Abstract
Background
Major depressive disorder (MDD) is a prevalent and severe disorder. Although effective treatments for MDD are available, many patients remain untreated, mainly because of insufficient treatment capacities in the health care system. Resulting waiting periods are often associated with prolonged suffering and impairment as well as a higher risk of chronification. Web-based interventions may help to alleviate these problems. Numerous studies provided evidence for the efficacy of web-based interventions for depression. The aim of this study is to evaluate a new web-based guided self-help intervention (GET.ON-Mood Enhancer-WL) specifically developed for patients waiting to commence inpatient therapy for MDD.
Methods
In a two-armed randomised controlled trial (n = 200), the web-based guided intervention GET.ON-Mood Enhancer-WL in addition to treatment as usual (TAU) will be compared with TAU alone. The intervention contains six modules (psycho education, behavioural activation I & II, problem solving I & II, and preparation for subsequent inpatient depression therapy). The participants will be supported by an e-coach, who will provide written feedback after each module. Inclusion criteria include a diagnosis of MDD assessed with a structured clinical interview [SCID] and a waiting period of at least three weeks before start of inpatient treatment. The primary outcome is observer-rated depressive symptom severity (HRSD24). Further (explorative) questions include whether remission will be achieved earlier and by more patients during inpatient therapy because of the web-based preparatory intervention.
Discussion
If GET.ON-Mood Enhancer-WL is proven to be effective, patients may start inpatient therapy with reduced depressive symptom severity, ideally leading to higher remission rates, shortened inpatient therapy, reduced costs, and decreased waiting times.
Trial registration
German Clinical Trial Registration (DRKS): DRKS00004708.
Keywords: Internet therapy, Waiting time, Major depression, Inpatient treatment, Remission
Background
Major depressive disorder (MDD) is one of the most prevalent psychiatric disorders, with a lifetime prevalence that is currently estimated at about 16% [1-3] and predicted to further increase in the foreseeable future [4,5]. By 2030, depressive disorders are anticipated to be responsible for the highest disease burden in high-income countries among all diseases [6]. Suffering from MDD is accompanied by a substantial loss in quality of life, not only for patients but also for their relatives [7-9]. Furthermore, suffering from a depressive episode is associated with a high risk of relapse and recurrence [1,10] as well as a chronic course [11], increased mortality rates [12], significant disability, high medical service use, and major economic costs [13-16].
Although numerous studies provide evidence for the efficacy of available psychological and pharmacological treatments [17,18], many individuals remain untreated [19,20]. The reasons for this treatment gap are twofold. First, individuals who likely to benefit from treatment do not seek treatment because they lack knowledge on available treatment options, anticipate negative (social) consequences, live in underserved areas, fear prohibitive costs, or prefer self-help [20]. Limited availability of clinicians and difficulties in attending therapy during usual business hours are further barriers [21]. Second, those who do seek help rarely receive immediate access to treatment due to long waiting lists for both inpatient and outpatient psychotherapy [20,22]. Consequently, people with an urgent need for therapy are left alone with their burden, which poses several ethical, practical, and therapeutic problems. In addition to high levels of suffering, long waiting times might increase symptom severity and hence increase the need for more intense and longer treatments [23,24].
Another related problem is that because of factors such as limited financial resources and time, inpatient patients are often discharged from the clinic at a very early stage, leaving them with substantial residual symptoms. However, even low levels of residual symptoms are known to increase the risk for relapse and recurrence [25-28]. Recent meta-analyses show that between 40 and 60% of patients with MDD relapse after the initial response to an acute-phase treatment [27].
The use of the internet to provide guided self-help might contribute to solving these problems. First, meta-analytical evidence has shown comparable effects of such interventions compared to traditional psychological treatments when there is at least some support from a professional [29-31]. Furthermore, web-based interventions may represent a far-reaching method for supporting patients during the waiting time for psychotherapy [32].
This method has been well accepted by patients and shown to be effective in the acute treatment phase as well as the maintenance phase [33-37]. The adaptation of internet-based strategies for the waiting phase has several advantages: (a) patients can begin their treatment immediately with no additional waiting time; (b) the online program can be used 24 hours a day, independent of office hours, every day of the week; (c) the material can be reviewed as often as needed; (d) the patient can use it in a familiar environment, without any time or travel costs, which allows for privacy and consistency of care [34,38,39]; and (e) web-based interventions can help patients to practise skills that are relevant for their subsequent therapy (i.e., self-monitoring, problem-solving competencies, behavioural activation).
However, to the best of our knowledge, only one study has evaluated the use of internet-based guided self-help for patients on a waitlist for psychotherapy [40]. In this non-randomised observational study, the researchers found large and significant between-group effect sizes for online treatment for depression (d = 0.94) compared to a waiting control group after five weeks. The majority of eligible patients preferred the web-based problem-solving therapy instead of waiting for face-to-face treatment. Participation in this intervention increased the speed of improvement for symptoms of depression during the following therapy [40].
Given the high level of suffering from a depressive episode and the limited availability of psychotherapy resources, new and innovative approaches are needed to address the long waiting times. Using waiting times effectively by providing patients with evidence-based guided self-help methods might result in higher remission rates at the end of inpatient treatment or an earlier remission, thereby reducing costs.
Trial objectives and purpose
The aim of this multi-centre randomised controlled trial is to evaluate whether a newly developed web-based guided self-help intervention (GET.ON-Mood Enhancer-WL) is effective in reducing depressive symptom severity in patients waiting for inpatient therapy when compared to treatment-as-usual. Moreover, it will be explored whether participants would respond or achieve remission earlier in the course of the subsequent inpatient therapy and would be more likely to be fully remitted at discharge than would controls.
Methods
Study design
In this two-armed randomised controlled trial, we will compare GET.ON-Mood Enhancer-WL combined with TAU to TAU alone. The target group will consist of individuals (n = 200) who have been referred to inpatient treatment of major depressive disorder by their general practitioner, psychotherapist, or psychiatrist and are awaiting inpatient therapy in one of the German study clinics (Schön Klinik Bad Arolsen/Bad Staffelstein/Bad Bramstedt). The study will be implemented as part of the routine mental health service of the study clinics. Primary and secondary outcome measures will be assessed at baseline, post-treatment (three weeks), at intake for inpatient therapy, weekly during inpatient therapy, and after inpatient therapy. Table 1 gives an overview of the assessments at all planned time points.
Table 1.
Overview of assessments
| Measure | Description | Items |
T
0
|
T
1
|
T
2
|
T
3
|
T
4
|
T
5
|
T
6
|
T
7
|
T
8
|
T
9
|
T
10
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| baseline pre-treatment | weekly monitoring | post-treatment | pre-inpatient therapy | weekly monitoring | post-inpatient therapy | ||||||||
| SCID |
clinical interview, DSM-V criteria |
|
X |
|
|
|
|
|
|
|
|
|
|
| HRSD primary outcome |
depressive symptoms, clinician-rated |
24 |
X |
|
|
X |
|
|
|
|
|
|
|
| QIDS-C |
depressive symptoms and severity, clinician-rated |
16 |
X |
|
|
X |
|
|
|
|
|
|
X |
| PHQ-9 |
depressive symptoms |
9 |
X |
X |
X |
X |
X |
X |
X |
X |
X |
X |
X |
| Penn State-worry questionnaire–short version |
worrying |
3 |
X |
|
|
X |
|
|
|
|
|
|
X |
| BA-DS–short version |
behavioural activation |
9 |
X |
|
|
X |
|
|
|
|
|
|
X |
| Social problem solving inventory–short version |
problem solving |
10 |
X |
|
|
X |
|
|
|
|
|
|
X |
| EuroQoL |
life quality |
5 |
X |
|
|
X |
|
|
|
|
|
|
X |
| Brief scale for measuring subjective prognosis of gainful employment |
subjective prognosis of gainful employment |
3 |
X |
|
|
|
|
|
|
|
|
|
|
| PATHEV |
therapy expectations |
11 |
X |
|
|
X |
|
|
|
|
|
|
X |
| HAQ | help alliance | 11 | X | X | X | ||||||||
All procedures were approved by the ethics committee at the Philipps University of Marburg in November 2012 (reference number: 2012-37kr). The trial is registered at the German Clinical Trial Register (DRKS00004708).
Inclusion and exclusion criteria
Patients will be included in this trial when they (a) are awaiting to be treated with routine mental health care at any of the three study centres, (b) are scheduled to have a waiting time of at least three weeks, (c) are 18 years of age or older, (d) meet criteria of a major depressive episode (according to DSM-V criteria), (e) are motivated to actively participate in the self-guided internet intervention to improve their depressive mood during the waiting time, (f) have access to a computer with an internet connection and a valid email address, and (g) return the signed informed consent form.
We will exclude patients with bipolar disorder or acute psychotic symptomatology (according to DSM-V criteria) or patients showing a notable suicidal risk, as assessed during the structured clinical interview.
Recruitment
Patients who apply for inpatient therapy via the clinic website (http://www.schoen-kliniken.de/ptp/kkh/bar/anmeldung/krankenhaus/) will be immediately informed about the current trial and can sign up to receive further information. Patients who directly contact the clinic’s head office will receive by mail an information letter that contains the hyperlink to the above-mentioned website.
Assessment of eligibility and randomisation
After signing up for further information via the website, prospective participants will receive an email from the research team that includes detailed information about the study. They will be asked to send back an informed consent form via e-mail if they are willing to participate. Patients providing informed consent will be interviewed by telephone to clarify whether they fulfill the inclusion criteria. These structured clinical interviews for DSM disorders (SCID) will be conducted by psychotherapists-in-training who will be weekly supervised by an experienced clinician. Participants providing informed consent, meeting all of the inclusion and none of the exclusion criteria will enter the study. They will be randomly allocated to treatment conditions and complete initial assessment. The allocation will be performed by an independent researcher not otherwise involved in the study using an automated, computer-based random integer generator (randlist). The allocation will be concealed in advance from the participants, researchers involved in recruitment, and inpatient therapists. Patients will be informed that they can withdraw from the study at any time, without any consequences for their subsequent treatment. See Figure 1 for participants’ flow throughout the study.
Figure 1.
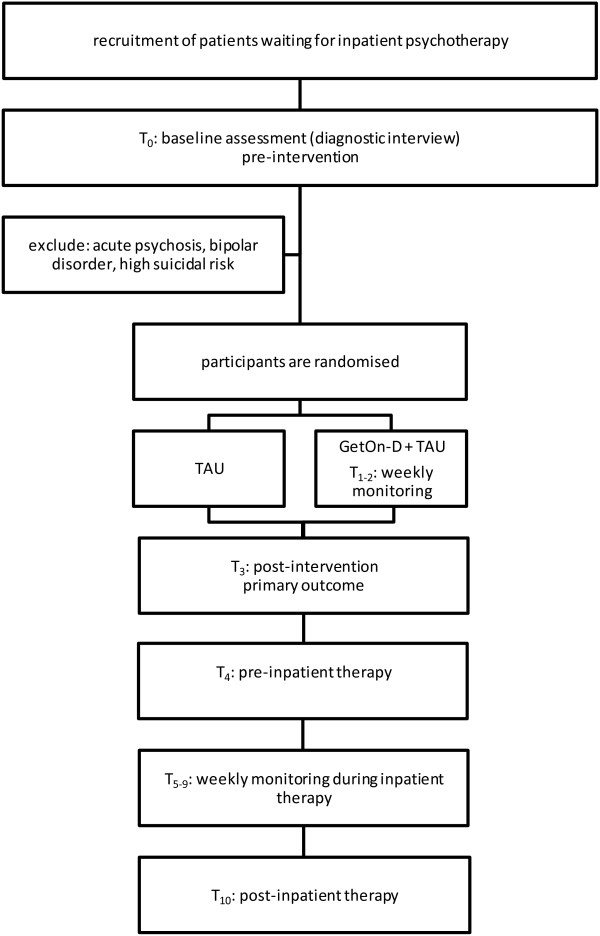
Study flow diagram.
Assessments
Self-report and observer-rated assessments will take place at baseline, post-intervention (three weeks after randomisation), at intake for inpatient treatment, weekly during inpatient therapy, and after completion of inpatient therapy (see Figure 1 and Table 1 for a detailed overview). Self-report data will be collected using a secure web-based assessment system (AES, 256-bit encrypted), and observer-based assessments will be conducted via the telephone by trained interviewers. Observer-rated assessments will be recorded to examine interrater reliability. In cases of disagreement, the two raters will discuss until a consensus is formed, and the rating agreed upon will be used for further analyses. If no agreement is reached after discussion, the assessment will be rated by an experienced diagnostic rater, and this rating will be used for analysis.
Blinding
The research staff conducting the observer-based rating of depressive symptoms will be blinded to the participants’ assigned conditions. Considerable effort is being undertaken to ensure blindness, including the following: (a) an explanation to the participants as to why it is important not to inform the interviewer about the condition to which they were assigned, (b) a written reminder in the interview manual prompting the interviewer to ask the participant not to inform him or her about the randomisation status, (c) verbal reminders to the patient before the interview, and (d) a documentation after the assessment of whether or not the interviewer is still blind to the treatment condition. If the interviewer finds out about the treatment condition another independent interviewer will conduct the interview instead. Participants will not be blinded to the treatment condition.
Interventions
GET.ON-Mood Enhancer-WL–experimental group
The primary purpose of the web-based intervention (GET.ON-Mood Enhancer-WL) is to reduce depressive symptomatology prior to intake for inpatient treatment. In addition GET.ON-Mood Enhancer-WL aims to prepare patients for subsequent inpatient therapy by providing relevant information (psycho education) and using effective and well known elements that are mainly based on behavioural therapy and problem-solving therapy. Abundant evidence exists to support components such as psycho education [18,35], behavioural activation [41,42], and problem solving [43,44] in the treatment of major depression.
A previous meta-regression analysis examining the relationship of treatment intensity to treatment outcome in the treatment of depression indicated that more frequent therapy sessions may be associated with a better outcome compared to less frequent sessions [45]. Thus, we included six modules and advised participants to complete at least one, but preferably two, lessons per week. In all, the training lasts approximately three weeks. We will not include more modules because (a) a recent meta-analysis [46] found web-based interventions for depression including more than seven modules to be less effective (d = 0.36) than interventions with seven or fewer modules (d = 0 .75) and (b) we wanted to lower the threshold for individuals as much as possible. Table 2 gives an overview of the sessions and their content.
Table 2.
Overview of content
| Session | Content |
|---|---|
| Session 1: psychoeducation |
First, patients should learn about their disease (symptoms, causes, and types of depression). In addition, the role of motivation in getting through this program should be emphasised. |
| Sessions 2 and 3: behavioural activation |
Second, two behavioural activation sessions will teach the patient about the association between activity and mood. Thus, positive activities can be planned and implemented into the daily routine. In addition, possible obstacles will be considered. The planning of positive activities remains part of the program during the subsequent sessions. Furthermore, participants can work through the facultative module about sleep problems. |
| Sessions 4 and 5: problem-solving techniques |
Sessions 4 and 5 are concerned with problem solving in which the patient learns to distinguish between solvable and unsolvable problems and practises using a six-step plan as a tool to solve problems. Information about unsolvable problems is given as well. Moreover, techniques to stop worrying are introduced. |
| Session 6: evaluation and preparation | Finally, the patient evaluates his gains and receives a summary of the program. Furthermore, he is encouraged to think about a future plan (such as choosing topics to work on during his inpatient stay). |
Given the fact that some studies show a better effect for interventions with at least a low level of guidance compared to unguided interventions [46-48], this strategy might be a promising approach to encourage high treatment adherence. Therefore GET.ON-Mood Enhancer-WL provides a low level of guidance, including individualised feedback for the patient after finishing each of the six sessions. This feedback will be given by psychotherapists-in-training who will receive weekly supervision by an experienced clinician. After completion of the program, there will be no further guidance provided, but the patient will be free to continue with the program or to repeat the exercises.
Some studies have found that highly interactive interventions are more engaging, create higher expectations for improvement, and promote increased motivation and satisfaction in general [49,50]. Hence, the program contains several interactive components for the patients, including a diary to rate their mood and activity level, videos, testimonials, exercises, homework exercises, optional modules, and a library. A strong focus is placed on transfer tasks (homework assignments) to integrate newly acquired strategies and techniques into daily life. In the beginning of each subsequent lesson, participants are invited to reflect on their experiences with the newly acquired skills. The training is adaptive in a sense, as the content is tailored to the specific needs of the individual participant by continuously asking participants to respond by choosing from various response options. Subsequent content is then tailored to the participant’s response. Using responsive web design, participants can follow the program on the internet using a computer, tablet, or mobile phone. An integrated read-aloud function allows participants to follow an audio narration of the lessons.
Treatment as usual (TAU)–control group
TAU includes a wide variety of treatment alternatives, such as antidepressant medication, counselling, face-to-face psychotherapy, or no treatment at all. However, to control for potential confounding effects, treatment utilisation as well as changes in the dose of antidepressant medication will be closely monitored during the study period.
Inpatient treatment–both groups
Inpatient treatment will generally base on Cognitive Behavioral Therapy (CBT). Patients will receive one to two session of individual therapy (50 minutes) and an average of six sessions of group therapy (90 minutes) per week. Interventions will be supplemented with sports-and physiotherapy, as well as medical treatment (including medication) when necessary. Duration of treatment usually range between 21 and 56 days.
Sample size
This study will be designed to detect a difference of d = 0.40 between the groups as the primary outcome. As patients expect to be treated for their depression in the subsequent inpatient psychotherapeutic treatment, we do expect a somewhat smaller effect size for our intervention than what has been found in the most recent meta-analysis of internet-based guided self-help treatments for depression [35]. With a power of 0.80 in a two-tailed test and α = .05, a sample of n = 200 participants would need to be included at baseline (calculated using GPower 3.1).
Primary and secondary outcomes
Primary outcome
The primary outcome is depressive symptom severity, as measured by the Hamilton Rating Scale for Depression (HRSD24) [51], with assessments conducted pre-and post-treatment. The HRSD is likely the most widely used clinician-rated scale for measuring depression. It assesses depressed mood, vegetative and cognitive symptoms of depression, and anxiety symptoms during the prior seven days. Items are rated on either a five-point or a three-point scale, and the total score is derived by summing the individual item scores. Higher scores indicate greater symptom severity. The HRSD has an interrater-reliability of 0.90 [51] and shows high internal consistency (α = 0.88) [52]. Furthermore, it is sensitive to change over time and treatment and corresponds well with overall clinical ratings of severity [53,54]. The cut-off points of 10, 19, 27, and 35 represent the thresholds for mild, moderate, severe, and very severe depression, respectively [52].
Secondary outcomes
Depressive symptomatology
Observer-based ratings of depressive symptom severity will additionally be collected using the 16-item Quick Inventory of Depressive Symptomatology–Clinician-Rating (QIDS-CR16) [52] to achieve a more nuanced understanding of the symptom severity. The QIDS-CR16 is a brief clinician-report rating scale developed from the 30-item Inventory of Depressive Symptomatology [55,56]. Unlike the HRSD, the QIDS-CR16 evaluates only the nine depression criterion symptom domains (i.e., sad mood, concentration, self-criticism, suicidal ideation, interest/involvement, energy/fatigability, sleep disturbance, appetite/weight change, and psychomotor agitation/retardation) from the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) [57] during the prior seven days. Each item is scored on a scale from 0 to 3 points, with higher scores indicating higher symptom severity. This measure has shown good psychometric properties, such as strong internal consistency (α = 0.85), concurrent validity, and sensitivity to symptom change in patients with MDD [56]. The cut-off points of 6, 11, 16, and 21 represent the thresholds for mild, moderate, severe, and very severe depression, respectively.
Self-reported depressive symptoms will be assessed with the Patient Health Questionnaire (PHQ-9) [58]. This measure has comparable sensitivity and specificity to many other depression measures, although it is significantly shorter than most other measures [59]. The internal reliability of PHQ-9 reaches values between α = 0.86 and 0.89. The score ranges from 0 to 27 because each of the nine items can be scored from 0 (“not at all”) to 3 (“nearly every day”). The cut-off points of 5, 10, 15, and 20 represent the thresholds for mild, moderate, moderately severe, and severe depression, respectively [58,59].
Quality of life
Health-related quality of life will be measured with the generic EuroQol [60]. The EuroQol includes the EQ-5D and a visual analogue scale. The EQ-5D consists of five items covering five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). The items are rated as causing “no problems”, “some problems”, or “extreme problems”. This questionnaire shows good psychometric properties in terms of validity and reliability in Germany [61].
Problem-solving skills
Problem-solving ability (i.e., generalised appraisal, beliefs, expectancies, and emotional responses) will be measured with two subscales of the Social Problem-Solving Inventory-Revised (SPSI-R) [60]. The positive problem orientation (PPO) subscale represents a constructive dimension, whereas the negative problem orientation (NPO) subscale is viewed as a dysfunctional dimension. Both subscales demonstrate strong psychometric properties. Cronbach’s alphas for these subscales are α = 0.76 for the PPO dimension and 0.83 for the NPO dimension [62].
Behavioural activation
Participants’ activation towards goals/values and pleasant activities as well as avoidance behaviours will be measured with the BADS-Short Form (BADS-SF) [63]. The BADS-SF includes nine items comprising two subscales (activation and avoidance). The items are rated on a seven-point scale. Higher scores indicate that the individual scores high on the area of interest. The BADS-SF shows good psychometric properties. The internal consistency is α = 0.82 [63].
Worrying
Worrying will be assessed with the ultra-brief version of the Penn State Worry Questionnaire (PSWQ) [64]. This version consists of three items derived from the standard version, with each item being rated on a seven-point scale. The total score ranges from 0-18, with a higher score indicating more worry. The ultra-brief version shows similar psychometric properties as the standard version and an internal consistency of α = 0.85 [64].
Therapy expectations and helping alliance
Therapy expectations will be assessed with the Patient Questionnaire on Therapy Expectation and Evaluation (PATHEV) [65], which includes the following three scales: hope for improvement, fear of change, and suitability. The items are rated on a three-point-scale. The reliability of the scales has been shown to be good to sufficient (α = 0.73-0.89) [65].
Therapeutic alliance will be measured with the Helping Alliance Questionnaire (HAQ) [64]. This self-report questionnaire contains 11 items rated on a six-point-scale and including two subscales: “helpfulness” and “cooperation”. The scale exhibits excellent internal consistency (α = 0.89) and test-retest reliability [66,67].
Response remission, and time to remission
Based on the recommendation of Rush (2006), we will use a definition of response/remission that reflects a clinically significant benefit, depending on the specific setting and needs in this trial [68]. A decline in the PHQ-9-score of at least five points will be taken as a clinically significant response. Remission in this specific context will be understood as a symptom-free state, an absolute PHQ-9-score of less than ten will be defined as partial remission, and a PHQ-9-score of less than five will be defined as remission [58]. Time to remission will be defined as the number of days until the symptom-free state is achieved for the first time.
Statistical analyses
This clinical trial will be conducted in compliance with the protocol of the Declaration of Helsinki and GCP. Aiming at an intention-to-treat design we will include all participants who will be randomly assigned to conditions. Additional per protocol analyses (PPA) will be conducted, including only participants’ satisfying protocol treatment.
Missing data will be handled using multiple imputations (MI). MI is especially robust with respect to missing data [69]. Nevertheless, to assess systematic effects of missing data that cannot be ignored, pattern mixture analyses for multi-level longitudinal approaches [70] will be conducted. To determine whether the treatment effect is dependent on missing data, the missing-data pattern of each participant will first be coded and then included in a three-way interaction (missing-data pattern x condition x change in depression severity) in the main outcome analyses. If no significant interactions between the missing-data pattern and the treatment outcome are found, it can be concluded that it is very unlikely that missing data skewed the results.
The mean improvement scores on all continuous outcome measures will be analysed within and between groups via mixed-model analyses of variance. For all mixed-model analyses, Cohen’s d[71] will be calculated by standardising the differences between baseline and follow-up scores by the pooled standard deviation of baseline scores.
The clinically significant improvements between pre-treatment and post-treatment will be examined with regard to the definition of Kroenke (2002) [58]. Differences in response and remission rates will be analysed using chi-square tests. We will also calculate the number needed to be treated (NNT) to achieve response, partial remission, or remission. Time to remission will be measured in days, and the differences between groups in time to remission will be compared using a t-test for independent samples.
Analyses will be performed using an alpha level of 0.05 and one-sided tests will be used for unidirectional and two-sided tests for bidirectional hypotheses. All analyses will be conducted using SPSS 21.
Discussion
Major depression is a prevalent and severe disorder. Several circumstances lead to the fact that patients remain untreated despite their urgent need for help. Web-based treatments may be an appropriate way of bridging the time gap for patients on a waiting list. Using waiting time efficiently by introducing patients to upcoming therapeutic components before the start of inpatient therapy might be a promising approach to reduce the burden of disease for the patients, to promote earlier discharges and, as a result, to achieve shorter waiting times for subsequent patients.
This study will probably contribute to the literature by evaluating a new web-based intervention for depression compared to treatment as usual in patients on a waiting list for inpatient psychotherapy in a rater-blind randomised controlled trial. We will (a) test the main hypothesis that providing patients access to internet-based, guided self-help will lead to reduced symptom severity before inpatient treatment starts. Moreover, we will (b) investigate whether patients achieve remission earlier and (c) whether we can find significantly more patients with remission or response at the end of inpatient treatment.
There are several strengths to this study: This study will likely be one of the first randomised controlled studies that investigates a web-based intervention for patients on a waiting list for inpatient psychotherapy. We will also (a) use validated clinician-rated measures administered by independent raters blind to treatment condition in addition to self-report, (b) include a specific sample defined by standard diagnostic measures, (c) implement an appropriate statistical analysis plan, and (d) use state-of-the-art methods to cope with missing data.
This trial has also several limitations: As the trial will be conducted within the context of routine mental health care, the time span between the post-treatment assessment (conducted after the web-based treatment) and the beginning of inpatient therapy depends on both the capacities of the clinic and the eagerness of the patient and therefore will vary between patients. We will assess post-treatment data in both conditions at three weeks after randomisation to ensure a comparable time frame. Hence, patients will be at varying states within the online training when the post-treatment assessment takes place. Furthermore, we chose not to include a placebo/attention control condition because the TAU condition cannot be foreknown and is expected to be quite heterogeneous. Besides it is our aim is to study the effectiveness of GET.ON Mood Enhancer-WL in addition to and compared with usual care, as is standard in pragmatic trials [72]. However, due to the lack of such an active control condition, the mechanisms responsible for any possible effects will remain unclear. Last, we will include follow-up assessments only until the end of inpatient treatment. Therefore, we cannot draw conclusions about the effects on the long-term course of symptoms.
In the long term, it would be a desirable step to increasingly implement a new procedure such as this into the daily routine of inpatient as well as outpatient therapy. It would be good practice for the therapist to know in detail what steps the patient has taken previously and to be able to continue the previous gains. This knowledge would assist both the patient and the therapist, saving time and effort, and allowing them to concentrate on further issues and to intensify the treatment process.
Future research could make use of a homogenous control group, focus on various modifications of the program to identify active ingredients, compare different interventions that are likely to be effective as pre-inpatient treatments, evaluate web-based interventions for other disorders than depression or change the setting into the field of outpatient therapy.
Competing interests
Professor Berking is a minority shareholder of Minddistrict GmbH, which will provide the platform for the web-based interventions.
Authors’ contributions
MB obtained funding for this study. JR, DE, HR, and MB contributed to the development of the GET.ON depression training. All authors contributed to the study design. JR drafted the manuscript. JR, DE and MB contributed to the further writing of the manuscript. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Jo Annika Reins, Email: reins@inkubator.leuphana.de.
David Daniel Ebert, Email: ebert@inkubator.leuphana.de.
Dirk Lehr, Email: lehr@inkubator.leuphana.de.
Heleen Riper, Email: h.riper@vu.nl.
Pim Cuijpers, Email: p.cuijpers@vu.nl.
Matthias Berking, Email: berking@staff.uni-marburg.de.
Acknowledgements
This study is funded by the European Union (EFRE: ZW6-80119999, CCI 2007DE161PR001).
References
- Kessler RC. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Alonso J, Angermeyer M, Lépine J. The European study of the epidemiology of mental disorders (ESEMeD) project: an epidemiological basis for informing mental health policies in Europe. Acta Psychiatr Scand. 2004;109:5–7. doi: 10.1111/j.1600-0047.2004.00325.x. [DOI] [PubMed] [Google Scholar]
- Waraich P, Goldner EM, Somers JM, Hsu L. Prevalence and incidence studies of mood disorders: a systematic review of the literature. Can J Psychiatry. 2004;49:124–138. doi: 10.1177/070674370404900208. [DOI] [PubMed] [Google Scholar]
- Ansseau M, Dierick M, Buntinkx F, Cnockaert P, De Smedt J, van Den Haute M, Vander Mijnsbrugge D. High prevalence of mental disorders in primary care. J Affect Disord. 2004;78:49–55. doi: 10.1016/S0165-0327(02)00219-7. [DOI] [PubMed] [Google Scholar]
- Briley M, Lépine. The increasing burden of depression. NDT. 2011;7:3–7. doi: 10.2147/NDT.S19617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatr. 2005;162:1171–1178. doi: 10.1176/appi.ajp.162.6.1171. [DOI] [PubMed] [Google Scholar]
- Ebmeier K, Donaghey C, Steele JD. Recent developments and current controversies in depression. Lancet. 2006;367:153–167. doi: 10.1016/S0140-6736(06)67964-6. [DOI] [PubMed] [Google Scholar]
- Luppa M, Heinrich S, Angermeyer MC, König H, Riedel-Heller SG. Cost-of-illness studies of depression. J Affect Disord. 2007;98:29–43. doi: 10.1016/j.jad.2006.07.017. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Dunn TW, Jarrett RB. Reducing relapse and recurrence in unipolar depression: a comparative meta-analysis of cognitive-behavioral therapy’s effects. J Consult Clin Psychol. 2007;75:475–488. doi: 10.1037/0022-006X.75.3.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW. Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiatry. 2008;65:513. doi: 10.1001/archpsyc.65.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord. 2002;72:227–236. doi: 10.1016/S0165-0327(01)00413-X. [DOI] [PubMed] [Google Scholar]
- Spijker J, Bijl RV, De Graaf R, Nolen WA. Care utilization and outcome of DSM-III-R major depression in the general population: results from the Netherlands mental health survey and incidence study (NEMESIS) Acta Psychiatr Scand. 2001;104:19–24. doi: 10.1034/j.1600-0447.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- Andrews G, Titov N. Depression is very disabling. Lancet. 2007;370:808–809. doi: 10.1016/S0140-6736(07)61393-2. [DOI] [PubMed] [Google Scholar]
- Smit F, Cuijpers P, Oostenbrink J, Batelaan N, De Graaf R, Beekman A. Costs of nine common mental disorders: implications for curative and preventive psychiatry. J Ment Health Policy Econ. 2006;9:193–200. [PubMed] [Google Scholar]
- Wang PS, Simon G, Kessler RC. The economic burden of depression and the cost-effectiveness of treatment. Int J Methods Psychiatr Res. 2003;12:22–33. doi: 10.1002/mpr.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Van Straten A, Andersson G, Van Oppen P. Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies. J Consult Clin Psychol. 2008;76:909–922. doi: 10.1037/a0013075. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Van Straten A, Warmerdam L, Andersson G. Psychological treatment of depression: a meta-analytic database of randomized studies. BMC Psychiatry. 2008;8:36. doi: 10.1186/1471-244X-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bebbington P, Brugha T, Meltzer H, Jenkins R, Ceresa C, Farrell M, Lewis G. Neurotic disorders and the receipt of psychiatric treatment. Int Rev Psychiatry. 2003;15:108–114. doi: 10.1080/0954026021000046010. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch RJ, Laska EM, Leaf PJ, Manderscheid RW, Rosenheck RA, Walters EE, Wang PS. The prevalence and correlates of untreated serious mental illness. Health Serv Res. 2001;36:987–1007. [PMC free article] [PubMed] [Google Scholar]
- Moritz S, Schröder J, Meyer B, Hauschildt M. The more is needed, the less is wanted: attitudes toward face-to-face intervention among depressed patients undergoing online treatment. Depress Anxiety. 2013;30:157–167. doi: 10.1002/da.21988. [DOI] [PubMed] [Google Scholar]
- Schulz H, Barghaan D, Harfst T, Koch U. Psychotherapeutische Versorgung. Berlin: Gesundheitsberichterstattung des Bundes; 2008. [Google Scholar]
- Helbig S, Hähnel A, Weigel B, Hoyer J. Wartezeit für Psychotherapiepatienten–und wie sie zu nutzen ist: Waiting time in psychotherapy–and how to make use of it. Verhaltenstherapie. 2004;14:294–302. doi: 10.1159/000082839. [DOI] [Google Scholar]
- Barkham M, Mullin T, Leach C, Stiles WB, Lucock M. Stability of the CORE-OM and the BDI-I prior to therapy: evidence from routine practice. Psychol Psychother Theory Res Pract. 2007;80:269–278. doi: 10.1348/147608306X148048. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Walters HM, Vittengl JR, Krebaum S, Jarrett RB. Which depressive symptoms remain after response to cognitive therapy of depression and predict relapse and recurrence? J Affect Disord. 2010;123:181–187. doi: 10.1016/j.jad.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bockting CL, Spinhoven P, Koeter MWJ, Wouters LF, Schene AH. for the Depression Evaluation Longitudinal Therapy Assessment (DELTA) Study Group. Prediction of recurrence in recurrent depression and the influence of consecutive episodes on vulnerability for depression: a 2-year prospective study. J Clin Psychiatry. 2006;67:747–755. doi: 10.4088/JCP.v67n0508. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Moderators of continuation phase cognitive therapy’s effects on relapse, recurrence, remission, and recovery from depression. Behav Res Ther. 2010;48:449–458. doi: 10.1016/j.brat.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burcusa SL, Iacono WG. Risk for recurrence in depression. Clin Psychol Rev. 2007;27:959–985. doi: 10.1016/j.cpr.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spek V, Cuijpers P, Nyklícek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med. 2007;37:319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- Gregory RJ, Schwer Canning S, Lee TW, Wise JC. Cognitive bibliotherapy for depression: a meta-analysis. Prof Psychol: Res Pract. 2004;35:275–280. [Google Scholar]
- McKendree-Smith NL, Floyd M, Scogin FR. Self-administered treatments for depression: a review. J Clin Psychol. 2003;59:275–288. doi: 10.1002/jclp.10129. [DOI] [PubMed] [Google Scholar]
- Kok RN, Van Straten A, Beekman ATF, Bosmans JE, De Neef M, Cuijpers P. Effectiveness and cost-effectiveness of web-based treatment for phobic outpatients on a waiting list for psychotherapy: protocol of a randomised controlled trial. BMC Psychiatry. 2012;12:131. doi: 10.1186/1471-244X-12-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J, Ebert D, Lehr D, Berking M, Baumeister H. Internet based cognitive behavioral interventions: state of the art and implementation possibilities in rehabilitation: article in German. Rehabilitation. 2013;52:155–163. doi: 10.1055/s-0033-1343491. [DOI] [PubMed] [Google Scholar]
- Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N, Baune BT. Computer therapy for the anxiety and depressive disorders is effective acceptable and practical health care: a meta-analysis. PLoS ONE. 2010;5:e13196. doi: 10.1371/journal.pone.0013196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn Behav Ther. 2009;38:196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- Ebert D, Tarnowski T, Gollwitzer M, Sieland B, Berking M. A transdiagnostic internet-based maintenance treatment enhances the stability of outcome after inpatient cognitive behavioral therapy: a randomized controlled trial. Psychother Psychosom. 2013;82:246–256. doi: 10.1159/000345967. [DOI] [PubMed] [Google Scholar]
- Ebert DD, Gollwitzer M, Sieland B, Berking M. Who profits from a Transdiagnostic Internet-based maintenance Treatment? Who does not? Moderators of Outcome from a Randomized Controlled Trial. In press.
- Andersson G. Using the internet to provide cognitive behaviour therapy. Behav Res Ther. 2009;47:175–180. doi: 10.1016/j.brat.2009.01.010. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Marks IM, Van Straten A, Cavanagh K, Gega L, Andersson G. Computer‒aided psychotherapy for anxiety disorders: a meta‒analytic review. Cogn Behav Ther. 2009;38:66–82. doi: 10.1080/16506070802694776. [DOI] [PubMed] [Google Scholar]
- Kenter R, Warmerdam L, Brouwer-Dudokdewit C, Cuijpers P, Van Straten A. Guided online treatment in routine mental health care: an observational study on uptake, drop-out and effects. BMC Psychiatry. 2013;13:43. doi: 10.1186/1471-244X-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruwaard J, Schrieken B, Schrijver M, Broeksteeg J, Dekker J, Vermeulen H, Lange A. Standardized web-based cognitive behavioural therapy of mild to moderate depression: a randomized controlled trial with a long-term follow-up. Cogn Behav Ther. 2009;38:206–221. doi: 10.1080/16506070802408086. [DOI] [PubMed] [Google Scholar]
- Warmerdam L, Van Straten A, Jongsma J, Twisk J, Cuijpers P. Online cognitive behavioral therapy and problem-solving therapy for depressive symptoms: exploring mechanisms of change. J Behav Ther Exp Psychiatry. 2010;41:64–70. doi: 10.1016/j.jbtep.2009.10.003. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Van Straten A, Warmerdam L. Problem solving therapies for depression: a meta-analysis. Eur Psychiatry. 2007;22:9–15. doi: 10.1016/j.eurpsy.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Van Straten A, Cuijpers P, Smits N. Effectiveness of a web-based self-help intervention for symptoms of depression, anxiety, and stress: randomized controlled trial. J Med Internet Res. 2008;10:e7. doi: 10.2196/jmir.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Huibers M, Ebert DD, Koole SL, Andersson G. How much psychotherapy is needed to treat depression? A metaregression analysis. J Affect Disord. 2013;149:1–13. doi: 10.1016/j.jad.2013.02.030. [DOI] [PubMed] [Google Scholar]
- Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev. 2012;32:329–342. doi: 10.1016/j.cpr.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Johansson R, Andersson G. Internet-based psychological treatments for depression. Expert Rev Neurotherapeutics. 2012;12:861–870. doi: 10.1586/ern.12.63. [DOI] [PubMed] [Google Scholar]
- Berger T, Hämmerli K, Gubser N, Andersson G, Caspar F. Internet-based treatment of depression: a randomized controlled trial comparing guided with unguided self-help. Cogn Behav Ther. 2011;40:251–266. doi: 10.1080/16506073.2011.616531. [DOI] [PubMed] [Google Scholar]
- Camerini L, Schulz PJ. Effects of functional interactivity on patients’ knowledge, empowerment, and health outcomes: an experimental model-driven evaluation of a web-based intervention. J Med Internet Res. 2012;14:e105. doi: 10.2196/jmir.1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurling R, Fairley BW, Dias MB. Internet-based exercise intervention systems: are more interactive designs better? Psychol Health. 2006;21:757–772. doi: 10.1080/14768320600603257. [DOI] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Markowitz JC, Ninan PT, Kornstein S, Manber R, Thase ME, Kocsis JH, Keller MB. The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Soc Biol Psychiatry. 2003;54:573–583. doi: 10.1016/S0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Knesevich JW, Biggs JT, Clayton PJ, Ziegler VE. Validity of the Hamilton rating scale for depression. Br J Psychiatry. 1977;131:49–52. doi: 10.1192/bjp.131.1.49. [DOI] [PubMed] [Google Scholar]
- Miller IW, Bishop S, Norman WH, Maddever H. The modified Hamilton rating scale for depression: reliability and validity. Psychiatry Res. 1984;14:131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The inventory of depressive symptomatology (IDS): psychometric properties. Psychol Med. 1996;26:477. doi: 10.1017/S0033291700035558. [DOI] [PubMed] [Google Scholar]
- Trivedi M, Rush A, Ibrahim H, Carmody T, Biggs M, Suppes T, Crismon M, Shores-Wilson K, Toprac M, Dennehy E, Witte B, Kasher T. The inventory of depressive symptomatology, clinician rating (IDS-C) and self-report (IDS-SR), and the quick inventory of depressive symptomatology, clinician rating (QIDS-C) and self-report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychological medicine. 2004;34:73–82. doi: 10.1017/S0033291703001107. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders IV-TR. Washington DC: American Psychiatric Association; 2000. [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:1–7. [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9 validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The EuroQol Group. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- von der Graf Schulenburg J, Claes C, Greiner W, Uber A. Die deutsche version des EuroQol-Fragebogens: the German version of the EuroQol questionnaire. Zeitschrift für Gesundheitswissenschaften. 1998;6:3–20. [Google Scholar]
- D’Zurilla TJ, Nezu AM. MA: Social Problem-Solving Inventory-Revised (SPSI-R) New York: MHS; 2002. [Google Scholar]
- Manos RC, Kanter JW, Luo W. The behavioral activation for depression scale–short form: development and validation. Behav Ther. 2011;42:726–739. doi: 10.1016/j.beth.2011.04.004. [DOI] [PubMed] [Google Scholar]
- Berle D, Starcevic V, Moses K, Hannan A, Milicevic D, Sammut P. Preliminary validation of an ultra-brief version of the Penn State worry questionnaire. Clin Psychol Psychother. 2011;18:339–346. doi: 10.1002/cpp.724. [DOI] [PubMed] [Google Scholar]
- Schulte D. Messung der Therapieerwartung und Therapieevaluation von Patienten (PATHEV): patient questionnaire on therapy expectation and evaluation (PATHEV) Z Klin Psychol Psychother. 2005;34:176–187. doi: 10.1026/1616-3443.34.3.176. [DOI] [Google Scholar]
- Bassler M, Potratz B, Krauthauser H. Der “Helping Alliance Questionnaire” (HAQ) von Luborsky: Möglichkeiten zur Evaluation des therapeutischen Prozesses von stationärer Psychotherapie. Psychotherapeut. 1995;40:23–32. [Google Scholar]
- Luborsky L, Barber JP, Siqueland L, Johnson S, Najavits LM, Frank A, Daley D. The revised helping alliance questionnaire (HAQ-II): psychometric properties. J Psychother Pract Res. 1996;5:260–271. [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Kraemer HC, Sackeim HA, Fava M, Trivedi MH, Frank E, Ninan PT, Thase ME, Gelenberg AJ, Kupfer DJ, Regier DA, Rosenbaum JF, Ray O, Schatzberg AF. Report by the ACNP task force on response and remission in major depressive disorder. Neuropsychopharmacology. 2006;31:1841–1853. doi: 10.1038/sj.npp.1301131. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychol Methods. 1997;2:64–78. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, New York: Erlbaum; 1988. [Google Scholar]
- Roland M, Torgerson DJ. Understanding controlled trials: what are pragmatic trials? BMJ. 1998;316:285. doi: 10.1136/bmj.316.7127.285. [DOI] [PMC free article] [PubMed] [Google Scholar]


