2003; Lewinsohn, Rohde, & Seeley, 1995; Rohde, Lewinsohn, & Seeley, 1991). The process by which aggressive behaviors might lead to the development of internalizing conditions has been described in the failure model (Capaldi, 1992), which argues that aggressive and disruptive behaviors lead to conflict, social rejection, and failure experiences in social relationships and academic contexts that increase risk for anxiety and depression (Capaldi, 1992). Less attention has been devoted to delineating the mechanisms underlying the transition from internalizing disorders to aggressive behaviors.
It is possible that rumination might play a role in the transitions between internalizing problems and aggressive behavior in adolescents. Although Nolen-Hoeksema’s research focused primarily on the role of rumination in internalizing problems and escapist behaviors (i.e., binge eating and substance abuse; Heatherton & Baumeister, 1991), other theorists have argued that rumination plays an important role in the development of aggression (Caprara, 1986). According to such models, a provocation can be followed either by dissipation of anger or rumination on the provocation. Experimental evidence indicates that self-focused rumination following provocation leads to increases in aggressive behavior (Bettencourt, Talley, Benjamin, & Valentine, 2006; Bushman, Bonacci, Pedersen, Vasquez, & Miller, 2005; Vasquez et al., 2013). Using Nolen-Hoeksema and Watkins’s (2011) framework of divergent trajectories, we propose that aggressive behavior might be another outcome associated with rumination, with provocation events serving as a potential specific trigger that leads to aggression. Rumination might therefore underlie transitions from internalizing disorders characterized by high engagement in rumination, specifically depression and anxiety, to aggressive behavior. Rumination might also be involved in transitions from aggression to internalizing problems. Consistent with the failure model (Capaldi, 1992), adolescents with high levels of aggressive behavior are likely to experience a variety of negative social and academic consequences; these failure experiences might increase the likelihood of engagement in rumination. Indeed, stressful life events and social rejection have previously been shown to predict increases over time in rumination among adolescents (McLaughlin, Hatzenbuehler, & Hilt, 2009; Michl, McLaughlin, Shepherd, & Nolen-Hoeksema, 2013). Thus, in this investigation, we examined the extent to which rumination accounts for the reciprocal prospective associations between internalizing and externalizing pathology.
We approached this question by drawing on two areas of psychopathology research that were the focus of Nolen-Hoeksema’s work: (a) the role of emotion regulation strategies in shaping developmental trajectories of psychopathology, and (b) gender differences in those trajectories. One of the recommendations Nolen-Hoeksema and Watkins (2011) made was to place greater emphasis on developmental trajectories. Nolen-Hoeksema initially conceptualized rumination as a coping style that increased people’s vulnerability to depression (Nolen-Hoeksema, 1991) and anxiety (Nolen-Hoeksema, 2000). In a series of longitudinal and experimental studies, she provided evidence for the role of rumination in predicting increases over time in symptoms of depression and anxiety, novel onsets of major depression, and greater duration and severity of depressive episodes in samples of adults (Nolen-Hoeksema, 2000; Nolen-Hoeksema & Morrow, 1991; Nolen-Hoeksema, Morrow, & Fredrickson, 1993; Nolen-Hoeksema, Parker, & Larson, 1994). Similar patterns were later observed in samples of adolescents, with rumination predicting anxiety and depression trajectories characterized by increasing symptoms over time (McLaughlin & Nolen-Hoeksema, 2011, 2012; Nolen-Hoeksema, Girgus, & Seligman, 1992). More recently, Nolen-Hoeksema also demonstrated that rumination predicted later increases in symptoms of eating disorders and substance abuse (Nolen-Hoeksema et al., 2007). This line of work highlights the role of rumination as a risk factor for the development of both internalizing and externalizing psychopathology across the life course. The degree to which rumination is involved in the co-occurrence of internalizing and externalizing psychopathology over time, however, has not been previously examined.
Nolen-Hoeksema’s work also contributed to the development of a more nuanced understanding of gender differences in psychopathology, particularly depression. She wrote a series of influential theoretical papers on gender differences in the prevalence of major depression, arguing that females’ greater use of rumination in response to negative affect was one factor that accounted for these differences (Nolen-Hoeksema, 1987, 1990; Nolen-Hoeksema & Girgus, 1994). A large body of work has shown that females are more likely to engage in rumination than males (for reviews, see Nolen-Hoeksema & Hilt, 2009; Rood et al., 2009). This greater use of rumination in response to distress explains, at least in part, gender differences in risk for depression among adolescents and adults (Grant et al., 2004; Hilt, McLaughlin, & Nolen-Hoeksema, 2010; Nolen-Hoeksema, Larson, & Grayson, 1999; Roberts, Gilboa, & Gotlib, 1998), providing compelling support for Nolen-Hoeksema’s theory. Germane to this investigation, gender differences have recently been examined in studies of rumination as a transdiagnostic factor. Specifically, although rumination is more common in females than males, a recent study found no evidence of gender differences in the degree to which rumination explains concurrent and longitudinal co-occurrence of depression and anxiety symptoms (McLaughlin & Nolen-Hoeksema, 2011). If rumination does, indeed, explain co-occurrence of internalizing and externalizing psychopathology, it is possible that these relationships might vary across gender. For example, boys are more likely to engage in aggressive behavior relative to girls (Bettencourt & Miller, 1996; Card, Stucky, Sawalani, & Little, 2008). If rumination is more likely to lead to aggressive behavior in boys than girls, rumination may be a transdiagnostic factor in internalizing–externalizing symptom overlap only for boys (see Aldao, 2012).
In the current study, we extend Nolen-Hoeksema’s work on rumination as a transdiagnostic factor by examining rumination as a mechanism underlying the longitudinal associations between internalizing symptoms and aggressive behavior in adolescents. Specifically, we evaluated the temporal associations between rumination and aggression and the degree to which rumination explains (a) the longitudinal associations of depression and anxiety symptoms with subsequent changes in aggressive behavior, and (b) the longitudinal associations of aggressive behavior with subsequent changes in symptoms of depression and anxiety. We predicted that rumination would account for the reciprocal relationships between internalizing problems and aggressive behavior. We additionally investigated gender differences in the extent to which rumination explained the longitudinal co-occurrence of internalizing symptoms and aggressive behavior. We did not have specific predictions regarding possible gender differences in these associations, given the limited data on rumination and aggressive behavior.
Method
Participants
Adolescents were recruited from the total enrollment of two middle schools (Grades 6 to 8) in a small urban community in central Connecticut (metropolitan population of 71,538). Schools were selected for the study based on demographic characteristics of the school district and their willingness to participate. Students in self-contained special education classrooms and technical programs who did not attend school for the majority of the day did not participate.
The parents of all eligible children (N = 1,567) in the participating middle schools were asked to provide active consent for their children to participate in the study. Parents who did not return written consent forms to the school were contacted by telephone. Twenty-two percent of parents did not return consent forms and could not be reached to obtain consent, and 6% of parents declined to provide consent. Adolescent participants provided written assent. The overall participation rate in the study at baseline was 72%.
The baseline sample included 51.2% (n = 545) boys and 48.8% (n = 520) girls. Participants were evenly distributed across grade level (mean age = 12.2 years, SD = 1.0). The race/ethnic composition of the sample was as follows: 13.2% (n = 141) non-Hispanic White, 11.8% (n = 126) non-Hispanic Black, 56.9% (n = 610) Hispanic/Latino, 2.2% (n = 24) Asian/Pacific Islander, 0.2% (n = 2) Native American, 0.8% (n = 9) Middle Eastern, 9.3% (n = 100) biracial/multiracial, and 4.2% (n = 45) other racial/ethnic groups. Twenty-seven percent (n = 293) of participants reported living in single-parent households. These patterns are consistent with overall sociodemographic distributions from the schools that participated in the study. The participating middle schools reside in a predominantly low-SES community, with a per capita income of $18,404 (Connecticut Department of Education, 2006). School records indicated that 62.3% of students qualified for free or reduced lunch in the 2004 to 2005 school year.
Two additional assessments took place after the baseline assessment. Of the baseline participants, 221 (20.8%) did not participate at the Time 2 assessment, and 217 (20.4%) did not participate at the Time 3 assessment, largely due to transient student enrollment in the district. Over the 4-year period from 2000 to 2004, 22.7% of students had left the school district (Connecticut Department of Education, 2006).
Measures
Rumination
The Children’s Response Styles Questionnaire (CRSQ; Abela, Brozina, & Haigh, 2002) is a 25-item scale that assesses the extent to which children respond to sad feelings with rumination (defined as self-focused thought concerning the causes and consequences of depressed mood), distraction, or problem solving. The measure is modeled after the Response Styles Questionnaire (Nolen-Hoeksema & Morrow, 1991) that was developed for adults. For each item, youths are asked to rate how often they respond in a particular way when they feel sad on a 4-point Likert scale ranging from almost never (1) to almost always (4). Sample items include, “Think about a recent situation wishing it had gone better” and “Think ‘Why can’t I handle things better?’” The reliability and validity of the CRSQ have been demonstrated in samples of early adolescents (Abela et al., 2002). The CRSQ rumination scale demonstrated good reliability in this study (α = .86).
Aggressive behavior
A revised version of the Peer Experiences Questionnaire (RPEQ; Prinstein, Boergers, & Vernberg, 2001) was used to assess participants’ engagement in aggression toward peers. The RPEQ included 18 items that assess peer-directed aggressive behavior. Participants rate how often they engage in a specific behavior toward others in the past year (e.g., “I threatened to hurt or beat up another kid”) on a 5-point Likert scale ranging from never (1) to a few times a week (5). The RPEQ has high internal consistency and convergent validity (Prinstein et al., 2001). The RPEQ demonstrated good internal consistency in this sample (α = .90).
Depressive symptoms
The Children’s Depression Inventory (CDI; (Kovacs, 1992) is a widely used self-report measure of depressive symptoms in children and adolescents. The CDI includes 27 items consisting of three statements (e.g., “I am sad once in a while,” “I am sad many times,” “I am sad all the time”) representing different levels of severity of a specific symptom of depression. The CDI has sound psychometric properties, including internal consistency, test–retest reliability, and discriminant validity (Kovacs, 1992; Reynolds, 1994). The item pertaining to suicidal ideation was removed from the measure at the request of school officials and the human subjects committee. The CDI demonstrated good reliability in this sample (α = .82).
Anxiety symptoms
The Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997) is a 39-item measure of child anxiety. The MASC assesses physical symptoms of anxiety, harm avoidance, social anxiety, and separation anxiety, and is appropriate for children ages 8 to 19. Each item presents a symptom of anxiety, and participants indicate how true each item is for them on a 4-point Likert scale ranging from never true (0) to very true (3). Example items include, “I feel tense or uptight” and “My heart races or skips beats.” The MASC has high internal consistency and test–retest reliability across 3-month intervals, and established convergent and divergent validity (Muris, Merckelbach, Ollendick, King, & Bogie, 2002). The MASC demonstrated good reliability in this sample (α = .88).
Procedure
Participants completed study questionnaires during their homeroom period. Symptom measures were administered at Time 1 and Time 3, and rumination was measured at all three time points. Four months elapsed between the Time 1 (November 2005) and Time 2 (March 2006) assessments, and three months elapsed between Time 2 and Time 3 (June 2006) assessments. This time frame was chosen to allow the maximum time between assessments to observe changes in internalizing and externalizing symptoms while also ensuring that all assessments occurred within the same academic year to avoid high attrition. Participants were assured of the confidentiality of their responses and the voluntary nature of their participation. The study was approved by the Institutional Review Board at Yale University.
Data Analysis
Structural equation modeling was used to perform the mediation analyses using Mplus 7.1 software (Muthén & Muthén, 2012). Analyses were conducted using the full-information maximum likelihood (FIML) estimation method to handle missing data. Estimation with FIML is superior to other procedures for handling missing data, such as listwise deletion, and is less likely to produce biased estimates (Schafer & Graham, 2002).1 Multiply indicated latent variables were created for rumination, aggressive behavior, depressive symptoms, and anxiety symptoms using parcels of items from the relevant scales (see Supplemental materials). Parcels were created using the domain representative approach, which accounts for the multidimensionality of these constructs, such that each parcel included items from each of these subscales (Little, Cunningham, Shahar, & Widaman, 2002). The use of parcels to model constructs as latent factors, as opposed to an observed variable representing a total scale score, confers a number of psychometric advantages including greater reliability, reduction of error variance, and increased efficiency (Kishton & Wadaman, 1994; Little et al., 2002). Subscales used to create parcels were drawn from the established lower order factors of each construct based on prior research and exploratory factor analysis in our data. Subscales of rumination included brooding, reflection, and dysphoria (Treynor, Gonzalez, & Nolen-Hoeksema, 2003); subscales of aggressive behavior included overt, relational, and reputational aggression, and lack of prosocial behavior (Prinstein et al., 2001); subscales of depressive symptoms included internalizing (dysphoria, self-deprecation, and social problems) and externalizing (school problems, and aggression/disobedience) dimensions (Craighead, Smucker, Craighead, & Ilardi, 1998); and subscales of anxiety symptoms included physical symptoms, social anxiety, harm avoidance, and separation anxiety (March et al., 1997).
After testing the measurement model for all constructs, we examined the role of rumination as a mechanism (a) linking aggressive behavior to subsequent increases in depression and anxiety symptoms, and (b) linking depression and anxiety symptoms to subsequent increases in aggressive behavior. Analyses were first examined in the total sample. We then conducted multigroup analyses to examine whether the process of mediation was moderated by gender. The regression coefficients for the mediation paths were constrained to be equal for males and females, and the difference in model fit was examined using a chi-square test. When a significant deterioration in model fit was observed after constraining these paths to equality, we estimated the final mediation model separately for males and females. Mediation analyses proceeded as follows: (a) Time 1 aggressive behavior was examined as a predictor of depression and anxiety symptoms at Time 3, controlling for Time 1 symptoms; (b) Time 1 aggression was examined as a predictor of Time 2 rumination, controlling for Time 1 rumination; (c) Time 2 rumination was evaluated as a predictor of depression and anxiety symptoms at Time 3, controlling for Time 1 rumination and symptoms; and (d) the full mediation model was examined to test the hypothesis that rumination mediates the longitudinal associations between aggressive behavior and subsequent internalizing symptoms. The indirect effect was estimated using the product of coefficients approach, and the significance of this effect was estimated using a bootstrapping procedure that provides 95% confidence intervals around the indirect effect (MacKinnon, Fritz, Williams, & Lockwood, 2007). We estimated 500 resamples in Mplus for each indirect effect. Confidence intervals that do not include zero indicate a significant indirect effect. This approach is associated with low bias and Type I error rate, accurate standard errors, and adequate power to detect small effects in large samples (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). The final mediation model accounted for the covariance between aggressive behavior, depressive symptoms, and rumination. A separate set of mediation analyses were conducted using this same approach to evaluate whether rumination mediates the longitudinal association between symptoms of depression and anxiety at Time 1 and aggressive behavior at Time 3, controlling for Time 1 aggressive behavior.
Results
Attrition
Missing data were present for 20.1% to 25.1% of participants present at the Time 1 assessment for primary variables of interest. Participants who completed the Time 1 but not the Time 2 assessment were more likely to be female, χ2(1) = 6.85, p < .01, and from a single-parent household, χ2(1) = 8.93, p < .01, but did not differ in grade level, race/ethnicity, Time 1 anxiety, depression, rumination, or aggressive behavior (ps > 0.10) compared with those who completed both assessments. Participants who were lost to follow-up by the Time 3 assessment were more likely to be from a single-parent household, χ2(1) = 26.92, p < .001, and had higher Time 1 symptoms of depression, F(1, 1065) = 9.63, p = .002, than adolescents who were present at all three assessments but did not differ in gender, race/ethnicity, or Time 1 anxiety symptoms.
Descriptive Statistics
Table 1 displays the mean and standard deviation of all measures at each time point by gender. Table 2 provides the zero-order correlations among all study measures. As expected, rumination was positively associated with aggressive behavior and symptoms of depression and anxiety, which were positively associated with one another.
Table 1.
Means and Standard Deviations of Rumination, Symptoms of Anxiety and Depression, and Aggressive Behavior
| Male
|
Female
|
|
|---|---|---|
| Measure | M (SD) | M (SD) |
| Time 1 | ||
| CRSQ Rumination | 9.40 (7.12) | 12.53 (7.84) |
| CDI Depression | 9.11 (6.37) | 10.25 (6.47) |
| MASC Anxiety | 36.67 (14.98) | 43.95 (14.94) |
| RPEQ Aggressive Behavior | 6.19 (6.24) | 5.30 (6.11) |
| Time 2 | ||
| CRSQ Rumination | 8.72 (6.66) | 12.24 (8.17) |
| Time 3 | ||
| CRSQ Rumination | 8.26 (7.31) | 11.43 (8.25) |
| CDI Depression | 9.70 (8.18) | 10.73 (7.74) |
| MASC Anxiety | 31.64 (18.51) | 37.49 (17.22) |
| RPEQ Aggressive Behavior | 6.88 (6.88) | 6.49 (6.68) |
Note. CRSQ = Children’s Response Styles Questionnaire; CDI = Children’s Depression Inventory; MASC = Multidimensional Anxiety Scale for Children; RPEQ = Revised Peer Experiences Questionnaire.
Table 2.
Correlations Between Rumination, Symptoms of Depression and Anxiety, and Aggressive Behavior
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. CRSQ | — | ||||||||
| Rumination T1 | |||||||||
| 2. CDI | .42* | — | |||||||
| Depression T1 | |||||||||
| 3. MASC | .55* | .28* | — | ||||||
| Anxiety T1 | |||||||||
| 4. RPEQ | .16* | .31* | .11* | — | |||||
| Aggressive Behavior T1 | |||||||||
| 5. CRSQ | .57* | .39* | .43* | .17* | — | ||||
| Rumination T2 | |||||||||
| 6. CRSQ | .48* | .35* | .41* | .17* | .61* | — | |||
| Rumination T3 | |||||||||
| 7. CDI | .23* | .54* | .13* | .28* | .33* | .44* | — | ||
| Depression T3 | |||||||||
| 8. MASC | .35* | .24* | .53* | .14* | .44* | .69* | .33* | — | |
| Anxiety T3 | |||||||||
| 9. RPEQ | .17* | .23* | .12* | .38* | .20* | .28* | .27* | .20* | — |
| Aggressive Behavior T3 |
Note. CRSQ = Children’s Response Styles Questionnaire; CDI = Children’s Depression Inventory; MASC = Multidimensional Anxiety Scale for Children; RPEQ = Revised Peer Experiences Questionnaire.
p < .01.
Measurement Model
The latent variables for rumination, aggressive behavior, depressive symptoms, and anxiety symptoms were each created from four parcels. The measurement model that included all four of these constructs and modeled the covariation between all constructs was a good fit to the data, χ2(98) = 370.55, p < .001, comparative fit index (CFI) = 0.97, and root mean square error of approximation (RMSEA) = .05, 90% CI [.04, .06].
Longitudinal Mediation Analyses
Aggressive behavior and subsequent depressive symptoms
In the total sample, aggressive behavior at Time 1 was associated with elevated depressive symptoms at Time 3, controlling for Time 1 depression, β = .11, p = .006, and this association did not vary by gender, χ2(1) = 1.02, p = .31. We next examined the role of rumination as a mediator of the association between aggression and depressive symptoms.
Time 1 aggression was associated with rumination at Time 2, controlling for Time 1 rumination, β = .08, p = .043. Rumination at Time 2 predicted Time 3 depressive symptoms, controlling for Time 1 rumination and depression, β = .17, p = .002. In the final mediation model, Time 1 aggressive behavior remained a significant predictor of Time 3 depressive symptoms, controlling for Time 1 depression and rumination, when Time 2 rumination was added to the model, β = .12, p = .004. The indirect effect of aggressive behavior on depressive symptoms through rumination was not statistically significant, β = .01, 95% CI [−.01, .01]. Fit indices indicated that the model fit the data well: χ2(162) = 469.7, p < .001, CFI = .96, and RMSEA = .05, 90% CI [.04, .05]. When the mediation paths of interest were constrained to equivalence across males and females, the model fit did not significantly worsen, χ2(5) = 8.12, p = .15, indicating that the process and strength of mediation was consistent across gender.
Aggressive behavior and subsequent anxiety symptoms
In the total sample, aggressive behavior at Time 1 was associated positively with anxiety symptoms at Time 3, controlling for Time 1 anxiety, β = .08, p = .029, and this association did not vary by gender, χ2(1) = 0.02, p = .88.
Time 1 aggression behavior was associated with rumination at Time 2, controlling for Time 1 rumination, β = .08, p = .043. Rumination at Time 2 predicted Time 3 anxiety symptoms, controlling for Time 1 rumination and anxiety, β = .40, p < .001. In the final mediation model, Time 1 aggressive behavior was no longer associated with Time 3 anxiety symptoms, controlling for Time 1 anxiety and rumination, when Time 2 rumination was added to the model, β = .05, p = .140. The indirect effect of aggressive behavior on anxiety symptoms through rumination was significant, β = .40, 95% CI [.01, .10]. The final mediation model fit the data well: χ2(162) = 453.15, p < .001, CFI = .98, and RMSEA = .04 90% CI [.03, .04].
We found evidence for variation in these relationships by gender, as evidenced by a significant reduction in model fit when the mediation paths were constrained to equivalence for boys and girls, χ2(5) = 11.11, p = .049. We re-estimated the mediation model, allowing the mediation paths to vary by gender, to determine which path differed for boys and girls. Two gender differences were observed in the model. First, Time 1 aggressive behavior was associated with Time 2 rumination among boys, β = .17, p = .003, but not among girls, β = .05, p = .37, after controlling for Time 1 rumination. In addition, the indirect effect of aggression on anxiety symptoms through rumination was statistically significant for boys, β = .05, 95% CI [.03, .23], but not for girls, β = .01, 95% CI [−.03, .08]. Figure 1 exhibits the full mediation model for boys. Fit indices for this final model, which estimated mediation paths separately for boys and girls, indicated good fit to the data: χ2(354) = 697.07, p < .001, CFI = .97, and RMSEA = .04, 90% CI [.04, .05]).
Figure 1.
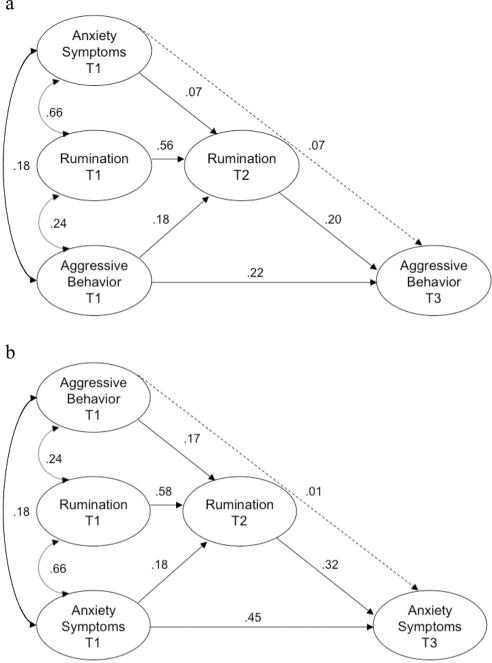
Final mediation model for the longitudinal association between (a) anxiety symptoms and aggressive behavior, and (b) aggressive behavior and anxiety symptoms among boys. Numbers represent standardized path coefficients (β). All paths shown are significant (p < .05), except those drawn with broken lines. All constructs were modeled as latent variables. Due to space constraints, indicator variables are not displayed.
Depressive symptoms and subsequent aggressive behavior
In the total sample, depressive symptoms at Time 1 were associated positively with aggressive behavior at Time 3, controlling for Time 1 aggression, β = .15, p = .002, and this association did not vary by gender, χ2(1) = 0.36, p = .55.
Time 1 depressive symptoms were associated positively with rumination at Time 2, controlling for Time 1 rumination, β = .19, p < .001. Rumination at Time 2 was associated positively with Time 3 aggressive behavior, controlling for Time 1 rumination and aggression, β = .15, p < .001. In the final mediation model, Time 1 depressive symptoms were no longer associated with Time 3 aggressive behavior, controlling for Time 1 aggression and rumination, when Time 2 rumination was added to the model, β = .08, p = .137. The indirect effect of depressive symptoms on aggressive behavior through rumination was significant, β = .02, 95% CI [.01, .07]. Fit indices indicated excellent fit to the data: χ2(162) = 489.6, p < .001, CFI = .97, and RMSEA = .04, 90% CI [.04, .04]).
These associations varied by gender, as evidenced by multi-group analyses revealing a significant reduction in model fit when the mediation paths were constrained to equivalence for boys and girls, χ2(5) = 12.80, p = .025. We next estimated the mediation model again and allowed the mediation paths to vary by gender in order to determine which path differed for boys and girls. Two gender differences were observed in the model. Among boys, rumination at Time 2 was associated with aggressive behavior at Time 3, controlling for Time 1 aggression and rumination, β = .23, p < .003, but Time 2 rumination was not associated with Time 3 aggressive behavior among girls, β = .07, p = .30. In addition, the indirect effect of depressive symptoms on aggressive behavior through rumination was significant among boys, β = .06, 95% CI [.01, .11], but not among girls, β = .02, 95% CI [−.02, .05]). Time 1 depressive symptoms were no longer associated with Time 3 aggressive behavior among boys, controlling for Time 1 aggression and rumination, when Time 2 rumination was added to the model, β = .02, p = .84. The final model estimating the mediation paths separately for boys and girls fit the data well: χ2(354) = 729.99, p < .001, CFI = .96, and RMSEA = .04, 90% CI [.04, .05].
Anxiety symptoms and subsequent aggressive behavior
In the total sample, anxiety symptoms at Time 1 were marginally associated with aggressive behavior at Time 3, controlling for Time 1 aggression, β = .08, p = .06, and this association varied by gender, χ2(1) = 5.42, p = .020. Specifically, the association between Time 1 anxiety symptoms and Time 3 aggressive behavior was significant for boys, β = .17, p = .011, but not for girls, β = −.04, p = .53. Because anxiety symptoms did not predict changes in aggressive behavior and rumination was not associated with subsequent changes in aggressive behavior among girls, we estimated the mediation model separately for boys only.
Among boys, Time 1 anxiety symptoms were associated positively with rumination at Time 2, controlling for Time 1 rumination, β = .66, p < .001. Rumination at Time 2 predicted Time 3 aggressive behavior, controlling for Time 1 rumination and aggression, β = .20, p = .015. In the final mediation model, Time 1 anxiety symptoms were no longer associated with Time 3 aggressive behavior, controlling for Time 1 anxiety and rumination, when Time 2 rumination was added to the model, β = .08, p = .33. The indirect effect of anxiety symptoms on aggressive behavior through rumination was marginally significant, β = .01, 95% CI [.00, .02]. Fit indices indicated excellent fit to the data: χ2(354) = 662.03, p < .001, CFI = .97, and RMSEA = .04, 90% CI [.04, .05]).
Discussion
Nolen-Hoeksema and colleagues have argued that rumination is a transdiagnostic factor involved in the etiology and co-occurrence of multiple forms of psychopathology (Nolen-Hoeksema & Watkins, 2011). Indeed, a growing literature suggests that rumination is associated concurrently and prospectively with a range of mental health problems (Aldao & Nolen-Hoeksema, 2010; Nolen-Hoeksema, 2000; Nolen-Hoeksema & Morrow, 1991; Nolen-Hoeksema et al., 2007). Yet only recently has rumination been examined as a factor explaining comorbidity within the same individuals across time (McLaughlin & Nolen-Hoeksema, 2011). We extend this literature by providing the first evidence, to our knowledge, that rumination explains the co-occurrence of internalizing symptoms and aggressive behavior over time, and that this association is specific to adolescent males.
We examined symptom co-occurrence by investigating the longitudinal associations between internalizing symptoms and aggressive behavior. We found evidence for reciprocal relationships, such that aggressive behavior predicted subsequent increases in both depression and anxiety symptoms, and depression and anxiety symptoms each predicted subsequent increases in aggression. These findings are consistent with numerous previous studies documenting elevated risk of depression and anxiety among youths with disruptive behavior problems, and heightened risk of conduct disorder and aggression among children with depression and anxiety symptoms (Angold & Costello, 1993; Angold et al., 1999; Biederman, Faraone, Mick, & Lelon, 1995; Bird, Gould, & Staghezza, 1993; Burke et al., 2005; Kim-Cohen et al., 2003; Lewinsohn et al., 1994, 1995; Offord et al., 1992; Rohde et al., 1991). Structural models of comorbidity also find strong associations between the underlying dimensions of internalizing and externalizing psychopathology (Krueger, 1999; Krueger & Markon, 2006). These associations were observed for both male and female adolescents with one exception: Anxiety symptoms were not associated with increases over time in aggressive behavior among girls. This suggests that adolescent girls might have a different pattern of symptom co-occurrence over time than boys, such that only certain types of internalizing problems (i.e., depressive symptoms) predict aggressive behavior in girls, whereas both anxiety and depressive symptoms are associated with aggression in males. This pattern might be explained, in part, by gender differences in the expression of aggressive behavior. For example, prior research suggests that relational aggression, which is more common in females than in males, is more strongly associated with depressive symptoms than with anxiety (Crick & Grotpeter, 1995).
Rumination emerged as an important mechanism explaining the longitudinal associations between internalizing symptoms and aggressive behavior for boys but not for girls. Our findings indicated that rumination predicts subsequent aggressive behaviors, and aggressive behaviors predict subsequent rumination, among adolescent boys only. Moreover, we found among adolescent boys but not girls that (a) rumination underlies the transition from aggressive behavior to anxiety, and (b) rumination explains the association of both depression and anxiety symptoms with subsequent increases in aggressive behavior.
Why might rumination explain the transition from aggressive behavior to anxiety among adolescent boys only? One potential explanation is that adolescent boys and girls ruminate about different kinds of problems, with boys more likely to ruminate following their own aggressive behavior. This pattern may be, in part, a function of boys’ greater tendency to engage in aggressive behavior, as well as gender differences in the manifestation of aggressive behavior. Boys are more likely than girls to engage in overt forms of aggression, such as physical aggression, in contrast to relational aggression (Crick & Grotpeter, 1995). This suggests that boys might experience more serious social and academic consequences for these behaviors (Burke et al., 2005; Capaldi, 1992; Dodge, 1993; Dodge et al., 2003) that may fuel rumination about the causes and consequences of those negative events and failure experiences. In this respect, rumination in response to these experiences might increase risk for the development of future anxiety symptoms.
Our findings also indicated that rumination explained the transition from internalizing symptoms to aggressive behavior among boys but not girls. Prior research suggests that boys with stronger masculine identity are more likely to engage in rumination during adolescence than those with less masculine gender role identification (Broderick & Korteland, 2004; Cox, Mezulis, & Hyde, 2010). As such, it is possible that males who ruminate are more likely to express the more stereotypically masculine behavior of aggression compared with crying or other depression-related behaviors. Alternatively, rumination in male adolescents with high levels of internalizing symptoms might lead to aggressive behavior if they are faced with provocation events (e.g., bullying). According to dissipation-rumination models of aggression, rumination on provocation events leads to increases in later aggression (e.g., Caprara, 1986). Male adolescents with internalizing pathology might be more likely to be bullied or subjected to other kinds of provocation (e.g., Egan & Perry, 1998; Hodges & Perry, 1999) and therefore might be more likely to ruminate on those provocation events when they occur. Although we assessed a general tendency to engage in rumination in response to sad mood, rather than rumination in response to specific provocations, it is likely that individuals with a ruminative response style are likely to ruminate following many different types of stressors (Robinson & Alloy, 2003), including provocation.
Importantly, rumination did not explain the longitudinal associations between internalizing symptoms and aggressive behavior among adolescent girls. As discussed previously, aggressive behavior predicted subsequent internalizing symptoms, and depressive symptoms predicted subsequent aggression among both boys and girls, but these relationships were not explained by rumination for girls. Factors other than rumination, such as other types of emotion dysregulation, social rejection, social-information-processing deficits, or shared biological vulnerability, may explain the increased risk of aggressive behavior among depressed girls (Burke, Loeber, & Birmaher, 2002; Dodge, 1993). Delineating the mechanisms underlying co-occurrence of internalizing symptoms and aggressive behavior among female adolescents is an important topic for future research.
This investigation had several limitations that warrant discussion. First, we assessed symptoms of depression, anxiety, and aggressive behaviors via self-report questionnaires. Although this approach is common in large sample studies, it nonetheless remains important to investigate the prospective associations between rumination and internalizing and externalizing disorders in adolescents diagnosed via clinical interview. Similarly, the use of a normative sample likely resulted in a restriction of variance in our symptom measures, which might help explain the nonsignificant mediation by rumination of the relationship between aggression and subsequent depression. Replicating these findings in clinical or high-risk samples of adolescents is therefore important. In addition, because we assessed rumination in response to sad mood, we were unable to specifically test whether rumination in response to anger or provocation (Bushman et al., 2005; Vasquez et al., 2013) or in response to stressful life events (Robinson & Alloy, 2003) might also contribute to explaining the associations between internalizing and externalizing psychopathology over time. This also prevented us from testing whether boys were indeed ruminating more than girls specifically about their aggressive behaviors. Thus, it will be essential for future investigations of rumination to anchor the use of such strategies to specific events, using retrospective as well as experience sampling designs (see Aldao, 2013). Importantly, the associations between depressive symptoms and aggressive behavior in our sample could be biased upward due to the presence of several items in the CDI that reflect externalizing behaviors that are common in children with depressive symptoms (disobedience, discord with peers, and poor school performance). Because the CDI is a validated scale whose psychometric properties are well-established (Kovacs, 1992; Reynolds, 1994), we retained these items in our analysis. However, we conducted a sensitivity analysis by recreating the CDI parcels after dropping the three items that reflect externalizing behaviors. The longitudinal association between depressive symptoms and changes in aggressive behavior remained significant, and the longitudinal association between aggressive behavior and changes in depressive symptoms also remained significant.2 An additional consideration is that our study design favored our hypothesized mediation model, because rumination was assessed at a time point (i.e., Time 2) that was closer in proximity to our outcomes (i.e., Time 3) than the psychopathology predictors measured at Time 1. This highlights the importance of replicating these findings in future multiwave longitudinal studies. Finally, although the associations of aggressive behavior with anxiety symptoms and rumination were statistically significant, the overall magnitude of associations was small. The associations of anxiety and depression with aggressive behavior are consistent with patterns in population-based data suggesting much greater overlap of adolescent disorders within the internalizing and externalizing dimensions than across these domains (Kessler et al., 2012). The associations between rumination and aggressive behavior suggest that rumination likely plays a much stronger role in the etiology of internalizing compared with externalizing problems, and that a variety of other factors are also involved in the transitions between internalizing and externalizing problems in adolescents.
Our findings suggest that rumination is an important transdiagnostic risk factor underlying the transitions between internalizing symptoms and aggressive behavior among adolescent boys. Although boys are less likely to ruminate than girls, rumination has negative consequences irrespective of gender, and explains specific patterns of symptom co-occurrence for boys. Our findings indicate that male youths with either internalizing symptoms or conduct problems could benefit from interventions targeting rumination, which might reduce comorbidity with internalizing problems over time. More generally, these findings offer support for extending the transdiagnostic model of rumination (Nolen-Hoeksema & Watkins, 2011) from internalizing psychopathology and escapist behaviors to encompass aggressive behavior. It is important that future research examine gender differences in this wider range of rumination-related outcomes, as patterns seen for depression might not extend to other forms of psychopathology. As the work on transdiagnostic factors continues to grow, it will be essential to examine whether the extent to which dysfunctional processes explain symptom comorbidity is a function of contextual factors, varies across the life-course, and is moderated by individual-level characteristics, including gender. Susan Nolen-Hoeksema’s pioneering work in these areas laid the groundwork for many exciting areas of inquiry in the future, and her legacy will continue to influence psychopathology research for many generations to come.
Supplementary Material
Acknowledgments
Katie A. McLaughlin was supported by a National Institute of Mental Health (NIMH) grant (K01-MH092526); Blair E. Wisco was supported by a NIMH grant (T32MH019836-15A2) awarded to Terence M. Keane.
Footnotes
We were all extremely fortunate to benefit from Susan’s mentorship as graduate students in her lab. In addition to being a gifted scientist, she was a generous, supportive, and dedicated mentor who was an inspiring role model to all of us. Susan always encouraged us to reach for the stars and believed we could achieve anything we set our minds to. We miss her terribly.
An alternative to FIML estimation is multiple imputation. We conducted a sensitivity analysis to determine whether parameter estimates for the main mediation paths of interest were similar when using FIML estimation compared with multiple imputation, and there were no meaningful differences in parameter estimates across these approaches.
When the three items on the CDI reflecting externalizing behaviors were removed, the longitudinal association between depressive symptoms and changes in aggressive behavior remained significant (p = .013), and the longitudinal association between aggressive behavior and changes in depressive symptoms also remained significant (p = .006).
Contributor Information
Katie A. McLaughlin, Department of Psychology, University of Washington
Blair E. Wisco, Department of Psychology, University of North Carolina-Greensboro
Amelia Aldao, Department of Psychology, The Ohio State University.
Lori M. Hilt, Department of Psychology, Lawrence University
References
- Abela JR, Brozina K, Haigh EP. An examination of the response styles theory of depression in third- and seventh-grade children: A short-term longitudinal study. Journal of Abnormal Child Psychology. 2002;30:515–527. doi: 10.1023/A:1019873015594. [DOI] [PubMed] [Google Scholar]
- Aldao A. Emotion regulation strategies as transdiagnostic processes: A closer look at the invariance of their form and function. Spanish Journal of Clinical Psychology. 2012;17:261–277. [Google Scholar]
- Aldao A. The future of emotion regulation research: Capturing context. Perspectives on Psychological Science. 2013;8:155–172. doi: 10.1177/1745691612459518. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S. Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behaviour Research and Therapy. 2010;48:974–983. doi: 10.1016/j.brat.2010.06.002. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ. Depressive comorbidity in children and adolescents: Empirical, theoretical, and methodological issues. The American Journal of Psychiatry. 1993;150:1779–1791. doi: 10.1176/ajp.150.12.1779. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. doi: 10.1111/1469-7610.00424. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/S0005-7894(04)80036-4. [DOI] [PubMed] [Google Scholar]
- Bettencourt BA, Miller N. Gender differences in aggression as a function of provocation: A meta-analysis. Psychological Bulletin. 1996;119:422–447. doi: 10.1037/0033-2909.119.3.422. [DOI] [PubMed] [Google Scholar]
- Bettencourt BA, Talley A, Benjamin AJ, Valentine J. Personality and aggressive behavior under provoking and neutral conditions: A meta-analytic review. Psychological Bulletin. 2006;132:751–777. doi: 10.1037/0033-2909.132.5.751. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Mick E, Lelon E. Psychiatric comorbidity among referred juveniles with major depression: Fact or artifact? Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:579–590. doi: 10.1097/00004583-199505000-00010. [DOI] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Staghezza BM. Patterns of diagnostic comorbidity in a community sample of children aged 9 through 16 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:361–368. doi: 10.1097/00004583-199303000-00018. [DOI] [PubMed] [Google Scholar]
- Broderick PC, Korteland C. A prospective study of rumination and depression in early adolescence. Journal of Clinical Child and Adolescent Psychology. 2004;9:383–394. [Google Scholar]
- Burke JD, Loeber R, Birmaher B. Oppositional defiant disorder and conduct disorder: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:1275–1293. doi: 10.1097/00004583-200211000-00009. [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry. 2005;46:1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Bushman BJ, Bonacci AM, Pedersen WC, Vasquez EA, Miller N. Chewing on it can chew you up: Effects of rumination on triggered displaced aggression. Journal of Personality and Social Psychology. 2005;88:969–983. doi: 10.1037/0022-3514.88.6.969. [DOI] [PubMed] [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: II. A 2-year follow-up at Grade 8. Development and Psychopathology. 1992;4:125–144. doi: 10.1017/S0954579400005605. [DOI] [PubMed] [Google Scholar]
- Caprara GV. Indicators of aggression: The Dissipation-Rumination scale. Personality and Individual Differences. 1986;7(86):763–769. 90074–7. doi: 10.1016/0191-8869. [DOI] [Google Scholar]
- Card NA, Stucky BD, Sawalani GM, Little TD. Direct and indirect aggression during childhood and adolescence: A meta-analytic review of gender differences, intercorrelations, and relations to maladjustment. Child Development. 2008;79:1185–1229. doi: 10.1111/j.1467-8624.2008.01184.x. [DOI] [PubMed] [Google Scholar]
- Connecticut Department of Education. Strategic school profile 2005–2006: New Britain Public Schools. Hartford, CT: Author; 2006. [Google Scholar]
- Cox SJ, Mezulis AH, Hyde JS. The influence of child gender role and maternal feedback to child stress on the emergence of the gender difference in depressive rumination in adolescence. Developmental Psychology. 2010;46:842–852. doi: 10.1037/a0019813. [DOI] [PubMed] [Google Scholar]
- Craighead WE, Smucker MR, Craighead LW, Ilardi SS. Factor analysis of the Children’s Depression Inventory in a community sample. Psychological Assessment. 1998;10:156–165. doi: 10.1037/1040-3590.10.2.156. [DOI] [Google Scholar]
- Crick NR, Grotpeter JK. Relational aggression, gender, and social-psychological adjustment. Child Development. 1995;66:710–722. doi: 10.2307/1131945. [DOI] [PubMed] [Google Scholar]
- Dear BF, Titov N, Schwencke G, Andrews G, Johnson L, Craske MG, McEvoy P. An open trial of a brief transdiagnostic Internet treatment for anxiety and depression. Behaviour Research and Therapy. 2011;49:830–837. doi: 10.1016/j.brat.2011.09.007. [DOI] [PubMed] [Google Scholar]
- Dodge KA. Social-cognitive mechanisms in the development of conduct disorder and depression. Annual Review of Psychology. 1993;44:559–584. doi: 10.1146/annurev.ps.44.020193.003015. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Lansford JE, Burks VS, Bates JE, Pettit GS, Fontaine R, Price JM. Peer rejection and social information-processing factors in the development of aggressive behavior in children. Child Development. 2003;74:374–393. doi: 10.1111/1467-8624.7402004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan SK, Perry DG. Does low self-regard invite victimization? Developmental Psychology. 1998;34:299–309. doi: 10.1037/0012-1649.34.2.299. [DOI] [PubMed] [Google Scholar]
- Ehring T, Watkins ER. Repetitive negative thinking as a transdiagnostic process. International Journal of Cognitive Therapy. 2008;1:192–205. doi: 10.1680/ijct.2008.1.3.192. [DOI] [Google Scholar]
- Grant KE, Lyons AL, Finkelstein JS, Conway KM, Reynolds LK, O’Koon JH, Hicks KJ. Gender difference in rates of depressive symptoms among low-income, urban, African American Youth: A test of two mediational hypotheses. Journal of Youth and Adolescence. 2004;33:523–533. doi: 10.1023/B:JOYO.0000048066.90949.be. [DOI] [Google Scholar]
- Harvey AG, Watkins E, Mansell W, Shafran R. Cognitive behavioural processes across psychological disorders. Oxford, UK: Oxford University Press; 2004. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford Press; 1999. [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Hilt LM, Cha CB, Nolen-Hoeksema S. Nonsuicidal self-injury in young adolescent girls: Moderators of the distress-function relationship. Journal of Consulting and Clinical Psychology. 2008;76:63–71. doi: 10.1037/0022-006X.76.1.63. [DOI] [PubMed] [Google Scholar]
- Hilt LM, McLaughlin KA, Nolen-Hoeksema S. Examination of the response styles theory in a community sample of young adolescents. Journal of Abnormal Child Psychology. 2010;38:545–556. doi: 10.1007/s10802-009-9384-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges EVE, Perry DG. Personal and interpersonal antecedents and consequences of victimization by peers. Journal of Personality and Social Psychology. 1999;76:677–685. doi: 10.1037/0022-3514.76.4.677. [DOI] [PubMed] [Google Scholar]
- Hoff ER, Muehlenkamp JJ. Nonsuicidal self-injury in college students: The role of perfectionism and rumination. Suicide and Life-Threatening Behavior. 2009;39:576–587. doi: 10.1521/suli.2009.39.6.576. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Fang A, Asnaani A. Emotion dysregulation model of mood and anxiety disorders. Depression and Anxiety. 2012;29:409–416. doi: 10.1002/da.21888. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Whitley MK. Comorbidity, case complexity, and effects of evidence-based treatment for children referred for disruptive behavior. Journal of Consulting and Clinical Psychology. 2006;74:455–467. doi: 10.1037/0022-006X.74.3.455. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, McLaughlin KA, Green JG, Lakoma MD, Pine DS, Sampson NA, Merikangas KR. Lifetime prevalence and comorbidity of DSM–IV disorders in the National Comorbidity Survey Replication Adolescent Supplement (NCSA) Psychological Medicine. 2012;42:1997–2010. doi: 10.1017/S0033291712000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM–IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Kishton JM, Wadaman KF. Unidimensional versus domain representative parceling of questionnaire items: An empirical example. Educational and Psychological Measurement. 1994;54:757–765. doi: 10.1177/0013164494054003022. [DOI] [Google Scholar]
- Kovacs M. Children’s Depression Inventory manual. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and clarifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. Psychosocial risk factors for depression. Journal of Abnormal Psychology. 1994;103:302–315. doi: 10.1037/0021-843X.103.2.302. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Adolescent psychopathology: III. The clinical consequences of comorbidity. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:510–519. doi: 10.1097/00004583-199504000-00018. [DOI] [PubMed] [Google Scholar]
- Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: Examining the question, weighing the evidence. Structural Equation Modeling. 2002;9:151–173. doi: 10.1207/S15328007SEM0902_1. [DOI] [Google Scholar]
- MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behavior Research Methods. 2007;39:384–389. doi: 10.3758/BF03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March JS, Parker JDA, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Hilt LM. Emotion dysregulation as a mechanism linking peer victimization to the development of internalizing symptoms among youth. Journal of Consulting and Clinical Psychology. 2009;77(894):904. doi: 10.1037/a0015760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Research and Therapy. 2011;49:186–193. doi: 10.1016/j.brat.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Nolen-Hoeksema S. Interpersonal stress generation as a mechanism linking rumination to internalizing symptoms in early adolescents. Journal of Clinical Child and Adolescent Psychology. 2012;41:584–597. doi: 10.1080/15374416.2012.704840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellings TMB, Alden LE. Cognitive processes in social anxiety: The effects of self-focus, rumination, and anticipatory processing. Behaviour Research and Therapy. 2000;38:243–257. doi: 10.1016/S0005-7967(99)00040-6. [DOI] [PubMed] [Google Scholar]
- Michl LC, McLaughlin KA, Shepherd K, Nolen-Hoeksema S. Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: Longitudinal evidence in early adolescents and adults. Journal of Abnormal Psychology. 2013;122:339–352. doi: 10.1037/a0031994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Ollendick T, King N, Bogie N. Three traditional and three new childhood anxiety questionnaires: Their reliability and validity in a normal adolescent sample. Behaviour Research and Therapy. 2002;40:753–772. doi: 10.1016/S0005-7967(01)00056-0. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus, Version 7.1. Los Angeles, CA: Author; 2012. [Google Scholar]
- Nolen-Hoeksema S. Sex differences in unipolar depression: Evidence and theory. Psychological Bulletin. 1987;101:259–282. doi: 10.1037/0033-2909.101.2.259. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Sex differences in depression. Stanford, CA: Stanford University Press; 1990. [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of the depressive episode. Journal of Abnormal Psychology. 1991;100:569–582. doi: 10.1037/0021-843X.100.4.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology. 2000;109:504–511. doi: 10.1037/0021-843X.109.3.504. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological Bulletin. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS, Seligman MEP. Predictors and consequences of childhood depressive symptoms: A 5-year longitudinal study. Journal of Abnormal Psychology. 1992;101:405–422. doi: 10.1037/0021-843X.101.3.405. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Harrell ZA. Rumination, depression, and alcohol use: Tests of gender differences. Journal of Cognitive Psychotherapy. 2002;16:391–403. [Google Scholar]
- Nolen-Hoeksema S, Hilt LM. Gender differences in depression. In: Hammen C, Gotlib I, editors. Handbook of depression. New York, NY: Guilford Press; 2009. pp. 386–404. [Google Scholar]
- Nolen-Hoeksema S, Larson J, Grayson C. Explaining the gender difference in depressive symptoms. Journal of Personality and Social Psychology. 1999;77:1061–1072. doi: 10.1037/0022-3514.77.5.1061. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology. 1991;61:115–121. doi: 10.1037/0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J, Fredrickson BL. Response styles and the duration of episodes of depressed mood. Journal of Abnormal Psychology. 1993;102:20–28. doi: 10.1037/0021-843X.102.1.20. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Parker LE, Larson J. Ruminative coping with depressed mood following loss. Journal of Personality and Social Psychology. 1994;67:92–104. doi: 10.1037/0022-3514.67.1.92. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Stice E, Wade E, Bohon C. Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. Journal of Abnormal Psychology. 2007;116:198–207. doi: 10.1037/0021-843X.116.1.198. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Watkins ER. A heuristic for developing transdiagnostic models of psychopathology explaining multifinality and divergent trajectories. Perspectives on Psychological Science. 2011;6:589–609. doi: 10.1177/1745691611419672. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Offord DR, Boyle MH, Racine YA, Fleming JE, Cadman DT, Blum HM, Woodward CA. Outcome, prognosis, and risk in a longitudinal follow-up study. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:916–923. doi: 10.1097/00004583-199209000-00021. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Boergers J, Vernberg EM. Overt and relational aggression in adolescents: Social-psychological adjustment of aggressors and victims. Journal of Clinical Child Psychology. 2001;30:479–491. doi: 10.1207/S15374424JCCP3004_05. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. Assessment of depression in children and adolescents by self-report measures. In: Reynolds WM, Johnston HF, editors. Handbook of depression in children and adolescents. New York, NY: Plenum Press; 1994. pp. 209–234. [DOI] [Google Scholar]
- Roberts JE, Gilboa E, Gotlib IH. Ruminative response style and vulnerability to episodes of dysphoria: Gender, neuroticism, and episode duration. Cognitive Therapy and Research. 1998;22:401–423. doi: 10.1023/A:1018713313894. [DOI] [Google Scholar]
- Robinson MS, Alloy LB. Negative cognitive styles and stress-reactive rumination interact to predict depression: A prospective study. Cognitive Therapy and Research. 2003;27:275–292. doi: 10.1023/A:1023914416469. [DOI] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comorbidity of unipolar depression: I. Comorbidity with other mental disorders in adolescents and adults. Journal of Abnormal Psychology. 1991;100:214–222. doi: 10.1037/0021-843X.100.2.214. [DOI] [PubMed] [Google Scholar]
- Rood L, Roelofs J, Bogels SM, Nolen-Hoeksema S, Schouten E. The influence of emotion-focused rumination and distraction on depressive symptoms in non-clinical youth: A meta-analytic review. Clinical Psychology Review. 2009;29:607–616. doi: 10.1016/j.cpr.2009.07.001. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. doi: 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27:247–259. doi: 10.1023/A:1023910315561. [DOI] [Google Scholar]
- Vasquez EA, Pedersen WC, Bushman BJ, Kelley NJ, Demeestere P, Miller N. Lashing out after stewing over public insults: The effects of public provocation, provocation intensity, and rumination on triggered displaced aggression. Aggressive Behavior. 2013;39:13–29. doi: 10.1002/ab.21453. [DOI] [PubMed] [Google Scholar]
- Verstraeten K, Bijttebier P, Vasey MW, Raes F. Specificity of worry and rumination in the development of anxiety and depressive symptoms in children. British Journal of Clinical Psychology. 2011;50:364–378. doi: 10.1348/014466510X532715. [DOI] [PubMed] [Google Scholar]
- Watkins ER. Depressive rumination and co-morbidity: Evidence for brooding as a transdiagnostic process. Journal of Rational-Emotive and Cognitive-Behavior Therapy. 2009;27:160–175. doi: 10.1007/s10942-009-0098-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D. Differentiating the mood and anxiety disorders: A quadripartite model. Annual Review of Clinical Psychology. 2009;5:221–247. doi: 10.1146/annurev.clinpsy.032408.153510. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


