Abstract
In dentistry, the term 'fusion' is used to describe a developmental disorder of dental hard tissues. In the permanent dentition, fusion of a normal tooth and a supernumerary tooth usually involves the incisors or canines. However, a few cases of fusion involving premolars have also been reported to date. We present a rare case in which fusion of the maxillary left second premolar and a supernumerary tooth in a 13-year-old girl was diagnosed using cone beam computed tomography (CBCT, Alphard-3030, Asahi Roentgen Ind. Co., Ltd.). The tooth was bicuspidized after routine nonsurgical root canal treatment, and the separated teeth underwent appropriate restoration procedures. The second premolar and supernumerary tooth remained asymptomatic without any signs of inflammation after a follow-up period of 9 years. Identification of anatomical anomalies is important for treatment in cases involving fusion with supernumerary tooth, and therefore the microscopic examinations and CBCT are essential for the diagnosis. Fused teeth can be effectively managed by the comprehensive treatment which includes both endodontic and periodontal procedures.
Keywords: Bicuspidization, Cone-beam computed tomography, Fused teeth, Supernumerary tooth
Introduction
Fusion and gemination are developmental disorders of dental hard tissues that occur because of the union of two or more developing teeth. Knezevic et al. examined over 3,500 models in order to assess the prevalence of twinned teeth (fusion and gemination).1 They observed twinned teeth in less than 0.5% of the cases, and 57% of these cases showed fusion and 43% showed germination.1
Gemination occurs due to invagination of the developing dental organ, which results in one tooth being split into two. A geminated tooth has a bifid crown, a single root, and an enlarged pulp chamber. Tooth fusion, on the other hand, is caused by the union of two discrete tooth germs to form a single tooth. Fused teeth are united by dental hard tissue and show separate pulp cavities.2 The etiology of fusion is still uncertain. However, developmental aberrations during morpho-differentiation of the tooth bud, local metabolic disturbances, and crowding of tooth germs during their development could be important etiological factors. Hereditary and racial differences could also be the contributing factors.3
Fusion of permanent and supernumerary tooth usually occurs in the maxillary anterior region. However, fusion involving premolars is rarely reported. The purpose of this article is to report a rare case involving fusion of the maxillary second premolar with a supernumerary tooth and its treatment using a combination of endodontic and prosthetic procedures.
Case Report
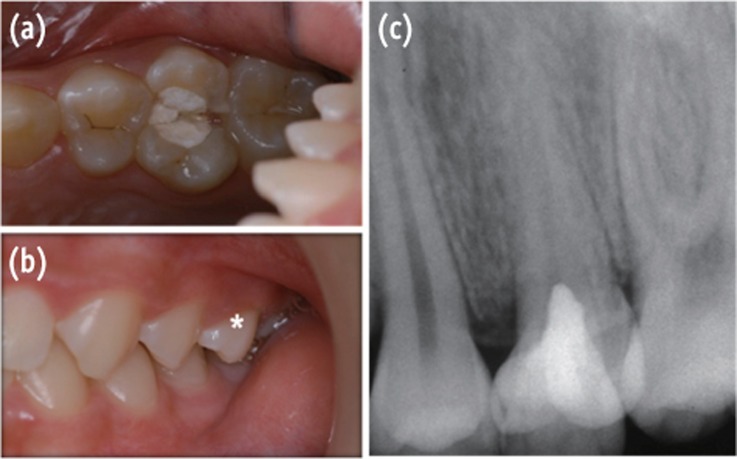
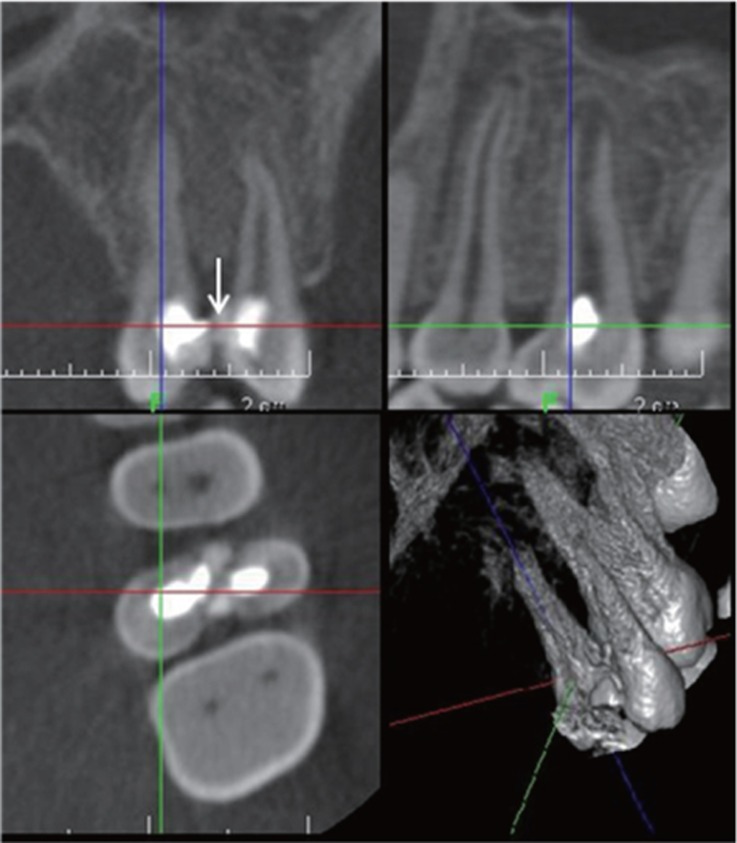
A 13-year-old girl was referred to the Department of Conservative Dentistry at Kyung Hee University Dental Hospital with the chief complaint of pain in the maxillary left second premolar (#25), which had undergone pulpotomy. (Figures 1a and 1b). The patient's medical history was not significant. A clinical examination showed the temporary filling in the access cavity of #25. The tooth was tender to percussion and biting. Its crown morphology was abnormal and a supernumerary tooth was located in close proximity to its palatal surface (Figure 1c). A cone beam computed tomography (CBCT, Alphard-3030, Asahi Roentgen Ind. Co., Ltd., Kyoto, Japan) image showed the continuity between the supernumerary tooth and the second premolar (white arrow), and the separation between the pulp cavities of each tooth (Figure 2). On the basis of these clinical and radiographic findings, fusion of the maxillary second premolar with the supernumerary tooth was diagnosed.
Figure 1.
(a) Intraoral photograph showing fusion between the maxillary left second premolar and a supernumerary tooth; (b) Asterisk indicates the fused teeth placed slightly buccally; (c) Periapical radiograph showing abnormal crown morphology of the maxillary left second premolar with a supernumerary tooth.
Figure 2.
Cone beam computed tomography images showing the continuity between the supernumerary tooth and the second premolar (white arrow) and complete separation of the pulp cavities of each tooth.
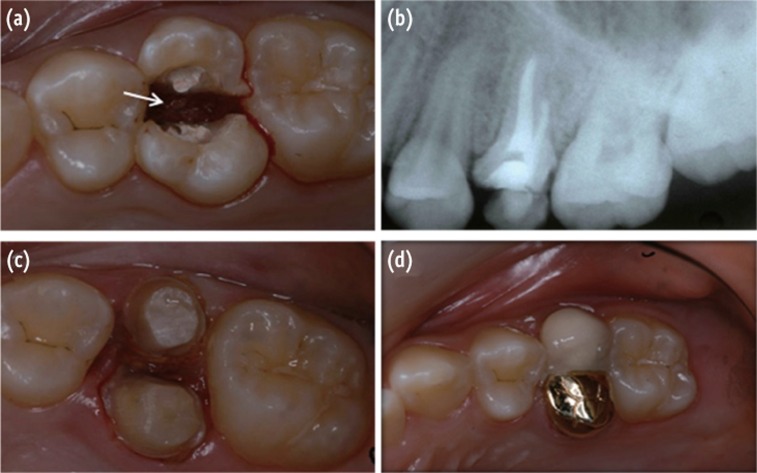
Root canal treatment and subsequent bicuspidization were planned. Microscopic observation (OPMI Pico, Carl Zeiss, Oberkochen, Germany) confirmed the diagnosis of fusion. The canals of both teeth were prepared using stainless-steel hand files (K-File, Dentsply Maillefer, Ballagiues, Swiss) with the step back technique. The canals of the premolar and the supernumerary tooth were enlarged to the sizes of a no. 40 and 45 files, respectively. During the preparation, the canals were irrigated with saline and 2.5% sodium hypochlorite. After two weeks, the tooth was asymptomatic, and obturation was performed using the lateral condensation technique with gutta percha cones and resin-based sealer (AH26, Dentsply Maillefer) (Figure 3b). After completion of root canal treatment, bicuspidization of the fused crown was performed using a diamond bur (TR12, MANI, Tochigi, Japan), followed by electro-cauterization (Figure 3a). A splint-type temporary restoration was inserted a week after the operation.
Figure 3.
(a) A white arrow indicates electro-cauterization of the interdental gingiva between fused teeth; (b) Periapical radiographs obtained after nonsurgical root canal treatment; (c) Tooth preparation after bicuspidization; (d) After double crown placement.
Periodontal healing was assessed at 5 weeks after the operation, and each separated crown was subsequently rebuilt with a composite resin core (LuxaCore, DMG-AMERICA, Englewood, NJ, USA). The second premolar and the supernumerary tooth underwent preparation to receive a metal ceramic crown and a gold crown, followed by provisional restorations (Figure 3c). After checking the proximal contacts and performing occlusal adjustments, two separate crowns were cemented on the buccal and palatal halves of each tooth by using resin-modified glass ionomer luting cement (GC FujiCEM 2, GC, Tokyo, Japan) (Figure 3d).
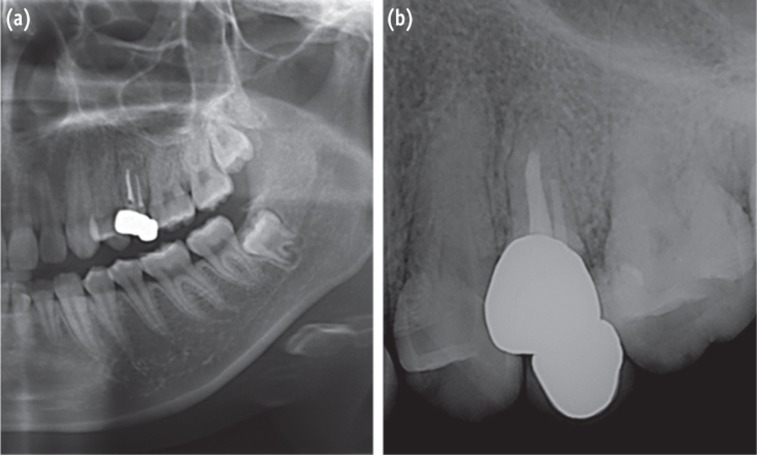
Nine years later, we recalled the patient and examined the teeth. The bicuspidized teeth remained asymptomatic and did not show any signs of periapical and periodontal inflammation (Figures 4a and 4b). Although a small gap existed between the teeth, food impaction in that region was minimized by using the dental floss. Follow-up examinations indicated that the treatment had successfully restored the function. However, further follow-up examinations are necessary to establish long-term prognosis.
Figure 4.
(a) Postoperative panoramic radiograph obtained after 9 years; (b) Postoperative periapical radiograph shows an uneventful healing state.
Discussion
Fusion of teeth is more common in the deciduous dentition. The frequency of fusion of permanent and supernumerary teeth is 0.1%. Most of these cases involve the incisors and canines.4,5,6,7 The fusion of supernumerary and posterior tooth has relatively rare occurrence with a prevalence of 0.1 to 0.5%.3 The present case is a rarity since the fusion occurred in the posterior region and involved the union of a second premolar and a supernumerary tooth.
In cases involving twinned teeth, it is clinically difficult to differentiate between fusion and gemination due to their similar morphological characteristics. Thus, radiographic examinations are essential for the diagnosis. However, the conventional intraoral periapical views have a limited scope as they produce superimposed 2-dimensional images of a 3-dimensional object. Conventional multidetector computed tomography (CT) imaging was introduced in dental practice in 1990.8 More recently, a new diagnostic tool, CBCT, is being increasingly used in endodontics. Matherne et al. reported that CBCT imaging is an effective tool for identifying root canal systems and tooth morphology.9 According to Song et al., geminated teeth have a single pulp canal and root, whereas fused teeth have independent pulp canals with combined dentin.10 In the present case, CBCT images (Figure 2) revealed two separate pulp chambers with the crowns combined at the level of the dentin. On the basis of these results, we diagnosed this as a case of fusion.
Bicuspidization could be a treatment option in cases of teeth fusion. The possible treatment options suggested in previous studies include bicuspidization of the tooth after completion of endodontic treatment for the fused tooth, extraction of the unwanted part, and orthodontic treatment for alignment.7,11,12 In the present case, the premolar and supernumerary tooth were similar in size and length, which made it difficult to identify the supernumerary tooth. We considered the palatally located tooth to be the supernumerary tooth on the basis of the findings reported previously. According to Liu et al., a total of 33 out of 626 supernumerary teeth including fused teeth were located at the premolar region (18 in the maxillary and 15 in the mandibular premolar region), and all supernumerary teeth were located palatal to the dental arch.13 In our case, the supernumerary tooth and the premolar showed functionally normal occlusion to the opposing teeth. Therefore, bicuspidization was performed instead of extraction. The fused teeth were separated into two crowns. The fused dentin was dissected immediately after the completion of the root canal treatment since the fused anatomical structure was very thin. Electro-cauterization of the furcation area was performed. The bicuspidization procedure enhanced access to the furcation region. Each separated crown was rehabilitated using buccal and palatal double crowns. In order to enable maintenance with dental floss, the double crowns were cemented without splinting.
The bicuspidized teeth remained asymptomatic throughout the 9-year follow-up period. Food impaction occurred occasionally between the double crowns but it was easily cleaned by the use of dental floss. The long-term prognosis of this case is dependent on the periodontal management of the space between the double crowns. Good plaque control and regular periodontal supportive care will be required to maintain the health of the periodontium in that region. Additional studies are required to compare the patient satisfaction associated with the double crown technique for fused teeth against other treatment modalities that require extraction of the supernumerary tooth followed by orthodontic alignment or placement of a dental implant.
Conclusions
It is important to be aware of anatomical anomalies in the management of fused teeth. Meticulous clinical and radiographic examinations are required. Microscopic examinations and CBCT can facilitate diagnosis and planning of treatment in such cases. Fused teeth can be successfully managed by comprehensive treatment protocols which include endodontic and periodontal procedures.
Acknowledgments
This research was supported by the Basic Science Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (KRF-20100023448).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Knezević A, Travan S, Tarle Z, Sutalo J, Janković B, Ciglar I. Double tooth. Coll Antropol. 2002;26:667–672. [PubMed] [Google Scholar]
- 2.Hernandez-Guisado JM, Torres-Lagares D, Infante-Cossio P, Gutierrez-Perez JL. Dental gemination: report of case. Med Oral. 2002;7:231–236. [PubMed] [Google Scholar]
- 3.Tsesis I, Steinbock N, Rosenberg E, Kaufman AY. Endodontic treatment of developmental anomalies in posterior teeth: treatment of geminated/fused teeth-report of two cases. Int Endod J. 2003;36:372–379. doi: 10.1046/j.1365-2591.2003.00666.x. [DOI] [PubMed] [Google Scholar]
- 4.Maréchaux SC. The treatment of fusion of a maxillary central incisor and a supernumerary: report of a case. ASDC J Dent Child. 1984;51:196–199. [PubMed] [Google Scholar]
- 5.de Siqueira VC, Braga TL, Martins MA, Raitz R, Martins MD. Dental fusion and dens evaginatus in the permanent dentition: literature review and clinical case report with conservative treatment. J Dent Child (Chic) 2004;71:69–72. [PubMed] [Google Scholar]
- 6.Karacay S, Guven G, Koymen R. Management of a fused central incisor in association with a macrodont lateral incisor: a case report. Pediatr Dent. 2006;28:336–340. [PubMed] [Google Scholar]
- 7.Cetinbas T, Halil S, Akcam MO, Sari S, Cetiner S. Hemisection of a fused tooth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e120–e124. doi: 10.1016/j.tripleo.2007.03.029. [DOI] [PubMed] [Google Scholar]
- 8.Tachibana H, Matsumoto K. Applicability of X-ray computerized tomography in endodontics. Endod Dent Traumatol. 1990;6:16–20. doi: 10.1111/j.1600-9657.1990.tb00381.x. [DOI] [PubMed] [Google Scholar]
- 9.Matherne RP, Angelopoulos C, Kulild JC, Tira D. Use of cone-beam computed tomography to identify root canal systems in vitro. J Endod. 2008;34:87–89. doi: 10.1016/j.joen.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 10.Song CK, Chang HS, Min KS. Endodontic management of supernumerary tooth fused with maxillary first molar by using cone-beam computed tomography. J Endod. 2010;36:1901–1904. doi: 10.1016/j.joen.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 11.Simratvir M, Prabhakar M. Clinical management of a unique case of fusion between supernumerary canine and maxillary first premolar. J Calif Dent Assoc. 2011;39:885–889. [PubMed] [Google Scholar]
- 12.Hülsmann M, Bahr R, Grohmann U. Hemisection and vital treatment of a fused tooth-literature review and case report. Endod Dent Traumatol. 1997;13:253–258. doi: 10.1111/j.1600-9657.1997.tb00051.x. [DOI] [PubMed] [Google Scholar]
- 13.Liu DG, Zhang WL, Zhang ZY, Wu YT, Ma XC. Three-dimensional evaluations of supernumerary teeth using cone-beam computed tomography for 487 case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:403–411. doi: 10.1016/j.tripleo.2006.03.026. [DOI] [PubMed] [Google Scholar]