Abstract
This article has been selected for the Anesthesiology CME Program. Learning objectives and disclosure and ordering information can be found in the CME section at the front of this issue.
PREVENTION, detection, and therapy of myocardial infarction have been fundamental goals of perioperative medicine for many years. As one of the first monitors dedicated to detecting myocardial ischemia, continuous electrocardiography for patients undergoing surgery became more commonly used in the 1950s. Indeed, by 1978, guidelines recommended routine baseline electrocardiogram testing for all adult patients before undergoing surgery.1 However, given that preoperative electrocardiographic abnormalities are not necessarily predicative of postoperative myocardial infarction,2 current practice advisories recognize that preoperative testing should rather be considered for patients with cardiovascular risk factors.3 Intraoperative echocardiography is routinely used for diagnosis and therapy in cardiac surgery.4,5 In addition, it can also be used safely in noncardiac surgery for the detection of new regional wall motion abnormalities indicative of myocardial ischemia.6,7 However, given the resources required for a complete diagnostic echocardiographic examination, its use as a screening tool for myocardial injury in noncardiac surgery is likely limited. A common test used for the diagnosis of perioperative myocardial injury is the measurement of plasma troponin levels. In the past, minor increases in serum troponin levels have often clinically been dismissed as less relevant cases of supply/demand mismatch. This is likely related to the fact that a troponin increase itself does not meet definition criteria for myocardial infarction and a lack of consensus on the most appropriate therapeutic approach. Although it seems intuitive that myocardial infarction leading to cell death is of greater consequence than myocardial ischemia without necrosis, the relevance of minor myocardial injury is not well defined. Furthermore, the progression from reversible ischemic damage to necrosis occurs on a biologic continuum, making cutoffs based on the presumed degree of cellular injury impractical at best. Defining clinical relevance of biomarkers such as Troponin T (TnT) according to their association with meaningful outcomes, such as 30-day mortality, adds substantial value for the practicing clinician. The significance of creatine muscle and brain isoenzyme and TnT to predict mortality and major cardiovascular events has previously been highlighted in a meta-analysis.8 The current study by the VISION Writing Group9 underlines the fundamental importance of even subtle perioperative TnT increases for morbidity and mortality in surgical patients. The current findings are a post hoc analysis of prospectively collected data from The Vascular events In noncardiac Surgery patIents cOhort evaluatioN trial.10 The reported analyses extend the interpretation of the The Vascular events In noncardiac Surgery patIents cOhort evaluatioN study, as they confirm the independent association of a TnT value of 0.03 ng/ml or greater with all-cause 30-day mortality after adjusting for preoperative risk factors and perioperative events.
Image: Silvia Martín-Puig (immunofluorescent monoclonal antibody staining of cardiac Troponin T in human fetal cardiomyocytes). Used with permission.
“The current study … underlines the fundamental importance of even subtle perioperative TnT increases for morbidity and mortality in surgical patients.”
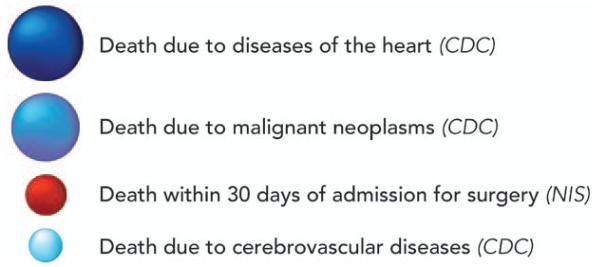
In a diverse cohort comprising 15,065 patients with age 45 years or older undergoing noncardiac surgery requiring at least overnight hospitalization, the authors observed a 30-day mortality rate of 1.7%. This is consistent with previously reported death rates within 30 days of surgery. In fact, the magnitude of all-cause perioperative mortality would make it the number three cause of death in the United States (fig. 1).11 The current study suggests that this staggeringly high rate of death after surgery is in many circumstances preceded by often subclinical myocardial injury.9 The authors used regression analysis to validate a cutoff value for TnT of 0.03 ng/ml or greater to define myocardial injury after noncardiac surgery. Moreover, they discovered that of the 8% of patients who developed myocardial injury after noncardiac surgery, 58.2% would not have fulfilled the universal definition for myocardial infarction. By using data from the 8,351 patients included in the PeriOperative ISchemic Evaluation trial, Devereaux et al.12 previously reported a mortality rate of 11.6% in patients affected by perioperative myocardial infarction. Even when applying less rigorous criteria for myocardial injury such as a peak TnT value of 0.03 ng/ml, the current study found affected patients to be 4.3 times as likely to die within 30 days.9 Furthermore, 1 of 10 patients with myocardial injury after noncardiac surgery did not survive 30 days after surgery. The combination of the high incidence of myocardial injury after noncardiac surgery, its prognostic relevance for 30-day mortality, and the ease and feasibility of the test to detect it (using TnT) point to tremendous opportunities for design of clinical studies to test novel interventions to attenuate myocardial injury and perioperative mortality.
Fig. 1.
Magnitude of perioperative mortality. The three leading causes of death in the Center for Disease Control’s (CDC) annual death table for the United States in 2006 were: (1) diseases of heart (n = 631,636), (2) malignant neoplasms (n = 559,888), and (3) cerebrovascular diseases (n = 137,119). By using the Nationwide Inpatient Sample (NIS) for the same year, Semel et al.13 reported 189,690 deaths within 30 days of admission for inpatients having a surgical procedure. In magnitude, all-cause 30-day inpatient mortality after surgery approximated the third leading cause of death in the United States. Figure adapted with permission from Lippincott Williams and Wilkins/Wolters Kluwer Health. Bartels K, Karhausen J, Clambey ET, Grenz A, Eltzschig HK: Perioperative organ injury. Anesthesiology 2013, copyright 2013.11
Although the need for new cardio-protective therapies has been convincingly demonstrated, causality of myocardial injury and mortality has not. Perioperative ischemia and inflammation are likely to lead to injury in other organs too. Similar to low-level myocardial injury, hypoxia-sensitive tissues such as kidney are also prone to ischemic damage. Although preoperative estimated glomerular filtration rate was not associated with mortality in the current study, it seems conceivable that more sensitive markers of renal injury, such as insulin-like growth factor-binding protein 7 or tissue inhibitor of metalloproteinases-2, could have shown a comparable response pattern to TnT. Hence, the observed mortality could have been due to multiorgan injury rather than isolated myocardial injury. Therefore, interventional clinical trials focused solely on prevention of myocardial infarction might not be successful. Clearly, the development of innovative, mechanism-based approaches to prevent or treat perioperative organ injury, including myocardial injury, is paramount. These will then need to be tested in rigorous clinical trials to translate the results of this study into improved patient outcomes.
Acknowledgments
This work was supported by National Institutes of Health (Bethesda, Maryland) grants R01-DK097075, R01-HL0921, R01-DK083385, R01-HL098294, POIHL114457-01, and a grant by the Crohn’s and Colitis Foundation of America (CCFA, New York, New York; to H.K.E.).
Footnotes
Competing Interests
The authors are not supported by, nor maintain any financial interest in, any commercial activity that may be associated with the topic of this article.
References
- 1.Resnekov L, Fox S, Selzer A, Campbell R, Childers R, Kaplan S, Lindsay A, McHenry P, Schlant R, Sylvester R. The quest for optimal electrocardiography. Task Force IV: Use of electrocardiograms in practice. Am J Cardiol. 1978;41:170–5. doi: 10.1016/0002-9149(78)90151-0. [DOI] [PubMed] [Google Scholar]
- 2.van Klei WA, Bryson GL, Yang H, Kalkman CJ, Wells GA, Beattie WS. The value of routine preoperative electrocardiography in predicting myocardial infarction after noncardiac surgery. Ann Surg. 2007;246:165–70. doi: 10.1097/01.sla.0000261737.62514.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Apfelbaum JL, Connis RT, Nickinovich DG, Pasternak LR, Arens JF, Caplan RA, Connis RT, Fleisher LA, Flowerdew R, Gold BS, Mayhew JF, Nickinovich DG, Rice LJ, Roizen MF, Twersky RS. Practice advisory for preanesthesia evaluation: An updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2012;116:522–38. doi: 10.1097/ALN.0b013e31823c1067. [DOI] [PubMed] [Google Scholar]
- 4.Eltzschig HK, Rosenberger P, Löffler M, Fox JA, Aranki SF, Shernan SK. Impact of intraoperative transesophageal echocardiography on surgical decisions in 12,566 patients undergoing cardiac surgery. Ann Thorac Surg. 2008;85:845–52. doi: 10.1016/j.athoracsur.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberger P, Shernan SK, Löffler M, Shekar PS, Fox JA, Tuli JK, Nowak M, Eltzschig HK. The influence of epiaortic ultrasonography on intraoperative surgical management in 6051 cardiac surgical patients. Ann Thorac Surg. 2008;85:548–53. doi: 10.1016/j.athoracsur.2007.08.061. [DOI] [PubMed] [Google Scholar]
- 6.Hilberath JN, Oakes DA, Shernan SK, Bulwer BE, D’Ambra MN, Eltzschig HK. Safety of transesophageal echocardiography. J Am Soc Echocardiogr. 2010;23:1115–27. doi: 10.1016/j.echo.2010.08.013. quiz 1220-1. [DOI] [PubMed] [Google Scholar]
- 7.Memtsoudis SG, Rosenberger P, Loffler M, Eltzschig HK, Mizuguchi A, Shernan SK, Fox JA. The usefulness of transesophageal echocardiography during intraoperative cardiac arrest in noncardiac surgery. Anesth Analg. 2006;102:1653–7. doi: 10.1213/01.ane.0000216412.83790.29. [DOI] [PubMed] [Google Scholar]
- 8.Levy M, Heels-Ansdell D, Hiralal R, Bhandari M, Guyatt G, yusuf S, Cook D, Villar JC, McQueen M, McFalls E, Filipovic M, Schünemann H, Sear J, Foex P, Lim W, Landesberg G, Godet G, Poldermans D, Bursi F, Kertai MD, Bhatnagar N, Devereaux PJ. Prognostic value of troponin and creatine kinase muscle and brain isoenzyme measurement after noncardiac surgery: A systematic review and meta-analysis. Anesthesiology. 2011;114:796–6. doi: 10.1097/ALN.0b013e31820ad503. [DOI] [PubMed] [Google Scholar]
- 9.VISION Writing Group. VISION investigators Myocardial injury after noncardiac surgery: A large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology. 2014;120:564–78. doi: 10.1097/ALN.0000000000000113. [DOI] [PubMed] [Google Scholar]
- 10.Vascular Events in Noncardiac Surgery Patients Cohort Evaluation Study I. Devereaux PJ, Chan MT, Alonso-Coello P, Walsh M, Berwanger O, Villar JC, Wang CY, Garutti RI, Jacka MJ, Sigamani A, Srinathan S, Biccard BM, Chow CK, Abraham V, Tiboni M, Pettit S, Szczeklik W, Lurati Buse G, Botto F, Guyatt G, Heels-Ansdell D, Sessler DI, Thorlund K, Garg AX, Mrkobrada M, Thomas S, Rodseth RN, Pearse RM, Thabane L, McQueen MJ, Vanhelder T, Bhandari M, Bosch J, Kurz A, Polanczyk C, Malaga G, Nagele P, Le Manach Y, Leuwer M, Yusuf S. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2012;307:2295–304. doi: 10.1001/jama.2012.5502. [DOI] [PubMed] [Google Scholar]
- 11.Bartels K, Karhausen J, Clambey ET, Grenz A, Eltzschig HK. Perioperative organ injury. Anesthesiology. 2013;119:1474–89. doi: 10.1097/ALN.0000000000000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Devereaux PJ, Xavier D, Pogue J, Guyatt G, Sigamani A, Garutti I, Leslie K, Rao-Melacini P, Chrolavicius S, Yang H, Macdonald C, Avezum A, Lanthier L, Hu W, Yusuf S. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: A cohort study. Ann intern Med. 2011;154:523–8. doi: 10.7326/0003-4819-154-8-201104190-00003. [DOI] [PubMed] [Google Scholar]
- 13.Semel ME, Lipsitz SR, Funk LM, Bader AM, Weiser TG, Gawande AA. Rates and patterns of death after surgery in the United States, 1996 and 2006. Surgery. 2012;151:171–82. doi: 10.1016/j.surg.2011.07.021. [DOI] [PubMed] [Google Scholar]