Abstract
Goals:
We designed this study to evaluate the efficacy of spleen salvage during distal pancreatectomy for patients with benign and borderline malignant tumors.
Background:
Despite the emphasis on its role, the spleen has commonly been removed in distal pancreatectomy.
Study:
From January 2005 to July 2009, 82 patients underwent distal pancreatectomy with splenectomy (DPS) and 78 patients underwent spleen-preserving distal pancreatectomy (SPDP). Medical records were retrospectively reviewed.
Results:
There were no significant differences in demographics, final diagnoses, estimated blood loss, intraoperative transfusion, and operative time between the 2 groups. More perioperative complications occurred in the DPS group than in the SPDP group (P=0.0344). Consequently, postoperative hospital stay was significantly shorter in the SPDP group than in the DPS group (P=0.0273). In the follow-up survey, episodes of common cold or flu were apparently more frequent in the DPS group (P=0.047). More patients in the DPS group felt fatigue (P=0.0481) and poor health condition (P=0.0371). Less newly developed (P=0.0193) and aggravated diabetes mellitus (P=0.0361) were also observed in the SPDP group. Platelet counts on postoperative day (POD) 5, hemoglobin on POD 3, WBC counts, and CRP level on POD 2 were significantly higher in the DPS group than in the SPDP group and these differences continued to be significant for months after surgery.
Conclusions:
In addition to frequent higher grade complications, prolonged hospital stays, and severe hematological abnormalities, DPS seemed to result in poor health condition based on the follow-up survey. Even an effort to preserve an adult spleen in distal pancreatectomy is worthwhile.
Key Words: spleen-preserving distal pancreatectomy, distal pancreatectomy, pancreatectomy
Distal pancreatectomy for benign or malignant disease in the body or tail of the pancreas has traditionally involved splenectomy as an integral part of the procedure simply because of its anatomic proximity to the distal pancreas and for the sake of technical simplicity. However, splenectomized patients are at a potential risk for infection because the spleen is known to be the largest aggregation of the lymphoid tissue in the body. Recently reported studies, confirming such detrimental splenectomy sequelae as a increased lifetime risk for developing overwhelming postsplenectomy infection (OPSI) any time after removal of the spleen,1 compromised antitumor immunity,2 and a higher risk for diabetes mellitus3 have awakened interest in spleen-preserving surgery for benign lesions or tumors with low-grade malignant potential of the body and tail of the pancreas. In contrast, some authors suggest that splenic preservation is more difficult, time consuming, and is associated with increased blood loss from small venous tributaries.4
In this study, we compared the perioperative and postoperative long-term follow-up results of spleen-preserving distal pancreatectomy (SPDP) with distal pancreatectomy with splenectomy (DPS). In doing so, we tried to find practical reasons for preserving the spleen in distal pancreatectomy for benign lesions or tumors with low-grade malignant potential of the body and tail of the pancreas.
MATERIALS AND METHODS
From January 2005 to July 2009, 82 patients underwent DPS and 78 patients underwent SPDP for benign or low-grade malignant disease at First People’s Hospital affiliated to Huzhou University Medical College, Huzhou, Zhejiang Province, China. Spleen preservation was achieved in which the pancreas was dissected off the splenic vessels. The medical records were reviewed to evaluate the clinical outcomes such as surgical factors (operation time, estimated blood loss, transfusion), perioperative complications, postoperative hematological changes, and postoperative long-term outcomes (endocrine/exocrine function, health condition, and recurrence). Written informed consent was obtained from all patients. Approval of the study was obtained from the Institutional Review Board.
DPS was performed in a standard manner. Division of the pancreatic parenchyma was carried out by electrocautery and mass. Direct ligation of the main pancreatic duct was done with nonabsorbable suture. The pancreatic stump is oversewn, and the omentum mobilized and sutured to the pancreatic stump. An external close suction drain is placed near the pancreatic cut surface. In SPDP, both the splenic artery and vein were preserved. An external close suction drain was positioned in the splenic fossa close to the transected pancreas. Postoperative octreotide was administered subcutaneously (dose 100 mg every 8 h) for 2 weeks in both groups. A pancreatic fistula was defined according to the guidelines of the International Study Group on Pancreatic Fistulas.5 Postoperative bleeding was defined as proposed by the International Study Group on Pancreatic Surgery.6 Three different grades of postpancreatectomy hemorrhage (grades A, B, and C) were defined according to the time of onset, site of bleeding, severity, and clinical impact. Infectious complications were determined by microbiological culture study. Mortality was defined as death within 30 days postoperatively, in or out of the hospital.
Patients were assessed every month during the first postoperative year, and then every 3 months in the next few years after surgery. The baseline assessment involved a medical history taking, life quality assessment, physical examination, hematological tests, chest radiography, and abdominal ultrasonography or computed tomography. The diagnosis of recurrence was made on the basis of imaging and, if necessary, cytologic analysis or biopsy.
Continuous variables are expressed as mean±SD, and categorical variables are shown as frequency (percentage). Statistical differences were evaluated by the χ2 test, the Student t test, and the paired t test. A P-value <0.05 was regarded as statistically significant.
RESULTS
Patient Characteristics
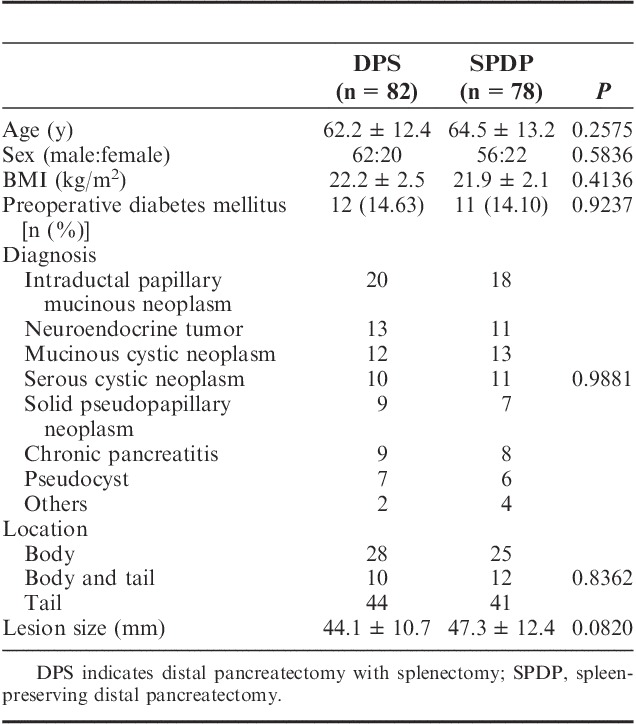
Clinical features of patients and indications for DPS or SPDP are shown in Table 1. There were no significant differences in age, sex, preoperative diabetes mellitus, preoperative WBC count, platelet count, body mass index, tumor location, lesion size, and final diagnoses. SPDP was successfully performed in all 78 patients. Conservation of the splenic artery and vein during SPDP was possible in all patients.
TABLE 1.
Patient Characteristics
Perioperative Details and Complications
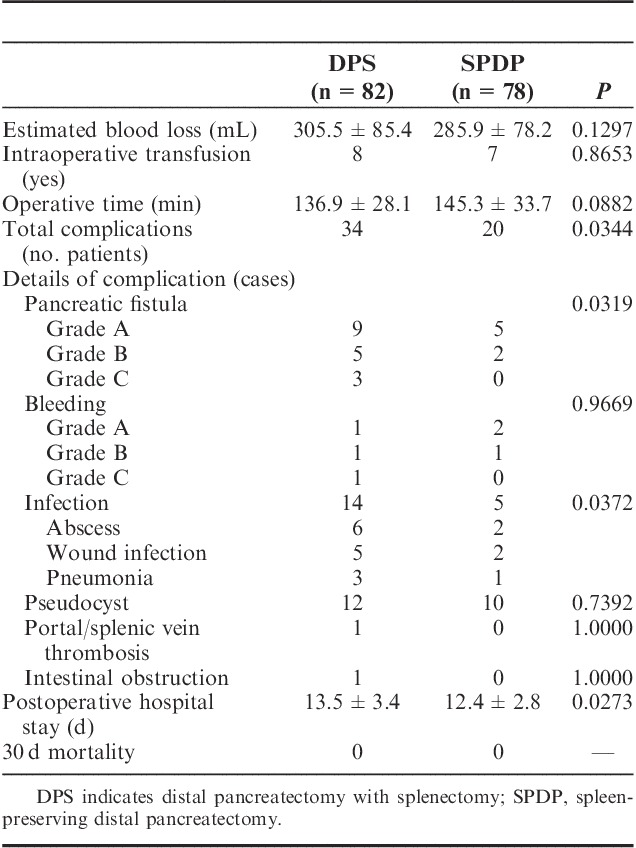
Perioperative details and complications are shown in Table 2. There were no significant differences in estimated blood loss, intraoperative transfusion, and operative time between the 2 groups. There was no postoperative 30-day mortality. However, more perioperative complications occurred in the DPS group than in the SPDP group (34/82 vs. 20/78, P=0.0344). Consequently, postoperative hospital stay was significantly shorter in the SPDP group than in the DPS group (13.5±3.4 vs. 12.4±2.8 d, P=0.0273). Patients in the DPS group had more postoperative pancreatic fistulas of a higher grade (P=0.0319). Furthermore, more frequent and various infectious complications occurred in the DPS group, including intra-abdominal abscess, wound infection, and pneumonia (P=0.0372).
TABLE 2.
Perioperative Details and Complications
Hematological Changes
WBC counts on postoperative day (POD) 2 (Fig. 1) were significantly higher in the DPS group than in the SPDP group (14.2±3.3 vs. 10.2±2.8, P=0.0000), and this difference continued until postoperative month (POM) 1.
FIGURE 1.
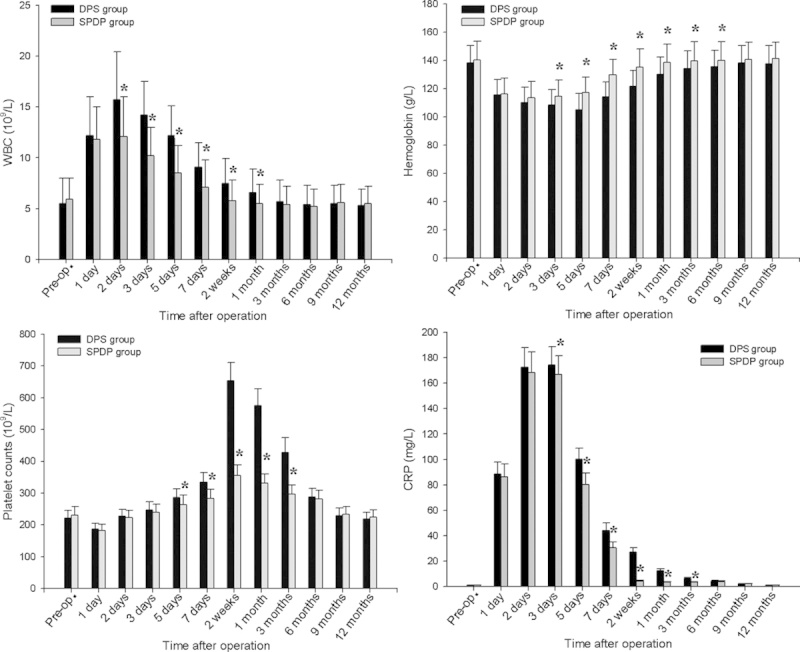
Postoperative hematological changes in the SPDP and DPS groups. Data are expressed as mean±SD. *P<0.05. DPS indicates distal pancreatectomy with splenectomy; SPDP, spleen-preserving distal pancreatectomy.
Serum hemoglobin level (Fig. 1) in the SPDP and DPS groups remained low from POD 1 to POD 5, and then started to increase thereafter. Serum hemoglobin on POD 3 was significantly higher in the SPDP group than in the DPS group (114.7±11.4 vs. 108.4±10.4, P=0.0004), and this difference continued until POM 6.
Platelet counts (Fig. 1) in both groups were significantly decreased compared with the preoperative levels on POD 1 to 2, increased to the maximum levels at 2 weeks after surgery, and decreased thereafter. Platelet counts on POD 5 were significantly higher in the DPS group than in the SPDP group (285.7±28.4 vs. 264.4±29.2, P=0.000), and this difference continued until POM 3.
Serum CRP levels (Fig. 1) increased from POD 1 to POD 3, and decreased thereafter. Serum CRP levels on POD 2 were significantly higher in the DPS group than in the SPDP group (174.5±14.2 vs. 166.7±14.7, P=0.0008), and this difference continued until POM 3. Serum albumin levels did not differ significantly between the 2 groups at any postoperative time point.
Long-Term Outcome
Long-term follow-up outcomes are shown in Table 3. A total of 160 patients [follow-up rate 100%, median follow-up period 42 (range, 24 to 76) months] were contacted by telephone and all of them agreed to respond to the follow-up survey. Visits to the doctor because of infection were rare in both groups. However, it was noteworthy that episodes of common cold or flu were apparently more frequent in the DPS group (P=0.047); there were 13 patients who had caught a cold >5 times a year, as compared with only 5 patients in the SPDP group. There were significantly more patients in the DPS group who felt fatigue (P=0.0481) and poor health condition (P=0.0371).
TABLE 3.
Long-Term Outcomes
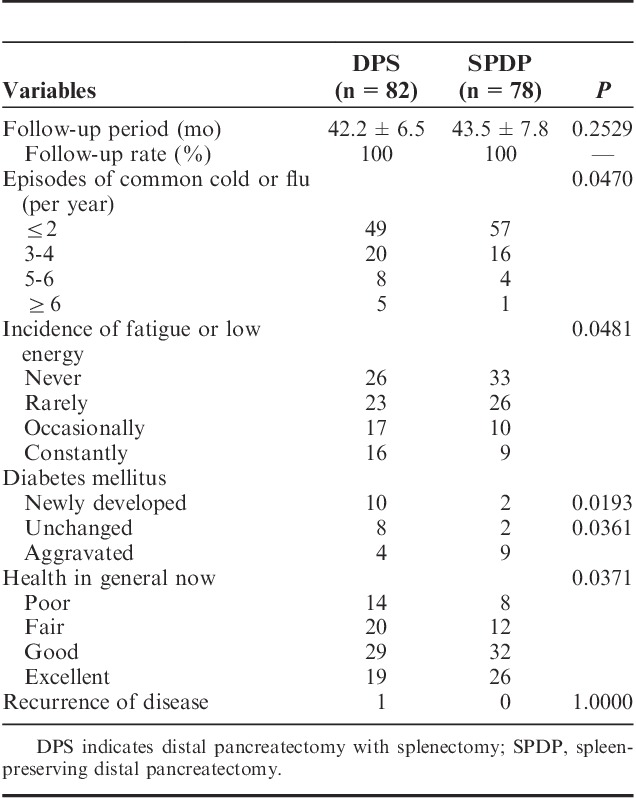
Regarding endocrine function, 10 and 2 patients had newly developed diabetes mellitus in the DPS group and SPDP group (P=0.0193) among the patients with preoperative normoglycemia, respectively. Diabetes aggravated more frequently in the DPS group than in the SPDP group (P=0.0361). Recurrence occurred in 1 patient 5 years after undergoing DPS because of intraductal papillary mucinous neoplasm. Total pancreatectomy was performed and the permanent pathologic report showed intraductal papillary mucinous carcinoma.
DISCUSSION
Splenectomy involved in other major abdominal organ resection was found to be responsible for increased postoperative morbidity, especially infectious complications. White et al7 demonstrated that distal pancreatectomy with spleen preservation reduced perioperative infectious complications, severe complications, and length of hospital stay, suggesting the value of spleen preservation in distal pancreatectomy. In addition, OPSI and increasing concern for the potential risk of malignancy after splenectomy have raised the necessity of spleen preservation.8 As the role of the spleen has gradually become recognized over the past several decades, many surgeons now try to preserve the spleen whenever performing distal pancreatectomy in benign or borderline malignant tumors of the distal pancreas. However, despite the theoretical background of the spleen’s role, clinical adverse events related to splenectomy seem to be very rare. Some surgeons may not agree with the value of the spleen in adult patients. In addition, considering the technical demands of SPDP as compared with conventional DPS, some may argue against the efforts to preserve the adult spleen when performing distal pancreatectomy.4 However, according to our present results, there were no significant differences in estimated blood loss, intraoperative transfusion, operative time, and postoperative 30-day mortality between patients who underwent SDPD and DPS. In addition, SPDP was demonstrated to yield better perioperative outcomes, with shorter hospital stays, lower grade complications, lower incidence of pancreatic fistula, and, most importantly, lower incidence of infection-related complications than DPS. Even these perioperative results suggest that it is best to conserve the spleen whenever possible.
The most frequent time interval between splenectomy and OPSI was 10 to 19 years, and their overall mortality reached approximately 50%. This finding is very important to patients with a high chance of long-term survival, such as the current patient group.9 The frequency of common cold or flu in the DPS group may indirectly suggest a lifetime chance of developing OPSI. According to our results, patients who undergo DPS are thought to be vulnerable to respiratory tract infection and can develop critical infectious complications such as OPSI.
Several studies have compared the early perioperative hematological outcomes of SPDP and DPS.10,11 However, serial measurements of hematological parameters have not been carried out. Therefore, in the present study, we continuously investigated the platelet and WBC counts, hemoglobin level as an index of anemia, serum albumin as an index of nutrition, and serum CRP as an index of inflammation in both groups. In this study, the WBC count differed significantly from POD 1 until POM 1. The increases in WBC count early after DPS did not reflect the surgical stress level, but may have been a physiological reaction to splenectomy.12 The clinical significance of an elevated WBC count early after splenectomy is unclear, but it may be a risk factor for myocardial infarction.13 A significantly higher platelet count was observed from 5 days through 3 months after DPS than after SPDP. The significant increase in the platelet count after DPS may have been because of loss of the spleen, which serves as a site of platelet sequestration. It is reported that thrombocytosis after splenectomy, injury, and coronary bypass increases the risk for thromboembolic complications.14 Hemoglobin level decreased early after operation, and then started to recover after POD 5. Recovery of the hemoglobin level was significantly greater in the SPDP group than in the DPS group. This difference may have been because of the preservation of the spleen, which is a site of iron storage and splenic macrophages are able to efficiently reuse iron.15 The CRP levels were significantly higher in the DPS group than in the SPDP group from POD 3 until POM 3, possibly because of prolonged mild inflammation.16
Additional advantages of spleen preservation were observed in the long-term follow-up study, with better results in terms of fatigue and general condition. Less newly developed and aggravated diabetes mellitus were also observed in the SPDP group. These problems, however, could act as factors that influence the quality of life; thus, care must be taken during the follow-up period.
In summary, distal pancreatectomy with or without splenectomy can be performed safely; however, in this study, more frequent severe complications, prolonged hospital stays, and severe hematological abnormalities were noted in the DPS group. In addition, this long-term follow-up study indirectly suggested vulnerability to respiratory infection and impaired quality of life after DPS. Therefore, surgeons are advised to apply a spleen-preserving policy when performing distal pancreatectomy, even in adult patients. This extra effort and responsibility on the part of the surgeon would have invaluable benefits for the patients.
Footnotes
The authors declare that they have nothing to disclose.
REFERENCES
- 1.Hansen K, Singer DB.Asplenic-hyposplenic overwhelming sepsis: postsplenectomy sepsis revisited.Pediatr Dev Pathol. 2001;4:105–121. [DOI] [PubMed] [Google Scholar]
- 2.Sasson AR, Hoffman JP, Ross EA, et al. En bloc resection for locally advanced cancer of the pancreas: is it worthwhile?J Gastrointest Surg. 2002;6:147–157discussion 57-58. [DOI] [PubMed] [Google Scholar]
- 3.Hutchins RR, Hart RS, Pacifico M, et al. Long-term results of distal pancreatectomy for chronic pancreatitis in 90 patients.Ann Surg. 2002;236:612–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shoup M, Brennan MF, McWhite K, et al. The value of splenic preservation with distal pancreatectomy.Arch Surg. 2002;137:164–168. [DOI] [PubMed] [Google Scholar]
- 5.Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition.Surgery. 2005;138:8–13. [DOI] [PubMed] [Google Scholar]
- 6.Wente MN, Veit JA, Bassi C, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition.Surgery. 2007;142:20–25. [DOI] [PubMed] [Google Scholar]
- 7.White SA, Sutton CD, Berry DP, et al. Value of splenic preservation during distal pancreatectomy for chronic pancreatitis.Br J Surg. 2000;87:124. [DOI] [PubMed] [Google Scholar]
- 8.Jones P, Leder K, Woolley I, et al. Postsplenectomy infection - strategies for prevention in general practice.Aust Fam Physician. 2010;39:383–386. [PubMed] [Google Scholar]
- 9.Waghorn DJ.Overwhelming infection in asplenic patients: current best practice preventive measures are not being followed.J Clin Pathol. 2001;54:214–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee SE, Jang JY, Lee KU, et al. Clinical comparison of distal pancreatectomy with or without splenectomy.J Korean Med Sci. 2008;23:1011–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kimura W, Yano M, Sugawara S, et al. Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein: techniques and its significance.J Hepatobiliary Pancreat Sci. 2010;17:813–823. [DOI] [PubMed] [Google Scholar]
- 12.Djaldetti M, Bergman M, Salman H, et al. On the mechanism of post-splenectomy leukocytosis in mice.Eur J Clin Invest. 2003;33:811–817. [DOI] [PubMed] [Google Scholar]
- 13.Cerletti C, de Gaetano G, Lorenzet R.Platelet—leukocyte interactions: multiple links between inflammation, blood coagulation and vascular risk.Mediterr J Hematol Infect Dis. 2010;2:e2010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kashuk JL, Moore EE, Johnson JL, et al. Progressive postinjury thrombocytosis is associated with thromboembolic complications.Surgery. 2010;148:667–674discussion 74-75. [DOI] [PubMed] [Google Scholar]
- 15.Munoz M, Villar I, Garcia-Erce JA.An update on iron physiology.World J Gastroenterol. 2009;15:4617–4626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nemeth E, Valore EV, Territo M, et al. Hepcidin, a putative mediator of anemia of inflammation, is a type II acute-phase protein.Blood. 2003;101:2461–2463. [DOI] [PubMed] [Google Scholar]


