To the Editor
The US Food and Drug Administration first approved intra-articular hyaluronic acid injections (also known as “viscosupplementation”) for use in patients with severe knee osteoarthritis in 1997. The effectiveness of these injections, however, has recently been called into question. In 2013, the American Academy of Orthopedic Surgeons issued a clinical practice guideline that stated: “We cannot recommend using hyaluronic acid for patients with symptomatic [osteoarthritis] of the knee,” with a “strong” rating.1 The rating was based on high-quality evidence that hyaluronic acid injections were not associated with clinically meaningful improvement in symptoms, as compared to placebo injections.1 A meta-analysis published in 2012 reported similar findings.2 Using recent Medicare Part B claims data, we examined patterns of use for intra-articular hyaluronic acid injections across the United States.
Methods
We analyzed 2012 Medicare Utilization and Payment data available for public use. The file contains all Part B claims for the Medicare fee-for-service population aggregated by provider, with certain exclusions.3 We tabulated administrations (“bene-days”) for all formulations of hyaluronic acid (Healthcare Common Procedure Coding System codes J7321, J7323, J7324, J7325, J7326) according to health referral region (HRR, large regionalized health care markets defined by patients’ travel for tertiary care).4 We calculated total payments by Medicare from reported payments to each provider for (1) hyaluronic acid products and (2) the Current Procedural Terminology (CPT) code for large joint injections (20610). All injections on the same day were counted as one injection.
Using data from the Dartmouth Atlas of Health Care, we divided the raw totals for the number of hyaluronic acid administrations by the total number of Medicare beneficiaries within each HRR.4 We used logistic regression to correlate the number of procedures performed in each HRR (per 1000 beneficiaries) with the number of physicians per capita.5 We applied previously described methods to assess clustering among high-use regions.6
Aggregated records derived from ≤10 beneficiaries were excluded from this public use file. The dataset also did not contain information on individual patients, including indications for treatment. The institutional review boards at our institutions exempted the study from review.
Results
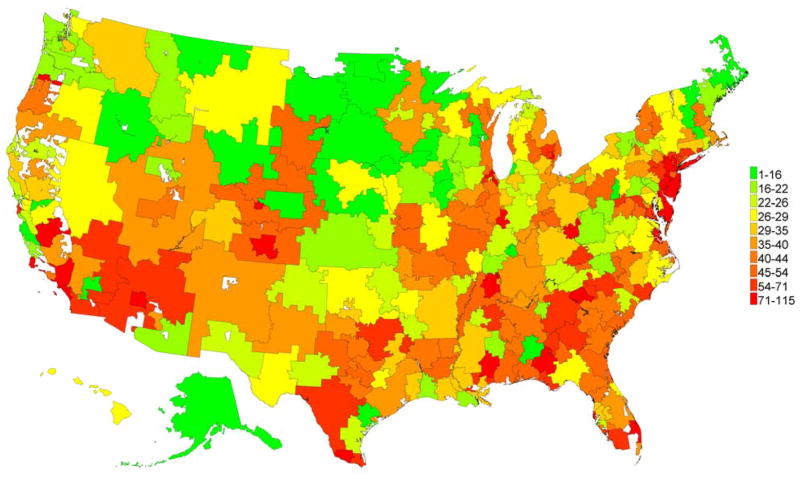
In 2012, Medicare Part B reimbursed for 1,161,924 administrations of intra-articular hyaluronic acid among 423,669 unique patients by 12,761 unique physicians or other clinicians. Most formulations of hyaluronic acid are administered as a course of 3 injections one week apart. Medicare paid $207 million for the hyaluronic acid product and $80 million for the associated large-joint injection CPT code. Thus, on average per administration, Medicare paid $179 for the drug and $69 for the injection. The clinicians most likely to provide administer intra-articular hyaluronic acid were orthopedic surgeons (59%), primary care physicians (11%, including family, general, and internal medicine, and geriatrics), physician assistants (10%), and rheumatologists (8%). An analysis by HRRs showed that rates of viscosupplementation varied from 1 to 115 administrations per 1000 Medicare beneficiaries (mean 39 per 1000 Medicare beneficiaries, coefficient of variation 0.56 (Figure)). These HRRs were clustered (p < 0.001). Higher rates of injection of intra-articular hyaluronic acid in a region were associated with higher numbers of physicians, surgeons, and rheumatologists (adjusted for population size) but were not correlated with the number of orthopedists (Table).
Figure. Injections of Intra-articular Hyaluronic Acid in 2012 per 1000 Medicare beneficiaries, by Health Referral Region.
Number of hyaluronic acid administrations derived from 2012 Medicare Payment and Utilization data, and total number of Medicare beneficiaries from the Dartmouth Atlas of Health Care.3,4
Table.
Association between Physician Supply and the Odds of Intra-articular Hyaluronic Acid Injections in a Health Referral Region
| Physician supply (per 100,000 residents) | Mean (SD) in HRR* | Median (IQR) in HRR* | Odds (95% CI) of being in top HRR decile of hyaluronic acid injections (per 1000 Medicare beneficiaries) |
|---|---|---|---|
| Total physicians | 193.1 (30.4) | ||
| Tertile 1 (low) | 166 (156 – 174) | Referent | |
| Tertile 2 | 188 (183 – 194) | 1.0 (0.3, 3.2) | |
| Tertile 3 (high) | 218 (210 – 236) | 3.4 (1.3, 8.9) | |
| Total surgeons | 41.2. (6.4) | ||
| Tertile 1 (low) | 36 (33 – 37) | Referent | |
| Tertile 2 | 41 (40 – 41) | 1.0 (0.3, 3.2) | |
| Tertile 3 (high) | 47 (44 – 50) | 3.4 (1.3, 8.9) | |
| Primary care physicians | 70.4 (12.0) | ||
| Tertile 1 (low) | 59 (55 – 62) | Referent | |
| Tertile 2 | 69 (67 – 71) | 1.9 (0.7, 5.4) | |
| Tertile 3 (high) | 82 (78 – 88) | 2.3 (0.8, 6.3) | |
| Orthopedic surgeons | 6.5 (1.3) | ||
| Tertile 1 (low) | 5 (4 – 6) | Referent | |
| Tertile 2 | 6 (6 – 7) | 0.8 (0.3, 2.0) | |
| Tertile 3 (high) | 8 (7 – 8) | 1.2 (0.5, 3.0) | |
| Rheumatologists | 1.1 (0.4) | ||
| Tertile 1 (low) | 0.7 (0.6 – 0.8) | Referent | |
| Tertile 2 | 1.0 (0.9 – 1.1) | 1.9 (0.6, 5.8) | |
| Tertile 3 (high) | 1.4 (1.3 – 1.7) | 3.6 (1.2, 10.1) |
Data calculated from Dartmouth Atlas of Health Care, selected hospital and physician capacity measures data, 20065
HRR: Health referral region
IQR: interquartile range
Discussion
In the United States in 2012, we found that intra-articular hyaluronic acid was administered frequently to Medicare beneficiaries despite strong evidence that this therapy is of low value for its approved indication of severe knee osteoarthritis. The injections are costly, and have limited clinical benefit. We also found that the frequency of use varied widely, and was correlated with the number of physicians, but not the number of orthopedic surgeons in a region. Among the limitations of our study are that we could not determine the indications for treatment, such as the percentage of injections to patients with severe knee osteoarthritis. We also could not determine if any patients developed infections, or other complications.
Based on recent guidelines and studies, intra-articular hyaluronic acid injections represent low-value care and an inefficient use of healthcare resources.2,3 Medicare beneficiaries and society would be better served if physicians and others involved in paying for and delivering healthcare worked together to minimize the use of such low-value care.
Acknowledgments
Support: This publication was supported by K23 AR063770 (GS) and K23 AR060259 (JY).
Footnotes
Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
The authors report no conflicts of interest to disclose.
References
- 1. [Accessed on April 16, 2014]; at http://www.aaos.org/news/aaosnow/jun13/cover1_t1.pdf.
- 2.Rutjes AW, Jüni P, da Costa BR, Trelle S, Nüesch E, Reichenbach S. Viscosupplementation for osteoarthritis of the knee: a systematic review and meta-analysis. Ann Intern Med. 2012;157(3):180–91. doi: 10.7326/0003-4819-157-3-201208070-00473. [DOI] [PubMed] [Google Scholar]
- 3.http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Downloads/Medicare-Physician-and-Other-Supplier-PUF-Methodology.pdf
- 4. [accessed on April 16, 2014];“ZIP code to HSA to HRR crosswalk, 2012” and “Selected measures of primary care access and quality, 2010”. at http://www.dartmouthatlas.org/tools/downloads.aspx?tab=39.
- 5. [accessed on April 16, 2014];Selected hospital and physician capacity measures data. 2006 at http://www.dartmouthatlas.org/tools/downloads.aspx?tab=35.
- 6.Zhang Y, Baik SH, Fendrick AM, Baicker K. Comparing local and regional variation in health care spending. N Engl J Med. 2012;367(18):1724–31. doi: 10.1056/NEJMsa1203980. [DOI] [PMC free article] [PubMed] [Google Scholar]