Abstract
Purpose of review
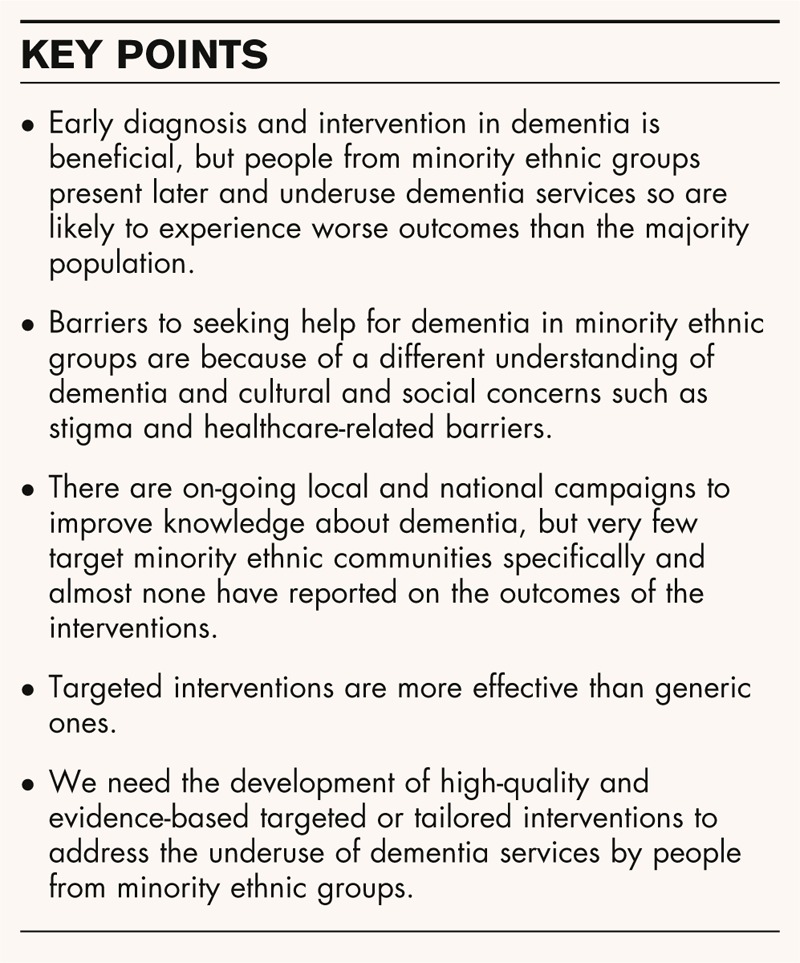
Only a minority of people with dementia receive a formal diagnosis despite a growing body of evidence highlighting the benefits of early diagnosis and intervention. People from minority ethnic groups are even more disadvantaged, as they tend to access dementia services later in the illness. Studies exploring the reasons behind underuse of dementia services by minority ethnic groups have highlighted the barriers to help-seeking that seem specific to the cultural groups studied. Understanding the barriers to help-seeking should help to identify the targets for interventions to encourage help-seeking in minority ethnic communities. This review sought to highlight the progress in this field and show what interventions have been developed so far.
Recent findings
Many countries are carrying out educational campaigns in an effort to increase awareness about dementia and reduce stigma, but none of these have reported any measurable outcomes of their interventions. Studies show that knowledge about dementia has the potential to increase help-seeking, but information should be targeted to the recipient audience.
Summary
Not enough has been done to address the inequality in service use for dementia in minority ethnic groups compared with the majority population. The time has come for the development of targeted and evidence-based interventions in order to improve access and affect outcomes.
Keywords: access, dementia, ethnicity, healthcare, minority
INTRODUCTION
Dementia is a growing national and international health concern. It currently affects over 800 000 people in the UK and costs the UK economy £23 billion per year [1]. Worldwide, it is estimated there are 24.3 million people living with dementia and the number of people affected is expected to double every 20 years to 81.1 million by 2040 [2].
There is no current cure for dementia, but early diagnosis of dementia is important, as it allows people to plan better for their future and to start treatments that slow the disease progression [1] Obtaining a diagnosis in a timely way enables people to access support, reduces carer stress, avoids crises and delays institutionalization [3,4▪]. The economic costs associated with obtaining a diagnosis are likely to be offset by the financial benefits of having an early diagnosis [4▪]. Despite the importance of early diagnosis, it is estimated that fewer than a third of people with dementia ever receive a diagnosis [3].
Most developed countries have a sizeable ethnic minority population. For example, in the UK, minority ethnic people account for 15% of the English population and 39% of the London population [5]. The USA 2012 census reports that 34% of its citizens are from an minority ethnic (White and non-Hispanic) group [6]. People from minority ethnic groups have an equally high prevalence of dementia compared with the majority ethnic population, with a higher prevalence in the African-Caribbean population [7], possibly because of increased vascular risk factors. The minority ethnic population in the UK and USA is younger than the majority population, but these groups tend to have a higher percentage of young-onset dementia [8], so the overall burden of dementia as the population ages is still substantial. Minority ethnic communities vary greatly between countries. In the USA, Hispanic and Latino Americans comprising 15% and Black Americans comprising nearly 13% of the population are the largest minority groups. In the UK, Irish and other non-UK white groups, and Indian and Pakistani ethnic groups, are the largest. There is as much variation within minority ethnic groups in terms of socioeconomic power, geography and experiences as in the majority group.
Box 1.
no caption available
Studies from the Western countries including the USA, UK and Australia have found that people from ethnic minority groups underuse dementia services [9], and this inequality of service use has become a significant concern because of its implications for poorer outcomes in dementia amongst minority ethnic groups. The UK government has suggested creating special memory services for minority ethnic groups and making sure services are culturally targeted and appropriate [8]. Equal access to dementia services for all ethnic groups is important to ensure everyone has access to the same potential health benefits. This review will first explore why people from minority ethnic groups may underuse dementia services and will then outline how this issue could be addressed.
DELAYED ACCESS TO DEMENTIA SERVICES IN MINORITY ETHNIC GROUPS
In order to improve access to diagnostic and intervention services efficiently, we need to first understand why people from minority ethnic groups are not accessing help for dementia at the moment. In our recent systematic review, we found that 13 studies have investigated this, mostly in the USA [10]. There was significant overlap in the barriers to accessing dementia services that these studies reported in a broad range of minority ethnic groups. These were attributing the symptoms to normal ageing or other physical, spiritual or psychological causes; denial that there was a problem or normalization of symptoms; concerns about stigma related to dementia; perceived ethical imperative to care for one's own family members without accessing help; and negative experiences of the healthcare service and feeling there was nothing that could be done for dementia. The only facilitator to help-seeking found was knowledge about dementia. As would be expected, people tend not to seek help for something which they believe is normal or not treatable with conventional medical input. For those who may have felt a medical opinion was needed, being dismissed by healthcare professionals, encountering language barriers or not knowing who to get help from would act as further barriers, even if stigma and societal pressures could be overcome.
Only two of the studies in the systematic review compared help-seeking for dementia in different ethnic groups. We subsequently carried out a qualitative study [11▪] to explore further whether barriers to accessing help for dementia differ across different ethnic groups and whether the perceived barriers to help-seeking have an impact on the subsequent help-seeking and diagnostic pathway. We interviewed the carers of people with dementia from different ethnic groups and showed certain barriers to help-seeking seemed specifically to occur in minority ethnic groups, such as different beliefs about the cause of symptoms, concerns about stigma and the perceived benefit of looking after your own family until you could no longer cope. The value of a diagnosis alone was also felt to be less beneficial amongst minority ethnic carers compared with their White UK counterparts. This study also replicated findings from a previous study [12] that showed that people from minority ethnic groups tended to obtain a diagnosis of dementia as a result of a crisis rather than in a planned way.
Overall, this indicates that barriers to help-seeking for dementia are culturally specific and that encouraging help-seeking in minority ethnic groups will therefore require an approach that takes these particular concerns into account.
REDUCING THE BARRIERS TO HELP-SEEKING
The three main categories of barriers to help-seeking for dementia in minority ethnic groups seem to be
knowledge related, that is, different beliefs about the cause and knowing the purpose of a diagnosis;
society related, that is, the concern about stigma and cultural expectations of looking after your own relatives until you can no longer cope;
healthcare related, that is, any hesitation in approaching healthcare professionals or any barriers within the healthcare system itself.
The UK government spends millions in information campaigns in other healthcare areas such as encouraging healthier lifestyle or reducing smoking. A review of these campaigns suggests that information about health topics can be a tool for changing behaviour, but simple provision of information is not sufficient [13]. It is useful to consider how this report's findings might inform how, what and to whom we should seek to provide information about dementia. They found that the content and source of the message, the way it is delivered and the target population may all affect its impact. Simple messages may be easier to communicate, but there is no evidence that these are more effective than more complex messages. Some research suggests that people view the government with mistrust, so that health messages are perceived in a more positive light if they come from an independent source. Health messages regarding lower risk behaviours benefit from framing in a positive light and highlighting the benefits of engaging in a certain behaviour, whereas higher risk behaviours seem more amenable to change if the dangers of the behaviour are highlighted. The impact of health messages are further affected by the mind-set and ‘stage of change’ that the recipient audience is in. People who are already worried about their health will respond more to a health promotion message than those who are not.
Information regarding dementia should specifically address the concerns and barriers of the minority ethnic carers and patients to whom it is directed. For example, the erroneous belief we and others have found to be particularly prevalent in minority ethnic groups is that dementia occurs because of nonbiological causes and that there is nothing that can be done about it. It might be that community organizations or religious organizations would be able to deliver the information more effectively than general practitioners or the Department of Health, or general practitioners more than the Department of Health, depending on whom those targeted by the information view as more trustworthy or relevant to their lives. How the message is delivered is also important. Generic communication which is not personalized is usually less effective than targeted or tailored (individualized) communication. A study looking at increasing the uptake of colorectal cancer screening found that the uptake was approximately 50% higher in the groups which had a targeted or tailored interventions compared with those who received generic information [14].
INTERVENTIONS TO INCREASE HELP-SEEKING FOR MENTAL HEALTH PROBLEMS
A recent study [15] found that a media intervention about mental health services increased positive attitudes towards help-seeking for mental health problems, but this did not necessarily translate into positive intentions to seek help for interpersonal difficulties. Bhugra and Hicks [16] found that people who received a pamphlet about depression and its treatment expressed a greater intention to seek help for depression and suicidality, and felt that antidepressants could be helpful. Actual help-seeking was not measured and the authors note that only 40% of those approached for participation agreed to take part. This raises the question of how to reach people who are not interested in receiving health-related messages.
Gulliver et al.[17] conducted a systematic review of eight different interventions designed to increase knowledge about mental health problems and encourage help-seeking. They found that mental health literacy content improved attitudes to help-seeking, but did not alter help-seeking behaviour. However, there was less evidence for the benefit of efforts to de-stigmatize or provide help-seeking information on help-seeking attitude. An exploratory randomized controlled trial (RCT) by the same group found that literacy about mental health problems increased positive attitudes towards help-seeking and reduced stigma, but did not increase help-seeking [18]. However, the authors state that this study was underpowered to detect an effect. This body of research suggests that providing information about an illness may improve attitudes towards help-seeking for that behaviour, but it does not alter stigma around the condition and may not translate to actual help-seeking behaviour.
INTERVENTIONS TO INFORM ABOUT DEMENTIA
The efforts to tackle stigma and improve public awareness about dementia, however, continue at a rapid pace. The National Dementia Awareness campaign in the UK was launched in September 2012 (http://www.dh.gov.uk/health/2011/09/raising-dementia-awareness). This involves TV adverts, online resources and development of an information leaflet. Similar campaigns are being run locally, for example, in Nottingham (http://www.nottingham.ac.uk/impactcampaign/campaignpriorities/healthandwell-being/dementia/dementia.aspx) and the south west (http://www.dementiaawareness.co.uk/). These are all for the general population, but a campaign specifically aimed at the South Asian population has been on-going in Bradford since 2009 (http://www.meriyaadain.co.uk). The latter is a social services led initiative that carries out community road shows, radio programmes and hosts groups to raise awareness of dementia and improve access to dementia services amongst this ethnic group, which currently underuses the services. Internationally, there are multiple awareness campaigns in different countries aimed at reducing the stigma associated with dementia using a variety of techniques such as providing information, hosting social events and facilitating the involvement in the arts for people with dementia [19]. All of these initiatives seem to be a rational approach to raising awareness and reducing stigma and are described by people involved with them in very positive terms, but there is no data on their effect on outcomes such as attitudes to help-seeking for dementia or actual help-seeking behaviour.
Is providing information about dementia of any use in changing behaviour? One study which approached this question from the other end was by Hurt et al.[20]. They compared the participants who sought help for subjective memory complaints versus those who did not seek help. The objective cognitive impairment in both groups was the same, but those who sought help were more likely to believe their symptoms had more serious consequences and were also more likely to believe the symptoms to be because of a biological cause that might be amenable to medical treatment. This seems to strengthen the argument that altering beliefs about dementia will encourage help-seeking behaviour for it.
INTERVENTIONS TO ENCOURAGE HELP-SEEKING FOR DEMENTIA
The only study we found which tested an intervention to encourage help-seeking for dementia found some promising results [21]. This project was designed to target the South Asian population in Kent. The researchers developed a bilingual leaflet (English/Punjabi) entitled ‘Ageing and Memory Problems: the help available’, providing information on the most common types of dementia, reversible causes of memory problems and local services. The leaflet was sent to 167 South Asian patients from a particular Primary Health group practice, who were over the age of 65 years and who did not have a diagnosis of dementia, with a letter encouraging them to make an appointment with the Asian nurse practitioner (who had undergone training in recognition of dementia symptoms) if they had concerns about their memory. After the initial 6-week period, leaflets were left in the general practice waiting area. A total of five South Asian patients made appointments regarding their memory in the initial 6-week period compared with no South Asian patients seen for memory problems in the preceding 3 months. Over the 12-month study period, there was a 37% increase in referrals to the local memory service compared with the previous year, although only a small proportion of these were from minority ethnic groups. This project suggests that it may be possible to increase help-seeking rates through a targeted written intervention. However, the increase specific to the South Asian population was relatively modest. In addition, the authors highlight a case study of an Asian man who sought help for his memory in response to receiving the leaflet. His memory was actually normal, but, on further involvement of healthcare services, he was found to be caring for his mother, who had profound dementia. The authors state ‘The family viewed the mother's memory problems as normal “old age”. Even her son, who had received the dementia leaflet and letter in his own right, had not considered that his mother may have dementia or need help from outside the family.’ This highlights that simply providing general information about dementia may not be enough to raise awareness of dementia amongst minority ethnic groups and that culturally targeted information is likely to be more effective in bringing about change.
REDUCING THE HEALTHCARE BARRIERS
Increasing knowledge and decreasing the stigma relating to dementia might increase the numbers of people seeking help from health services. In the UK, the primary point of contact for most people would be their general practitioner. However, barriers to early diagnosis within the healthcare system also exist and require targeting.
General practitioners are sometimes reluctant to diagnose dementia, as they assume the patient would not wish to receive the diagnosis because of stigma [22] or because of their own feelings that a diagnosis is pointless [23]. In the latter study, general practitioners stated they felt an early diagnosis of dementia was important but were not proactive in referring so that a diagnosis was made. Two systematic reviews [24,25] of educational interventions to improve diagnosis of dementia by primary care physicians concluded that providing education in a large group in a relatively passive way had no impact on diagnostic rates, but that small group learning and decision-support software could be effective in improving the diagnosis of dementia in primary care. At least two trials of educational interventions to improve dementia diagnosis by general practitioners are currently underway [26,27].
WHAT INTERVENTIONS ARE NEEDED?
There is preliminary evidence from one small study that providing information to South Asian UK minority groups and encouraging them to make an appointment with a South Asian worker to discuss their memory may increase help-seeking for memory concerns. This is promising, but there is now a pressing need to engage with minority ethnic communities to develop culturally sensitive interventions and to test their effectiveness in RCTs. Ultimately, the goal of such interventions is for dementia to be diagnosed earlier and more frequently. Effecting any kind of behavioural change is a complex process. Behavioural change interventions are important in addressing population health matters, but are difficult to design [28]. Behavioural change interventions should be based on a theoretical model with components that can be measured so that the mechanisms of successful or nonsuccessful interventions can be clarified, for example, whether knowledge change or attitude change makes a difference to behaviour [29].
CONCLUSION
Minority ethnic people are less likely to access services for dementia and do so at a later stage. As yet, no interventions to increase help-seeking and promote earlier diagnosis in dementia amongst minority ethnic groups have been tested in RCTs, although there is preliminary evidence from one small study that a culturally tailored intervention for South Asian people may improve help-seeking. An intervention to encourage access to dementia services for people from ethnic minorities should be based on the evidence available and address known barriers to accessing services in a culturally appropriate way. To have the highest chance of being effective, the intervention would have to come from a trusted source and be targeted at the relevant population and should be delivered to people for whom it would have more salience. All elements of the intervention should be clearly described and based on theory so that key effective or ineffective components of the intervention can be established. So far, there is work on-going in raising the awareness of dementia nationally and internationally, but it is important to ensure that interventions are having an effect on people's attitudes and behaviours to optimize our use of resources.
Acknowledgements
None.
Conflicts of interest
None.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
Additional references related to this topic can also be found in the Current World Literature section in this issue (p. 425).
REFERENCES
- 1.Luengo-Fernandez R, Leal J, Gray A. Dementia 2010: the prevalence, economic cost and research funding compared with other major diseases. A report prepared by the Health Economics Research Centre, Oxford University, for the Alzheimer's Research Trust. Alzheimer's Research Trust; 2010. [Google Scholar]
- 2.Ferri CP, Prince M, Brayne C, et al. Global prevalence of dementia: a Delphi consensus study. Lancet 2005; 366:2112–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Health. Living well with dementia: a National dementia strategy. London: Department of Health; 2009. [Google Scholar]
- 4▪.Prince M, Bryce R, Ferri CP. World Alzheimer Report 2011: the benefits of early diagnosis and intervention. London: Alzheimer's Disease International; 2011. [Google Scholar]; A coherent and convincing presentation of the benefits of timely dementia diagnosis.
- 5.Office of National Statistics. Population estimates by ethnic group. London: Office of National Statistics; 2007. [Google Scholar]
- 6.US Census Bureau. Statistical abstract of the United States: 2012. Washington, DC: US Census Bureau; 2011. Report No.: 131st ed. [Google Scholar]
- 7.Adelman S, Blanchard M, Rait G, et al. Prevalence of dementia in African-Caribbean compared with UK-born White older people: two-stage cross-sectional study. Br J Psychiatry 2011; 199:119–125. [DOI] [PubMed] [Google Scholar]
- 8.National Audit Office. Improving services and support for people with dementia. London: The Stationery Office; 2007. [Google Scholar]
- 9.Cooper C, Tandy R, Balamurali TBS, Livingston G. A systematic review and metaanalysis of ethnic differences in use of dementia treatment, care, and research. Am J Geriatr Psychiatry 2010; 18:193–203. [DOI] [PubMed] [Google Scholar]
- 10.Mukadam N, Cooper C, Livingston G. A systematic review of ethnicity and pathways to care in dementia. Int J Geriatr Psychiatry 2011; 26:12–20. [DOI] [PubMed] [Google Scholar]
- 11▪.Mukadam N, Cooper C, Basit B, Livingston G. Why do ethnic elders present later to UK dementia services? A qualitative study. Int Psychogeriatr 2011; 23:1070–1077. [DOI] [PubMed] [Google Scholar]; A summary of the barriers that people from minority ethnic groups may face in accessing help for dementia. This suggests targets for interventions to improve health in these underserved communities.
- 12.Hinton L, Franz C, Friend J. Pathways to dementia diagnosis: evidence for cross-ethnic differences. Alzheimer Dis Assoc Disord 2004; 18:134–144. [DOI] [PubMed] [Google Scholar]
- 13.Robertson R. Kicking bad habits: using information to promote healthy behaviours. London: King's Fund; 2008. [Google Scholar]
- 14.Myers RE, Sifri R, Hyslop T, et al. A randomized controlled trial of the impact of targeted and tailored interventions on colorectal cancer screening. Cancer 2007; 110:2083–2091. [DOI] [PubMed] [Google Scholar]
- 15.Demyan AL, Anderson T. Effects of a brief media intervention on expectations, attitudes, and intentions of mental health help seeking. J Couns Psychol 2012; 59:222–229. [DOI] [PubMed] [Google Scholar]
- 16.Bhugra D, Hicks MH. Effect of an educational pamphlet on help-seeking attitudes for depression among British South Asian women. Psychiatr Serv 2004; 55:827–829. [DOI] [PubMed] [Google Scholar]
- 17.Gulliver A, Griffiths KM, Christensen H, Brewer JL. A systematic review of help-seeking interventions for depression, anxiety and general psychological distress. BMC Psychiatry 2012; 12:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gulliver A, Griffiths KM, Christensen H, et al. Internet-based interventions to promote mental health help-seeking in elite athletes: an exploratory randomized controlled trial. J Med Internet Res 2012; 14:e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Batsch NL, Mittelman MS. World Alzheimer Report 2012: overcoming the stigma of dementia. London: Alzheimer's Disease International; 2012. [Google Scholar]
- 20.Hurt CS, Burns A, Brown RG, Barrowclough C. Why don’t older adults with subjective memory complaints seek help? Int J Geriatr Psychiatry 2012; 27:394–400. [DOI] [PubMed] [Google Scholar]
- 21.Seabrooke V, Milne A. Early intervention in dementia care in an Asian community: lessons from a dementia collaborative project. Qual Ageing 2009; 10:29–36. [Google Scholar]
- 22.Koch T, Iliffe S. EVIDEM-ED project Rapid appraisal of barriers to the diagnosis and management of patients with dementia in primary care: a systematic review. BMC Fam Pract 2010; 11:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moore V, Cahill S. Diagnosis and disclosure of dementia – a comparative study of Irish and Swedish General Practitioners. Aging Mental Health 2013; 17:77–84. [DOI] [PubMed] [Google Scholar]
- 24.Koch T, Iliffe S. Dementia diagnosis and management: a narrative review of changing practice. Br J Gen Pract 2011; 61:e513–e525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perry M, Draskovic I, Lucassen P, et al. Effects of educational interventions on primary dementia care: a systematic review. Int J Geriatr Psychiatry 2011; 26:1–11. [DOI] [PubMed] [Google Scholar]
- 26.Iliffe S, Koch T, Jain P, et al. Developing an educational intervention on dementia diagnosis and management in primary care for the EVIDEM-ED trial. Trials 2012; 13:142–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pond CD, Brodaty H, Stocks NP, et al. Ageing in general practice (AGP) trial: a cluster randomised trial to examine the effectiveness of peer education on GP diagnostic assessment and management of dementia. BMC Fam Pract 2012; 13:12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Michie S. Designing and implementing behaviour change interventions to improve population health. J Health Serv Res Pol 2008; 13 (Suppl.9):64–69. [DOI] [PubMed] [Google Scholar]
- 29.Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008; 337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]


