Abstract
Clopidogrel, a second generation thienopyridine has been the mainstay of ACS (Acute Coronary Syndrome) treatment for more than a decade. Clopidogrel Resistance has been associated with increased mortality in ACS patients with an increase in number of Stent Thrombosis. This review article tries to find out the causes of Clopidogrel Resistance, the main factors involving it, Laboratory evaluation of Clopidogrel Resistance. The overall incidence of Clopidogrel Resistance across the Globe & India has also been considered. The article also discusses the clinical significance of Clopidogrel Resistance & its relationship with adverse cardiovascular events. This review ends with the probable solutions to Clopidogrel Resistance & the new generation of antiplatelets which can be used for the same.
Keywords: Clopidogrel resistance, Platelet reactivity, Stent thrombosis, Prasugrel, Ticagrelor
1. Introduction
Clopidogrel inhibits platelet activation and inhibition by selectively and irreversibly blocking P2Y12 receptor.1 The CAPRIE (Clopidogrel versus Aspirin in Patients at risk of Ischemic Events) study demonstrated the benefit of using clopidogrel + Aspirin compared to Aspirin alone in selected patients due to the different receptor and pathway of inhibition.2 Combined therapy of Clopidogrel with Aspirin is considered in all patients with acute coronary syndromes requiring Percutaneous Intervention (PCI).3 The benefit of combined therapy in major trials was also associated with adverse ischemic events including stent thrombosis. The previous trials were focused on the clinical events without the laboratory evaluation of platelet function. Laboratory assessment of non-responsiveness to clopidogrel was shown to be associated with adverse ischemic events.
2. Mechanism of action
Clopidogrel acts by inhibiting ADP induced platelet aggregation. It also inhibits collagen and thrombin induced platelet aggregation which can be overcome by increased concentration of these agonists. Clopidogrel is rapidly absorbed from the intestine and converted to a short lived active metabolite by hepatic cytochrome P450 enzymes (CYP3A4, CYP3A5, and CYP2C19). The active metabolite permanently binds to the P2Y12 receptor via disulphide bridges and there is inhibition of platelet activation.4
3. Clopidogrel resistance
Clopidogrel Resistance is defined as the failure of the molecule to inhibit the target of its action. Clopidogrel resistance is best demonstrated by the evidence of residual post treatment P2Y12 activity by measuring ADP induced platelet aggregation before and after treatment. No single receptor signaling pathway mediated platelet activation is responsible for its activity. Therefore a single treatment strategy may not be sufficient to overcome clopidogrel resistance.5
4. Laboratory evaluation of clopidogrel responsiveness
A standardized method to evaluate in-vivo platelet response is still lacking. Clopidogrel inhibits one of the two ADP receptors; ex-vivo measurement of ADP induced platelet aggregation by light transmittance aggregometry is the most commonly used “Gold standard” method to evaluate clopidogrel responsiveness.6
Lately it was suggested that since clopidogrel induced platelet disaggregation was better demonstrated by measuring late platelet aggregation at 6 min after stimulation with ADP rather than maximum aggregation. Flow cytometric measurements of expression of GpIIb/IIIa receptor and p selectin expression after ADP stimulation can also identify clopidogrel nonresponsiveness. In addition, measurements of ADP induced fibrin clot strength is measured by whole blood throomboelastography and the verify Now P2Y12 receptor assay using ADP as agonist. The PFA-100 method using collagen ADP based cartridges and whole blood aggregometry are associated with inconsistent estimates of platelet reactivity to ADP. The phosphorylation state of vasodilator stimulated phosphoprotein is a specific intracellular marker for residual P2Y12 receptor reactivity in patients treated with clopidogrel, but the method is difficult.7
5. Clopidogrel resistance & time of treatment
The prevalence of clopidogrel resistance in various studies was 5%–44%.4 Refer to Table 1.
Table 1.
Clopidogrel resistance world wide data.
| Investigators | Number of patients | Clopidogrel loading dose | Resistance |
|---|---|---|---|
| Jaremo et al (J Invest Med.2002;252:233) | 18 | 300 | 28% |
| Gurbel et al (Circulation 2003;107:2908) | 92 | 300 | 31–35% |
| Muller et al (Thromb Haemost 2003;89:783) | 105 | 600 | 5–11% |
| Mobley et al (Am J Cardiol 2004;93:456) | 50 | 300 | 30% |
| Lepantalo et al (Eur Heart J 2004;25–476) | 50 | 300 | 40% |
| Angiolillo et al (Thromb Res 2005;115:101) | 48 | 300 | 44% |
| Matetzky et al (Circulation 2004;109:3171) | 60 | 300 | 25% |
| Dzieweierz (Kardiol Pol 2005;62:108) | 31 | 300 | 23% |
| Gurbel et al (J Am Coll Cardiol 2005;45:1392) | 192 | 300/600 | 8–32% |
| Lev et al (J Am Coll Cardiol 2006;47:27) | 150 | 300 | 24% |
| 5–44% |
Data adapted from: Gurbel PA, Tantry US. Clopidogrel Resistance? Thromb Res. 2007; 120(3):311–21. Epub 2006 Nov 14.
Increasing the loading dose of clopidogrel to 600 mg is helpful in reducing resistance. Response variability to treatment with clopidogrel was seen in patients who were on clopidogrel post PCI. If the pre and post treatment ADP induced platelet aggregation was <10%, these patients were defined as “Clopidogrel Resistant”.8 A subgroup of patients had more platelet aggregation post Percutaneous Intervention (PCI) than before they were defined as “Heightened Platelet Reactivity to ADP”.9
6. Relation of clopidogrel resistance to adverse clinical events
The data linking clopidogrel resistance to clinical events are limited. Matetzky et al studied clopidogrel responsiveness in patients undergoing Stenting for ST elevated MI and found that patients who exhibited the highest quartile of ADP induced aggregation had a 40% probability of recurrent cardiovascular event in 6 months. Their study concluded that upto 25% STEMI (ST elevated Myocardial Infarction) patients would suffer from Stent Thrombosis due to clopidogrel Resistance.10
In PREPARE POST STENTING study (Platelet Reactivity in Patients and Recurrent Events POST STENTING), patients suffering from recurrent ischemic events within 6 months of Stenting had a high platelet reactivity to ADP than those without ischemic complications.9
In the CLEAR PLATELETS (Clopidogrel Loading with Eptifibatide to Arrest PLATELET reactivity) and CLEAR PLATELETS 1b studies, a 600 mg clopidogrel loading dose used to treat patients undergoing elective Stenting was associated with superior early platelet inhibition compared to a loading dose of 300 mg and this inhibition was associated with decrease in myocardial necrosis and inflammatory markers.11
These findings suggest that high platelet reactivity despite currently recommended antiplatelet therapy is a risk factor for ischemia in patients undergoing PCI.
7. Clopidogrel resistance in India
There is limited number of studies conducted on clopidogrel resistance in India. The results of these studies indicate that prevalence of clopidogrel resistance in India is in line with global scenario.
In a trial with 144 ACS (Acute Coronary Syndromes) Patients in Kolkata by Guha et al clopidogrel resistance was seen in 12.5% of patients and 19.44% patients were poor responders.12
Another study conducted by Kumar, Saran et al in 39 ACS patients showed 2.54% patients as clopidogrel resistant & 12.70% patients were termed as clopidogrel Semi resistant.13
A study conducted by Kar, Meena et al in 100 CAD Patients showed 19% patients as semi resistant & 13% were found to be poor responders.14
8. Mechanisms of clopidogrel resistance
Differences in intestinal absorption, hepatic conversion of active metabolite through cytochrome CYP2C19, ABC1 activity and platelet receptor polymorphisms have been suggested. Higher loading dose of clopidogrel 600 mg was associated with increased inhibition of ex-vivo ADP induced platelet aggregation in patients undergoing PCI and decreased prevalence of non-responders.CYP-450 (particularly CYP2C19, CYP3A4 and CYP3A5) enzymes play a vital role in generating the active metabolite of clopidogrel hence variation in production of those enzymes may be responsible for clopidogrel resistance.15
Genetic polymorphism of ABC1 as well as GpIIb-IIIa, GPIa-IIa and P2Y12 receptors also causes clopidogrel resistance. Patients with Diabetes exhibit heightened platelet reactivity and this may further aggravate non responsiveness to clopidogrel.5
Insufficient metabolite generation secondary to limitations in intestinal absorption, Drug-drug interaction at CYP 3A4 or genetic polymorphism of CYP isoenzymes are seen as the primary explanations for resistance rather than genetic polymorphism of platelet receptors or intracellular signaling mechanisms. It may be relevant in those patients who remain resistant and with high platelet reactivity to ADP even after high dosing strategies.
9. Management of clopidogrel resistance
9.1. Higher doses of clopidogrel
As mentioned earlier, various studies have shown that 600 mg dose was associated with higher level of platelet inhibition, lower mean post treatment reactivity of ADP than the 300 mg loading dose.
The CURRENT OASIS-7 (Double-dose versus standard-dose clopidogrel and high dose versus low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes) trial randomized 25,087 patients with unstable angina or acute MI to a high dose regimen (600 mg loading dose of clopidogrel, followed by 150 mg per day for 1 week) or the standard regimen (300 mg on the first day followed by 75 mg/day) showed benefit of 600 mg clopidogrel in ACS + PCI population but the primary end point was mainly driven by MI alone. The Current OASIS trial however showed a significant reduction in Definite Stent Thrombosis (58 [0.7%] vs. 111 [1.3%]; 0.54 [0.39–0.74], p = 0.0001).16
GRAVITAS (Gauging Responsiveness with A Verify Now assay—Impact on Thrombosis And Safety) trial, the first large-scale clinical trial, designed to examine whether adjustment of clopidogrel therapy, on the basis of platelet function testing using a point-of-care assay, safely improves outcome after PCI with drug-eluting stents in clopidogrel resistant patients, did not show any superiority of 150 mg vs. 75 mg of clopidogrel.17
In the CLEAR PLATELETS (Clopidogrel Loading with Eptifibatide to Arrest the Reactivity of Platelets) study; 600 mg loading dose was associated with a superior pharmacodynamic antiplatelet profile compared to a 300 mg clopidogrel loading dose, in the absence of a GPIIb/IIIa (Glycoprotein IIb/IIIa) inhibitor.11
However, in the recent ISARCHOICE (Intracoronary Stenting and Antithrombotic Regimen: Choice Between 3 High Oral doses for Immediate Clopidogrel Effect) Study, there was a ceiling effect in unchanged clopidogrel and clopidogrel metabolite levels and platelet inhibition with the 600 mg loading dose, and no significant additional effect was seen with the 900 mg loading dose.18
Recently ACC/AHA Guidelines recommended a Class IIb recommendation that “In patients in whom sub acute thrombosis may be catastrophic or lethal, platelet aggregation studies may be considered and the dose of clopidogrel needs to be increased to 150 mg per day if less than 50% inhibition of platelet aggregation is demonstrated.”19
10. New P2Y12 receptor antagonists: Prasugrel
Prasugrel is a novel thienopyridine introduced for the treatment of acute coronary syndromes.
Jernberg & Wallentine et al published that Prasugrel demonstrated higher and more rapid inhibition of platelet aggregation and a greater reduction of pharmacodynamic non-responders, compared with the standard clopidogrel dose of 75 mg.20
In another study Alexopoulos et al demonstrated in their trial that in ACS patients who are on HTPR (high on treatment platelet reactivity) after PCI (Percutaneous Intervention) Prasugrel is more effective compared to high dose clopidogrel in reducing platelet reactivity, particularly in CYP2C19*2 carriers.21
In recent ACAPULCO (Prasugrel Compared with High Dose Clopidogrel in ACS) study by Montalescot et al reinforced this observation by proving prasugrel's superiority in platelet inhibition compared to high dose clopidogrel MD 150 mg or 900 mg LD.22
11. Newer P2Y12 receptor antagonists: Ticagrelor & cangrelor
Ticagrelor an oral, direct-acting, reversible, P2Y12 receptor antagonist, was associated with less ischemic event occurrence than clopidogrel in patients with acute coronary syndromes in the Platelet Inhibition and Patient Outcomes (PLATO) trial.23
In RESPOND study the response to ticagrelor in clopidogrel non-responders in stable CAD patients was studied in detail.24 In ticagrelor treated patients, platelet reactivity was below the cut-off points previously associated with ischemic risk—measured by LTA (Light Transmittance Aggregometry), Verify Now P2Y12 assay, and VASP-P (Vasodilator Stimulated Phosphoprotein phosphorylation)—in 98%–100% of patients versus 44%–76% of patients after clopidogrel Therapy (Figure below).
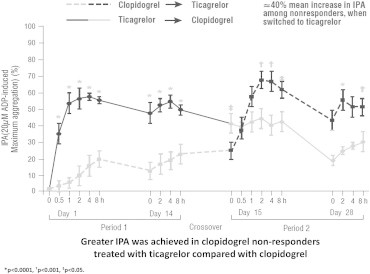
The study also demonstrated that ticagrelor therapy was associated with greater platelet inhibition compared with clopidogrel treatment in both clopidogrel responders and no responders. It was found that the antiplatelet effect of ticagrelor was not influenced by clopidogrel response status. It was clearly evident that ticagrelor overcame clopidogrel resistance. Nearly all patients during ticagrelor therapy, irrespective of clopidogrel response status, had platelet reactivity below the cut-offs associated with ischemic risk determined by all assays.
Switching from clopidogrel to ticagrelor not only overcame clopidogrel nonresponsiveness (mean increase in IPA of around 40% in non-responders) but also provided additional platelet inhibition in clopidogrel responders (around 20% increase in IPA).
Cangrelor, another reversible non-thienopyridine ADP receptor P2Y12 inhibitor, administered intravenously, was assessed in the CHAMPION-PLATFORM74 and the CHAMPION-PCI trials. Efficacy of Cangrelor in clopidogrel resistant patients is yet to be proved.25
12. Conclusion
Clopidogrel was a gold standard drug and has been used in combination with aspirin in patients with acute coronary syndrome. In recent studies it has been shown that high on platelet reactivity due to clopidogrel resistance was associated with adverse thrombotic events including stent thrombosis. The primary reason is suboptimal generation of the active metabolite due to individual variability in intestinal absorption, drug-drug interaction and polymorphism in the CYP isoenzymes. Clopidogrel resistance has been documented in the range of 5–44% across the world including India. Methods to identify clopidogrel resistance are not standardized and not freely available in India. One needs to confirm clopidogrel resistance especially in high risk ACS patients (e.g. Diabetic patients, Renal Compromised patients, Patients with prior h/o Stroke, TIA etc). Use of higher loading doses of clopidogrel (600 mg) or more potent P2Y12 receptor agents (e.g. prasugrel, ticagrelor, cangrelor) are the strategies to overcome clopidogrel resistance.
Conflicts of interest
The author has none to declare.
References
- 1.Ding Z., Kim S., Dorsam R.T., Jin J., Kunapuli S.P. Inactivation of the human P2Y12 receptor by thiol reagents requires interaction with both extracellular cysteine residues, Cys17 and Cys270. Blood. 2003;101:3908–3914. doi: 10.1182/blood-2002-10-3027. [DOI] [PubMed] [Google Scholar]
- 2.CAPRIE Streeing Committee A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet. 1996;348:1329–1339. doi: 10.1016/s0140-6736(96)09457-3. [DOI] [PubMed] [Google Scholar]
- 3.Yusuf S., Zhao F., Mehta S.R., Chrolavicius S., Tognoni G., Fox K.K., Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Eng J Med. 2001;345:494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 4.Gurbel Paul A., Tantry Udaya S. Clopidogrel resistance? Thromb Res. 2007;120:311–321. doi: 10.1016/j.thromres.2006.08.012. Epub 2006 Nov 14. [DOI] [PubMed] [Google Scholar]
- 5.Angiolillo D.J., Fernandez-Ortiz A., Bernardo E. Variability in individual responsiveness to clopidogrel: clinical implications, management, and future perspectives. J Am Coll Cardiol. 2007 Apr 10;49:1505–1516. doi: 10.1016/j.jacc.2006.11.044. [DOI] [PubMed] [Google Scholar]
- 6.Smock K.J., Saunders P.J., Rodgers G.M., Johari V. Laboratory evaluation of clopidogrel responsiveness by platelet function and genetic methods. Am J Hematol. 2011 Dec;86:1032–1034. doi: 10.1002/ajh.22112. Epub 2011 Aug 2. [DOI] [PubMed] [Google Scholar]
- 7.Aleil B., Ravanat C., Cazenave J.P., Rochoux G., Heitz A., Gachet C. Flow cytometric analysis of intraplatelet VASP phosphorylationfor the detection of clopidogrel resistance in patients with ischemic cardiovascular diseases. J Thromb Haemost. 2005;3:85–92. doi: 10.1111/j.1538-7836.2004.01063.x. [DOI] [PubMed] [Google Scholar]
- 8.Gurbel et al. Change in inhibition of platelet aggregation (IPA) of <10% using light transmittance aggregometry. Circulation 107:2908–2913. http://dx.doi.org/10.1161/01.CIR.0000072771.11429.83.
- 9.Gurbel P.A., Bliden K.P., Guyer K. Platelet reactivity in patients and recurrent events post-stenting: results of the PREPARE POST-STENTING Study. J Am Coll Cardiol. 2005;46:1820–1826. doi: 10.1016/j.jacc.2005.07.041. [DOI] [PubMed] [Google Scholar]
- 10.Matetzky S., Shenkman B., Guetta V. Clopidogrel resistance is associated with increased risk of recurrent atherothrombotic events in patients with acute myocardial infarction. Circulation. 2004 Jun 29;109:3171–3175. doi: 10.1161/01.CIR.0000130846.46168.03. [DOI] [PubMed] [Google Scholar]
- 11.Gurbel P.A., Bliden K.P., Zaman K.A., Yoho J.A., Hayes K.M., Tantry U.S. Clopidogrel loading with eptifibatide to arrest the reactivity of platelets: results of the clopidogrel loading with eptifibatide to arrest the reactivity of platelets (CLEAR PLATELETS) study. Circulation. 2005;111:1153–1159. doi: 10.1161/01.CIR.0000157138.02645.11. [DOI] [PubMed] [Google Scholar]
- 12.Guha S., Sardar P., Guha P. Dual antiplatelet drug resistance in patients with acute coronary syndrome. Indian Heart J. 2009 Jan–Feb;61:68–73. [PubMed] [Google Scholar]
- 13.Kumar S., Saran R.K., Puri A. Profile and prevalence of clopidogrel resistance in patients of acute coronary syndrome. Indian Heart J. 2007;59:152–156. [PubMed] [Google Scholar]
- 14.Kar R., Meena A., Yadav B.K. Clopidogrel resistance in North Indian patients of coronary artery disease and lack of its association with platelet ADP receptors P2Y1 and P2Y12 gene polymorphisms. Platelets. 2013;24:297–302. doi: 10.3109/09537104.2012.693992. Epub 2012 Jun 21. [DOI] [PubMed] [Google Scholar]
- 15.Lau W.C., Gurbel P.A., Watkins P.B. Contribution of hepatic cytochrome P450 3A4 metabolic activity to the phenomenon of clopidogrel resistance. Circulation. 2004;109:166–171. doi: 10.1161/01.CIR.0000112378.09325.F9. [DOI] [PubMed] [Google Scholar]
- 16.Mehta S.R., Tanguay J.F., Eikelboom J.W., CURRENT-OASIS 7 trial investigators Double-dose versus standard-dose clopidogrel and high-dose versus low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomised factorial trial. Lancet. 2010 Oct 9;376:1233–1243. doi: 10.1016/S0140-6736(10)61088-4. [DOI] [PubMed] [Google Scholar]
- 17.Price M.J., Berger P.B., Teirstein P.S. Platelet reactivity & cardiovascular outcomes after percutaneous coronary intervention-a time-dependent ANALYSIS of the Gauging responsiveness with a VerifyNow P2Y12 Assay: impact on thrombosis and safety (GRAVITAS) trial. JAMA. 2011 Mar 16;305:1097–1105. doi: 10.1161/CIRCULATIONAHA.111.029165. [DOI] [PubMed] [Google Scholar]
- 18.von Beckerath N., Taubert D., Pogatsa-Murray G. Absorption, metabolization, and antiplatelet effects of 300-, 600-, and 900-mg loading doses of clopidogrel. Results of the ISAR-CHOICE (Intracoronary stenting and antithrombotic regimen: choose between 3 high oral doses for immediate clopidogrel effect) Trial Circ. 2005;112:2946–2950. doi: 10.1161/CIRCULATIONAHA.105.559088. [DOI] [PubMed] [Google Scholar]
- 19.ACC/AHA/SCAI Writing Committee to update2001 guidelines for percutaneous coronary intervention. Circulation. 2006;113:e166–286. doi: 10.1161/CIRCULATIONAHA.106.173220. [DOI] [PubMed] [Google Scholar]
- 20.Winters K.J., Jernberg T., Wallentine L. Prasugrel achieves greater inhibition of platelet aggregation and a lower rate of non-responders compared with clopidogrel in aspirin-treated patients with stable coronary artery disease. Eur Heart J. 2006;27:1166–1173. doi: 10.1093/eurheartj/ehi877. [DOI] [PubMed] [Google Scholar]
- 21.Alexopoulos D., Dimitropoulos G., Davlouros P. Prasugrel overcomes high on-clopidogrel platelet reactivity post-stenting more effectively than high-dose (150-mg) clopidogrel the importance of CYP2C19*2 genotyping. J Am Coll Cardiol Intv. 2011;4:403–410. doi: 10.1016/j.jcin.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 22.Montalescot G., Sideris G., Cohen R. Prasugrel compared with high-dose clopidogrel in acute coronary syndrome. The randomised, double-blind ACAPULCO study. Thromb Haemost. 2010 Jan;103:213–223. doi: 10.1160/TH09-07-0482. [DOI] [PubMed] [Google Scholar]
- 23.Wallentin L., Becker R.C., Budaj A., PLATO Investigators Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045–1057. doi: 10.1056/NEJMoa0904327. [DOI] [PubMed] [Google Scholar]
- 24.Gurbel P.A., Bliden K.P., Butler K. Response to ticagrelor in clopidogrel nonresponders and responders and effect of switching therapies: the RESPOND study. Circulation. 2010;121:1188–1199. doi: 10.1161/CIRCULATIONAHA.109.919456. [DOI] [PubMed] [Google Scholar]
- 25.Harrington R.A., Stone G.W., McNulty S. Platelet inhibition with cangrelor in patients undergoing PCI. N Engl J Med. 2009;361:2318–2329. doi: 10.1056/NEJMoa0908628. [DOI] [PubMed] [Google Scholar]


